Anesthesia - Quiz 4
5.0(1)
Card Sorting
1/165
Earn XP
Description and Tags
Anesthesia Emergencies/Complications; Equine Anesthesia; Ruminant/Swine Anesthesia; Anesthesia with a Co-exiting Disease; Euthanasia
Last updated 4:13 PM on 5/1/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
166 Terms
1
New cards
What is important to remember during equine pre-anesthesia?
avoid excitement of the patient prior to and during induction/sedation
2
New cards
Should equines be fasted prior to anesthesia?
it is a clinician preference
fasting can decrease the pressure on the major abdominal vessels with less cranial displacement of the diaphragm
some texts recommend 8-12 hour fasting
fasting can decrease the pressure on the major abdominal vessels with less cranial displacement of the diaphragm
some texts recommend 8-12 hour fasting
3
New cards
What are the steps to pre-anesthesia in equines?
prepare, assess, and weight your patient
place an IV catheter
rinse out the mouth and clean out the hooves (helps reduce aspiration pneumonia) (if doing standing anesthesia, you don’t need to rinse out the mouth)
prepare equipment, drugs, fluids, induction materials, etc
make sure you have proper monitoring equipment
place an IV catheter
rinse out the mouth and clean out the hooves (helps reduce aspiration pneumonia) (if doing standing anesthesia, you don’t need to rinse out the mouth)
prepare equipment, drugs, fluids, induction materials, etc
make sure you have proper monitoring equipment
4
New cards
What is standing sedation used for?
eye procedures (laser, enucleation, corneal, ulcer treatments)
minor orthopedic procedures such as casting and x-rays
laceration repairs and hoof trims
minor orthopedic procedures such as casting and x-rays
laceration repairs and hoof trims
5
New cards
When performing anesthesia in the field, what will you use to measure the horse’s weight?
a weight tape
6
New cards
Why is it important to have a head prop of assistant to hold the horse's head in a neutral position?
to avoid congestion which can lead to respiratory obstruction
7
New cards
Mallard anesthesia machine
Bellows
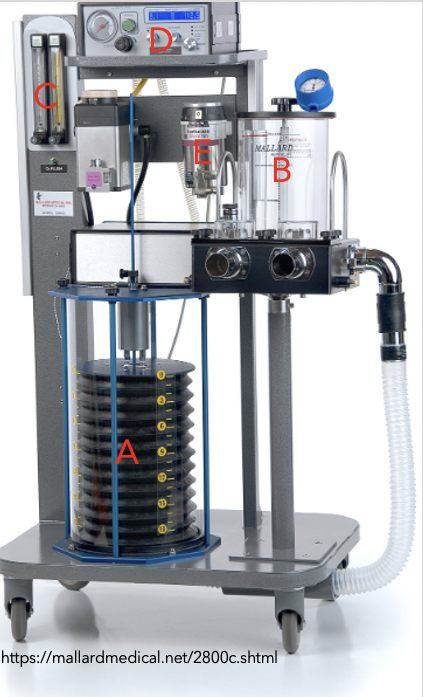
8
New cards
Tafonius anesthesia machine
piston driven

9
New cards
SurgiVet anesthesia machine

10
New cards
What is the difference between the SurgiVet, Mallard, and Tafonius machines?
The Tafonius is piston driven while the other two are bellows
11
New cards
Acepromazine is a good addition when…?
you have a patient who is young/excites or uncooperative
12
New cards
Who should you not give acepromazine to?
hypotensive patients and breeding stallions
low hematocrit and liver disease patients
low hematocrit and liver disease patients
13
New cards
When is Ace given?
30mins to 1 hour prior to anesthesia to help calm the horse down and allow for a smoother sedation and induction
14
New cards
Are full mu opioids used in horses?
No, they cause intestinal ileum and can lead to colic
15
New cards
What is the opioid of choice for equine pre meds?
Butorphanol (0.03mg/kg)
16
New cards
Euthanasia: a tool
a humane and responsible option
* failure to respond to RX
* no effective RX
* Poor quality of life
NOT a substitute for poor veterinary care
should be performed competently by willing individuals
* failure to respond to RX
* no effective RX
* Poor quality of life
NOT a substitute for poor veterinary care
should be performed competently by willing individuals
17
New cards
Humane Killing
subdivided into:
* euthanasia (individuals)
* human slaughter (large numbers)
* depopulation (large numbers)
* euthanasia (individuals)
* human slaughter (large numbers)
* depopulation (large numbers)
18
New cards
AVMA Euthanasia Guidelines
* periodically updated
* available in print and online
* presents physiology, animal and behavioral issues, modes of action, relative merits of various methods
* accepted as __THE__ definitive reference
* available in print and online
* presents physiology, animal and behavioral issues, modes of action, relative merits of various methods
* accepted as __THE__ definitive reference
19
New cards
Acceptable
methods producing humane death as the sole means of euthanasia
20
New cards
Acceptable with conditions
acceptable methods when certain conditions are met
21
New cards
Unacceptable
methods __not__ to be used under __any__ conditions
22
New cards
Depopulation and slaughter may employ euthanasia techniques, but not all depopulation or slaughter methods meet the AVMA criteria for euthanasia…
these activities may be termed humane killing
23
New cards
Pain perception requires functioning
cerebral cortex
24
New cards
Anesthetized or properly euthanized animals
do not feel pain
25
New cards
Loss of consciousness should precede
loss of muscle movement
26
New cards
What are the 3 basic mechanisms of euthanasia?
direct depression of neurons necessary for life functions
* anesthesia overdose; CO2
Hypoxia
* argon, nitrogen, CO2; exsanguination
Physical disruption of brain activity
* concussive stunning; electrocution; cervical dislocation; gunshot
* anesthesia overdose; CO2
Hypoxia
* argon, nitrogen, CO2; exsanguination
Physical disruption of brain activity
* concussive stunning; electrocution; cervical dislocation; gunshot
27
New cards
Loss of consciousness occurs at substantially different rates with different methods. T/F?
True
28
New cards
Suitability will depend on whether the animal experiences pain and/or distress _______________ loss of consciousness.
PRIOR TO
29
New cards
Events occurring _________ loss of consciousness, although unpleasant to watch, do not contribute to adverse welfare.
AFTER
30
New cards
Anesthetic Overdose
inhaled anesthetics
* expensive; personal exposure
* CO2
Injectable anesthetics
* Pentobarbital
* 1 min onset, minimal movement if properly restrained; carcass contamination
Death 2º to respiratory, cardiac arrest
* expensive; personal exposure
* CO2
Injectable anesthetics
* Pentobarbital
* 1 min onset, minimal movement if properly restrained; carcass contamination
Death 2º to respiratory, cardiac arrest
31
New cards
Hypoxia
gases that displace oxygen to
32
New cards
Physical disruption of brain function
bullet; penetrating captive bolt
* destroys cortex and midbrain
electrocution (2 steps)
* humane, painless if properly done; no drug residues
* follow with 2nd method to assure death
* destroys cortex and midbrain
electrocution (2 steps)
* humane, painless if properly done; no drug residues
* follow with 2nd method to assure death
33
New cards
Regardless of euthanasia method
death __MUST__ be confirmed.
34
New cards
All methods have potential to cause physical injury and death. T/F?
True
35
New cards
Psychological issues (the killing-caring paradox)
* transferal of personal feelings/fear onto the animal
* depression, grief, anger, guilt, sleeplessness
* job dissatisfaction may result in absenteeism, belligerence, careless/callous animal handling
* depression, grief, anger, guilt, sleeplessness
* job dissatisfaction may result in absenteeism, belligerence, careless/callous animal handling
36
New cards
People are less disturbed when they feel distanced from the physical act or when animal doesn’t move. T/F?
True
The “Trolley Problem” and “Fat Man Problem”
The “Trolley Problem” and “Fat Man Problem”
37
New cards
In many states, shelters can not obtain injectable DEA Schedule II or III drugs. T/F?
True
* injectable euthanasia can only be performed if a local vet is willing to participate
* leaves gas euthanasia chambers as only option
* injectable euthanasia can only be performed if a local vet is willing to participate
* leaves gas euthanasia chambers as only option
38
New cards
Some states have re-written their pharmacy laws to permit shelters to obtain their own DEA license. T/F?
True
* requires staff training and certification
* requires staff training and certification
39
New cards
Euthanasia in the face of a foreign animal disease:
Timely response necessary to prevent disease spread
* All infected within 24 hrs; all contiguous farms within 48 hrs
Euthanasia vs depopulation
* Euthanasia methods can be used for depop, but not all depop methods are euthanasia
* We owe it to the animals to do the best we can under the circumstances
* All infected within 24 hrs; all contiguous farms within 48 hrs
Euthanasia vs depopulation
* Euthanasia methods can be used for depop, but not all depop methods are euthanasia
* We owe it to the animals to do the best we can under the circumstances
40
New cards
Why is CO2 used?
Denser than air; noninflammable
Extensibly studied
* anesthesia due to ↓ pHi; not reliant on hypoxia
* minimally affected by respiratory disease
* recommended by OIE, AVMA, AASV for human killing of swine
Far less labor intensive than bolt guns
Fewer people involved, less safety risk
Extensibly studied
* anesthesia due to ↓ pHi; not reliant on hypoxia
* minimally affected by respiratory disease
* recommended by OIE, AVMA, AASV for human killing of swine
Far less labor intensive than bolt guns
Fewer people involved, less safety risk
41
New cards
Medium or High-expansion Water-based Foams
Conditionally approved by USDAAPHIS (2006)
* Zoonosis; spreading infectious disease
* Unsound buildings
Uses air to form bubbles
* Immersion causes airway occlusion and death by suffocation
Add CO2 , N2 ?
* Zoonosis; spreading infectious disease
* Unsound buildings
Uses air to form bubbles
* Immersion causes airway occlusion and death by suffocation
Add CO2 , N2 ?
42
New cards
Horses
• Pentobarbital; large volumes (approx 100 mls) needed
* Not FDA approved for this species
* Major disposal issues
* Use of a jugular vein IV catheter will facilitate the procedure
* In some situations, may be easier to anesthetize the horse 1st, then euthanize
Intrathecal lidocaine during general anesthesia
* Humane; eliminates drug residue issues
In certain situations, gunshot or penetrating captive bolt is acceptable
* Not FDA approved for this species
* Major disposal issues
* Use of a jugular vein IV catheter will facilitate the procedure
* In some situations, may be easier to anesthetize the horse 1st, then euthanize
Intrathecal lidocaine during general anesthesia
* Humane; eliminates drug residue issues
In certain situations, gunshot or penetrating captive bolt is acceptable
43
New cards
Zoo and Wildlife
Must consider what will happen to the carcass
* Head shot, penetrating captive bolt, KCl IV or MgSO4 IV during general anesthesia to reduce toxicity to scavengers
Species-specific guidelines available
* Head shot, penetrating captive bolt, KCl IV or MgSO4 IV during general anesthesia to reduce toxicity to scavengers
Species-specific guidelines available
44
New cards
Euthanasia of Pregnant Animals
Mammalian embryos and fetuses are unconscious and insentient throughout pregnancy and birth
* Several in utero neuroinhibitors present during prenatal life initially maintain unconsciousness
* An isoelectric EEG, which is incompatible with consciousness, rapidly appears after cessation of placental oxygen supply
Embryos and fetuses cannot consciously experience any sensations or feeling such as breathlessness or pain, and therefore cannot suffer while dying in utero, whatever the cause
* Similar conclusions have been drawn regarding the possibility that consciousness may not occur until after hatching in domestic chickens
* Several in utero neuroinhibitors present during prenatal life initially maintain unconsciousness
* An isoelectric EEG, which is incompatible with consciousness, rapidly appears after cessation of placental oxygen supply
Embryos and fetuses cannot consciously experience any sensations or feeling such as breathlessness or pain, and therefore cannot suffer while dying in utero, whatever the cause
* Similar conclusions have been drawn regarding the possibility that consciousness may not occur until after hatching in domestic chickens
45
New cards
Fetal Resuscitation
Attempts to remove the fetus from the uterus or to revive a fetus following death of the dam are likely to result in serious welfare complications for the newborn
* Physiological immaturity; effects of fetal hypoxemia; once removed from uterus and spontaneous breathing occurs, potential for consciousness and sentience
* IP pentobarbital is recommended for fetuses that have been removed from the uterus
* Physiological immaturity; effects of fetal hypoxemia; once removed from uterus and spontaneous breathing occurs, potential for consciousness and sentience
* IP pentobarbital is recommended for fetuses that have been removed from the uterus
46
New cards
The function of the cardiovascular system is to
circulate blood and ensure delivery of oxygen to the body
47
New cards
Vasodilation
Decreased systemic vascular resistance (think about a drink straw compared to a coffee stirrer)
48
New cards
Oxygen delivery =
Cardiac Output x oxygen content
49
New cards
MAP (mean arterial pressure) =
CO x SVR (systemic vascular resistance)
50
New cards
Four Mechanisms that can cause hypotension
Vasodilation
Bradycardia
Decrease in cardiac preload (directly related to ventricular filling)
Decrease in myocardial contractility
Bradycardia
Decrease in cardiac preload (directly related to ventricular filling)
Decrease in myocardial contractility
51
New cards
What are the causes of vasodilation?
Anesthetic agents
* propofol
* acepromazine
* inhalant anesthetics
Hypothermia (extreme cases)
Cardiac drugs
Sepsis
Anaphylaxis
* propofol
* acepromazine
* inhalant anesthetics
Hypothermia (extreme cases)
Cardiac drugs
Sepsis
Anaphylaxis
52
New cards
What are the causes of bradycardia?
excessive anesthetic depth
arrhythmias
hypothermia (extreme cases)
opioids
alpha-2 adrenergic agonists (initially vasoconstriction)
arrhythmias
hypothermia (extreme cases)
opioids
alpha-2 adrenergic agonists (initially vasoconstriction)
53
New cards
What are the causes of decreased preload?
* hemorrhage
* dehydration (vomiting, diarrhea)
* 3rd spacing (effusions, ascites, GI fluid) - occurs when too much fluid moves from the intravascular space (blood vessels) into the interstitial or “third” space - can cause edema, reduced cardiac output, and hypotension
* vascular compression/obstruction - occurs when blood vessels are under abnormal pressure, limiting the size of the blood vessel and the amount of blood that flows through it
* positive pressure ventilation -due to cardiac compression
* vasodilation
* dehydration (vomiting, diarrhea)
* 3rd spacing (effusions, ascites, GI fluid) - occurs when too much fluid moves from the intravascular space (blood vessels) into the interstitial or “third” space - can cause edema, reduced cardiac output, and hypotension
* vascular compression/obstruction - occurs when blood vessels are under abnormal pressure, limiting the size of the blood vessel and the amount of blood that flows through it
* positive pressure ventilation -due to cardiac compression
* vasodilation
54
New cards
Stage A
patient at risk but no clinical signs
55
New cards
Stage B
B1
* murmur, no past or present clinical signs of heart enlargement or failure
B2
* murmur and cardiomegaly but asymptomatic
* murmur, no past or present clinical signs of heart enlargement or failure
B2
* murmur and cardiomegaly but asymptomatic
56
New cards
Stage C
patients with past or present clinical signs of heart failure with structural cardiac disease
57
New cards
Stage D
patients with end-stage heart failure that are refractory to standard therapies
58
New cards
Stage A & B1
generally do not require intensive management
59
New cards
Stage B2
* keep patient heart rates normal
* keep patients normothermic
* avoid alpha-2 adrenergic agonists (depends on clinician)
* keep patients normothermic
* avoid alpha-2 adrenergic agonists (depends on clinician)
60
New cards
Stage C & D
* rely on balanced anesthesia
* avoid alpha-2 adrenergic agonists (depends on clinician)
* use opioids/benzodiazepines to reduce amounts of induction and inhalant agents needed
* avoid alpha-2 adrenergic agonists (depends on clinician)
* use opioids/benzodiazepines to reduce amounts of induction and inhalant agents needed
61
New cards
What is hypertrophic cardiomyopathy?
Thickening of the cardiac muscle leading to stiffening and failure of relaxation and adequate filling (think of body builders)
62
New cards
Anesthetic Management of hypertrophic cardiomyopathy
Dissociatives are contraindicated in severe HCM because the increase in HR, contractility, & BP can lead to reduced cardiac output while also increasing cardiac workload and oxygen demand – can and will cause death
Cautious with fluid administration
Balanced Anesthesia
Cautious with fluid administration
Balanced Anesthesia
63
New cards
What is dilated cardiomyopathy?
primary loss of myocardial contractibility that can lead to dilation of the ventricles
64
New cards
What is the anesthetic management of dilated cardiomyopathy?
Cautious with fluid administration
Manage arrhythmias
Inotropic support
Balanced Anesthesia
Alpha-2 adrenergic agonist are contraindicated due to the increase in afterload(amount of pressure that the heart needs to exert to eject the blood during ventricular contraction) whichcan cause a decrease in cardiac output
Manage arrhythmias
Inotropic support
Balanced Anesthesia
Alpha-2 adrenergic agonist are contraindicated due to the increase in afterload(amount of pressure that the heart needs to exert to eject the blood during ventricular contraction) whichcan cause a decrease in cardiac output
65
New cards
Do not give dissociative to cats with
thyroid problems
* if they have a thyroid problem, they most likely also have HCM
* if they have a thyroid problem, they most likely also have HCM
66
New cards
Minute ventilation
volume of gas inhaled or exhaled in lungs per minute ventilation
67
New cards
Maintain CO2 levels (35-45 mmHg) and pH (7.35-7.45)
these parameters are directly related
68
New cards
Hb
what binds to O2 – the body’s oxygen carrying capability
69
New cards
SaO2
the percentage of available binding sites on hemoglobin that are bound with oxygen in arterial blood
* how much hemoglobin is available
* how much hemoglobin is available
70
New cards
PaO2
the alveolar partial pressure of oxygen is the driving force for the diffusion of oxygen across the alveolar membranes, through pulmonary capillary walls, and into the arterial blood flow and erythrocytes (RBC) for transport throughout the body into peripheral tissues
* ARE THE LUNGS UP TAKING OXYGEN
* ARE THE LUNGS UP TAKING OXYGEN
71
New cards
What are the causes of hypoxemia?
* Low inspired oxygen fraction –FiO2
* Hypoventilation – increased CO2
* Diffusion impairments – gases do not move normally across the lung tissues into the blood vessels of the lung – decreased oxygen levels – increased CO2 levels - secondary to primary respiratory disease
* Ventilation-perfusion mismatching – areas of the lungs are poorly perfused but well ventilated or poorly ventilated and well perfused
* Right-to-left shunts – non oxygenated blood may flow directly back to the rest of the body – it may flow from the right chamber to the left chamber and never pass through the lungs to be oxygenated – cardiac defect
* Hypoventilation – increased CO2
* Diffusion impairments – gases do not move normally across the lung tissues into the blood vessels of the lung – decreased oxygen levels – increased CO2 levels - secondary to primary respiratory disease
* Ventilation-perfusion mismatching – areas of the lungs are poorly perfused but well ventilated or poorly ventilated and well perfused
* Right-to-left shunts – non oxygenated blood may flow directly back to the rest of the body – it may flow from the right chamber to the left chamber and never pass through the lungs to be oxygenated – cardiac defect
72
New cards
Examples of obstructive issues:
Asthma
Laryngeal paralysis
Brachiocephalic
Tracheal collapse
Laryngeal paralysis
Brachiocephalic
Tracheal collapse
73
New cards
What is the anesthesia management for obstructions?
Minimize excitement and stress
Mild sedation may be warranted
* Butorphanol, acepromazine
Mild sedation may be warranted
* Butorphanol, acepromazine
74
New cards
Ventilation refers to
CO2
75
New cards
Perfusion refers to
oxygen
76
New cards
Examples of decreased lung capacity:
Aspiration pneumonia
Muscle rigidity
Obesity
Intra-abdominal changes – tumor – GDV - hemoabdomen
Muscle rigidity
Obesity
Intra-abdominal changes – tumor – GDV - hemoabdomen
77
New cards
What is the anesthetic management of decreased lung capacity?
* Protect airway and suction mouth as needed
* Pre-oxygenate
* Mechanical ventilation
* Monitor oxygenation
* Pre-oxygenate
* Mechanical ventilation
* Monitor oxygenation
78
New cards
Neurological Disease
Brain injury, trauma, tumors, hydrocephaly
* Cerebral perfusion – (blood flow to the brain) BP affects the cerebral perfusion pressure, if BP is low the blood flow to the brain may be limited
* Intracranial pressure – if ICP is too high – blood flow to the brain may be limited
* Cerebral perfusion – (blood flow to the brain) BP affects the cerebral perfusion pressure, if BP is low the blood flow to the brain may be limited
* Intracranial pressure – if ICP is too high – blood flow to the brain may be limited
79
New cards
What is the anesthetic management for neurological disease such as Brain injury, trauma, tumors, or hydrocephaly?
* Maintain MAP
* Oxygen and ventilatory support
* Mannitol – diuretic – helps treat brain swelling and reduce ICP
* Hypertonic saline – helps treat brain swelling and reduce ICP
* Oxygen and ventilatory support
* Mannitol – diuretic – helps treat brain swelling and reduce ICP
* Hypertonic saline – helps treat brain swelling and reduce ICP
80
New cards
What is the anesthetic management for neurological diseases such as Spinal injuries or intervertebral disc disease?
* Patients at risk for developing neuropathic pain – can happen if your nervous system is damaged or not working correctly – you can feel pain from any of the various levels of the nervous system – the peripheral nerves, the spinal cord and the brain
* Adjunct analgesics to opioids beneficial
* Ketamine, lidocaine
* Adjunct analgesics to opioids beneficial
* Ketamine, lidocaine
81
New cards
The liver provides multiple essential functions such as….
* Bile formation and excretion – filters bilirubin, cholesterol, drugs and toxins – intestinal absorption
* Metabolic functions – changes food and water into energy
* Plasma proteins- stabilizes osmotic pressure – helps maintain pH – fights infection
* Metabolic functions – changes food and water into energy
* Plasma proteins- stabilizes osmotic pressure – helps maintain pH – fights infection
82
New cards
Complications associated with hepatic disease
* Hepatic encephalopathy – loss of brain function (liver not filtering toxins)
* Hypokalemia – can worsen insulin resistance leads to fatty liver
* Hypoglycemia – liver responsible for maintaining plasma glucose
* Hypoalbuminemia – doesn’t produce enough ALB to keep fluid in vessels
* Ascites – fluid build up on the abdomen
* Coagulopathy – houses clotting factors
* Hypotension – hypertension in portal vein
* Impaired drug biotransformation – poor filter
* Storage of glycogen – enzymes break down glycogen into glucose when the body needs energy
* Hypokalemia – can worsen insulin resistance leads to fatty liver
* Hypoglycemia – liver responsible for maintaining plasma glucose
* Hypoalbuminemia – doesn’t produce enough ALB to keep fluid in vessels
* Ascites – fluid build up on the abdomen
* Coagulopathy – houses clotting factors
* Hypotension – hypertension in portal vein
* Impaired drug biotransformation – poor filter
* Storage of glycogen – enzymes break down glycogen into glucose when the body needs energy
83
New cards
Most anesthetic drugs rely on liver for metabolism and duration of effect may be prolonged. T/F?
True
* Use lower doses if possible
* Use shorter acting drugs if possible
* Use reversible drugs if possible
Balanced anesthesia
Monitor glucose
Monitor blood pressure and provide oncotic support – (large protein fluids)
* Use lower doses if possible
* Use shorter acting drugs if possible
* Use reversible drugs if possible
Balanced anesthesia
Monitor glucose
Monitor blood pressure and provide oncotic support – (large protein fluids)
84
New cards
GI disease could cause
* Anorexia – loss of appetite for food
* Dehydration – the loss or removal of water
* Hypovolemia – decreased volume of circulating blood in the body
* Acid-base & electrolyte imbalance – when your electrolyte levels are out of balance due to dehydration, you experience acid/base imbalance
* Protein loss – albumin and other protein-rich materials leak into the intestine
* Abdominal pain – multitude of causes
* Dehydration – the loss or removal of water
* Hypovolemia – decreased volume of circulating blood in the body
* Acid-base & electrolyte imbalance – when your electrolyte levels are out of balance due to dehydration, you experience acid/base imbalance
* Protein loss – albumin and other protein-rich materials leak into the intestine
* Abdominal pain – multitude of causes
85
New cards
Anesthetic Management with GI Disease
Correct any imbalances before anesthesia – if possible correct dehydration over 24 hours prior –Does your patient need a blood or plasma transfusion? – run blood gas and correct any issues
Monitor blood pressure – IBP or NIBP
Provide volume or oncotic support (large protein fluid therapy)
Lower anesthetic drug dosage if possible
Monitor blood pressure – IBP or NIBP
Provide volume or oncotic support (large protein fluid therapy)
Lower anesthetic drug dosage if possible
86
New cards
Neoplasia in mouth may cause difficult intubation
Retrograde intubation - nasal
Pharyngeal intubation
Tracheostomy
Pharyngeal intubation
Tracheostomy
87
New cards
Esophageal disease
* Megaesophagus
* Regurgitation and aspiration
* Be fast but patient
* Protect airway – high instance of aspiration
* Suction mouth and esophagus
* Regurgitation and aspiration
* Be fast but patient
* Protect airway – high instance of aspiration
* Suction mouth and esophagus
88
New cards
Upper GI Hemorrhage
Monitor PCV
*
*
89
New cards
The kidneys function in:
* Excretion of metabolic waste and toxins
* Regulation of blood volume and extracellular fluid by controlling sodium and water balance and maintaining extracellular fluid volume homeostasis ( an increase in sodium and water consumption leads to an increase in extracellular fluid volume which in turn increases blood volume - osmolality (measures the body’s water/electrolyte balance) – an increase osmolality of serum can help diagnose dehydration, diabetes, and shock - electrolyte balance (directly related to osmolality)
* Aids in acid-base regulation – kidney’s reabsorb HCO3 from urine back into blood – ultimately balancing pH
* Filtration is related to blood flow although most of the time the kidneys can compensate (autoregulation) for changes in blood pressure. These factors can alter the kidney’s ability to compensate.
* Pain
* Chronic hypertension
* Acute renal failure
* Sepsis
* Regulation of blood volume and extracellular fluid by controlling sodium and water balance and maintaining extracellular fluid volume homeostasis ( an increase in sodium and water consumption leads to an increase in extracellular fluid volume which in turn increases blood volume - osmolality (measures the body’s water/electrolyte balance) – an increase osmolality of serum can help diagnose dehydration, diabetes, and shock - electrolyte balance (directly related to osmolality)
* Aids in acid-base regulation – kidney’s reabsorb HCO3 from urine back into blood – ultimately balancing pH
* Filtration is related to blood flow although most of the time the kidneys can compensate (autoregulation) for changes in blood pressure. These factors can alter the kidney’s ability to compensate.
* Pain
* Chronic hypertension
* Acute renal failure
* Sepsis
90
New cards
Some abnormalities with kidney injury or disease…
* Increased BUN – kidneys aren’t working well – dehydration, urinary obstruction
* Increased Creatinine – same as above
* Increased potassium – hyperkalemia – kidneys remove potassium from the blood, when K+ is too high, kidney’s aren’t working
* Changes in urine output – amount, color, smell
* Metabolic acidosis – decreased HCO3- decreased pH
* Hypertension – because arteries are small, kidney’s aren’t getting enough blood, they react by making a hormone that causes your BP to rise – damaged kidneys do not filter blood well
* Dehydration - kidneys can’t keep body fluids balanced and you become dehydrated
* Nausea/vomiting – due to toxin build up
* Increased Creatinine – same as above
* Increased potassium – hyperkalemia – kidneys remove potassium from the blood, when K+ is too high, kidney’s aren’t working
* Changes in urine output – amount, color, smell
* Metabolic acidosis – decreased HCO3- decreased pH
* Hypertension – because arteries are small, kidney’s aren’t getting enough blood, they react by making a hormone that causes your BP to rise – damaged kidneys do not filter blood well
* Dehydration - kidneys can’t keep body fluids balanced and you become dehydrated
* Nausea/vomiting – due to toxin build up
91
New cards
Anesthetic Management with Renal Disease
Monitor and maintain blood pressure
Monitor and correct acid-base and electrolyte status – ventilation? – HCO3? – iCa? – Na? – K+?
Maintain hydration – BUN? – CREA? – Hypernatremia? – PCV? – TS? – Lactate?
Monitor and correct acid-base and electrolyte status – ventilation? – HCO3? – iCa? – Na? – K+?
Maintain hydration – BUN? – CREA? – Hypernatremia? – PCV? – TS? – Lactate?
92
New cards
Thyroid
* Hypothyroid – hormone imbalance - decreased
* Decrease metabolism – weight gain without an increase in appetite
* Weak muscles – myopathy – weakness – functional limitation – autoimmune – body attacks itself
* Bradycardia – hypothyroidism causes constriction of blood vessels and increased blood pressure which causes a reflex bradycardia
* Hypothermia – due to decrease in metabolism
* Hyperthyroid – hormone imbalance - increased
* Hypertension – increases systolic BP by decreasing systemic vascular resistance, increasing HR and raising cardiac output
* Hyperthermia – increases metabolism
* Cardiac changes (ventricular hypertrophy) – thickening of the wall of the heart’s main pumping chamber – poor pumping action – typically due to high BP
* Decrease metabolism – weight gain without an increase in appetite
* Weak muscles – myopathy – weakness – functional limitation – autoimmune – body attacks itself
* Bradycardia – hypothyroidism causes constriction of blood vessels and increased blood pressure which causes a reflex bradycardia
* Hypothermia – due to decrease in metabolism
* Hyperthyroid – hormone imbalance - increased
* Hypertension – increases systolic BP by decreasing systemic vascular resistance, increasing HR and raising cardiac output
* Hyperthermia – increases metabolism
* Cardiac changes (ventricular hypertrophy) – thickening of the wall of the heart’s main pumping chamber – poor pumping action – typically due to high BP
93
New cards
Hypercoagulability
increased production of clotting factors caused by cushing’s
94
New cards
Pregnancy
Regurgitation & Aspiration
* Cranial displacement of the stomach due to size of uterus
* Decreased esophageal sphincter tone
* Decreased gastric motility
Decreased lung capacity
* Cranial displacement of enlarged uterus
Cardiovascular
* Physiologic anemia
* Increased blood plasma w/o increase in RBC
* Increased cardiac workload
* Increased stroke volume, heart rate and cardiac output
* Blood pressure Regulation
* Increased estrogens decrease SVR
* Weight of uterus can compress caudal vena cava and aorta decreasing venous return and cardiac output
Hypoglycemia
Hypocalcemia
Dehydration
Exhaustion
* Cranial displacement of the stomach due to size of uterus
* Decreased esophageal sphincter tone
* Decreased gastric motility
Decreased lung capacity
* Cranial displacement of enlarged uterus
Cardiovascular
* Physiologic anemia
* Increased blood plasma w/o increase in RBC
* Increased cardiac workload
* Increased stroke volume, heart rate and cardiac output
* Blood pressure Regulation
* Increased estrogens decrease SVR
* Weight of uterus can compress caudal vena cava and aorta decreasing venous return and cardiac output
Hypoglycemia
Hypocalcemia
Dehydration
Exhaustion
95
New cards
Anesthesia Management with Pregnancy
Induce and intubated quickly to protect airway
H2 antagonist (famotidine) and metoclopramide considered preoperatively
Pre-oxygenate and ventilate for patient
Prep patient while she is awake
Left lateral recumbency as much as possible
Monitor glucose and calcium
Maintain normovolemia
Short-acting drugs until neonates are delivered
H2 antagonist (famotidine) and metoclopramide considered preoperatively
Pre-oxygenate and ventilate for patient
Prep patient while she is awake
Left lateral recumbency as much as possible
Monitor glucose and calcium
Maintain normovolemia
Short-acting drugs until neonates are delivered
96
New cards
Newborns
Airway
* Suction mouth
* Stimulate breathing
* Don’t sling/swing puppies
Cardiovascular
* Chest compression \~120bpm
* Epinephrine drop under tongue
Temperature
* Keep warm
* Suction mouth
* Stimulate breathing
* Don’t sling/swing puppies
Cardiovascular
* Chest compression \~120bpm
* Epinephrine drop under tongue
Temperature
* Keep warm
97
New cards
Common Emergencies that require Anesthesia…
C-section
Respiratory Distress
GDV
Sepsis
Hemoabdomen
Respiratory Distress
GDV
Sepsis
Hemoabdomen
98
New cards
What are the elements of a basic triage?
get a complete history
take a physical assessment
* TPR
* Hydration Status
* Auscultation
run bloodwork/diagnostics
* big 4
* Azo stick, glucose, PCV, TS
* ECG
take a physical assessment
* TPR
* Hydration Status
* Auscultation
run bloodwork/diagnostics
* big 4
* Azo stick, glucose, PCV, TS
* ECG
99
New cards
What is the procedure for a C-section?
be considerate when choosing pre-med agents
* almost everything that will effect the mother will also effect the babies
Pre-oxygenation/clipping/prepping
Fast and efficient induction
* Alfaxalone/propofol
* inhalant
* epidural/lineblock
Intra-operative care/support
* Full mu opioid after delivery
* supportive therapy
Post-operative care
* almost everything that will effect the mother will also effect the babies
Pre-oxygenation/clipping/prepping
Fast and efficient induction
* Alfaxalone/propofol
* inhalant
* epidural/lineblock
Intra-operative care/support
* Full mu opioid after delivery
* supportive therapy
Post-operative care
100
New cards
What is the procedure for neonatal care after c-section?
make sure you have all supplies ready
establish a clean airway
stimulate the babies
check to make sure the babies are breathing - have a palpable pulse
Give dopram or epinephrine as a respiratory stimulant under the tongue (1 drop)
oxygen supplementation
once stable:
* dry
* ligate and disinfect the umbilicus
* keep warm until the mother is recovered
establish a clean airway
stimulate the babies
check to make sure the babies are breathing - have a palpable pulse
Give dopram or epinephrine as a respiratory stimulant under the tongue (1 drop)
oxygen supplementation
once stable:
* dry
* ligate and disinfect the umbilicus
* keep warm until the mother is recovered