Exam 1 Patho Review
1/160
Earn XP
Description and Tags
everything
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
161 Terms
Varicose Veins
Enlarged, twisted veins often found in the legs. They occur when the valves inside the veins malfunction, cuasing blood to flow backward and pool
Thrombus formation
Can happen with varicose veins due to stagnant blood flow, leading to potential complications such as deep vein thrombosis and increases the risk of a pulmonary embolism
Thrombus
Blood clot that forms within a blood vessel and remains attached to the site of formation or can dislodge and travel to other parts of the body turning into an embolus
Deep vein thrombosis
A condition where a blood clot forms in a deep vein, usually in the legs, potentially leading to serious complications if the clot dislodges
Hypertension
Occurs when the force of blood against the artery walls is consistently too high —> over time can damage arteries and lead to complications
Orthostatic hypotension
Form of low blood pressure that can happen when you stand up to quickly from sitting or lying down - can cause dizziness. lightheadedness, or fainting ass the body struggles to adjust to the sudden change in position
Aneursym
a bulge or ballooning in a blood vessel caused by a weakness in the vessel wall
Types of aneurysms
include healthy. vesel, saccular, fussiform, dissection, and false, each differing in shape and location
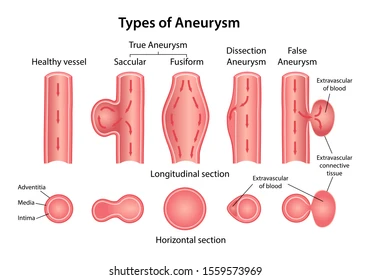
True aneurysm
Involve all 3 layers of the arterial wall and are best described as a weakening of the vessel wall that have a wide base, walls composed of myocardium, and are low risk for rupture; they are the saccular and fusiform aneurysms
What is another name for a berry aneurysm
Cerebral aneurysm
Cardiac aneurysm
Most common form after MI when intraventricular tension stretches the non-contracting infarcted muscle
Why is the aorta particularly susceptible to aneurysm formation
Due to its high pressure and stress, combined with age-related degeneration of the vessel wall and the absence of penetrating vsa vasorum in the media layer
Most common cause of arterial aneurysm
Atherosclerosis, which leads to vessel wall weakening and dilation and plague formation erodes the vessel well and contributes to inflammation
Proteinases (proteases)
Enzymes that break down proteins into smaller peptides or amino acids, process called proteolysis
Atherosclerosis
Buildup of fatty deposits (plaque) on the inner walls of arteries, which can restrict blood flow - condition is a major cause of heart disease
Peripheral artery disease (PAD)
Narrowing or blockage of the arteries outside of the heart and brain, typically in the legs causing reduced blood flow and potential complications like pain, ulcers, or gangrene.
Coronary artery disease
narrowing or blockage of the coronary arteries, which supply blood to the heart muscle - usually caused by atherosclerosis and can lead to chest pain, MI, and heart failure
Most common cause of heart disease
Coronary artery disease
Superficial main coronary arteries
include the left main coronary artery and right coronary artery, which supply blood to the heart muscle
Left coronary artery
Anterior descending artery, circumflex
Right coronary artery
Posterior descending artery, marginal artery
Anastomoses
Communication between blood vessels
Preload
Primary factor affecting stroke volume, pressure in the ventricles at the end of diastole and is influenced by the volume of blood returning to the heart
Frank - Starlings Law of the Heart
The principle that the stroke volume of the heart increases in response to an increase in the volume of blood filling the heart, due to the myocardial stretch
Afterload
Resistance against which the ventricle must overcome, highly influenced by peripheral vascular resistance
Tunica Intima
Single cell layer, innermost and narrowest layer of the artery
Tunica Media
Elastic fibers and muscle layer responsible for regulating blood vessel diameter and maintaining blood pressure
Tunica adventitia
Fibrous tissue covering the outermost layer of blood vessels, providing structural support and protection
Peripheral circulation
Arteries → arterioles → capillaries → venules, veins
SNS
fight or flight, epinephrine/norepinephrine, alpha-adrenergic receptors, beta-1 adrenergic receptors
Alpha-adrenergic receptors
Receptors that respond to epinephrine and norepinephrine, primarily causing vasoconstriction and increased blood pressure.
Beta 1 adrenergic receptors
Heart: increase HR and contractility
Beta 2 adrenergic receptors
Lungs: bronchodilation
Chemical neurotrnasmitter
Acetylcholine
Cholinergic receptors
Receptors that respond to acetylcholine, involved in parasympathetic nervous system functions
SLUDGE Pneumonic for cholinergic response
Symptoms include Salivation, Lacrimation, Urination, Defecation, Gastrointestinal issues, and Emesis
Anticholinergic response
Mad as a hatter, blind as a bat, red as a beet, dry as a bone
Examples of tachydysrythmias
uncontrolled afib, atrial flutter, paroxysmal supra-ventricular tachycardia, vtach
Bradydysrythmias
sinus bradycardia, av blocks, junctional rhythms, idioventricular rhythms
Risk factors of varicose veins
age, female, family hx, obesity, pregnancy, DVT, prior leg injury
Varicose vein cause
blood pooling in the vein due to valve damage and the effects of gravity, leading to gradual venous distention over time
when does valve damage occur for varicose veins
when prolonged increased pressure renders the valve of the vein, unable to maintain normal pressure, the vein swells from the extra pressure and the surrounding tissue becomes oedematous due to increased hydrostatic pressure
Chronic venous insufficiency (CVI)
inadequate venous return over a long period of time, inflammatory rx in the vessels are caused by venous hypertension, circulatory stasis, and tissue hypoxia
Symptoms of chronic venous insufficiency
edema of the lower extremities, hyperpigmentation of the feet and ankles
Venous stasis ulceration
circulation to the extremities can become sluggish, which reduces the supply of oxygen and nutrients to the cells and impedes waste removal from the cells
Venous stasis ulcers
are skin sores that occur due to poor circulation and prolonged venous hypertension, often resulting from chronic venous insufficiency and can lead to significant pain and complications if left untreated
Tx of varicose veins/CVI
noninvasive treatments such as elevating the legs, wearing compression stockings, and performing physical exercise; invasive management includes ablation and sclerotherapy, surgical ligation, conservative vein resection, and vein stripping
Thrombus
Blood clot that remains attached to a vessel wall
detached thrombus name
Thromboembolism
are venous or arterial thrombi more common
venous thrombi as flow and pressure are lower in the veins than the arteries
Where is DVT occur primarily
lower extremities, and is more likely to cause a pulmonary embolism
Where are DVTs involves 90% of the time
femoral and popliteal veins as it is the more dependent part of the body and prone to stasis
3 factors that promote DVT
venous stasis, venous endothelial damage, hypercoagulative states (inherited disorders, malignancy, pregnancy, use of oral contraceptives or hormone replacement therapy)
High likelihood of DVT resulting from
orthopedic sx, spinal cord injury, obstetric/gynaecological procedure
Antiplatelet
medications that prevent blood clot formation by inhibiting platelet aggregation (ex. ASA)
What does hypertension result from
Sustained increase in peripheral resistance (arteriolar vasoconstriction)or increased cardiac output, leading to elevated blood pressure
Pre Hypertension
Systolic 120-139 mmHg and Diastolic 80-89 mmHg
Hypertension Stage 1
Systolic 140-159 mmHg and Diastolic 90-99 mmHg
Hypertension Stage 2
Systolic 160 mmHg or higher and Diastolic 140 mmHg or higher
Malignant hypertension
A severe form of hypertension characterized by extremely high blood pressure, often exceeding 180/140 mmHg, and can lead to organ damage.
Endothelial dysfunction
A condition where the endothelium (inner lining of blood vessels) loses its normal function, contributing to various cardiovascular diseases
shift in pressure - natriuresis relationship
A physiological response where changes in blood pressure affect the kidneys' ability to excrete sodium, impacting fluid balance and blood volume
What organs do the hormones specifically come from the RAAS system come from?
The hormones from the Renin-Angiotensin-Aldosterone System (RAAS) primarily come from the kidneys, liver, and adrenal glands. Renin is produced by the kidneys, angiotensinogen is produced by the liver, and aldosterone is secreted by the adrenal glands
What does high hydrostatic pressure in the capillaries cause?
High hydrostatic pressures in the capillaries cause vascular fluid to push into the interstitial space
Encephalopathy
a broad term for brain dysfunction, which can result from various causes, including metabolic disturbances, infections, or toxins
Papilledema
swelling of the optic nerve head due to increased intracranial pressureIt can lead to vision problems and is often a sign of serious underlying conditions
Orthostatic Hypotension
refers to a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within 3 min of moving to a standing position
what is the mediated reflex arteriolar
response to changes in blood pressure that helps maintain cerebral perfusion during postural changes
What happens when we go from a sitting to standing position
The baroreceptor - mediated reflex arteriolar and venous constriction and increased HR compensate for the gravitational changes
What is the equation for the carbonic acid-bicarbonate buffer system
CO2+H2O = H2CO3 = HCO3- + H+
Marfan’s syndrome
A genetic disorder affecting connective tissue causing structural abnormalities and problems with tissue homeostasis
Syphillis
A sexually transmitted infection caused by the bacterium Treponema pallidum, which can lead to serious health complications if left untreated
Aortic dissection
Tearing of intimal layer of the aorta likely to occur in areas which are under the greatest stress
ascending aorta distal to the aortic valve
descending aorta just beyond to L subclavian artery
What may aortic dissection cause
aortic valve insufficiency if dissection progresses toward aortic valve
Aortic root aneurysm
a bulge in the wall of the aorta where it leaves the heart
Thoracic Aortic Aneurysm
true aneurysm of the portion of the aorta, which is the thoracic space, beyond the main aortic branches
What most commonly causes thoracic aortic aneurysms
Atherosclerosisis the most common cause, often leading to weakening of the aortic wall, and turbulent blood flow
Symptoms of a thoracic aortic aneurysm
Chest, neck and/or back pain, in cases of rupture, “tearing” pain is severe, cough and/or dyspnea (if pressure on trachea), difficulty swallowing (if pressure on the esophagus)
Arterial Thrombus: 2 potential threats to circulation
The thrombus may grow large enough to occlude the artery, causing ischemia in tissues supplied by the artery, the thrombus may dislodge, become a thromboembolism that travels through the vascular system until it occludes flow into a distal vascular bed
Pharacological treatment for an arterial thrombus
Heparin, warfarin derivates, thrombin inhibitors, or thrombolytics are commonly used to prevent clot formation or dissolve existing clots
Emboli (mobile)
Matter circulating in the blood stream that can lead to an obstruction of a vessel, can consist of: dislodged thrombus, air bubble, aggregate of amniotic fluid, fat, bacteria, cancer cells, foreign cells, foreign substance and object
Where does an embolus travel to
Travels in the bloodstream until it reaches a vessel it cannot pass through
Pulmonary emboli
originates on the venous side (mostly from deep veins of the legs) and the system circular or in the right heart
Arterial emboli
Most commonly originate in left side of the heart and are associated with thrombus after MI, valvular disease, left ventricular failure, endocarditis, and dysrhythmias
Embolism
Causes ischemia or infarction is tissues distal to the obstruction, producing organ dysfunction and pain
Infarction
Tissue death due to insufficient blood supply, often resulting from occlusion of blood vessels
Occlusion of a coronary artery causes what?
MI
Occlusion of a cerebral artery causes what?
Stroke or TIA
Leading cause of CAD and cerebrovascular disease
Arteriosclerosis
Prostaglandins in arterial blood
Arterial blood flow becomes more turbulent, and platelets release prostaglandins which draw more platelets to the area and worsen inflammation —> further obstruction and potential thrombus formation
What starts to happen with a total obstruction from a fully occluded artery
Begins with injury to the endothelial cells that line artery walls, leading to increased permeability and platelet aggregation, which can promote thrombus formation
How do plaque form and rupture?
macrophages release growth factors that stimulate smooth muscle cell proliferation
smooth muscle cells in the region of endothelial injury proliferate, produce collage, and migrate over the fatty streak, forming a fibrous plaque
the fibrous plaque may calcify, protrude into the vessel lumen, and obstruct blood flow to distal tissues (especially during exercise), which may cause symptoms
Ex. Angina and myocardial infarction.
Clinical manifestations of atherosclerosis
Presents with S&S of inadequate perfusion of tissues because of obstruction of the vessels supplying the tissues such as chest pain, fatigue, and shortness of breath, which can lead to critical conditions like heart attack or stroke.
Interventions for acute ischemia, MI, or stroke
Cardiac catheterization, tissue plasminogen activator (tPA) or through mechanical removal of thrombi
Major cause of myocardial ischemia
Atherosclerosis leading to CAD
Peripheral artery disease
a circulatory atherosclerosis disease characterized by narrowed arteries reducing blood flow to the limbs and often leads to leg pain, cramping, can cause gradual or acute lower extremity ischemia
How should symptomatic PAD be managed?
Vasodilators in combination with antiplatelet and antithrombotic medication and cholesterol-lowering medications
How do CAD and hyperlipidemia affect heart health
Can have suboptimal cardiovascular health stratus secondary to multiple cardiovascular risk factors; increased rates of obesity and diabetes, uncontrolled hypertension, dyslipidemia
Dyslipidemia
unhealthy level for one or more fats in the patients blood
Difference between stable and unstable angina
Stable angina is characterized by predictable chest pain that occurs with exertion and is relieved by rest, while unstable angina presents as unpredictable chest pain that may occur at rest or with minimal exertion and indicates a higher risk of heart attack