W6 Translational - Cell Death
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
which are the initiator caspases?
C2, 8, 9, 10
which are the executioner caspases?
C3, 6, 7
two key domains of initiator caspases (2, 8, 9, 10)
Adaptor-binding domain (N-terminal) – binds to adaptor proteins.
Protease domain (C-terminal) – has the active site, but needs activation.

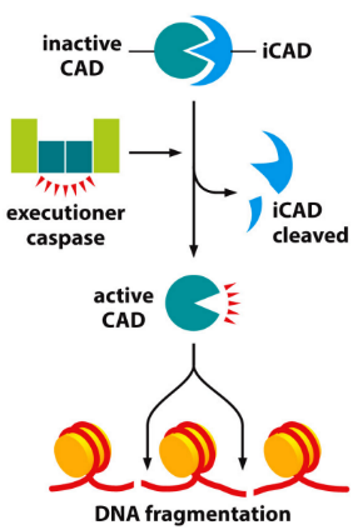
what causes DNA fragmentation in apoptosis?
Caspase 3 cleaves iCAD
CAD released and activated
active CAD cuts DNA between nucleosomes → produces fragments
Why is apoptosis hard to detect?
Specificity: Some features can overlap with necrosis → multiple assays are often needed for accurate detection.
Timing → apoptotic cells are cleared quickly → leads to false negatives if sampled too early or too late.
Sensitivity: Some assays require a high number of cells (e.g., DNA laddering).
common apoptosis features used for detection
DNA Fragmentation (gel electrophoresis/ DNA laddering)
Caspase Activity & Substrate Detection (Caspase-3 assay, WB, TUNEL assay)
Membrane Alterations (Annexin V binding assay)
Mitochondrial Assay (cytochrome C release)
How can gel electrophoresis be used to measure apoptosis?
DNA fragmentation = hallmark feature of apoptosis
Caspase-3 cleaves iCAD → activates CAD → cuts DNA between nucleosomes → DNA fragmentation
In gel electrophoresis → bands indicate DNA
as time goes by, increased DNA fragmentation is visualised as increased bands

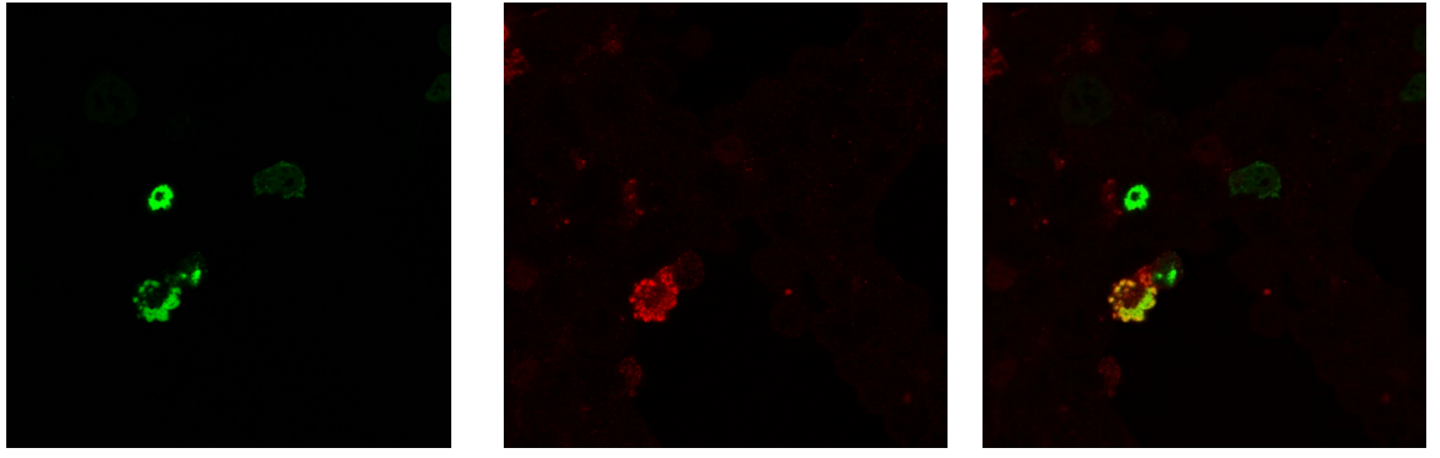
How does TUNEL assay measure apoptosis?
EARLY STAGE DETECTION
assay endonuclease cleavage products
TdT enzyme labels DNA strand breaks with fluorescent dUTP
Detected by light microscopy or flow cytometry.
Highly sensitive but may give false positives (e.g. from necrosis or active gene transcription).
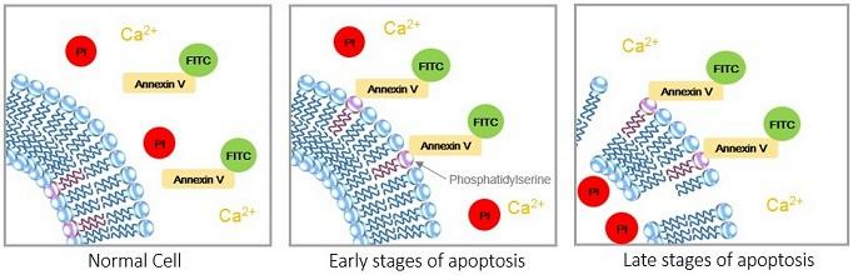
How does Annexin V measure apoptosis?
EARLY STAGE DETECTION
Annexin V = high affinity for phosphatidylserine, which flips to the outer membrane early in apoptosis.
Annexin V = tagged with fluorescent probe
detected via flow cytometry or fluorescence microscopy.
where and what are the anti-apoptotic Bcl2 proteins? and what do they do?
location: Mitochondrial outer membrane
what: Bcl2, BclXL
How: inhibit apoptosis by by inhibiting pro-apoptotic proteins → blocking Cytochrome C release
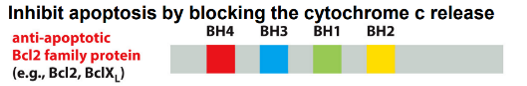
what are the pro-apoptotic Bcl2 proteins? and what do they do?
What: Bax, Bak
Where: Bax = cytosol → mitochondria on signal; Bak = always at mitochondria
How: promote apoptosis by forming transition pore to enhance Cytochrome C release
where and what are the pro-apoptotic BH3-only proteins? and what do they do?
What: Bad, Bim, Puma, Noxa
Where: Cytosol → activated on signal
How: inhibiting anti-apoptotic Bcl2s and/or activating Bax/Bak → promotes apoptosis by enhancing Cytochrome C release

what is the role of IAPs?
Function: Block apoptosis unless it's truly necessary by regulating caspase activation → set an inhibitory threshold that caspases must overcome to trigger apoptosis
Mechanism:
Contain BIR domains → bind to active caspases and inhibit them.
Some also polyubiquitylate caspases, marking them for degradation by proteasomes
Why is apoptosis important?
Balancing Act: crucial for maintaining a healthy balance between cell proliferation (growth) and cell death → This ensures that cells survive only where and when they are needed (prevents cancer growth)
Development: During development, apoptosis plays a vital role in sculpting tissues and organs. E.g. elimination of excess nerve cells → This ensures that all target cells are properly innervated, and redundant cells are removed.
Quality Control: Apoptosis removes damaged, infected, or potentially harmful cells (e.g., precancerous cells).
what are the ‘eat me’ signals in apoptosis
Phosphatidylserine → Normally on the inner leaflet of the plasma membrane. During apoptosis, it "flips" to the outer leaflet
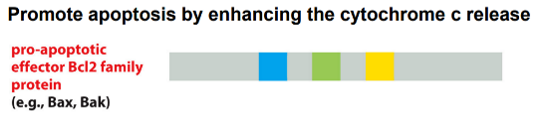
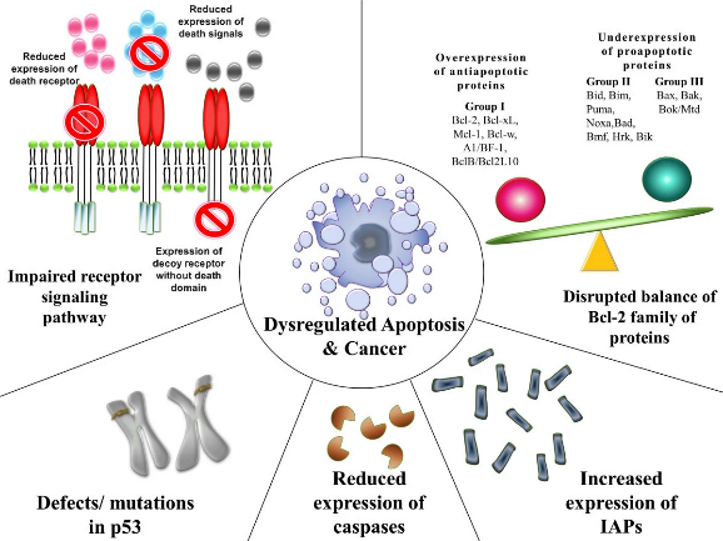
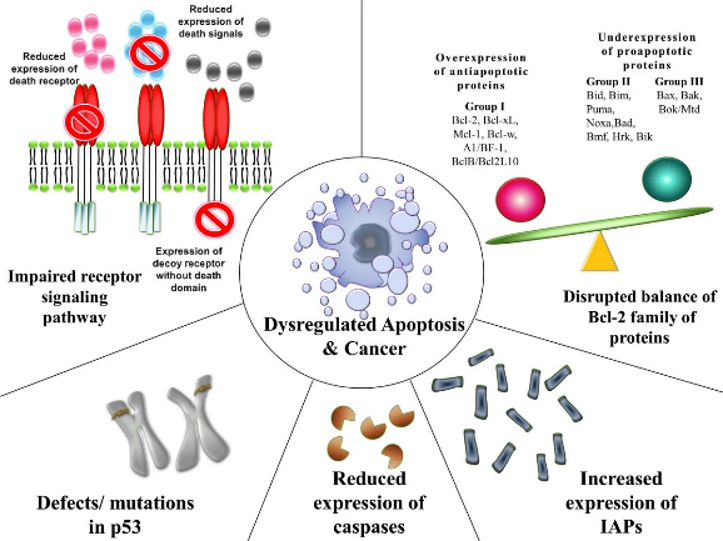
Pathological Apoptosis - too little — EFFECT
If cells that should die (e.g., damaged cells, precancerous cells) don't undergo apoptosis, they can survive, proliferate uncontrollably, and lead to tumor formation.
diseases: cancer, autoimmune
Pathological Apoptosis - too little — CAUSE
Disrupted balance of pro- and anti-apoptotic proteins: E.g., overexpression of anti-apoptotic proteins (like Bcl2) or underexpression of pro-apoptotic proteins.
Mutations in p53: Mutations in p53 (found in ~50% of cancers) can impair the suppression of tumours, allowing damaged cells to survive.
Increased expression of IAPs: IAPs inhibit caspases, thus blocking apoptosis.
Pathological Apoptosis - too much — EFFECT
Neurodegenerative Diseases: Excessive apoptosis of neurons contributes to the progressive loss of brain cells in diseases like Alzheimer's, Parkinson's, and Motor Neuron Disease (MND).
Ischemic Injury (e.g., Stroke, Heart Attack): While necrosis is primary in the core of an ischemic event, apoptosis can occur in the surrounding "penumbra" region, contributing to tissue damage.
Pathological Apoptosis - too much — CAUSE
Disrupted balance of pro- and anti-apoptotic proteins: E.g., under-expression of anti-apoptotic proteins (like Bcl2) or over-expression of pro-apoptotic proteins.
Mutations in p53: Mutations in p53 can increase the suppression of tumours, allowing damaged cells to survive.
decrease expression of IAPs: IAPs inhibit caspases, thus decreases apoptosis.
Why and How do we target Apoptosis in Cancer Treatment?
Why: Since decreased apoptosis contributes to many cancers, drugs that restore or stimulate the apoptotic pathway can be effective cancer treatments.
How: Block anti-apoptotic Bcl2 family proteins (e.g., Bcl2, BclXL). This would unleash the intrinsic apoptotic pathway, leading to increased cancer cell death.
Example: ABT-737
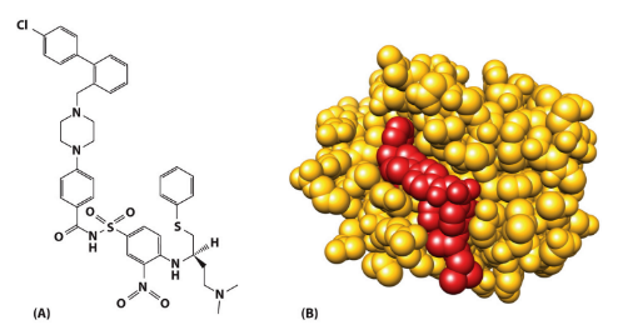
What is the role of ABT-737 in cancer treatment?
ABT-737 = chemical designed to mimic pro-apoptotic BH3-only proteins
binds to the hydrophobic groove of anti-apoptotic Bcl2 proteins (like BclXL).
neutralises its anti-apoptotic function
promotes apoptosis in cancer cells that depend on BclXL for survival.
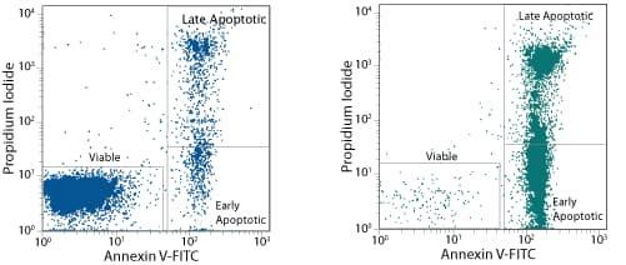
How does Flow Cytometry measure apoptosis?
cells suspended in fluid/ solution → laser passed through cells → scattered light and fluorescence are detected → indicates cell parameters
Helps distinguish between early and late apoptosis, and necrotic cells.
Healthy cells: Annexin V negative, PI negative.
Early apoptotic cells: Annexin V positive, PI negative (PS externalized, but membrane intact).
Late apoptotic/Necrotic cells: Annexin V positive, PI positive (PS externalized, and membrane compromised).
importance of apoptosis in CNS
critical for proper development of the brain and spinal cord, regulating cell numbers and forming efficient neuronal networks.
Mice lacking Apaf1 have enlarged brains due to impaired neuronal apoptosis during development, leading to lethality.
Deleting the pro-apoptotic gene Bax in mice largely eliminates neuronal cell death in the CNS during development.
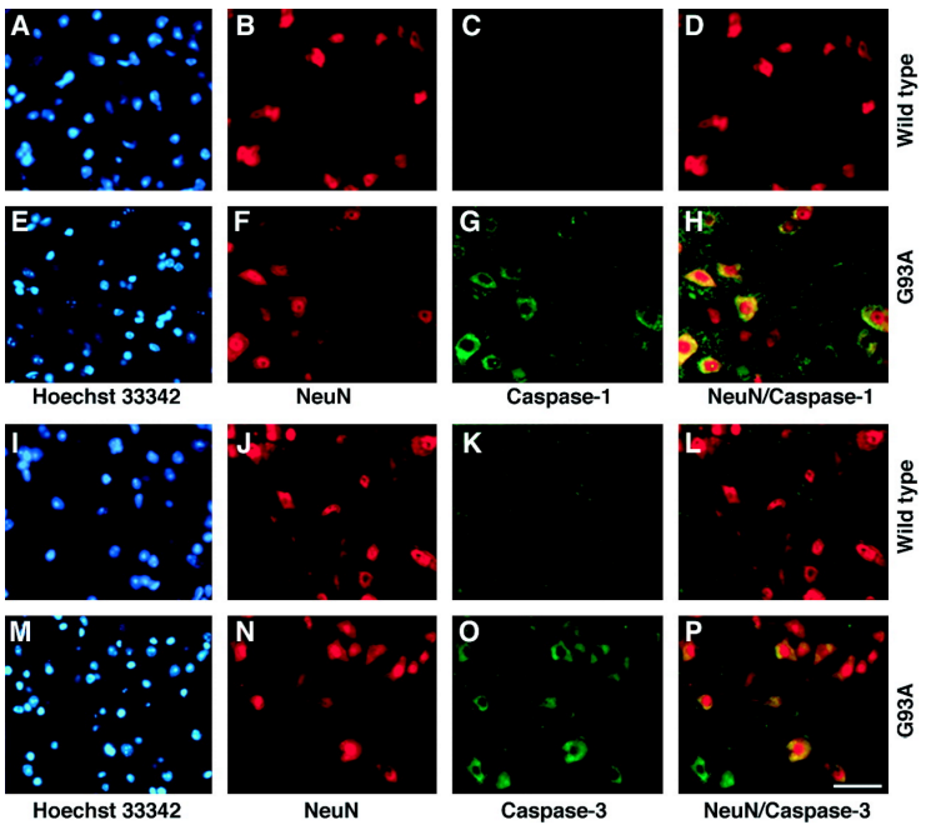
Apoptosis in ALS - SOD1 (mutant mice) & Caspase activity (human)
MND mouse models = SOD1 mutation linked to motor neuron death
increased levels of caspase-1 (initiator) & caspase-3 (executioner) found in spinal MN of human ALS patients