HNN124 Exam Revision
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
Pre-procedural assessment considerations
Age-related considerations
Infants’ physiological functions are immature - therefore at risk during surgery
Surgical morbidity and mortality rates for ppl over 90 are higher than 70-75 age group
Complicated by chronic disease
Social and cultural considerations
Spiritual considerations
E.g. requesting to see a minster of religon before surgery, not allowing blood transfusions as part of treatment
Psychosocial status
Assess degree or understanding + anxiety regarding procedure
Assess knowledge of procedure + expected outcomes
Pre-procedural physical assessment
skin condition, pre-existing conditions, nutrition status, physical/mobility limitations
Includes nursing/ medical hx + physical examination
medications, allergies
Complete assessment performed at outpatient clinic during pre-admission visit
On the day of surgery, conduct focused assessment to ensure current, accurate data
Evaluate anxiety and fear level
Pre-procedural general survey
Observe person's condition
E.g. gait, assistance with mobility, skin temperature, level of consciousness + orientation, response to questions
Skin (everywhere) – temperature, texture, integrity
ROM – everywhere including oral cavity
head + neck
Assess if eye contact is maintained
Condition of scalp - e.g. alopecia or seborrheic dermatitis
Oral cavity - loose teeth, tongue. Mucous membranes
Lips and tongue, dentures, caps, bridges or crowns
Neck - strength of carotid pulses, palpate jugular veins, cervical lymph nodes
Upper extremities
Brachial + radial pulses - rate + character of pulse
Capillary refill
Anterior and posterior chest + abdomen
Inspect + palpate chest wall - note breathing pattern and expansion
Auscultate heart sounds
Anterior and posterior breath sounds - crackles, gurgles, wheezing
Lower extremities
Length and position of legs
Palpate bilateral strength of femoral, popliteal and pedal pulses
Capillary refill
Preoperative problem identification
deficient knowledge caused by: pre-op preparation to decrease post-op risks
anxiety caused by
deficient knowledge
risk factors + anaesthesia
fear caused by
unknown
effects o
Intraoperative problem identification
risk for perioperative positioning injury caused by:
oedema
ineffective tissue perfusion
impaired physical mobility
disturbed sensory perception
impaired skin integrity
risk for injury caused by
physical, environmental, positional, chemical
fluid volume
cardiac output
risk for infection caused by
invasive procedure
imbalanced nutrition
impaired skin/ tissue integrity
latex allergy
hypothermia caused by
decreased metabolic rate
exposure to cool enviro
excess/ deficient fluid volume
Common nursing identified problems pre-op
Deficient knowledge related to surgery
Anxiety and/ or fear
Postoperative problem identification
ineffective airway clearance caused by
anaesthesia (diminished cough reflex)
increased pulmonary ingestion
e.g. pneumonia, atelectasis, pulmonary embolism
ineffective tissue perfusion (cardiopulmonary) caused by
anaesthesia
position or immobility
imbalanced nutrition (less than body req.) caused by:
anaesthesia
surgical manipulation of intestines
fasting
e.g. GIT → N+V, constipation retention of tas
urinary retention caused by
anaesthesia
surgical manipulation of the bladder
e.g. UTI
acute pain
risk for infection
e.g. dehiscence, evisceration
low self-esteem
altered body image + effects of surgery
dependence on others during recovery
Pre-op preparation (implementation)
review surgery + prescribing practitioner orders
obtain person’s hx, physical assessment, blood + urine specimens; notify prescribing practitioner of abnormal diagnostic test results
Pre-op checklist
Surgical consent form
Nurse should verify that consent has been obtained
Can identify problems when pt:
Can't explain procedure/ identify risks
Signed the form over a year before surgery
Had unauthorised person sign consent form
Didn't sign consent form
Signed a form with incorrect surgical site/ incongruent procedure
Individual teaching
Teaching pt + family is responsibility of multi-disc team
Verify pt/family can describe reason for surgery, what will be done, side effects of anaesthesia + complications
Nurse - plays role in relieving anxiety + reinforcing teaching regarding pre-op care
Teaching aids should reinforce nurse's verbal instructions
Discharge planning - role of the nurse
Communicating openly with pt's + family etc. + shared decision making
Ensuring discharge summary has correct + relevant info
Providing tailored patient education
Ensuring discharge requirements are documented and met
Role of the nurse in relation to therapeutic and professional communication
Registered Nurse
Therapeutic communication aims to build trust with the patients, encouraging them to express feelings and providing emotional support
Active listening
Empathy
Open-ended questions
Professional communication is structured and goal-orientated when you interact with other healthcare workers. Both will help to better patient outcomes.
Individual teaching
Nurse - plays role in relieving anxiety + reinforcing teaching regarding pre-op care
Prepare peri-operative procedures and spinal precautions
Risks that need to be considered pre-procedurally to manage care
Age
comorbid conditions/ medical problems
lifestyle: nutrition; smoking/ alcohol/ substance abuse
pregnancy
diabetes
medications
cognitive problems
Ask patient questions - test their understanding e.g. what the procedure name means to them
Identify patients correctly
Use medicines safely
Before a procedure, label all medicines (e.g. medicines in syringes, cups and basins)
Be aware or patients who take medicines to thin their blood
Record + pass correct info about patient's medicines
Find out what meds they're taking + compare to new medicines
Give education about medicine
Ensure they bring up to date list of medicines when visiting a doctor
Identify patient safety risks E.g. falls + reduce risk for suicide
Prevent mistakes in surgery
Ensure correct surgery done on correct patient
Mark correct place on patient's body where surgery is to be done
Pause before surgery - prevent mistakes'
Perform peri-operative procedures and spinal precautions
Instrument nurse: establishes + maintains the safety, efficiency and integrity of the sterile field throughout the surgical or invasive procedure
circulating nurse: coordinates + directs the activities of intra-op environment during the surgical procedure; supports scrub nurse + gathers additional equipment if needed
anaesthetic nurse: prepares equipment and the person for anaesthesia; assists anaesthetist in all phases of anaesthesia
Post- op monitoring
Consider: surgery type, anaesthetic type
Includes:
Vital signs
State of consciousness
Pain and comfort
Nausea
Wound + drains
Catheters
IV fluids and site
Fluid balance
Postoperative limb and chest physio
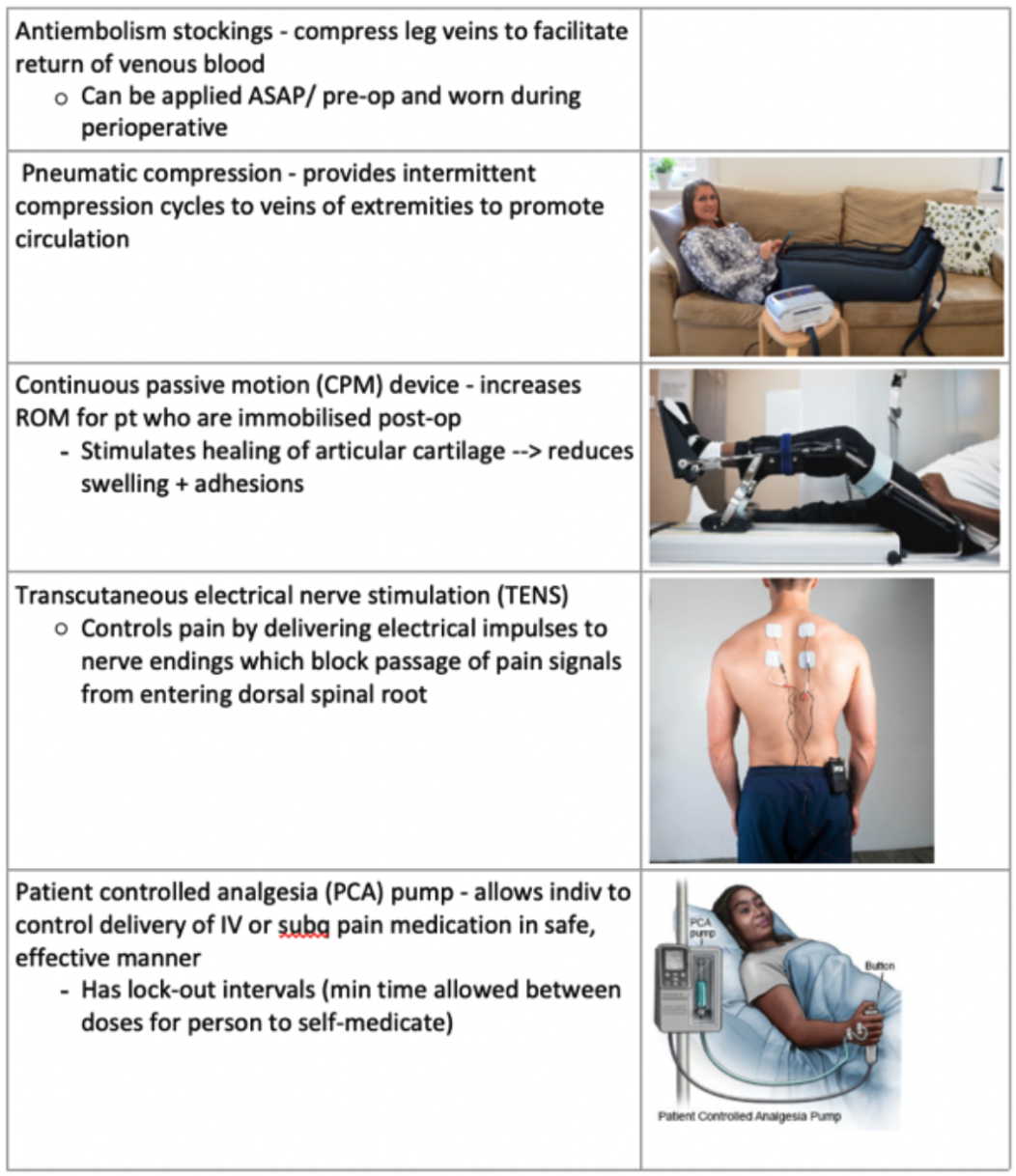
Devices that prevent post-op complications/ pain
Principles of respiratory management
Airway maintenance: keep airway clear using suction/ intubation
Ventilation support: e.g. oxygen therapy or mechanical ventilation
Monitoring: pulse oximetry, ABGs, capnography (monitoring of CO2 conc. in resp. gas)
Lung expansion: encourage deep breathing, proper positioning and incentive spirometry to prevent lung collapse
Preventing complications: use chest physiotherapy, ensure hydration and control infection
Medications: such as bronchodilators, corticosteroids and antibiotics
Patient education: teach breathing techniques + encourage smoking cessation
Three fundamental respiratory management techniques
optimise gas flow
Sit them up, support with pillows
Do a pain assessment
Guedel airways
Nasal/oral/ oral endotracheal/ tracheostomy tubes
What therapeutic substances can improve the person's respiratory function + oxygenation?
Oxygen therapy
Through a nebulizer/ metered inhaler/ spacer (aimed at dilating airways)/
Mobilising secretions
Strategies: appropriate positioning, chest physiotherapy, percussion, Yankauer sucker, hydration,
Prepare, provide and document oxygen therapy
oxygen is used to treat hypoxia or any condition that could cause it
standard ward flow is 15L oxygen
nasal prongs maximum 4-6L minutes
simple face masks at least 5L/ min
more than 8L requires Venturi mask
Respiratory management (Assessment)
patient history, respiratory status, auscultation of lungs, monitoring oxygen saturation,
physical examination
inspect effort, distress, positioning, chest configuration, cyanosis, oedema, clubbing
Chest palpation related to compromised ventilation
Vocal fremitus: palpable vibration felt on a patient's chest wall when they speak, caused by sound vibrations from the vocal cords that are transmitted through the lungs
Displacement of the trachea
Percussion: Hyper-resonance, dull tone, changes in density of the lungs + surrounding tissues
Auscultation
Adventitious breath sounds: abnormal noises beyond typical breathing
e.g. fine/ coarse crackles, sibilant/ sonorous wheezes, pleural friction rub, stridor)
factors affecting oxygenation
age
older ppl - req increased effort to expand lungs + more susceptible to respiratory infection
due to decreased cilia activity
environmental + lifestyle factors
smoke, smog, dust, asbestos, toxic chemicals at home/work
significant physical/ emotional stress
over/ underweight
diseases
COPD - airways are blocked
diffusion defects
circulatory influences
ventilation-perfusion mismatching: imbalance between ventilation + perfusion
haemoglobin alterations
Respiratory management (Problem identification)
Ineffective airway clearance
obstruction (by tongue, secretion, foreign object) or by oedema of the larynx
partial occlusion of bronchi / bronchioles by infection
Impaired gas exchange
Occurs when adequate oxygen doesn't enter arterial blood OR CO2 isn't removed from the venous blood
Decreased cardiac output
Impairs oxygen delivery to the tissues
May be a factor in impaired gas exchange
Ineffective tissue perfusion
May be widespread (e.g. decreased CO)
or confined to one or more tissues or organs of the body
CO + tissue perfusion likely to be experiencing:
oedema of lower extremities + lungs
Fatigue
Activity intolerance
other problems:
Deficient knowledge
Activity intolerance (impact of illness on person's ability to perform ADL)
Insomnia
Imbalanced nutrition
Acute pain
Anxiety
Respiratory management (planning)
sets goals
e.g. improving oxygenation, clearing airway, preventing complications
Intervention to improve oxygen uptake and delivery
Administer oxygen
% of oxygen in inspired air is fraction of inspired oxygen (FIO2)
Expressed as %
Normal atmospheric air has FIO2 of 21%
Supplemental O2 delivery systems can increase FIO2 to anywhere from 24% to nearly 100%
78% of inspired air is nitrogen
Keeps alveoli open (just by occupying space)
Complications/ hazards of oxygen administration
Those with chronic pulmonary disease assoc w CO2 retention (hypercapnia) (e.g. COPD) can become insensitive to CO2 levels to drive their RR
May depend on chronic low O2 blood level (hypoxaemia) to stimulate respiratory drive
Excessive O2 administration may obliterate hypoxic drive --> apnoea
O2 toxicity: may be caused from prolonged administration of high FIO2 (>50% for >2hrs)
Damage to lung tissue + prod severe resp difficulties
Interventions to increase cardiac output + tissue perfusion
Manage fluid balance
If congestive heart failure present:
Fluid intake is restricted - prevent oedema + circulatory overload
Sodium intake limited (Sodium promotes fluid retention)
Diuretics may be given to increase fluid excretion by kidneys
Should be given before mid-afternoon so sleep isn't affected
Monitor fluid I&O + daily weights
Activity restrictions + assistance with ADLs
Purpose of assisting --> decrease oxygen demands of body
Tolerance may be slowly increased through cardiac rehab program
Proper positioning
Done to increase fluid load to heart
Decrease development of pulmonary oedema
Venous system can pool blood (when assisted with gravity)
'venous capacitance' (aka pooling effect) is increased when head + upper body is elevated, legs are in dependent position
Supine position may be detrimental for person with congestive heart failure
Administer medications
Diuretics: affects renal tubules → increased water excretion → lowers BP + cardiac workload
Cardiac glycosides: increases force of cardiac contraction + slows HR
Inotropic agents: increases force of cardiac contraction
Antihypertensives: lowers BP → decreases workload
Nitrates: dilates coronary arteries + peripheral vessels → increase cardiac O2 supply → decrease cardiac workload
Vasodilators: widens vascular system to improve blood flow + reduce BP
Interventions to address associated respiratory problem
Lifestyle + activity adaptations
3 general purposes:
Minimise energy + oxygen consumption
Complete bed rest is often NOT the best option
Lifestyle adaptations aimed at reducing factors contributing to disease process:
Removal of allergens
Stopping smoking
Control modifiable risk factors for heart disease
Modification of cardiac risk factors:
Stop smoking
Dietary alterations + weight control
Control of diabetes + hypertension
Exercise + stress management
Encourage dietary + nutritional modifications
Usually include: reduction of sodium, total fat and cholesterol intake
Person receiving inadequate nutrient intake from poor appetite/ severe dyspnoea will need help in finding ways to increase intake
Promote comfort
Pain related to tissue ischaemia is best relieved by --> improving O2 delivery to tissues while reducing oxygen demand
Rest the affected tissue e.g. rest the leg/arm
May involve positioning legs lower than heart level (elevating them often makes pain worse)
Heart pain related to iscahemia (angina pectoris) should be dealt with first and foremost by resting
Complementary therapies
Meditation + yoga produce relaxation + calmness
Explain and demonstrate the role of the nurse in relation to chest physiotherapy
Collaboration
working with physiotherapists to develop + adjust patient care plans
Assessment
conducting initial assessments and monitoring patients’ progress during therapy
Patient Education
informing patients about the benefits of physiotherapy and teaching prescribed exercises
Support
assisting patients physically during therapy sessions and providing emotional support
Documentation
recording patients’ responses to therapy and ensuring CoC
Rehabilitation (more detail later)
Chest physiotherapy (rehabilitation techniques)
Teach effective coughing
Should be preceded by slow, deep breaths
E.g. huffing: delivering a series of short, forceful exhalations
Intent is to raise sputum to level where it can be coughed out
Assisting person to sitting position will increase effectiveness of the cough
Initiate postural drainage + chest physiotherapy
Intended to promote the drainage of secretions from the lungs
Accompanied by percussion or vibration applied to chest wall to loosen secretions
Administer medications
Assist in airway clearance e.g. expectorants, mucolytics and bronchodilators
Monitor environmental and lifestyle conditions
e.g. Smoking
Introduce artificial airways
Guedel's airway
Maintains the tongue away from posterior oropharynx in unconscious person
Essential to choose correct size --> too large may cause occlusion; too small may compress tongue + stimulate vomit
Endotracheal tubes: bypass the upper airway structures
Passed beyond vocal cords into trachea
Nutritional care
Providing entera feeding / total parenteral nutrition
Suction the airway
May be necessary to clear secretions the person cannot remove by coughing
Especially important when endotracheal/ tracheostomy tube is present --> coughing is impaired by these devices
Nasotracheal or endotracheal suctioning
Properly position person
Help them breath
Tripod position
Teach controlled-breathing exercises
Improve breathing efficiency
E.g. pursed-lip breathing
Involved forced exhalation against pursed lips
Deep breathing exercises: encourage slow, deep breaths
(instead of rapid, shallow, breathing) --> May be present in restrictive lung disease or anxious people
Incentive spirometry: measures volume of air displaced by moving float ball/ similar device up a column
Manage chest-drainage systems
removing accumulations of air + fluid from pleural space (improve breathing patterns)
Recognise requirements of escalation of care and basic life support algorithm
DRSABCD
Danger, response, send for help, airway, breathing, compressions, defibrilator
Escalation of care requirements
Assessment: regularly monitor vital signs and use clinical judgment to identify pt deterioration
Recognising deterioration be aware of early warning signs, such as confusion or changes in VS, and utilise scoring systems like Early Warning Scores (EWS)
Initiating protocols: follow established escalation protocols, notify a physician or activate emergency response teams as necessary
Communication: ensure effective handover + keep patient’s family informed about changes in condition
Emergency interventions
Remove airway obstruction
Complete airway obstruction is characterised by inability to speak/cough
Victim may raise hands to throat, appear very anxious
Initiate CPR (cardiopulmonary resuscitation)
Cardiac/ respiratory arrests require artificial support of circulation + ventilation
Pharmacological acute pain management
analgesics:
non-opioids: acetaminophen and NSAIDS for mild-moderate pain
opioids: for moderate to severe pain (with careful monitoring)
adjuvants: antidepressants + anticonvulsants for neuropathic pain
routes: orally, IV or regionally
multimodal: combines different medications for improved relief
preferred method for providing post-op pain management
Involves the use of meds from diff drug classes targeting diff pain pathways to control pain
With the goal of using fewer or ideally eliminating need for opioids
monitoring: regular pain assessments + side effect
pt education: inform about medications + safe usage
Trying to avoid morphine + opioids --> due to addictive properties + unwanted side effects
Non-pharmacological acute pain management
Physical:
heat/ cold therapy, physical therapy,
Cognitive-behavioural
Meditation music, relaxation, distraction, mindfulness
acupuncture + massage (alternative for relaxation + pain relief)
environmental modifications: create calming enviro to enhance comfort
Nurse’s role in acute pain management
Pain management goal: relieving pain while ensuring that side effects are kept to a minimum
Assessment
Regularly assess effectiveness of pain management interventions by monitoring pain levels, functional abilities, and overall patient satisfaction
Problem identifiation
pain
anxiety etc.
Planning
Modify pain management plan as necessary based on the evaluation findings and any changes in the patient’s condition
Implementation
non-pharm./ pharm. interventions
Patient’s role in pain management
Provide feedback about effectiveness of pain management strategies – what worked/ didn’t work
Actively communicate changes in pain levels/ new symptoms during treatment
Describe, perform and document pain assessment in the post-procedural context
PQRST or COLDSPA
Provocation, quality, region, severity, time
Character, onset, location, duration, severity, pattern, associated factors
Once patient can communicate (anaesthesia wears off), nurse can consider using:
Numerical pain rating scale (0-10)
Wong Baker scale
Prepare, perform and document parenteral analgesia
Prepare
Pt identity, medical hx, current pain level
Obtain prescribed analgesic + gather supplies (syringe, alcohol swabs, gloves)
6 rights: Time, dosage, medication, patient, route, documentation
Prepare medication by cleaning vial, drawing up correct dosage, ensuring no air bubbles
Perform
Position comfortable + select appropriate site
IM: deltoid, ventro-gluteal
Subcutaneous: abdominal, thigh
Clean site
Administer injection
Documentation
Pt info, medication details, time of administration
Record patient’s pre- and post-administration pain levels and any observed responses or side effects
Subcutaneous
Fat + connective tissue
Risks:
Bruising
Pain
Swelling
Infection
Redness
Local reactions
Fibrosis
abcess
Intramuscular
Muscle
More blood flow + more absorption
. | Absorption | Angle of insertion | Site | Needle size | Volume to be injected |
Subcutaneous - fat + connective tissue | Slower | 45º | Abdominal | 25-27g | ~2ml |
Intramuscular - muscle | Faster (more blood flow to muscles) | 90º | Deltoid Ventrogluteal | 23-25g | ~5ml |
Explain the pathophysiology of fluid and electrolyte imbalanceFluid imbalance:
Types: hypovolemia (decreased fluid volume) and hypervolemia (increased fluid volume)
Causes: fluid loss (e.g. vomiting, diarrhoea) or retention (e.g. heart or renal failure)
Mechanisms: changes in osmotic gradients and hormonal regulation (e.g. aldosterone, ADH)
Electrolyte imbalance:
Types: hyponatremia (low sodium), hypokalaemia (low potassium) and hyper- vice versa
Causes: decreased intake, increased losses (e.g. urine, sweat)n or shifts between compartments
Mechanisms: disruption of cellular function and hormonal regulation (e.g. PTH for calcium)
Consequences
CVS issues
Muscle dysfunction
Neurological symptoms
Respiratory distress
Electrolyte: compound that when dissolved in water or another solvent forms or dissociates into ions
Electrically charged particles
Provide inorganic chemicals - for cellular reactions and control mechanisms
Have special physiological functions in the body that:
Neuromuscular irritability
Maintain body fluid osmolarity
Regulate acid-base balance
Distribute body fluids between the fluid compartments
Measured in terms of their electrical combining
Quantities of cations and anions (expressed as millimoles per litre mmol/L)
Produce either positively charged ions (cations) or negatively charged ions (anions)
Critical regulators in the distribution of body fluid
Electrolytes in body fluid are sodium (Na+), potassium (K+), calcium (Ca2+), magnesium (Mg2+)
-tonic definitions
Isotonic: equal solute concentration; no net water movement
Hypertonic: higher solute concentration; water moves out of cell
Hypotonic: lower solute concentration; water moves into cells
Sodium
Function: maintains fluid balance, facilitates nerve transmission and supports muscle contraction
Sources: table salt, processed foods, meats, dairy products
Potassium (K+)
Function: regulates cellular function, supports nerve transmission, maintains CVS health
Sources: rich in bananas, oranges, potatoes, spinach, avocados and legumes
Calcium (CO2+)
Function: essential for bone health, muscle contraction, nerve transmission, blood clotting
Sources: dairy products, leafy greens, almonds, tofu, fortified foods
Magnesium (Mg2+)
Functions: acts as a cofactor for enzymatic reactions, regulates muscle + nerve function, supports bone health
Sources: present in whole grains, nuts, seeds, legumes and green leafy vegetables
Diffusion
Diffusion: particles move across permeable membrane
rate is influenced by size of molecule, concentration, temperature of solution,
and electrical charge: +ve ions pulled towards -ve ions etc.
move with conc gradient
osmosis
osmosis: solvent moves across membrane to an area where there is a higher concentration of solute that can’t pass through the membrane
osmotic pressure: force created when 2 solutions of diff. conc. are separated by selectively permeable membrane
rate is influenced by net movement of water + semipermeability of membrane
active transport
active transport: cell membrane MOVES molecules/ ions against electrochemical gradient (and against conc gradient)
must be carrier + ATP inside the cell membrane
hydrostatic pressure (HSP)
hydrostatic pressure (HSP): force of fluid pressing outward against blood vessel wall; drives fluid out of the blood vessel
HSP of arterial end of capillary bed = HSP venous end x2
fluid + solutes go from arterial → interstitial space
force is influenced by: force by which heart pumps, rate of blood flow, arterial + venous BP
filtration
filtration: movement of fluid through semi-permeable membrane from area with higher HSP → area with low HSP creates outward gain of fluid in the interstitial spaces
governed by presence of a greater HSP in arterial end cap. than interstitial spaces
body achieves total fluid balance when excess fluid + solutes remaining in interstitial spaces are returned to intravasc. compartment by lymphatic
colloid osmotic pressure
colloid osmotic pressure: movement of fluid between intravasc. and interstit. compartments
colloids: protein or diffusible substance
crystalloids: intravenous fluids composed of small molecules (e.g. salts, sugars) that can pass through cell membranes easily
used to expand extracell. fluid volume. Typically iso-, hypo- or hyper-tonic.
Effective for hydration, electrolyte replacement, maintaining fluid balance
based on no. of solute particles on the conc. side + presence of semipermeable membrane
created by solutes / colloids in plasma
Principles of fluid and electrolyte management
Assessment: regularly evaluate patient’s fluid and electrolyte status through clinical signs, vital signs, intake and output monitoring and lab tests
Fluid + electrolyte replacement: use oral or intravenous solutions for fluid and electrolyte replenishment, choosing the right type based on specific imbalance
Understanding physiological principles: recognise roles of osmolarity + hormonal regulation in fluid and electrolyte balance
Prevention of complications: avoid rapid corrections of imbalances and educate patients on recognising signs of disturbances
Role of the nurse in relation to altered fluid and electrolyte status using the nursing process
Assessment: conduct comprehensive assessments that include pt hx, physical examination, lab values, monitoring or I+O to identify issues (e.g. dehydration, oedema, electrolyte imbalances)
Problem identification: recognise specific problems or risk factors related to fluid and electrolyte imbalances. Common issues might include:
Excessive fluid loss/ gain
Electrolyte deficits or excesses
Impaired ability to regulate fluid and electrolyte balance
Risk for complications related to fluid overload or dehydration
Planning
Implementation: carry out interventions aimed at addressing identified problems (e.g. administering fluids/ electrolytes), educating patient about fluid management, monitoring for signs of complications
Evaluation: continuously assess effectiveness of interventions to determine if identified problems are being resolved or if further action is required
Prepare parenteral fluid and electrolyte administration
Indications | Risks | Nursing considerations |
|
|
|
Assess pt needs + select appropriate solution (crystalloids or colloids)
Gather necessary supploes, perform hand hygiene, prepare IV site with an aseptic technique
Perform parenteral fluid and electrolyte administration
Insert IV catheter , connect + prime IV set, begin infusion at prescribed rate.
Changing the IV bag:
don’t let the old bag empty entirely - to prevent air entering drip chamber + line
when bag has ~50 mL of fluid remaining, stop flow of solution
prepare to change bag when there’s about an hour’s worth of fluid remaining in old bag
Document parenteral fluid and electrolyte administration
solution bag changes
discontinuation of fluid order
appearance of IV site
type + amount of fluid infused
infusion rate
person’s response to procedure
abnormal findings
Principles of wound management
TIMERS
Tissue
Infection/ inflammation
Moisture
Edge of wound
Regeneration
Social factors
Pathophysiology of diabetes and health outcomes
diabetes can damage:
large blood vessels (aka macrovascular complications) —> heart attack, stroke, circulation problems in lower limbs + feet
small blood vessels (aka microvascular complications) —> problems in eyes, kidneys, nerves (e.g. in feet, sexual function)
body, skin, teeth, gut, gums
large blood vessels
main cause of damage to LBV in ppl with diabetes is atherosclerosis
atherosclerosis: occurs when plaque - made up of cholesterol, other blood fats + substances - builds up inside the wall of the blood vessels
causes blood vessels to narrow + reduces blood flow to organs + other parts of body
if plaque breaks, can form blood clot that can block blood supply to organs and other parts of body
wounds need blood to heal
Insulin and glucagon balance
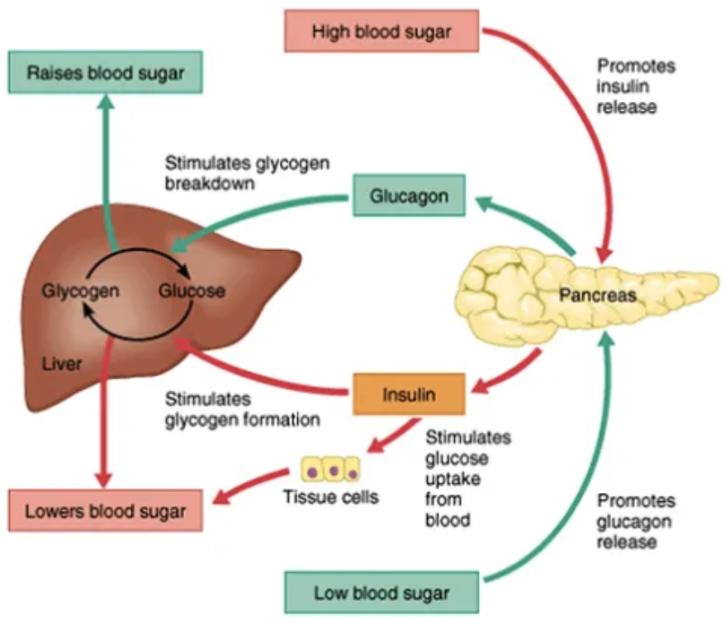
high blood sugar
→ insulin release from pancreas → stimulates glucose uptake (glucose turns into glycogen
Type 1 VS Type 2 diabetes
Features | Type 1 diabetes | Type 2 diabetes |
5-10% of diabetes cases | 87% of all diabetes cases | |
Onset (rapid or slow?) | rapid (often abrupt) - relieved when insulin given | slow (gradual, often over year) - some ppl don’t have symptoms, can remain undiagnosed for yea |
Pathophysiology | Insulin deficiency due to autoimmune destruction of beta cells | Cells become resistant to insulin, inadequate insulin secretion by pancreas |
Risk factors | family hx, genetics, autoimmune diseases | family hx, obesity, sedentary, lifestyle, age, ethnicity, hypertension |
Common age at onset | childhood/ adolescence (usually <30 y.o) | adulthood (usually >40 y.o increasingly seen in younger ages) |
Symptoms leading to diagnosis | polyuria, polydipsia (excessive thirst), weight loss, fatigue, rapid onset of symptoms, thrush/ genital itching. slow wounding healing, blurred vision (glucose builds up in lens of eye), hunger (triggered by body seeking energy), ketonuria (ketones in urine), dry mouth + itchy skin | Polyuria, polydipsia, fatigue, slow onset, often detected incidentally, blurred vision, slow healing, thrush, hunger, dry mouth + itchy skin |
Long term symptoms | Increased risk of kidney disease, retinopathy, neuropathy, cardiovascular disease. yeast infection (yeast feeds on glucose) slow healing cuts + sores, pain + numbness in feet + legs (from nerve damage) | Same complications as type 1, but also increased risk due to late diagnosis. |
Treatment/ management | Insulin injections, blood sugar monitoring, diet, exercise | Lifestyle changes, oral medications, possibly insulin, blood sugar monitoring, resensitising receptors with drugs |
Does insulin have to be provided? | Yes, always | Not always; may eventually be needed if oral medications aren't enough |
Prevention | Can’t be prevented | Can often be prevented or delayed with external changes |
Factors that may influence wound healing
Age
Body type
Obesity 🡪 fatty tissue has poor blood supply
Emaciation (very thin) 🡪 lack of oxygen + nutritional stores
Malnutrition 🡪 reduces humoral + cell-mediated factors => immunocompromise => impairing wound healing + increasing infection risk
Nutrition
Oxygenation
Decreased arterial O2 => synthesis of collagen + formation of epithelial cells
Anaemia decreases oxygen delivery to tissues + interferes with tissue repair
Chronic disease
Other: smoking, repeated trauma (onto wound), infection, maceration
Hyperglycaemia: high BGL damages blood vessels + impairs immune response
Long term effects of hyperglycaemia
Neuropathy: loss of sensation increases risk of unnoticed wounds.
Vascular damage: impaired circulation leads to poor oxygenation and delayed healing
infection risk: high glucose levels promote bacterial growth + worsen infection outcomes (slow healing)
Role of the nurse in relation to the principles of wound management using the nursing process
Assessment
TIMERS
Collect data about the wound (size, type, depth, exudate, infection), overall pt heath (e.g. nutrition + circulation)
Problem identification
Identify key issues affecting wound healing (e.g. impaired circulation, risk of infection, delayed healing due to diabetes)
Planning
Develop a care plan with goals (e.g. reducing wound size, preventing infection)
Select appropriate interventions (e.g. dressings, medication, lifestyle changes)
Implementation
Perform wound care, apply dressings, monitor for complications, educate patient on home care
Evaluation
Monitor healing progress, reassess problems + modify care plan if needed
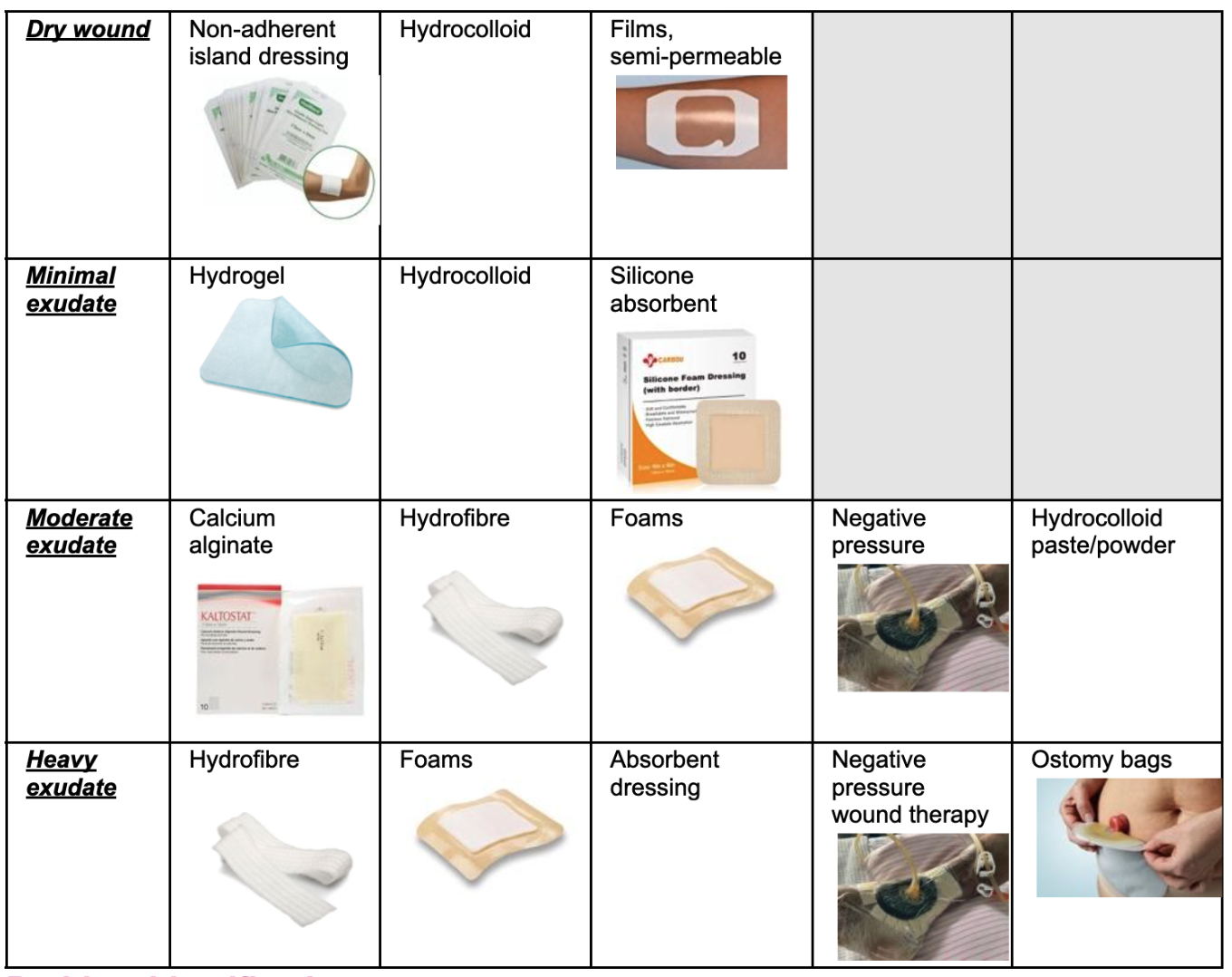
Types of wound dressing for types of wounds
Perform the donning of sterile gloves and explain when sterile gloves are indicated.
Check date + integrity of the glove packaging prior to opening sterile glove in a package onto a clean surface
Open up glove packet
Place dominant hand into glove – only touch distal portion of cuff (the inside)
Use dominant gloved hand to put glove onto other hand (DON’T TOUCH OUTSIDE AREA USING DOM HAND)
Prepare wound dressing
***Provide analgesia prior to dressing
PPE
Gown
Sterile gloves
Normal gloves (to remove the dressing depending on nature of wound + hospital policy)
Equipment
Surgical dressing pack
Dressing equipment (alginate, sterile scissors if needed)
Sterile solution
Sodium chloride to irrigate
Perform wound dressing
Hand hygiene
Set up dressing pack + all sterile equipment
Remove old dressing
Put on sterile gloves
Clean wound (from cleanest to dirtiest area)
Assess wound – does the packing material need to be cut?
Pack under the edge of the skin (edges first)
Packing should be BELOW skin level – otherwise will grow abnormally
Put film on top
Suture/ staple removal
Prepare suture/ staple removal
Equipment: stitch cutter (like a hook blade) OR staple remover
Perform suture/ staple removal
HH + gloves
Get dressing pack + saline
Clean the cut - using saline + tweezers
Grab tweezers + scissors (sutures) OR staple removers + sharps bin (staples
Sutures: pull the suture up using tweezers, slide underneath + cut with scissors
Staples: slide under the staple, press down, discard in sharps bin
Clean again
Principles of post procedural gastrointestinal management
Monitoring: VS, pain, GI function for complications
Manage pain: medications (avoiding ones that cause constipation)
Gradually reintroduce fluids + food as tolerated
Prevent complications: e.g. N+V, constipation
Interventions such as positioning + medication
Educate: pt on post-op care, diet + signs of complications
Role of the nurse in relation to post procedural gastrointestinal management using the nursing process
Assessment
Collect data: VS, bowel sounds, abdominal distension, pain levels, fluid/ nutritional intake
Complications e.g. N+V or bleeding
Problem identification
Common presenting symptoms: constipation, diarrhoea, N+V
Infection
Pressure injuries
Pain
Impaired GI motility
Dehydration
Disorders (more info later)
Planning
create goals e.g. relieving pain, ensuring adequate hydration + nutrition, preventing complications (e.g. aspiration + constipation)
Implementation
interventions such as administering prescribed analgesics, gradually reintroducing fluids + food, managing nausea, positioning pt (reduce discomfort + pressure injuries)
Evaluation
reassess patient’s condition to determine effectiveness of interventions, monitor progress in bowel function recovery + adjust care plan as needed
Disorders of the GIT
Peptic ulcer disease: break/ ulceration in mucosal lining of the lower oesophagus, stomach or duodenum
Damages lining
Inflammatory bowel disease: inflammatory conditions of the bowel
Appendicitis: inflammation of the appendix
Prepare NGT
Equipment
NGT
lubricant
catheter tip syringe (to aspirate)
drainage bag
nose stickers (to hold the NGT)
Indications | Risks | Nursing Considerations |
|
|
|
Perform NGT
Wear gloves
Measure from tip of nose to ear, to xiphoid process. Note length/number
Attach end to catheter needle
Lubricant
Put it in from nose, keep pushing in until noted length
Sticker it to nose
Aspirate to check it’s in stomach
Kink/fold it (so it doesn’t leak) and remove from needle and attach to drainage bag
Post insertion
X ray and aspirate to ensure it’s in tight spot
PH test
Document NGT
Type + size of NGT used
Confirmation of placement + length of tube (from nares to hub)
Amount of aspirate and its nature, including pH
Type of apparatus connected (e.g. suction + pressure setting, gravity drain)
Person’s response to procedure
Prepare stoma assessment + appliance change
Indications | Risks | Nursing Considerations (for position) |
|
|
|
Equipment
Kidney pan (leakage)
Clean pouch
Stoma measuring guide
Ostomy scissors (to cut the guide)
Clean gloves
Adhesive remover
Bluey
Locker bags
Perform stoma appliance change
Wear apron and gloves
clean area, remove any leaked feces
remove old bag
measure NEW stoma, cut it to fit.
Stick it on
Close bag
Document stoma assessment/ appliance change
each stomal assessment
alteration in stomal size
change in colour (pallor/ cyanosis → indicative of altered circulation)
presence + degree of skin irritation
amount + type of drainage and/ or effluent
skills learnt by pt
bleeding of stoma
altered circulation
diminished or increased drainage
consistency
Pathophysiology + signs/ symptoms of a post procedural wound
Post-procedural wound
hemostasis: clot formation to stop bleeding
inflammatory phase: white blood cells clean wound 🡪 redness + swelling
proliferative phase: granulation tissue forms as new blood vessels and collagen develop
remodelling phase: collagen reorganises to strengthen the wound
Signs and symptoms
redness (erythema)
swelling
fever - high temp
drainage
clear - doesn’t indicate infection. may mean other things
yellow, murky - usually indicative of bacterial infection
green - pseudomonas infection of a wound (treated differently)
lots of pain
foul odour
non-healing
Pathophysiology + signs/ symptoms of a chest infection
community acquired: can occur from organisms entering (strep + flu bacteria/virus)
ventilator acquired: bacteria/ organisms/ etc that enter tube can grow → cause pneumonia infection
device connected to tube delivering O2 to pt
aspiration (acquired): common for pt who vomit - can aspirate it into lungs (open epiglottis)
infection is inside alveoli 🡪 alveolar tissue inflames + leaks fluid 🡪 air goes DOWN, but is blocked by fluid 🡪 blocks entering of oxygen + exiting of CO2
signs + symptoms
dyspnoea (SOB)
chest pain
cough - body trying to eject fluid
fever - infection
What is antimicrobial stewardship?
Antimicrobial stewardship: careful use of antimicrobials to prevent bugs from developing resistance
Role of the nurse in antimicrobial stewardship
Assessment: evaluate patients for infection and review medical histories to ensure appropriate antimicrobial use
Make sure you always check if the patient has their allergies recorded and encourage patients/parents to report side effects promptly.
Encourage patients/parents to report side effects promptly.
Education: inform patients about responsible antibiotic use and adherence to prescriptions
Help patients/families to understand the importance of avoiding unnecessary antibiotics – for example, explain that antibiotics don't work for viral infections like the flu.
Collaboration: work with healthcare teams to select, dose and monitor antimicrobial therapies based on guidelines
Ask the medical team what the antibiotics are being used for if the indication has not been documented on the medication chart to avoid miscommunication.
Monitoring: track patient responses to treatment and adjust as necessary
Doctors sometimes miss ceasing treatment in a timely way. It is OK to ask: "how many more days of antibiotics are expected?"
Data collection: help gather information on antimicrobial use and resistance to improve practice
Ensure that the appropriate tests (e.g. urine specimen, blood cultures) are taken before antibiotics are commenced when possible.
Role of the nurse in infection prevention and control
Adherence to protocols: follow HH, PPE, aseptic techniques
Environmental cleaning: maintain cleanliness in pt areas and ensure proper sterilisation of equipment
Patient education: teach infection prevention practice to Pt + families
Surveillance: monitor patients for signs of infection + report outbreaks
Reporting + documentation: document infection rates + interventions for tracking effectiveness
Role of the nurse in relation to pre-procedural infection prevention and control
Assessment
Evaluate pt hx, existing skin integrity
Wound assessment
Problem identification
Identify risks (e.g. compromised immunity or lack of patient education)
Planning
Develop a care plan with interventions like administering prophylactic antibiotics
prophylactic antibiotics: prevent infection
education pt on hygiene + preparation
Implementation
use HH + PPE
prepare surgical site aseptically
administer any antibiotics as needed
Evaluation
monitor patient’s understanding
reassess surgical site for signs for infection
Role of the nurse in relation to post-procedural infection prevention and control
Assessment
monitor VS, pain, signs of infection at surgical site
Problem identification
identify risks such as impaired skin integrity + inadequate wound care
Planning
create a care plan outlining infection prevention strategies + wound care instructions
Implementation
educate patient on proper wound care
ensure sterile techniques during dressing changes
Evaluation
regularly reassess surgical site for infection signs + evaluate effectiveness of patient education
Prepare + perform antibiotic infusion
Prepare:
vial
bevelled needle (for vial)
10ml syringe
WFI 10 ml
100 ml N/saline (blue side = spike, white side = drug)
line for pump
blue label
x2 swab (for vial + IV site)
Perform
prepare WFI + antibiotic in preparation room beforehand
not bedside
clean drug insertion on IV bag
draw drug → syringe → IV bag
put drug label on
follow iv process
Prepare + perform antibiotic push
Prepare
vial
bevelled needle (for vial)
x2 swab (for vial + IV site)
WFI
10 ml N/S ampoule
syringe x2 10 ml
~label sticker
Perform
prepare stuff in treatment room first
draw up WFi
clean vial + take out drug/water
check patency → flush/drawback
drawback THEN flush
10 mls ⇒ 2-3 mls/ minute
do slowly
too fast might ⇒ seizure, itchiness
pathophysiological responses associated with grief and loss
stress overload
increased cortisol => fatigue + illness (immune suppression)
fatigue + insomnia: grief disrupts sleep patterns => exhaustion / difficulty sleeping
appetite changes: grief => loss of appetite/ overeating
cardiac effects: chest pain/ tightness
psychological responses associated with grief and loss
shock + denial: e.g. initial numbness/ disbelief
anger + guilt
sadness + depression: affecting daily life and interests
acceptance and healing: gradual adjustment to the reality of loss => more manageable emotions over time
role of the nurse in relation to grief + loss (for a GRIEVING person)
assessment → to differentiate healthy grieving from at-risk
problem identification
planning → clarify expected outcomes when planning care for the grieving person
implementation → understand person, counselling, support, support groups
evaluation → follow their own time schedule
Explain and demonstrate the role of the nurse in relation to end-of-life care using the nursing process
assessment
pt’s awareness of terminal nature of illness
assess support systems + history of previous positive coping skills
physical/ emotional status
presence of advance directives for health care decisions
unfinished business expressed by patient or family
problem identification
powerlessness + hopelessness
risk of harm to self
planning
schedule time to be available to the patient
balance the person’s need for independence + their need for assistance
respect the person’s confidentiality
answer questions + provide factual information to pt + family
implementation
communicate a caring attitude
EOL care
learning needs of patient and family
physiological needs
promoting comfort
hospice/ home care
psychosocial/ spiritual needs
family support
questions to consider asking to maintain cultural sensitivity
'What should I know about you to help me take care of you the best I can?'
'What do you find the most distressing at present?'
'What is most important to you in relation to your care?'
'Who else (or what else) will be affected by what’s happening with your health?'
'Who would you like to be involved to help support you?'
'What do you think about the time ahead?'
offer to contact clergy
Describe self-care strategies to support yourself, and other nurses, when working with patients experiencing grief and loss.
lifestyle/ personal
embrace the outdoors
move your body
connect with loved ones
prioritise quality sleep
unleash your creativity
practice self-compassion
honour your pt in a way that aligns w your beliefs
external resources
support, education + assistance in coping w the death of patients
use peer support
trained professional
identify and cope w burnout