Distal Tract Pathologies
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Functions of the appendix
immunoprotective and lymphatic functions
maturation of B lymphocytes and the production of IgA
storage for useful bacteria present in the colon
What causes appendicitis and how?
fecoliths or obstructions like hypertrophy of lymphatic tissue
Obstruction prevents drainage of mucus. → mucus fills lumen → limited expansion→ increased intraluminal pressure
Amplified by appendiceal microbiota (toxins).
Distension stimulates visceral afferent fibers → diffuse dull pain
signs and symptoms of appendicitis
Acute abdominal pain starting in the mid-abdomen and later localising to the right lower quadrant.
Fever (low-grade), anorexia, nausea, vomiting, and elevation of the neutrophil count.
Diarrhoea / constipation
Reduced bowel sounds = sign of perforated appendix
What can appendicitis lead to and what are the symptoms?
Peritonitis/sepsis
Signs of infection increase
diffuse pain
Rigidity/guarding
How do you diagnose appendicitis?
Physical exam
Rebound tenderness - (when you let go it hurts worse than when you press down)
Psoas sign (passive extension of the right hip causes pain) / Obturator sign (passive internal rotation of the flexed right hip causes pain)
Rovsings sign (press on LLQ and they feel rebound pain in the RLQ when pressure is released)
Bloods – WBC/CRP
CT/ ultrasound
What landmark do you need to find to check for appendicitis?
Mcburneys point
one-third of the way from the right anterior superior iliac spine to the navel (umbillicus)
What are Diverticula?
Diverticula - sac-like protrusions/ pouches of mucosa through the muscular wall of the colon
Occurs where vasa recta penetrate the bowel wall
Diverticulosis vs diverticulitis
Diverticulosis - presence of diverticula
Diverticulitis - inflammation of a diverticulum
Risk factor of diverticular disease
Increased risk with age
Increased risk in men <50yrs, and women >50yrs
Dietary risk factors: low dietary fibre, high salt, meat, and sugar intake
Obesity (BMI >30)
Smoking.
Medications – Corticosteroids/NSAIDs
Immunosuppression
What is complicated diverticulitis?
diverticulitis with abscess, perforation, stricture, obstruction, and/or fistula
Causes of diverticular formation
unknown
thought to occur due to abnormal colonic motility ↑ intraluminal pressure
Symptoms of diverticular disease
Intermittent pain
Change in bowel habit
Painless bleeding
Symptoms of acute diverticulitis
Acute abdominal pain
Localised abdominal tenderness (site of inflammation)
Signs of infection (fever, ↑ WBC)
complications of diverticular disease
Bleeding can lead to substantial blood loss
Stricture/Bowel obstruction
→ Signs: colicky abdominal pain, absolute constipation (passage of no flatus or stool), vomiting or abdominal distention
Perforation and peritonitis/sepsis
fistulae
Abscess
→ Signs: abdominal mass on examination / peri-rectal fullness on D
Diagnosis of diverticular disease
Abdominal examination:
– Tenderness on palpation
– Abdominal mass
– Guarding
Pelvic examination – women
Full blood count, CRP, faecal occult blood test, urinalysis
Imaging/endoscopy – confirm and exclude
Treatment if diverticular disease
Depends on severity
diet change, liquid diet, antibiotics, surgery
What is the function of the rectum and at what vertebral level does it start?
Function: temporary storage of faeces and control of faecal excretion
the Rectal ampulla relaxes to accumulate and temporarily store faeces
begins at level of S3
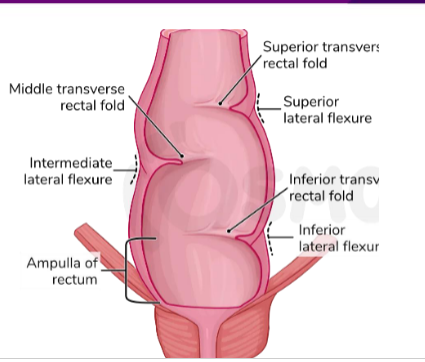
Name the flexures in the rectum
anteroposterior flexures:
Sacral flexure: follows the natural concavity of the sacrum
Anorectal flexure: puborectalis muscle pulling rectum anteriorly (important for faecal continence)
lateral:
superior
intermediate
inferior

When does the rectum become the anal canal?
As rectum passes through hiatus in levator ani it transitions to anal canal
Where are the valves in the rectum?
Superior rectal valve - upper convexity on the left side of the rectum
Middle rectal valve - intermediate convexity on the right side
Inferior rectal valve - lower convexity on the left side of the intestine
** help reduce direct pressure on anal canal
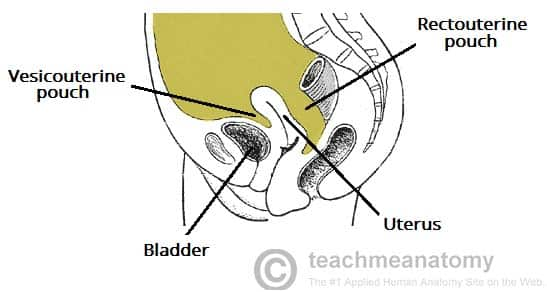
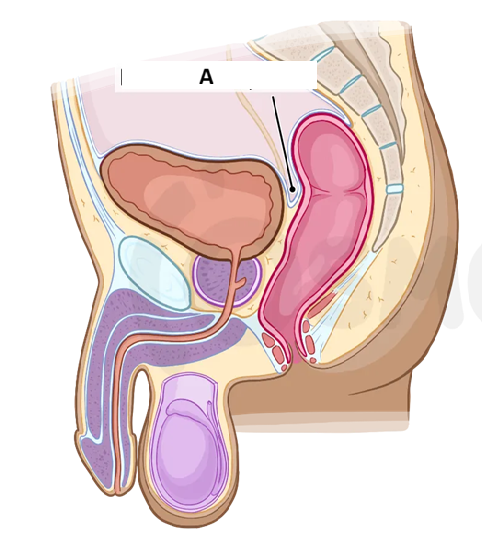
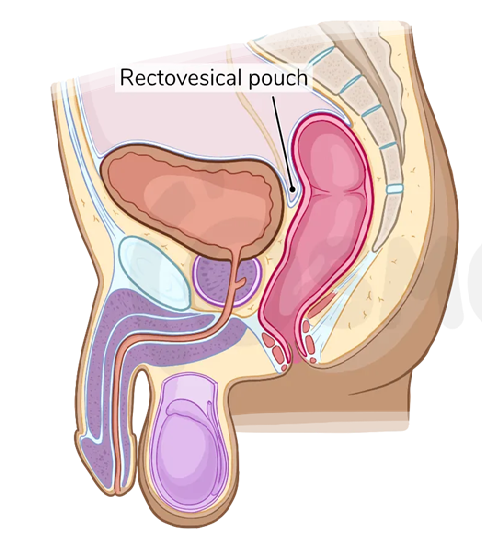
What part of the rectum in retro/intra peritoneal
proximal 1/3 intraperitoneal (but only covers anterior and lateral surface)
Middle 1/3 predominantly retroperitoneal (only anterior surface covered).
distal 1/3 sub-peritoneal (below pelvic diaphragm)
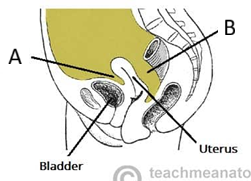
rectouterine pouch = pouch of Douglas
What is the anal sphincter complex made up of?
Internal anal sphincter (IAS) → tonically contracted at rest (autonomic control)
Conjoint longitudinal muscle layer
External anal sphincter (EAS) → tonically contracted at rest (conscious control)
Where are faeces held in the anal canal
held around pectinate line by EAS (and small contribution from IAS)
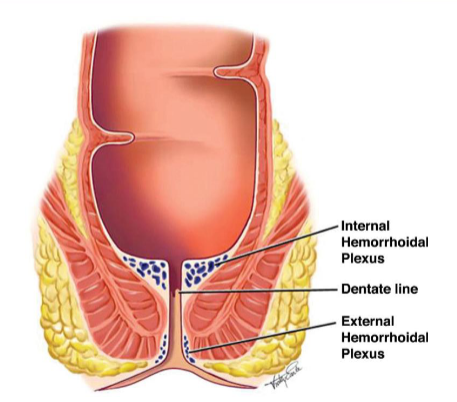
Where is the pectinate/ dentate line and how is the anal canal different below and above it?
Junction of hindgut and proctodaeum (ectoderm)
Above the pectinate line
• ANS innervation
• Columnar epithelium
Below the pectinate line
• Somatic innervation
• Stratified squamous epithelia
Function of Anal cushions/Hemorrhoidal plexus
maintaining fecal continence by engorging with blood and closing the anal canal and by protecting the anal sphincter during defecation
Blood supply to the rectum
Superior rectal artery – terminal continuation of the inferior mesenteric artery.
Middle rectal artery – branch of the internal iliac artery.
Inferior rectal artery – branch of the internal pudendal artery
Venous drainage of the rectum
superior rectal vein → empties into the portal venous system
middle and inferior rectal veins → empty into the systemic venous system The superior rectal vein empties into the portal venous system,
Anastomoses between the portal and systemic veins are located in the wall of anal canal, making this a site of portocaval anastomosis
Nerve supply to the rectum
Sympathetic nerves: lumbar splanchnic nerves, superior and inferior hypogastric plexuses
Parasympathetic nerves: from S2-4 via the pelvic splanchnic nerves and inferior hypogastric plexuses
External anal sphincter: Somatic innervation –inferior rectal nerve (branch of pudendal nerve)
Lymphatic drainage of the rectum
Proximal 2/3: pararectal lymph nodes → drain into the inferior mesenteric nodes.
Distal 1/3: drains directly into the internal iliac lymph nodes
Process of defecation
stimulus: distension in rectum
response:
contraction in rectum and sigmoid colon
relaxation of internal anal sphincter
contraction of external anal sphincter
then:
relaxation of external anal sphincter
relaxation of puborectalis muscle
peristalsis + Valsalva manoeuvre (increased abdominal pressure)
What is diarrhoea?
↑ in stool frequency, liquidity, or volume.
WHO - three or more loose or liquid stools per day (or more frequent passage than is normal for the individual)
Properties of osmotic diarrhoea
Excess osmotically active particles in the gut lumen.
Variable volume, watery or loose consistency.
Osmotic gap >100mOsm/kg
Stops when the patient is fasted
underlying cause of osmotic diarrhoea
Osmotic laxatives (lactulose)
Excessive solutes within the lumen (e.g. lactose intolerance)
Inflammation within the mucosa (e.g. IBD, coeliac disease).
Motility disorders (e.g. IBS)
properties of secretory diarrhoea
Bowel mucosa secretes excess ions (chloride) into the lumen – water follows
Large volume, watery stool
Osmotic gap <100mOsm/kg
Continues when the patient is fasted
Underlying causes of secretory diarrhoea
Infections (cholera, E.coli, rotavirus)
Specific electrolyte transport defects (e.g. congenital chloride-losing diarrhoea
Management of diarrhoea
Determine the onset, duration, frequency, and severity of symptoms.
Enquire about the presence of red flag symptoms (e.g. blood in stool, weight loss)
fix dehydration
What is constipation?
unsatisfactory defecation characterized by infrequent stools, difficult stool passage or both
Risk factors of constipation
More common in elderly
More common in women (very common in pregnancy)
relatively common in children <5y
Dehydration/low fibre intake ↑ risk
Physical activity ↓ risk of constipation
Causes of constipation

Management of constipation
Lifestyle advice:
healthy, balanced diet (increased sorbitol, fruit and veg intake)
Ensure adequate fluid intake
Ascertain/Exclude other causes
Laxatives if above fails – bulk forming first, followed by osmotic, gradually reduce once symptoms subside
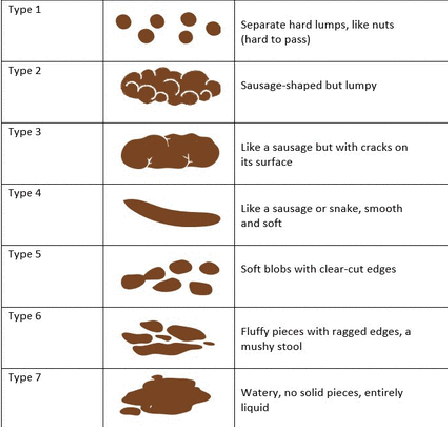
Bristol stool chart
What is a common cause or rectal bleeding and why?
Haemorrhoids
Caused by loss of connective tissue support
** pregnancy only risk factor
internal vs external haemorrhoids
internal haemorrhoids (most common):
Above dentate line (relatively painless)
Enlarge and prolapse through anal canal (Graded by degree of prolapse (i-iv))
Haematochezia (bright red blood)/pruritis ani
Can lead to “leakage”
External haemorrhoids
Below dentate line (very painful)
Less likely to bleed
More likely to thrombose.
What is an anal fissure and why does it happen?
Tear or ulcer in the lining of the anal canal which causes pain on defecation
Linked to local trauma (e.g. passing of hard stool).
Underlying causation
– High internal anal sphincter tone
– Reduced blood flow to anal mucosa
Causes of Haematochezia
Diverticular disease
Haemorrhoids
Anal fissure
IBD
Colorectal cancer
What is Melaena and what is it a sign of?
Passage of black, tarry stools (haemoglobin digested into haematin)
associated with upper GI bleed, Peptic ulcer disease, Variceal bleeds (oesophagus),Upper GI malignancy (e.g. Oesophageal/gastric cancer)