chapter 11, the human microbiome
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
microbiome
community of microorganisms living in/on the human body, they colonize the human body. They play rules in health digestion, immunity
The microbiome differs by microenvironment and body site.
Pathogens that are in different environments only affect specific parts. (One bacteria can cause troubles in the stomach, but not in the intestine).
Majority is in the gut (gastrointestinal tract) in order to digest food and produce vitamins. This helps support the immune system and its development.
(Microenvironment: immediate, small-scale environment surrounding a particular entity (cell, tissue, organism) and it has distinct physical/ chemical/ biological conditions compared to its broader surroundings. The conditions can influence behavior, survival and function of the organism)
where do microbes come form?
Passage through the birth canal.
Exposure to other humans (and animals)
Ingestion of food and fluids
Inhalation of air-borne microbes
Mostly of early life. Exposing microbes in early life builds up a diverse microbiome (this is good!)
What changes our microbiota?
Everything
Microbiome is not static
ex// diet, lifestyle, settings/ env, change in microbes
Weather: temperature and moisture (in different parts of the country)
Age: children have more varied microbiota
Diet: metabolites = nutrients
Hygiene habits
Health status (& antibiotics). Taking antibiotics frequently is NOT good. The immune system is not as developed
Microbiota: term that refers to the accrual community of microorganisms living in a specific environment (human skin, gut, soil) they are the same bacterial species that colonize the same anatomical sites in all people
Static: the composition and function of microbial communities are dynamic and constantly changing in response to various internal and external factors
host- microbe interactions: (5)
1. Benefits to the microbes
2. Benefits to the host
3. Adaptation (intermicrobe conditions). Competition between microbes
4. Harmful aspects. Competition between microbes
5. Other potential consequences. Abundance of microbes
(1) host- microbe interactions: benefits to microbes
Nutrient availability: host provides continuous source of nutrients (depending where in the body)
Environmental stability: host temperature, solutes, etc are tightly regulated (in human health)
Transportation: host carries and spreads microbes
(2) host- microbe interactions: benefits to host (3)
(1) Microbial antagonism: ways microbes prevent pathogen infection (competition & niches). This minimizes the host susceptibility to pathogens
C diff establishes infection when people are on antibiotics for long periods of time
stool is harvested from a healthy donor and dried out
stool is transplanted into the intestines of the patient with C. Difficile infection
The organisms from the donor sample restores a healthy gut microbiome in the patient
Not very effective
(2) Nutritional synergism: host provides habitat and food/ produce vitamins and nutrients, microbes metabolize things we can’t (indigestible fibres)
mutually beneficial relationship between gut microbiota and the human body where microbes produce essential vitamins and nutrients we cannot make ourselves, break down indigestible fibers into beneficial compounds, enhance absorption of minerals and other nutrients
vitamin K2 produced my e. coli
(3) Immune stimulation: regulate and stimulate immune system
The gut microbe actively communicates with the host immune system playing a crucial role in training immune cells to distinguish friend from foe, preventing excessive inflammation, enhancing pathogen defense. The process is called immune stimulation. Immune modulation.
This allows them to react to pathogens or non- pathogens accordingly
Epithelial cells with receptors:
They have pathogen recognition receptors PRRs that trigger immune response. They are surrounded by mucus
Microbes will produce antimicrobial substances (peptides)
Body will start producing IGA antibodies, they neutralize pathogens if they enter your body
(3) host- microbe interactions: adaptation (intermicrobe conditions, competition between microbes)
microbes adapting to host niches: pH, O2 levels, nutrient availability
(4) host- microbe interactions: harmful aspects. (competition between microbes)
Certain resident microbes can become pathogenic if conditions change. One type of bacterium outgrows the others it establishes infection
Grow to high density
Move to another location in the body (e.g. E. coli in intestine OK... UTI)
Host becomes unhealthy
Opportunistic pathogens
Pathogenic: to microorganisms that can cause disease in a host by invading tissues, producing toxins, triggering harmful immune responses
Opportunistic pathogens: harmless resident microbes that turn pathogenic under specific conditions. Normally would not cause infection, but overgrowth can cause infection
(5) host- microbe interactions: other potential consequences, abundance of microbes
Microbes produce compounds that have local or global effects
Gut-brain axis:
The things produce by microbes can affects brain cell development
Parkinson's, MS, Alzheimer’s, depression, PTSD, anxiety
Growth & Development:
Immunity & allergic disease
The microbiome has massive impacts on our health. Understanding these processes is helpful to maintain health and prevent disease. Microbiome profiling is necessary to figure out which taxa are present
Microbiome profiling: process of identifying and analyzing the microbial communities in a specific environment, the human gut, skin, soil to understand the composition, diversity and function
Microbiome profiling
necessary to figure out which taxa are present
process of identifying and analyzing the microbial communities in a specific environment, the human gut, skin, soil to understand the composition, diversity and function
sequence a part of the DNA from every microbe in the community
DNA sequences tell which species present (or taxonomic groups present)
Amount of DNA from each species tells you the species abundance of the species. See who and what is there
Which part of the DNA is sequenced in microbiome profiling?
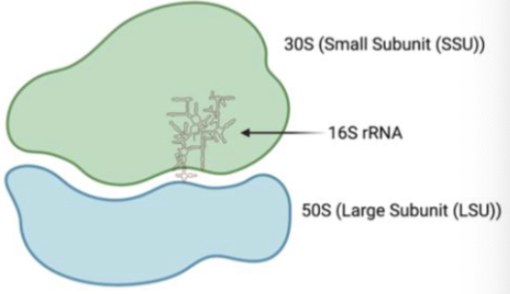
Ideal: 16S rRNA, found in all life forms, sequences change without losing function, changes accumulate very slowly
Bacterial groups have unique 16S rRNA sequences. When you sequence rRNA, we can identify the bacteria present and their relative abundance
16S rRNA: what makes ribosomes
microbial diversities (3)
richness
abundance
phylogenetic distance
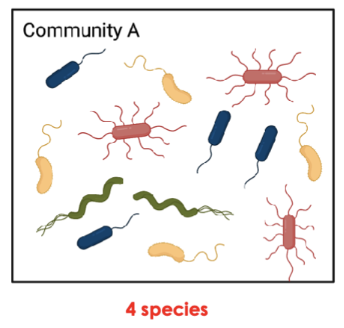
(1) microbial diversities: richness
number of unique species
More species, higher richness, higher diversity

(2) microbial diversities: abundance
prevalence of unique species (inverse of evenness)
High % of one species, high abundance, low evenness, lower diversity
Yellow is more abundant than green species
Opposite: evenness: same repetitive proportion of diff species, even microbial community

(3) microbial diversities: phylogenetic distance
relatedness of species/ distance of diff species on phylogenetic tree
Higher phylogenetic distance, more diversity
Define human microbiome.. What is it and where do you find it?
What factors affect the composition/diversity of your microbiome?
What are some pros and cons of human-microbiome interactions?
What is 16S rRNA and why is it used to study microbiome diversity?
What are some common ways to measure diversity?