Complicated Pregnancy: Vaginal Bleeding
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
ectopic, implantation, fibroids, ectropion, loss, abruption, rupture
Vaginal Bleeding During Pregnancy
-First Trimester
______ pregnancy, early pregnancy loss, threatened abortion, __________ bleeding, vaginitis, polyps, uterine ________, cervical __________
-Second and Third Trimester
Pregnancy ____, placenta previa, placental _________, bloody show associated with labor, uterine ________, and vasa previa
fallopian tube, hemorrhage, first, PID, IUD
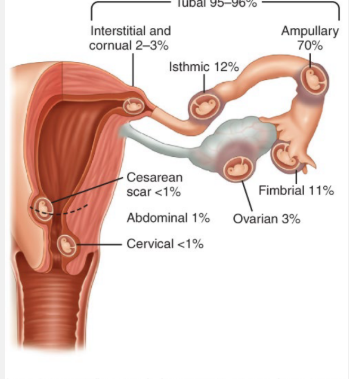
Ectopic Pregnancy: Background
-Pregnancy in which the developing blastocyst implants at a site other than the endometrium of the uterine cavity, with 96% occurring in the _______ _____
-___________ from ectopic pregnancy is the leading cause of maternal mortality in the _____ trimester
-Risk Factors → previous ectopic pregnancy, tubal pathology (from ___), tubal sterilization, ___ use, and IVF
pain, 5-7, bleeding, reproductive, rupture, hypotension, transabdominal, resucitation
Ectopic Pregnancy: Signs and Symptoms
-Abdominal or pelvic ____, usually adnexal or lower quadrant
Usually presents between _____ weeks gestation as the tube becomes distended
May be continuous or intermittent, dull or sharp, or mild or severe
Abrupt onset of severe pain → possible tubal rupture
-Irregular vaginal __________ or spotting
-Ectopic pregnancy should be suspected in any patient of ___________ age with these symptoms, especially those who have risk factors for ectopic pregnancy
-Patients may become hemodynamically unstable if there is a _______ and hemorrhage from the structure in which the pregnancy is implanted
Severe or persistent pain, feeling faint, ___________, tachycardia, shoulder pain due to diaphragmatic irritation by blood in the peritoneal cavity
If hemodynamically unstable → ___________ ultrasound to assess for intraperitoneal hemorrhage. Fluid ___________ and immediate surgical treatment is indicated
hCG, gestational sac, TVUS, 3510, intrauterine, extraovarian
Ectopic Pregnancy: Diagnosing in Hemodynamically Stable Patient
-___
hCG discriminatory zone → the serum hCG level above which a __________ ___ should be visualized on a transvaginal ultrasound (____)
Discriminatory zone for TVUS is ____ milli-IU
-TVUS
__________ pregnancy (IUP) visualized → ectopic ruled out
>89% of ectopic pregnancies show an __________ adnexal mass
methotrexate, <, cardiac, salpingectomy, instability, breastfeeding, rupture
Ectopic Pregnancy: Management
-______________ if the patient meets the following criteria
Hemodynamically stable
hCG _ 5000
No fetal _____ activity detected on TVUS
Ectopic mass size < 4 cm
Patient is willing to comply with post-treatment follow up
-Surgery (___________ or salpingostomy) if the following are true
Hemodynamic instability
Coexisting visible intrauterine pregnancy or ______________ (MTX contraindicated)
Signs or symptoms of impending ________
Renal insufficiency, immunodeficiency, active TB, PUD
early, intrauterine, 20, loss, decreases, not
Spontaneous Pregnancy Loss: Background
-The most common complication of _____ pregnancy
-Generally defined as a nonviable ______________ pregnancy up to __ weeks gestation
-Most common type is early pregnancy ____ (first trimester)
-Incidence of spontaneous abortion
First trimester → as high as 31%
___________ to approximately 10% when considering only losses occurring in clinical recognized pregnancies. Meaning, a lot of woman do ___ know they have had an early pregnancy loss and just assumes that their period was late
Second trimester → <1%
Abortion
Refers to pregnancy loss up to 20 weeks (sometimes called spontaneous abortion) or pregnancy termination at any gestational age
Anembryonic Pregnancy
Refers to a nonviable pregnancy with a gestational sac that does not contain a yolk sac or embryo
-”Blighted ovum”
-Includes pregnancies in which an embryo may have been present but has since been resorbed
Early pregnancy loss
A nonviable, intrauterine pregnancy within the first trimester
Embryonic demise
A pregnancy measuring <10 weeks by ultrasound with a visible embryo >7mm without cardiac activity
Fetal Demise
A fetus without cardiac activity is visualized, > 10 weeks
Miscarriage, two, 13, 20, infection, 20
Additional Terms: Fetal Loss
-__________ → synonymous with pregnancy loss
-Recurrent pregnancy loss → spontaneous loss of ____ or more pregnancies
-Second trimester pregnancy loss → pregnancy loss that occurs after __ weeks and prior to __ weeks of gestation
-Septic abortion → refers to any abortion, spontaneous or induced, that is complicated by uterine ____________
-Stillbirth/fetal death → pregnancy loss that occurs at __ weeks gestation or later, or at a weight of 350 grams or greater
35, chromosomal abnormalities, obesity, lead
Spontaneous Loss: Risk Factors
-Advanced maternal age ( > __ years)
Due to strong association with __________ ___________
-Prior pregnancy loss
-Maternal morbidity → CV disease, _______, thyroid disease, thrombophilia, infection
-Substance use
-Exposure to toxins and pollutants like ionizing radiation, ____, and arsenic
-Black, indigenous, and other POC
chromosomal, 20, polyps, trauma, infection, uterine, trisomy, premature
Spontaneous Pregnancy Loss: Etiology
-General Etiologies
___________ abnormalities cause up to 70% of pregnancy loss before __ weeks
Maternal anatomic anomalies such as fibroids, ______, and adhesions
Significant _______
-Second Trimester
_________ like chorioamnionitis, maternal viral infection
Chronic stressors of racial/ethnic disparities, financial disparities, food or housing insecurity
_____ malformation
Cervical insufficiency
Fetal malformation/syndromes like anencephaly, ______, renal agenesis, hydrops
Thrombophilia
Abruption
_________ preterm rupture of membranes
bleeding, dilated, infection
Spontaneous Pregnancy Loss: Presentation and Complications
-Clinical presentation → __________, cramping, asymptomatic
-Cervix may be ________
-Complications → hemorrhage and ___________
hCG, decrease
Spontaneous Pregnancy Loss: Diagnosis
-Ultrasound
-____ monitoring → hCG will _________ if there has been a spontaneous abortion or if it is a nonviable pregnancy
-If the hCG does not go down over time, you need to worry about retained products of conception
first, pass, 13, NSAIDs, opioids, hCG, emptying, antibiotics, DIC
Expectant Management of Spontaneous Pregnancy Loss
-70-80% of ______ trimester (early) pregnancy loss will ____ on its own
If > __ weeks, medication or surgical management is preferred
-________ for pain, may need _______ if beyond first trimester
-Follow-up/confirmation of a completed miscarriage → can be done using US, serum ___ levels, patient symptoms or a combination
Follow-up every one to two weeks until completion
-Complications
Incomplete uterine _________/retained tissue
Infection → if infection is identified, uterine aspiration is needed with _________
Bleeding → heavy bleeding and cramping is expected but should improve. if bleeding heavily, uterine aspiration may be needed
___ is a very serious but rare condition in which small blood clots develop throughout the bloodstream
Mifepristone, misoprostol, diarrhea, retained, hemorrhage, ultrasound
Spontaneous Pregnancy Loss: Medication Management
-___________ taken orally followed by ___________ given vaginally, buccally, or sublingually
-Med ADRs → nausea, vomiting, ________, abdominal pain, and pyrexia
-Complications → _______ products of conception, infection, __________ requiring transfusion
-Follow-up → __________ to confirm passage of gestational sac
antibiotic, aspiration, dilation, 16, perforation
Spontaneous Pregnancy Loss: Surgical Management
-Requires ___________ prophylaxis and cervical preparation
-First-trimester up to 16 weeks → uterine ___________
-Second-trimester → ________ and evacuation
Wide mechanical dilation of the cervix performed in an OR
Beginning at __ weeks gestation
Complications can be related to anesthesia, uterine _________, cervical trauma, infection, and intrauterine adhesions
infection, endometritis, pain, discharge, bleeding, fluids, antibiotics
Septic Abortion
-Abortion that is complicated by ________, commonly _________
-S/S → pelvic and/or abdominal ____, uterine tenderness, purulent vaginal ________, vaginal _________, fever, sepsis
-Workup → blood cultures, STI testing, urinalysis, and urine culture
-If hemodynamically unstable, resuscitate first (______, transfusion, vasopressors) then treated with IV __________ and surgical evacuation of the uterus
two, genetic, uterine, lupus, antiphospholipid, thrombosis, karyotype
Recurrent Pregnancy Loss
-Evaluation of recurrent pregnancy loss is indicated after ___ consecutive pregnancy losses
-Diagnostic evaluation → complete medical, surgical, _______, and family history and a physical examination
-Laboratory and imaging tests
Sonohysterography for assessment of _______ abnormalities
Anticardiolipin antibody (IgG and IgM) titer and _____ anticoagulant performed twice, 12 weeks apart
____________ syndrome causes vascular ________ and pregnancy morbidity
TSH and thyroid peroxidase antibodies
Parental ___________ and karyotype of the abortus if the above examinations are normal
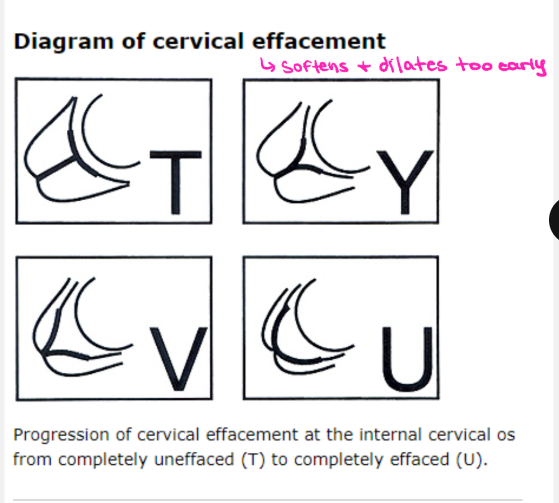
painless, recurrent, preterm, 24, weakness, trauma, congenital, short
Cervical Insufficiency: Background
-_________ cervical dilation that leads to second-trimester fetal expulsion
-A cause of ________ second-trimester pregnancy losses or extremely _______ live births
Often before __ weeks
-Defined by ACOG as “the inability of the uterine cervix to retain a pregnancy in the second trimester in the absence of clinical contractions, labor, or both”
-Pathogenesis → likely structural cervical __________
-Risk Factors → cervical _____, _________ cervical abnormality, and history of _____ cervical length
asymptomatic, pressure, contractions, discharge
Cervical Insufficiency: Symptoms
-Often ___________
-May have mild symptoms of pelvic ________, Braxton-Hicks-like contractions, premenstrual-like cramping and/or backache, change in vaginal ________
-Symptoms, if present, typically begin between 14-20 weeks
transvaginal, short, amniotic, history, ultrasound
Cervical Insufficiency
-___________ ultrasound
Cervical length is typically _____
Debris may be seen in the _________ fluid
-Making the diagnosis
Based on either a classic obstetric _______ or on a combination of obstetric history and transvaginal ___________ measurement of cervical length
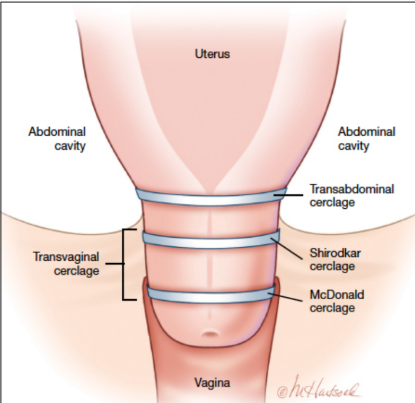
cerclage, progesterone, suture, strength, transvaginally
Cervical Insufficiency: Treatment
-Cervical _________ + vaginal ___________ supplementation
Cerclage → surgical procedure where a _______ is used to mechanically increase the tensile _________ of the cervix of patients with cervical insufficiency
Essentially stitching the cervix closed
-Can be done ___________ or transabdominally
Transvaginal usually attempted first
If not successful at preventing preterm labor, then transabdominal is done
unrelated, previa, rupture
Third Trimester Bleeding
-Bleeding _________ to labor and delivery
-Seen in 4-5% of pregnancies
-Causes → placenta _____, placental abruption, uterine _______, and vasa previa
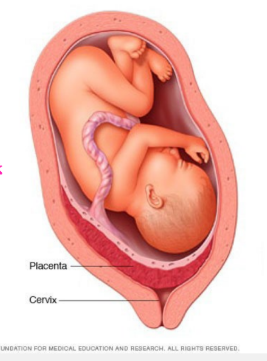
internal, bleeding, 20, painless, contractions, placental, before, hemorrhage
Placenta Previa: Background
-The presence of placental tissue that extends over the _______ cervical os, which can potentially lead to severe antepartum ________, preterm birth, and postpartum hemorrhage
-Should be suspected in any pregnant woman beyond __ weeks gestation who presents with __________ vaginal bleeding
Causes bleeding when uterine ___________ or gradual changes in the cervix and lower uterine segment apply shearing forces to the inelastic _________ attachment site
-For women who have not had a second-trimester ultrasound, bleeding after 20 weeks of gestation should prompt an ultrasound ______ a digital vaginal examination is performed
Palpation of the placenta can cause severe ___________
cesarean, surgery, age, endometriosis
Placenta Previa: Risk Factors
-Previous placenta previa
-Previous _________ delivery
-Multiple gestation
-Previous uterine ________
-Increasing parity
-Increasing maternal ___
-Infertility treatment
-Maternal smoking
-Maternal cocaine use
-Male fetus
-_____________
-Abortion
asymptomatic, 20, painless, persistent, transabdominal, TVUS, not, internal
Placenta Previa: Clinical Presentation and Diagnosis
-___________ is the most common
Found on anatomy ultrasound at 18-20 weeks
90% found on ultrasound before __ weeks of gestation resolve before delivery
-_________ vaginal bleeding is the cardinal symptom
90% of ________ cases
10-20% of women present with uterine contractions, pain, and bleeding
-Diagnosis → _________ ultrasonography
Subsequent ____ is performed when optimal visualization of the placenta and cervix is needed
-Low lying placenta → when the placental edge is <20 mm from, but ___, over the ________ os, the placenta is labeled as “low-lying”
These can go back up on their own or become complete previa
digital, orgasm, bleeding, exercise, c-section
Placenta Previa: Management of Asymptomatic Patients
-Avoid ______ cervical exam
-After 20 weeks, avoid any sexual activity that may lead to ________
Orgasm may be associated with uterine contractions which may provoke ________
Vaginal penetration might cause direct trauma to the previa, resulting in bleeding
-After 20 weeks of gestation, avoid moderate and strenuous ________, heavy lifting, or standing for prolonged periods of time
Activity has been linked to increases in preterm birth
-_-_______ at 36-37 weeks of gestation
hospitalize, fetal, labor, bleeding, 34, magnesium sulfate
Placenta Previa: Management of Acutely Bleeding Patients
-__________ for monitoring
-Order a CBC, type and cross-match, coagulation tests
Give fluids and/or transfusion as needed
-Continuous _____ monitoring
-C-section if in active _____, concerning fetal heart rate tracing, severe and persistent vaginal _________ such that maternal hemodynamic stability cannot be achieved or maintained, or significant vaginal bleeding after __ weeks gestation
-___________ ________ for neuroprotection for pregnancies < 32 weeks
34, stable, corticosteroids, anemia, negative, C-section
Placenta Previa: Expectant Management
-<__ weeks of gestation who are hemodynamically ______ or quickly stabilized and have a normal fetal heart rate pattern are candidates for expectant management
-Antenatal _____________
-Correction of ______ with iron supplementation
-Rhogam for RhD-_________ patients
-_-_______ at 36 to 37 weeks
separation, decidua, 20, rupture, vessels
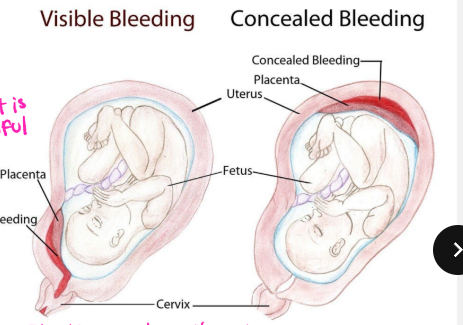
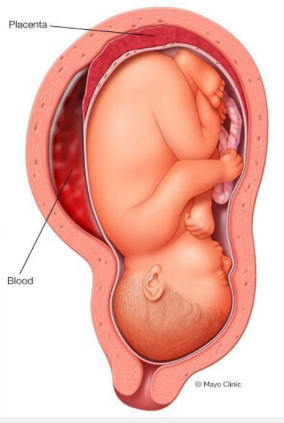
Placental Abruption: Background
-Also known as abruptio placentae
-Premature ___________ of the placenta from the ________ at or after __ weeks gestation
Decidua → specialized layer of endometrium that forms the base of the placental bed
Can be partial or complete
-Pathophysiology → immediate cause is _______ of maternal ________ in the decidua basalis
Can be acute or chronic
hemorrhage, complete, decompression, strain, stretch
Placental Abruption: Acute Severe Abruption
-High-pressure arterial ____________ in the placenta dissects through the placental-decidual interface and causes ________ or nearly complete placental separation
-A small proportion of abruptions are due to
Sudden mechanical events
Rapid uterine ____________
Due to strain between the pliable myometrium and the inelastic placenta
In MVAs, rapid acceleration-deceleration of the uterus causes uterine ______ exceeding concomitant placental _______ → leads to shearing force between the placenta and uterine wall
spiral, necrosis, hemorrhage, self-limited, hypertension, cocaine, smoking
Placental Abruption: Chronic and Risk Factors
-Abnormalities in the early development of the ______ arteries lead to decidual _________, placental inflammation and possibly infarction, and ultimately low-pressure venous ____________ at the periphery of the placenta
-Tends to be ____-__________ and results in a small area of separation
-Most common risk factors → _____________, ________, ________ use
abrupt, bleeding, pain, irritability, decidua, bleeding, preeclampsia
Placental Abruption: Features
-Acute abruption → ______ onset of vaginal _________, mild to moderate abdominal and/or back ____, uterine contractions, and firm/rigid/tender uterus
-Concealed abruption → uterine contractions/________ only
All or most of the blood is trapped between the fetal membranes and _______
-Chronic abruption → relatively light, chronic, intermittent, _________
At risk for developing oligohydraminos, fetal growth restriction, and _________
DIC, fibrinogen, hematoma
Placental Abruption: Labs and Imaging
-Labs
Severe abruptions → ___ → disruption of hemostasis
___________ level, which correlates best with severity of bleeding, presence of overt DIC, and the need for transfusion
-Ultrasound
Retroplacental __________ is more likely to be seen with more extensive placental separation and in patients who go on to have adverse who go on to have adverse maternal and perinatal outcomes
Absence does not exclude any interference
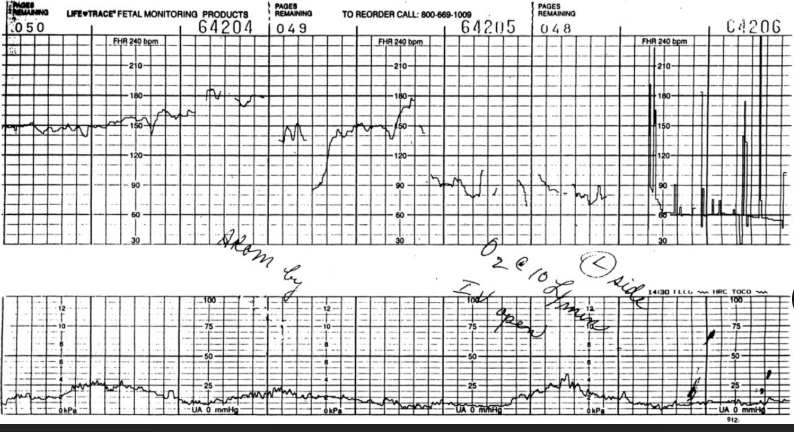
monitoring, transfuse, magnesium, corticosteroids, Rhogam, C-section, 37-38, Pitocin, 4
Placental Abruption: Management
-Continuous fetal heart rate _____________
-Assessment of blood loss and maternal hemodynamic status → resuscitate and _________ blood if needed
-Lactated ringers to maintain urine output above 30 mL/hour
-For patients likely to deliver within 24-48 hours:
_________ sulfate for neuroprotection for pregnancies <32 weeks of gestation
Antenatal _____________ for pregnancies <34 weeks
__________ for patients who are RhD-negative
-If mother is hemodynamically unstable → __-_______
-If fetal heart rate pattern is concerning → c-section
-If 34-36 weeks → vaginal delivery or C-section
-If <34 weeks and fetus and mother are both stable → monitor closely and deliver by _______ weeks (unless condition worsens)
-_________ (IV oxytocin) administered postpartum to stop bleeding
-In subsequent pregnancies, ultrasound every _ weeks starting at 24-28 weeks until birth to screen for growth restriction
umbilical, vessels, membranes, Wharton’s, os, unprotected
Vasa Previa: Definitions
-Wharton’s Jelly → a gelatinous connective tissue in the _________ cord present between the amniotic epithelium and the umbilical ________
-Velamentous umbilical cord insertion → when the placental end of the cord consists of divergent umbilical vessels surrounded only by fetal ___________, with no ___________ jelly
-Vasa previa → when fetal blood vessels are present in the membranes covering the internal cervical __, _________ by placental tissue or Wharton’s jelly
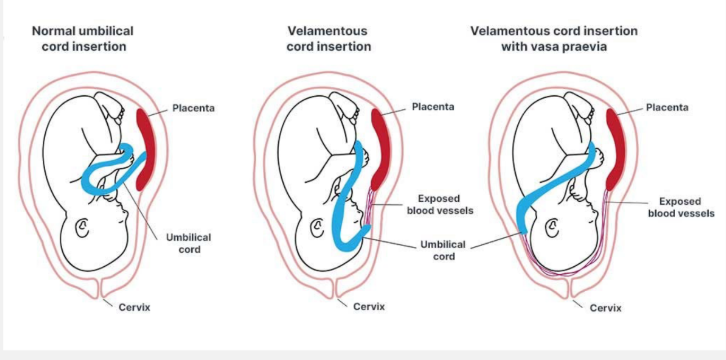
lower, previa, IVF, multiple
Vasa Previa: Risk Factors
-Velamentous cord insertion
-Umbilical cord insertion in the ______ third of the uterus at first-trimester ultrasound
-Placenta _______ or low-lying placenta on second-trimester ultrasound scan
-___ or other forms of ART
-_________ gestation
internal, sonolucency, normal, palpable, rupture, death, preterm
Vasa Previa: Diagnostics
-Imaging
Ultrasound → linear sonolucent area that passes over the _______ os
Color doppler flow and waveform analysis → umbilical artery or vein waveforms and confirms that the ___________ is a blood vessel
-Physical Exam
Usually ________
Rarely, pulsating vessels in the membranes overlying the cervical os are __________ on digital examination
-Why it’s dangerous
Spontaneous or iatrogenic ________ of the membranes → fetal bleeding → hypotension → fetal heart rate abnormalities → fetal ______ due to exsanguination
Pregnancies complicated by vasa previa and area also at increased risk for __________ birth
third, rest, 4, Betamethasone, c-section, transfusion
Vasa Previa: Management
-Confirm the diagnosis in the early _____ trimester
-Pelvic ____ and avoid high-impact activities
-Ultrasounds to evaluate fetal growth every _ weeks starting at 24 weeks
-____________ by 34 weeks gestation
-Hospital admission for close fetal surveillance between 30-34 weeks
-Scheduled _-________ at 34 to 35 weeks
-Emergency c-section if patient spontaneously goes into labor, has PROM, concerning fetal tracings, or vaginal bleeding accompanies by fetal tachycardia
-Type O negative blood should be available for emergency ___________ of a severely anemic newborn
Ectopic pregnancy
What is the most likely diagnosis in this patient?
A 29 y/o woman presents with left lower abdominal pain and light vaginal spotting for one day. Her last menstrual period was 7 weeks ago. She describes the pain as sharp and unilateral. Vital signs show BP 98/62, HR 112. A urine pregnancy test is positive. On pelvic exam, she has cervical motion tenderness and adnexal tenderness on the left. Transvaginal ultrasound does not show an intrauterine pregnancy.
Miscarriage
What is the most likely diagnosis in this patient?
A 33 y/o woman who is 10 weeks pregnant presents with vaginal bleeding and cramping pelvic pain. She reports passing “tissue” earlier today. On exam, the cervical os is open, and products of conception are visible in the vaginal vault. Ultrasound shows heterogenous material in the uterus but no identifiable embryo.
Cervical insufficiency
What is the most likely diagnosis in this patient?
A 26 y/o G2P1 woman at 18 weeks gestation presents for a routine prenatal visit. She reports mild pelvic pressure but no bleeding or contractions. Ultrasound shows a shortened cervix measuring 1.8 cm with funneling. Her first pregnancy ended in a painless delivery at 22 weeks.
Placenta previa
What is the most likely diagnosis in this patient?
A 35 y/o G3P2 woman at 32 weeks gestation presents with painless bright red vaginal bleeding after intercourse. She denies contractions and has normal fetal movement. Vital signs are stable. Fetal heart rate is 120 BPM. Transabdominal ultrasound shows the placenta covering the internal cervical os.
Placental abruption
What is the most likely diagnosis in this patient?
A 30 y/o woman at 36 weeks comes to the ED with sudden-onset severe abdominal pain, back pain, and vaginal bleeding. She is rigid and tender on exam. Fetal heart monitoring shows late decelerations. She has a history of cocaine use and chronic hypertension.
Vasa previa
What is the most likely diagnosis in this patient?
A 27 y/o woman at 35 weeks pregnant presents with painless vaginal bleeding that began after spontaneous rupture of membranes. Soon after the bleeding started, fetal heart tracing showed bradycardia. Ultrasound earlier in pregnancy noted a velamentous cord insertion.