Lecture: 1 Models of Health Behaviour
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What is WHO's definition of health?
A state of physical, mental and social well-being, not merely the absence of disease and infirmity.
What is health composed of?
Being - a state of wellbeing (absence of dis-ease)
Having - an absence of symptoms
Doing - capabilities/behaviours that people are able to do.
What is health?
defined as a continuum as well, not binary. Death on one end and optimal wellness on the other. Ultimately, health may be more complicated than it seems.
What is the biomedical approach?
every symptom has a direct physical cause, of which if physical causes can be treated, the symptom can be removed. Freud would come to recognise that there were maybe -intangible- causes to physical causes.
How has behaviours contributed to causes of death?
moved from physical processes causing symptoms, but also understanding that behaviours (not just psychological causes) may also be contributing to the death more and more.
What are the leading causes of death (in descending order) ?
Heart disease, cancer, stroke, accidental injuries, chronic lung disease, diabetes and aids. → note that all of these have behaviours that may increase risk factors
What is the biopsychosocial model?
Includes biological, sociological and psychological models. Biology factors include - genetics, physiological systems and physical functioning. Sociological factors include - family, community and culture. And psychological factors include - cognition, emotion and motivation. All three overlap to contribute to health.
Why are models of health behaviour important ?
Models allow for a pathway as to how to change behaviours → behaviours that are positive vs. negative (do more of vs. do less of ). ‘
What is the Locus of Control?
Belief about what causes particular outcomes - you have internal and external locus of controls,
Internal - personal control
External - focuses outside of you.
Explain the locus of control in the context of exercise?
Higher their internal locus of control the more likely they are to do regular exercise.
Apply to clinical psych - wherein we should be empowering people to do things and increase their personal locus of control
What is the self-efficacy theory?
perceived capability/confidence around performing behaviour given your abilities and the unique situation. The environment is an important factor. E.g running in good conditions vs. running in the snow.
How would you measure self-efficacy?
You could measure your confidence in the face of the various obstacles. Confidence is not static, it will vary depending on the environment. Additionally, this confidence can be complicated more as people may be more or less confident in different elements.
What are the elements that contribute to self-efficacy (according to theory)?
Past performance - e.g previous grades in a course
Vicarious experience - e.g what we see other people go through around us
Social persuasion - e.g what other people around you are saying
Physiological/affective states - e.g these are feelings/emotion currently happening as you do the behaviour - direct physical behaviours representing improvement.
What is the theory of reasoned action?
states that in order to carry out an action needs behavioural intention, of which needs an attitude towards behaviour and subjective norms that support these intentions.
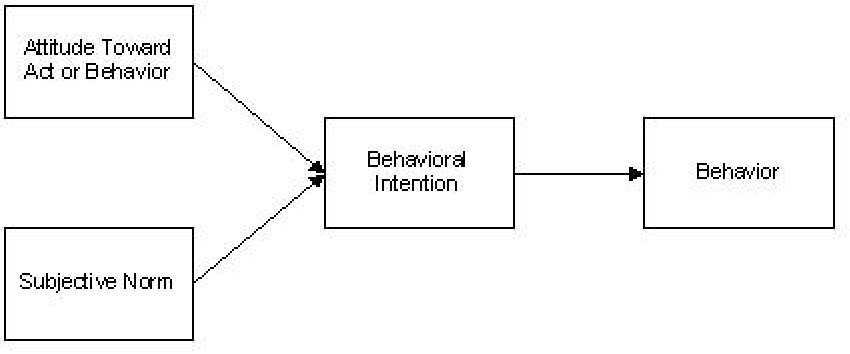
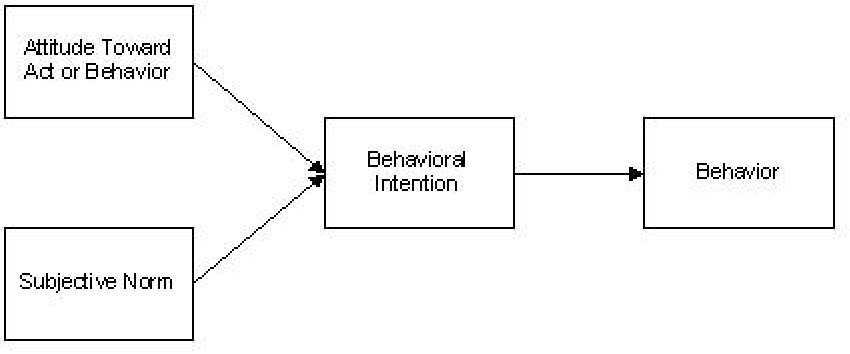
What is the difference between planned behaviour theory and theory of reasoned action?
Later added to the reasoned action theory to include perceived behavioural control (self-efficacy)→ the amount that you believe that you can exert power over intention, the behaviour and the relationship between the two. → this is the theory of planned behaviour
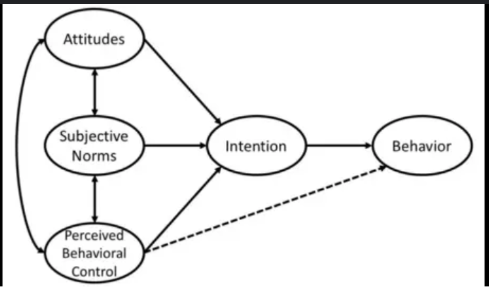
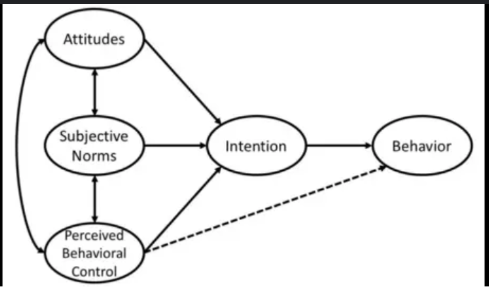
What is the biggest contributor to changes to smoking behaviour?
Attitude towards behaviour - biggest contributor
Behavioural intention’s impacting actual behaviour → 2nd bigger contributor.
What is the health beliefs model?
Originally intended to model the influence of risk factors.
Includes the impact of perceived susceptibility and perceived seriousness on the perceived threat which contributes to the likelihood of action.
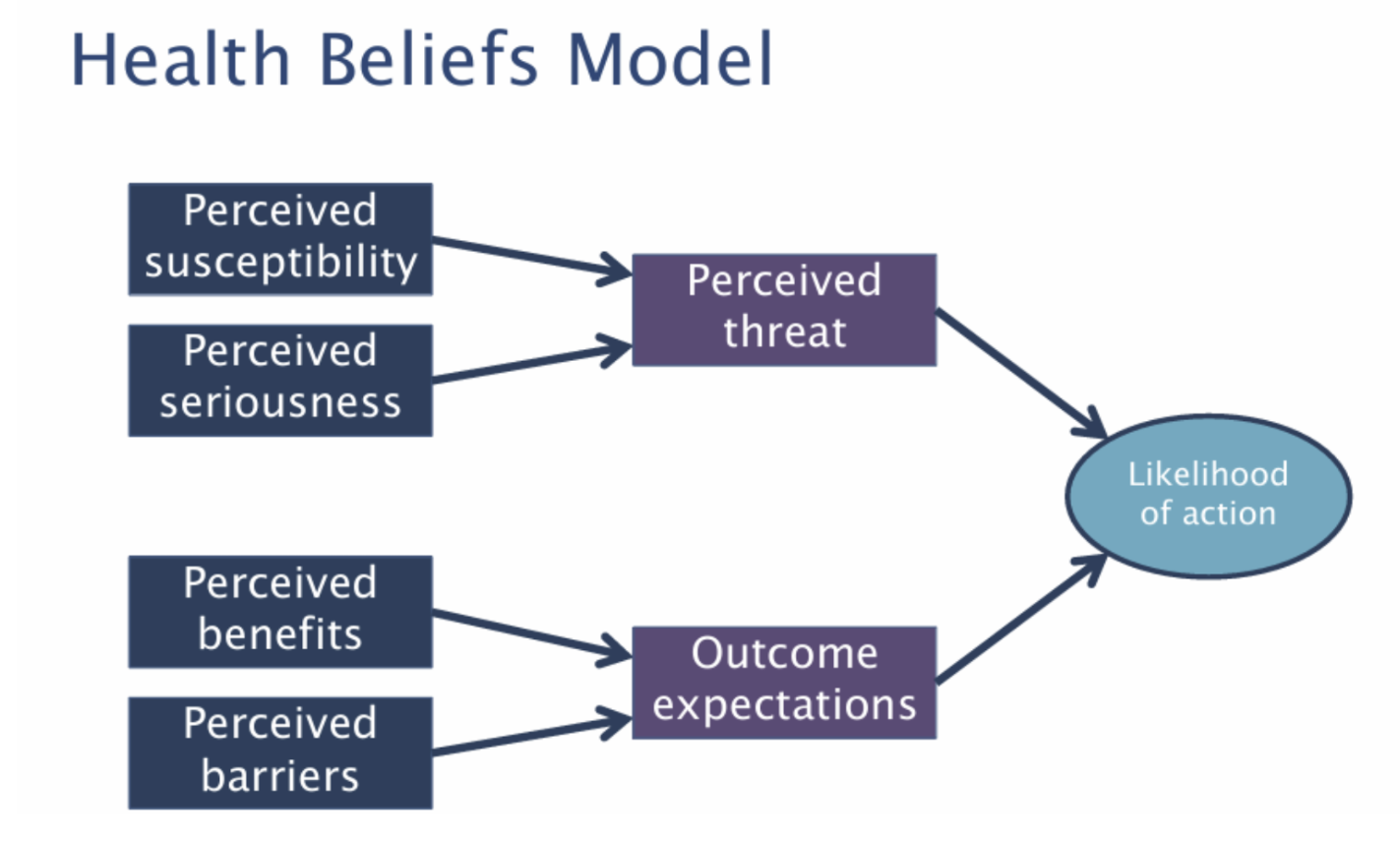
And the impact of perceived benefits and perceived barriers on outcome expectation which contribute to the likelihood of action.
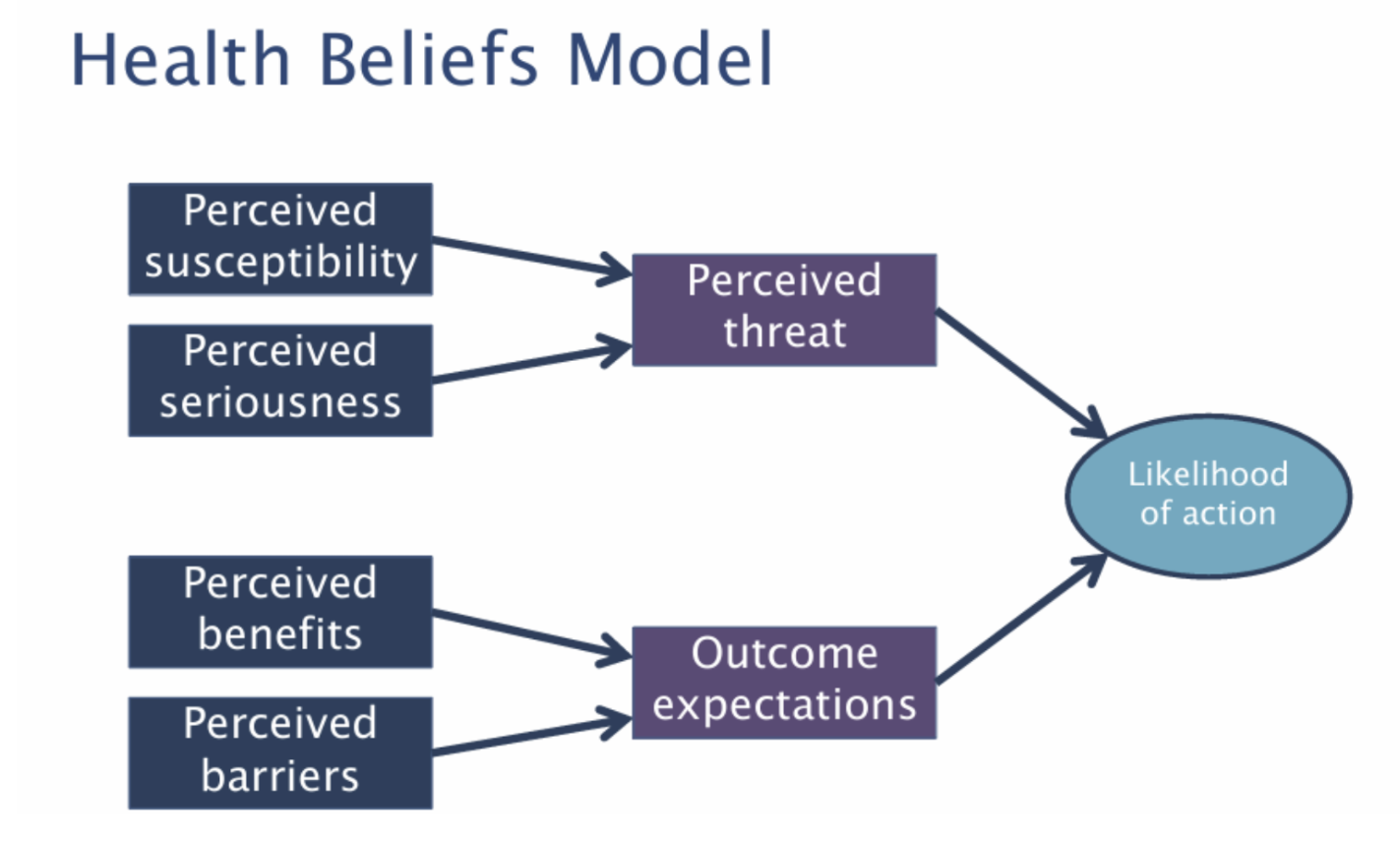
According to a meta-analysis of Health Belief Model, what influences the likelihood of actions more?
The influence of outcome expectations, that is, the perceived benefits and the perceived barriers is the largest.
Interesting to note that health campaigns often focus on the top branch, where research shows that we should be focusing on the bottom branch.
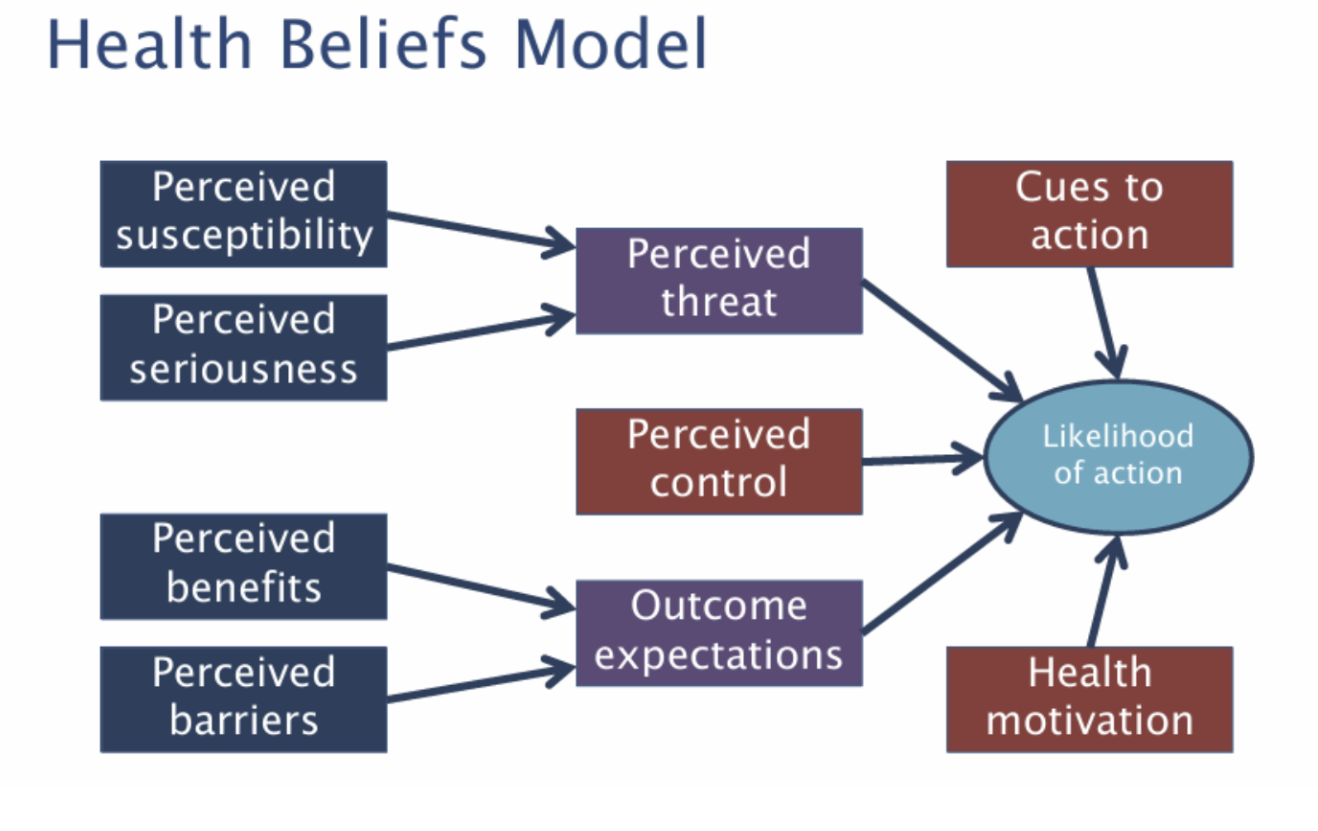
What did later iterations of the health beliefs of models do?
Added perceived control, the cues to action (e.g signs telling you not to eat, drink or smoke) and health motivation (if you just don’t care)
Are interventions based on these theories effective?
tends to be complicated. The TPB slightly better but HBM not so much.
What are the limitations of these models?
Assumes rationality of people
They fail to account for important variables (people are complicated and so is the world. )
Intentions may not account for all behaviour.
What is the Transtheoretical model/stages of change model?
Precontemplation – (I am not thinking about it) No recognition of problems, no intention to change - can also be recognition, but people just cannot change - e.g single mum with three kids, working 3 x jobs, studying at the same time – reality of the situation means that they don’t have the time.
Does not need both parts.
Contemplation – Intend to start change process within next 6 months
Preparation – Getting ready to change
Action – Engaging in change behaviours
Maintenance – Maintained change behaviour for 6 months.
What do you note about the stages of the model change?
Not a model that works linearly, may just hop between all the stages. Clinical Psych- likes to be manualised, but people often jump between stages of intentions.
Why is the idea of stages of change important?
may be useful in the sense that you should intervene differently at different points. Precontemplation - e.g. intervene with knowledge or to evaluate pros and cons. At Contemplation - e.g. an evaluation of what they would want to be
What is the difference between motivation phase vs. volitional phase?
A lot of the frameworks we use tend to get from the motivational phase to the volitional phase - in order to bridge this gap, we can use implementation intentions - e.g ‘if X happens, then I will do Y. ‘ It can often be useful to specify ‘how’ as well.
What is the effectiveness of implementation intentions?
In the context of encouraging men to do testicular self-examination - those who wrote an implementation intention were much more likely to change their behaviour. - from 8% to 46% in a month.
3 x components of Implementation intention
How is important → how will you exercise
To prevent an action → can attempt to tie a problem behaviour with a substitute action. For example, instead of smoking on — we will chew gum instead.
To ensure contingency plans → if you cannot do this, what will you do instead.
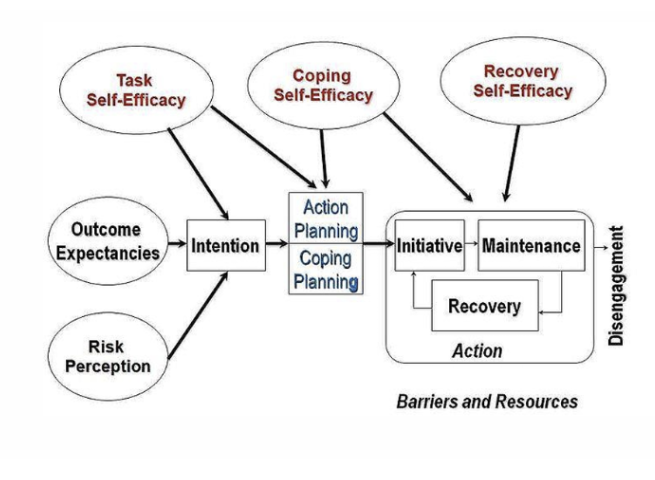
What is the health action process approach?
No need to completely memorise this. However, it is an attempt to capture all the elements of previous models.
E.g task self-efficacy, coping self-efficacy and recovery self-efficacy. → all versions of self-efficacy.
E.g the health beliefs model on the left.
E.g the stages of change on the right
What are some other factors to consider when changing health behaviours
Motivated reasoning
Self-presentation
Social learning - modelling
Operant conditioning
Economic factors - SES
What is motivated reasoning?
When it doesn’t suit our needs, we can ignore that stuff that we really should be paying attention to. Motivated to change despite valid reasons they wouldn’t be doing so.
Explain the ‘hot or not’ study?
Example of how people manipulate the information that they have to allow for seemingly reasoned action - e.g people were told people a lot of sexual partners, then told if they were hot or not. Those who were hot and had lots of sexual partners were more likely to have reduced risk of STI compared to not and lots.
What is self-presentation?
When the desire to convey a particular impression in order to increase rewards and minimise cost, this can influence a variety of health behaviours. E.g sun-tanning or vaping/smoking
What is social modeling?
The influence of peoples’ modelling on your behaviour. E.g bobo doll, adults behaviour observed by children, children would then go on to copy adult behaviours.
What is operant conditioning?
Learn to associate things between each other.
What is the influence of SES?
Tend to engage with less health habits, not just about knowledge but about capacity to change, the options to change.