all psychopathology and mental health unit 2 exam study flashcards
1/168
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
169 Terms
terms for depression
depression, major depressive disorder (MDD), unipolar depression
DSM-V criteria for a major depressive disorder
must meet at least 5 of the following during the same 2-week period. at least one must be 1) depressed mood or (2) loss of interest or pleasure (anhedonia)
depressed mood most of the day, nearly every day, as indicated by self report of observations made by others — NOTE (in children or adolescents an be irritable mood)
markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day. (a change of more than 5% of body weight in a month)
insomnia or hypersomnia nearly every day
psychomotor agitation or retardation nearly every day (observable by others)
fatigue or loss of energy nearly every day
feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day
diminished ability to think or concentrate, or indecisiveness, nearly every day
recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or suicide attempt or a specific plan for committing suicide
major depressive disorder criteria:
at least one major depressive episode
no manic or unequivocal hypomanic episodes
dysthymic disorder
low level mood for an extended period of time:
depressed mood for at least 2 years
never without these symptoms for more than 2 months within this 2-year period
no major depressive episode during the first 2 years
lifetime prevalence = 3%
lifetime prevalence of dysthymic disorder
3%
premenstrual dysphoric disorder (PMDD) — new DSM-5 diagnosis
for most menstrual cycles over the past year; 5 or more symptoms present during luteal phase that begin to remit following menses
prolonged grief disorder — new DSM-5 diagnosis
continued presence, for at least 12 months after the death of a loved one, of impairing symptoms associated w grief
unspecified mood disorder — new DSM-5 diagnosis
a residual category for presentations of mood symptoms that don’t meet full criteria for any of the disorders in either the bipolar of the depressive disorders diagnostic classes
depression and additional mood disorder specifiers: “with psychotic features”
depression w psychotic features = hallucinations or delusions; mood congruent; only happens during depressive episodes
depression and additional mood disorder specifiers: “chronic major depressive disorder”
depression that does not remit for > 2 years
depression and additional mood disorder specifiers: “seasonal affective disorder”
recurrent episodes with a seasonal pattern
common pattern = when days get shorter / less light —> more depression
depression epidemiology:
lifetime prevalence of MDD = 16-17%
16-17 year olds (adolescents) have the highest rate of MDD
major depression is the leading cause of disability (10%)
age onset = adolescence and young adulthood
earlier onset = more severe
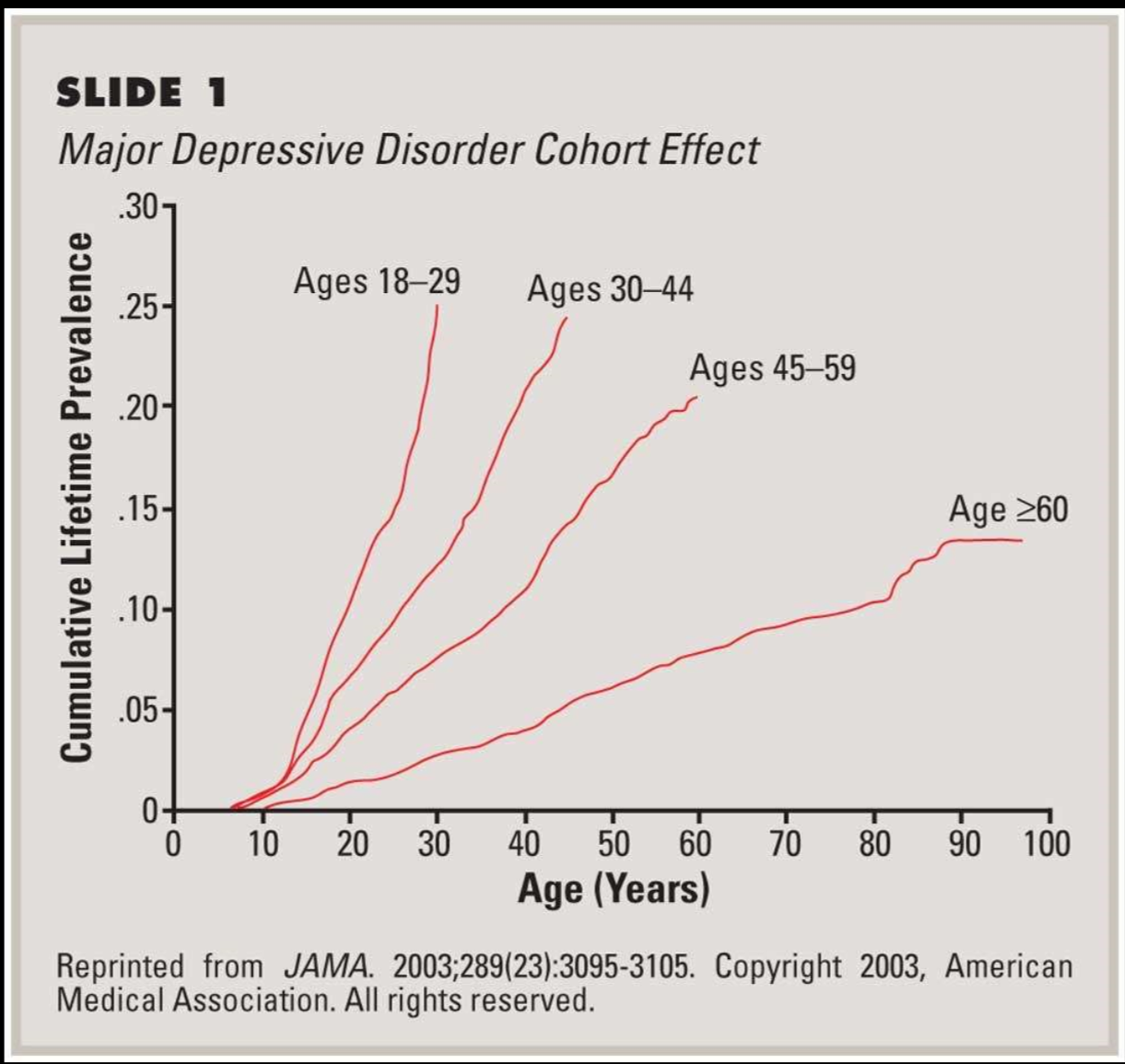
birth cohort trend for depression
prevalence is much higher in recent generations
why? we dont know. maybe awareness, technology, etc?
gender and depression
MDD: 2x as common in women relative to men
why?
women more liekly to present at health clinics, disclose feelings, seek treatment
men more likely to deal w in more externalizing ways (ex alcohol use). women externalize ore
rumination vs distraction
depression across cultures
universal phenomenon, but each culture expresses differently
ex: china and japan: more likely to be described in terms of somatic complaints (sleeping problems, headaches, loss of energy, stomach issues)
depression recovery
remission = period of recovery
full remission = at least 2 months with no significant depressive symptoms
partial remission = some symptoms, but no longer meet full criteria
relapse = return of active symptoms
statistic: 50% recover in 6 months
depression environmental factors
stressful life events
lack of social support
chronic stress
depression biological factors
HPA axis
genetic vulnerability
brain function
neurochemicals
depression psychological factors
information processing bias
cognitive distortions
rumination
personality / temperament
effects of uncontrollable stress on rats — depression study
induces a condition that resembles depression
depletion of: norepinephrine, serotonin, dopamine
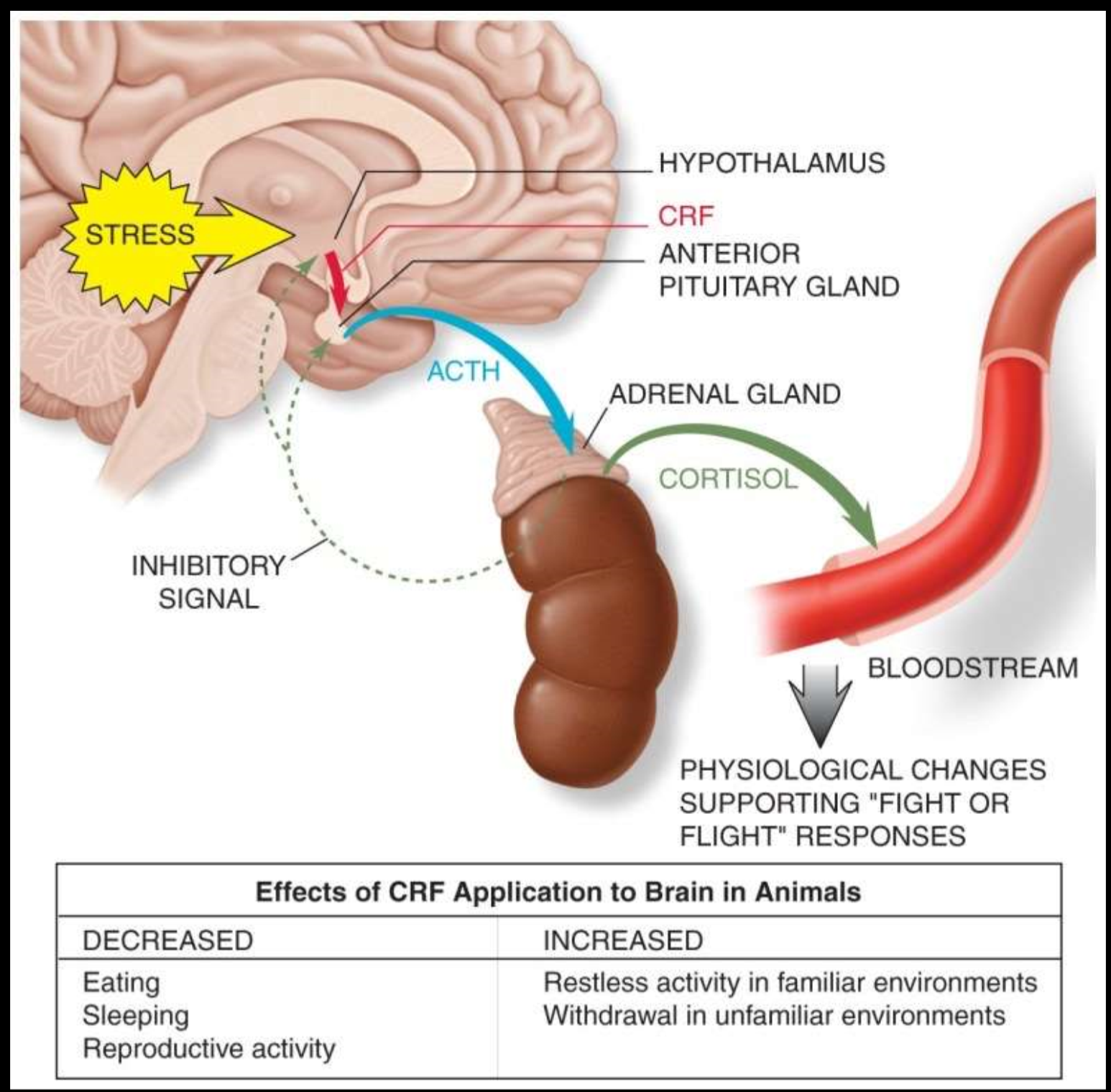
HPA axis: hypothalamic pituitary adrenal axis
individuals with depression: release a lot more CRF (corticotropin releasing factor) from their hypothalamus which stimulates more cotricotropin release form anterior pituitary which stimulates more cortisol release from adrenal cortex.
cortisol released into bloodstream and supports fight or flight responses.
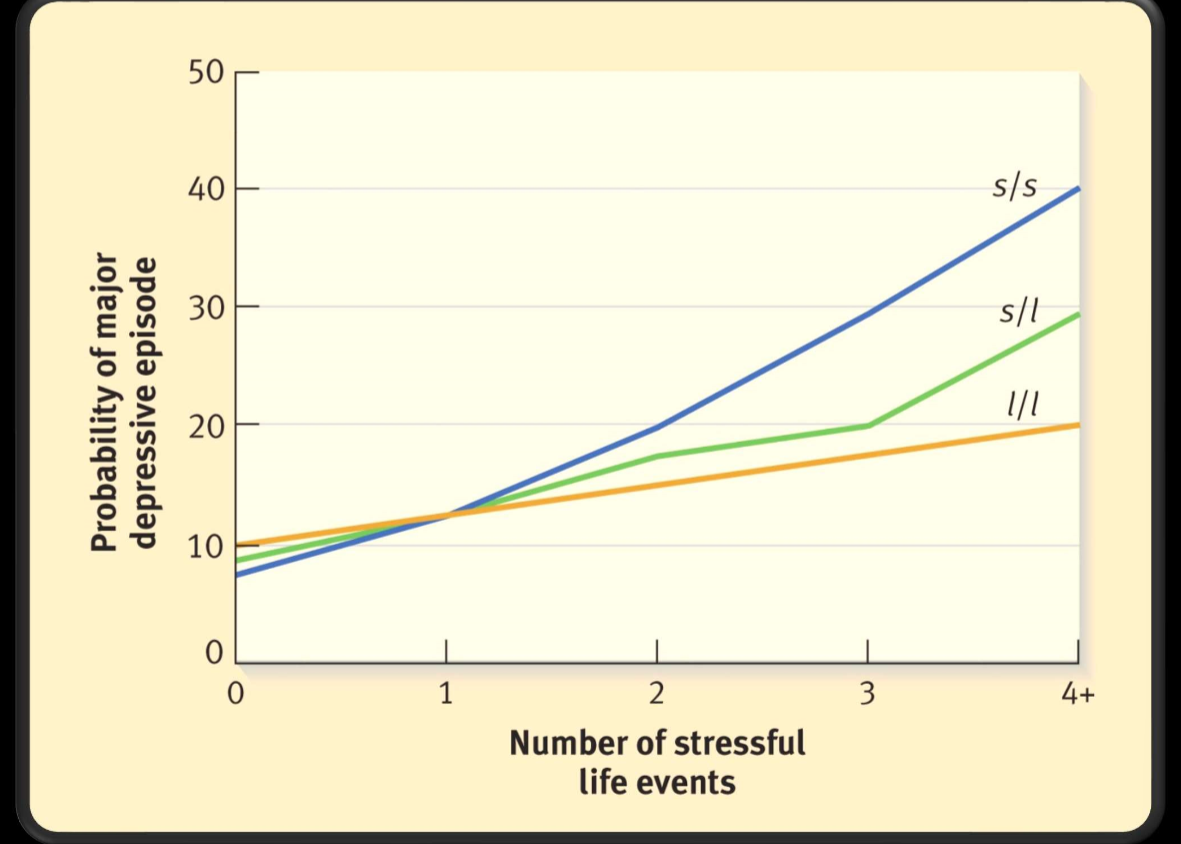
gene x environment interaction in depression
serotonin transporter gene = 5HTTLPR
short (s) allele = associated w increased risk of depression
long (l) allele not associated
homozygous for short allele at greatest risk for depression, especially if experience high stress event
twin studies: 30% increase with severity
1/3 of risk is attributed to genetics
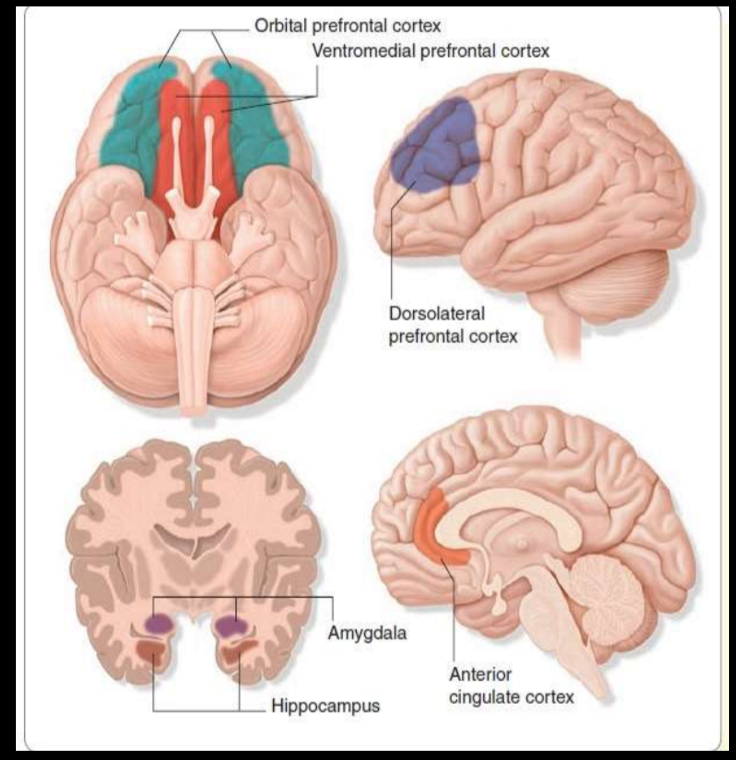
brain regions associated with depression
decreased functioning of:
orbital frontal cortex (OFC): related to reward functioning and how we respond to
ventral striatum: decision making functions and motor control
dorsolateral prefrontal cortex: cognitive control
Anterior cingulate cortex: selective attention
hippocampus (volume): learning and memory
increased functioning of:
amygdala: emotion and threat, fear
depression and reward
depressed individuals reacted less to both penalties and reward stimulus when compared to a normal control group. Shows reward center hypoactivation.
cognitive vulnerability to depression — why some individuals become depressed after stressful life events and some do not
pervasive and persistent negative thoughts about the self
pessimistic view of the environment
these thoughts are activated by the experience of negative life events
becks’ negative cognitive triad
triad of the self, the world, and the future
early negative life experiences —> formation of dysfunctional beliefs —> critical incidents —> beliefs activated —> negative automatic thoughts ←→ symptoms of depression
cognitive distortions (becks negative cognitive triad)
negative attribution style: internal, global, stable way of thinking ab the world; consistently views world in negative way or think that world views u in negative way
negative schemata: tend to view the world negatively and process info in negative ways as a result
rumination
negative automatic thoughts (Beck’s negative cognitive triad)
emerge automatically; rapid duration
not fully conscious
often occur in shorthand
not a result of deliberation, reasoning, or reflection
reflexive
difficult to turn off
validity is accepted without question
often precede a powerful emotion
treatment of depression
cognitive therapy / CBT
interpersonal therapy
behavioral activation treatement (CBT)
antidepressant medication
SSRI
SNRI
MAOI
TCA
alternative treatments
ketamine / psilocybin
deep brain stimulation
electroconvulsive therapy (ECT)
transcranial magnetic stimulation (TMS) — prelim data shows that increasing prefrontal cortex activity can help w depression. however TMS doesn’t reach deep brain structures well like ECT
bright light therapy for SAD — shown to be just as affective as fluoxetine
cognitive therapy for depression
focuses on identifying and replacing self-defeating thoughts with rational statements
deal w current experiences
effective for unipolar depression
interpersonal therapy for depression
focus on current relationships and attempts to improve these relationships via building communication and problem solving skills
idea: improved support system may improve depressive symptoms
behavioral activation treatment for depression
plan positive activities; force individual to get up and go
for indivs. who are severely depressed, just do one thing a week (ex. get out of bed and take a shower)
works very well with meds. not as affective without combination w meds tho.
four classes of antidepressant medication
SSRI: selective serotonin reuptake inhibitor (** current pref method)
SNRI: serotonin and norepinephrine reuptake inhibitor
MAOI: monamine oxidase inhibitors
inhibit enzymes that break down serotonin and norepinephrine
TCA: tricyclic antidepressants
inhibit norepinephrine reuptake (also serotonin tho lesser)
SSRI specifics
positive response: 50% or larger reduction of symptoms
remission: complete and sustained recovery
50% of patients show a pos response following 3-5 wks of treatment
prozac, paxil, zoloft
(also used for anxiety, OCD, bulimia, borderline personality disorder)
issues: nausea, insomnia, sexual problems
suicide relation to mental disorders
vast majority of ppl w mental disorders do not die by suicide
sociodemographic characteristics and stressful life events better predictors of suicide than mental disorders
risk factors: ppl experience crises, violence, abuse, loss, or isolation. also vulnerable groups that experience discrimination; refugees
at least 50% of suicides occur in the context of clinical depression
15-20% of depressed patients eventually commit suicide
many other disorders (schizophrenia, alcoholism) associated w higher suicide risk
active vs passive suicidal ideation
active: “I want to kill myself”
passive: “I don’t want to be alive. It would be better if I wasn’t here”
epidemiology of suicide
suicide rate: 12/100,000
highest completion rate: white men over 50
suicide rate increasing for: adolescents
between 1960 and 1980, completion rate tripled for males 15-24 (doubled for females)
suicide attempts vs completions statistics
in general: attempts to completions ratio = 10:1
among adolescents = 100:1
ages 15-19: females make 3 times as many attempts
male attempts use more lethal/destructive methods
Durkheim’s classifications: the 4 types of suicides
egotistic: individuals feel alienated and lost
altruistic: sacrifice for society (“im a burden, im doing this for others”)
anomic: breakdown of social order (“society is falling apart. this is my reaction”)
fatalistic: unbearable life circumstances (“life is unbearable, this is the only solution”)
Schneidman’s common elements of suicide
purpose: to seek a solution
goal: cessation of consciousness
Cognitive state: ambivalence
Perceptual state: constriction
Interpersonal act: communication of intention
Not always the case, especially for adolescents. Often an impulsive component
Pattern: consistency of lifelong styles
psychosocial factors associated with suicide
impulsivity
one of the main predictors of a suicide attempt. strongly associated w increased attempts compared to ideation
aggression
pessimism
family psychopathology or instability
genetics
sociocultural factors
prevalence of suicidal ideation
24% of high school girls and 15% of high school boys have serious suicidal thoughts
suicidal thoughts especially common amongst depressed adolescents
warning signs for student suicide
depressed and withdrawn
lowered self esteem
deterioration of personal hygiene
loss of interest in studies
communication of distress
students who have completed suicide attempts:
tend to be doing well in school
have low self esteem if academics are involved
have compromised interpersonal relationships
some significant life event / stressor
predictors of suicidal ideation in students: sex specific effects
men and women:
felt depressed and hopeless during the last year
men specifically:
experienced assault in the last year
women:
30 days of alcohol consumption
sexually assaulted
Klonsky’s Framework: From ideation to action (suicide)
two stages of suicide: ideation, attempts
different explanations for the two stages
pain, connectedness, and means
only when your have significant pain, significant loss of connectedness, and the means to do so, do you go from ideation to attempt
most people (~40%) with suicide ideation do not attempt
things that predict ideation do not always predict attempts
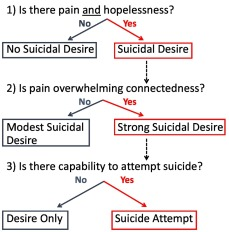
Thomas Joiner’s approach to suicide:
“perceived burdensomeness”
“thwarted belongingness” (social isolation)
acquired ability to inflict lethal self injury
mood disorder
an umbrella term that encompasses unipolar and bipolar disorders
disorders made up of episodes:
depressive episodes
manic episodes
hypomanic episodes
mixed episodes
mood disorders are made up of episodes
depressive episodes
manic episodes
hypomanic episodes
mixed episodes
the manic-depressive spectrum
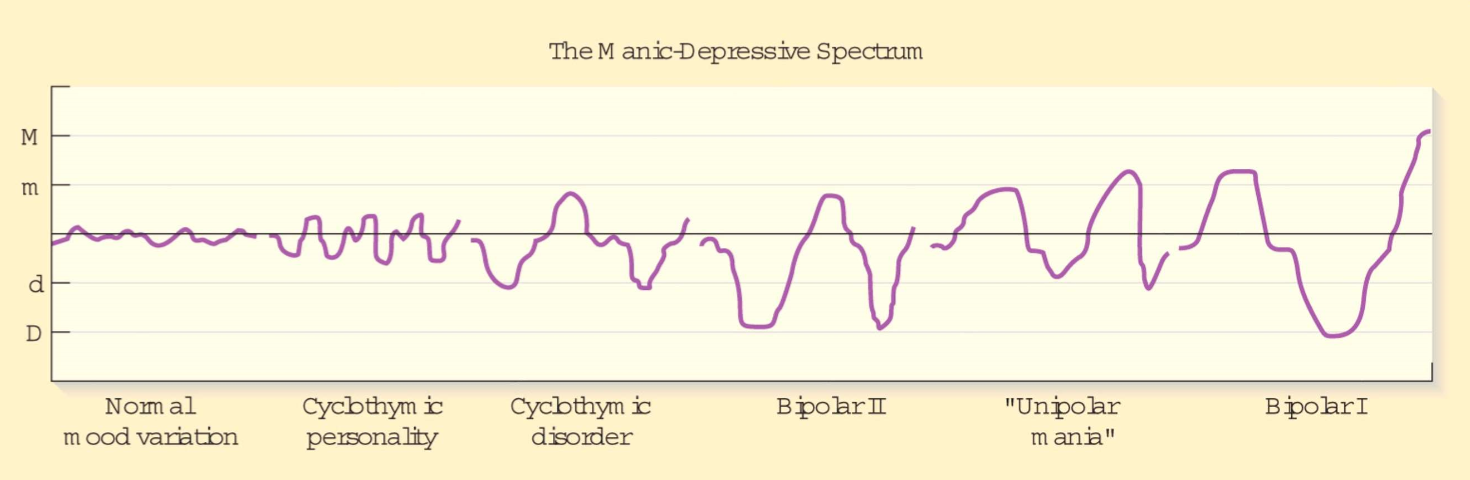
bipolar I criteria
at least one full manic (or mixed) episode
bipolar II criteria
at least one major depressive episode
at least one hypomanic episode
no manic episodes
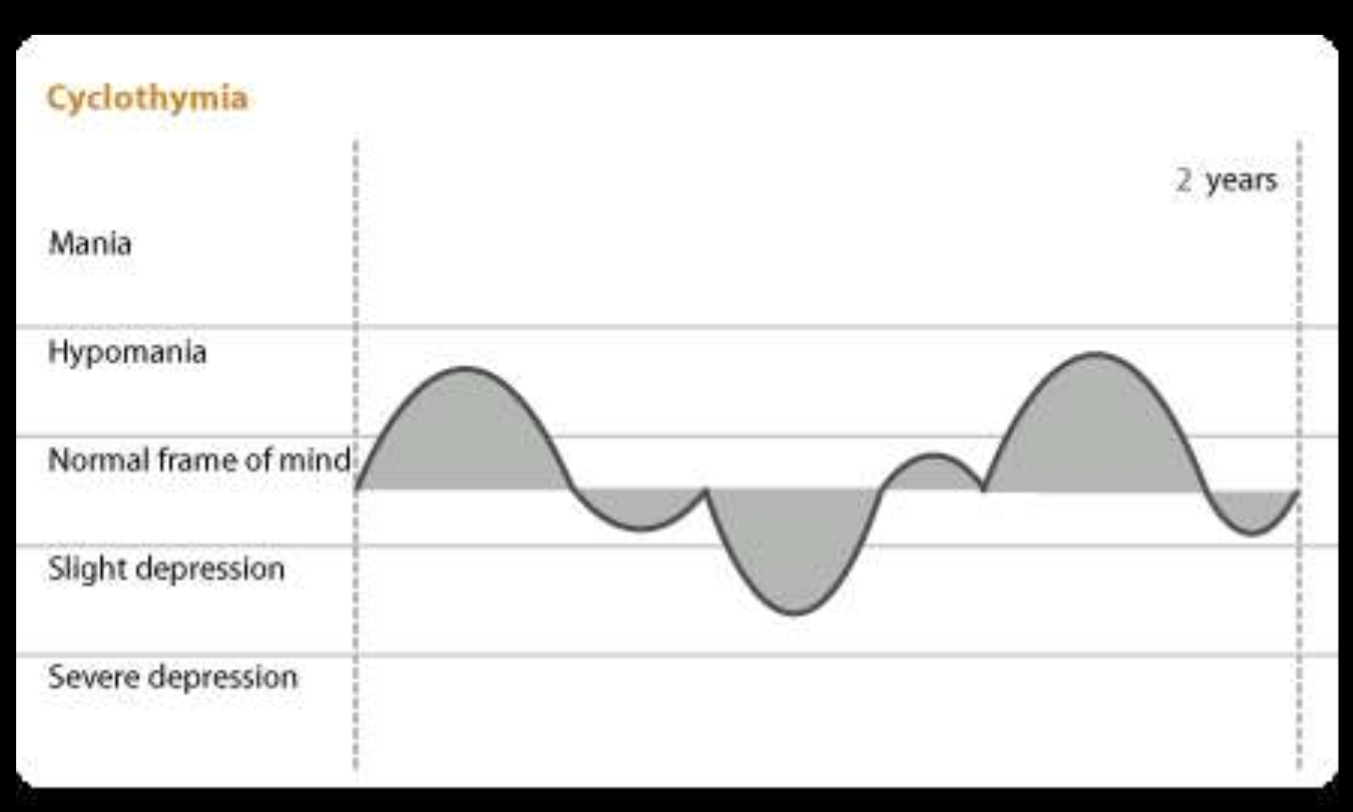
cyclothymia / cyclothymic disordercriteria
no manic or major depressive episodes for at least 2 years
rapid fluctuations in mood, but minor fluctuations (never the extremes of full manic or depressive episode)
lacks severe symptoms and psychotic features of bipolar
much less prevalent
criteria for a manic episode
a period of elevated, expansive, or irritable mood
lasts at least a week
at least 3 of the following: DIG FAST mnemonic
Distractibility
Irresponsibility / irritability — excessive risky pleasure seeking
Grandiosity
Flight of ideas
Activity — goal directed / agitation
Sleep decreased
Talkativeness — disorganized
characterized by significant distress or impairment
often some psychotic symptoms — most often grandiosity
prevalence of mood disorders
depression = 16-17%
dysthymia = ~3%
bipolar = ~4%
bipolar I less prevalent than bipolar II
cyclothymia = ~1%
epidemiology of bipolar disorder
occurs equally btwn males and females
age of onset: 22 years old avg. ( adolescence or young adulthood )
days depressed vs days manic: 3 times as many days are depressed as are manic/hypomanic
unipolar vs bipolar comparison
Unipolar:
Later onset
More prevalent in women
Responds to psychotherapy alone, tricyclic or SSRI antidepressant drugs alone, or combination
Bipolar:
Earlier onset
Equal prevalence among men and women
Responds best to lithium carbonate or other mood stabilizers; does NOT respond to psychotherapy alone
environmental risk factors — bipolar disorder
Stressful life events (HPA axis alteration)
Goal attainment (high)
Schedule disruption
Very important risk factor for relapse.
Lack of sleep -- more unique to manic.
Not only are they sleeping less. During manic episodes, also say that they require less sleep
Also common that prior to the manic episode, they notice they are getting less sleep
biological risk factors — bipolar disorder
Genetic vulnerability
Bipolar is HIGHLY HERITABLE — even moreso than schizophrenia
Brain function
psychological factors — bipolar disorder
cognitive distortions
grandiose thinking
genetics and bipolar disorder
twin studies found bipolar to be highly heritable (High MZ concordance rates)
genome-wide association study (GWAS) finds CACNA1C gene snp associated with bipolar
gene codes for subunit of the L-type calcium channel involved in general action potentials. associated w increased rates of bipolar
brain function associated with bipolar (reward circuitry)
hypoactivation of reward circuit to small gains
hyperactivated amygdala: heightened emotional state → mania
hypoactivated hippocampus and prefrontal cortex: decrease in rational decision making
ppl w mania require more stimulation to get activation of their reward system (Right ventral striatum)
treatment of bipolar disorders
lithium:
effective for mania
40% do NOT improve
side effects that lead to → noncompliance
anticonvulsants:
tegretol, depakene
~50% respond
used for rapid cycling
less severe side effects (gastrointestinal)
psychotherapy:
can supplement medication
NOT effective alone
cognitive therapy
combo of psychotherapy and medication works better than medication alone!!
anxiety disorders
specific phobias
social phobia
panic disorder and agoraphobia
generalized anxiety disorder
OCD and OCD related disorders
fear vs anxiety
fear = a normal, immediate reaction to an environmental stimulus
rxn to real, experienced danger
intensity builds quickly
helps behav responses to threats
anxiety = not as immediate, more of a period of that feeling. can be irrational or unprovoked
anticipation of future problems
general / diffuse emotional reactions
emotional experience is disproportionate to the threat
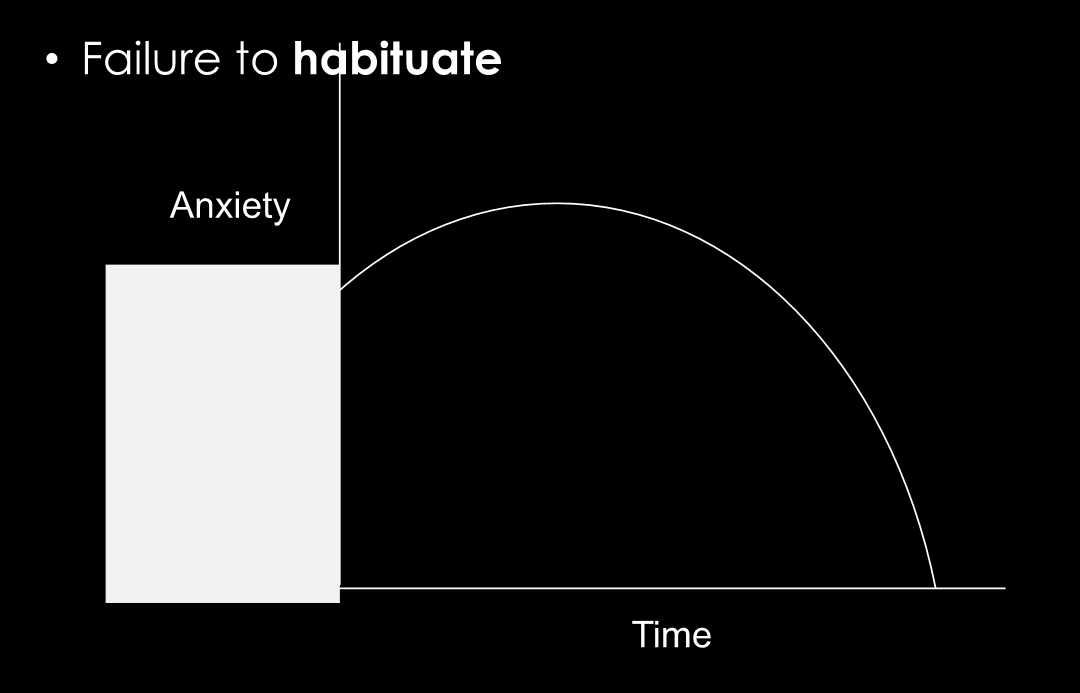
commonality across all anxiety disorders?
failure to habituate: anxious feelings dont go away, person does not get used to situation. anxiety levels stay high even after much time has passed
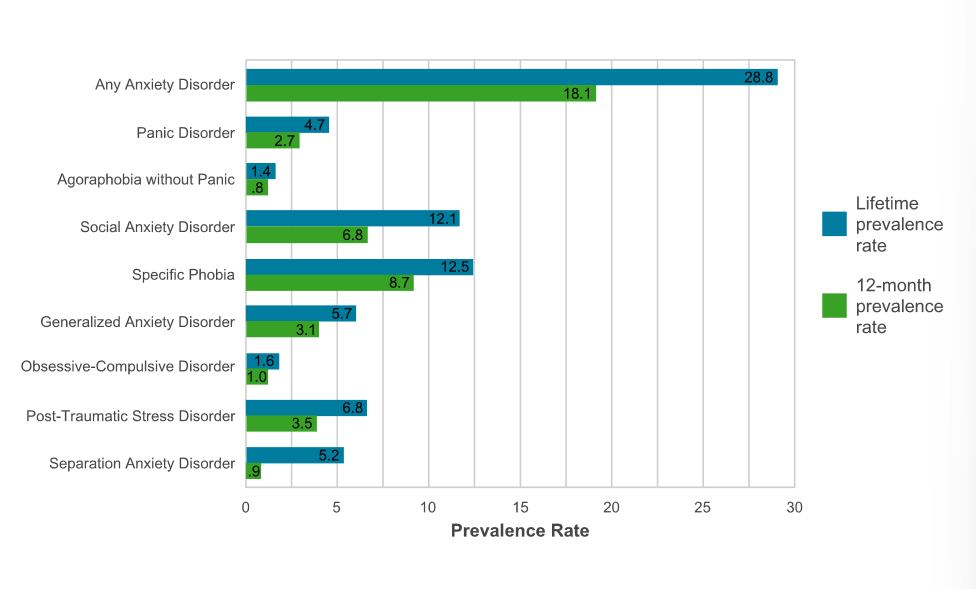
lifetime prevalence of anxiety disorders
any anxiety disorder = 28.8% lifetime prevalence
most common disorders = social anxiety and specific phobia
social factors - anxiety disorders
stressful life events
involving danger, deprivation of resources, insecurity, family, discord
in contrast, depression stressful life events involve LOSS
childhood adversity
abuse, neglect
exposed to more anxiety in parents
caregivers who are more anxious more likely to have kids that are more anxious (not necessarily genetics — behavior modeling)
biological factors — anxiety disorders
genetics: nonspecific for mood and anxiety disorders
cant find lots of specifics. lots of comorbid btwn mood and anxiety disorders
behavioral inhibition temperament
person has a more inhibited temperament
again, not v specific to anxiety
the amygdala — anxiety disorders
amygdala = fear and emotions
increased amygdala activity associated w increased anxiety reaction, especially w specific phobia

the insula — anxiety disorders
connected to autonomic nervous system
critical for interoception: how we interpret our bodily sensations (bodily perception) — some ppl more sensitive/intuitive of these than others
increased activity of this brain region in anxiety
phobia
Persistent, irrational, narrowly defined fears that are associated with a specific object or situation
Characterized by avoidance and reactions that are irrational and unreasonable to the situation/object
types of phobia disorders
specific phobia
social phobia
agoraphobia (**considered under panic disorder bc highly linked)
specific phobia DSM-5 criteria:
marked and persistent fear that is excessive or unreasonable cued by the presence of anticipation of a specific object or situation
exposure tho the phobic stimulus = immediate anxiety response (possible panic attack)
phobic situation is avoided (or endured w intense anxiety and distress)
fear, anxiety, or avoidance is persistent, typically lasts 6 months or more
*avoidance or distress interferes significantly w the persons routine, occupational functioning, or social activities
DSM-5 specific phobia subtypes
animal
natural environment
blood-injection-injury
situational
other
specific phobia epidemiology
very common
lifetime prevalence = 12%
3x more common in women than in men
blood-injection-injury phobia occurs in ab 3-4% of pop
age of onset varies widely typically bc there is some triggering event
etiology of phobias (risk factors)
evolutionary adaptation: phobias may have been adaptive at some point in human history/development
classical conditioning: phobia may be a result of repeated pairing of stimulus
preparedness theory of phobias:
we are biologically prepared for associations / anxious responses
prepared associations learned in one trial and are very difficult to extinguish.
easy to condition fear to fearful objects (snakes, spiders, etc), but more difficult to condition neutral objects.
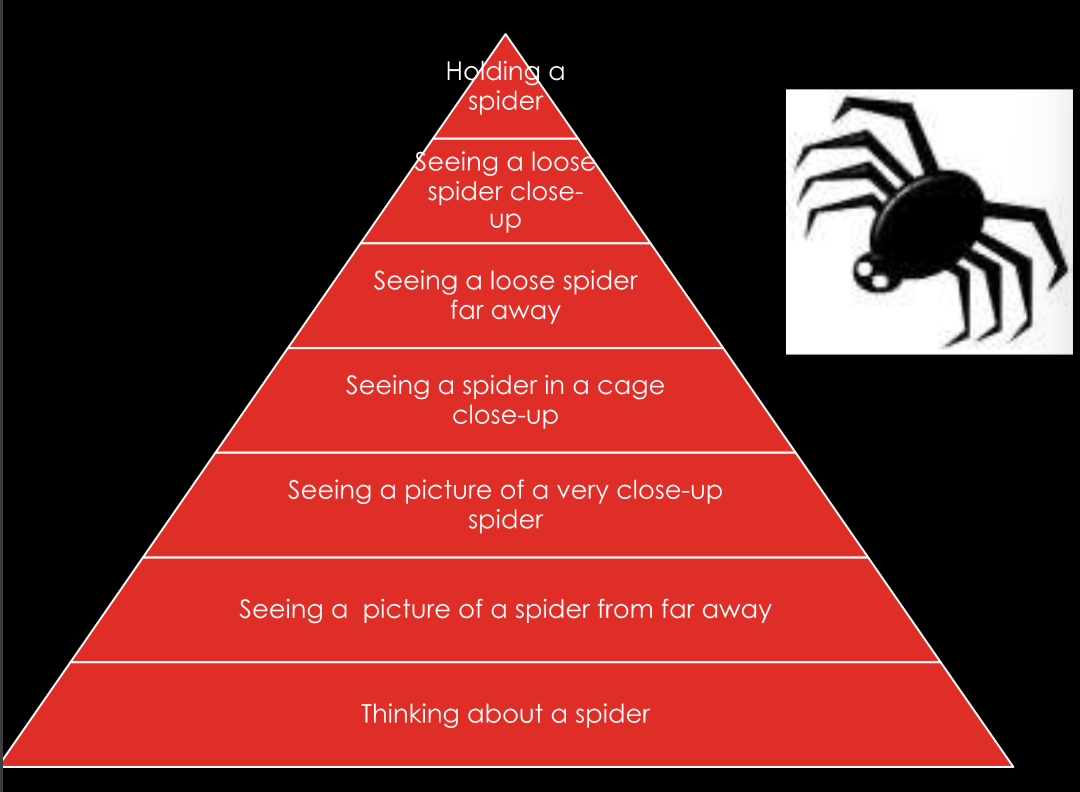
phobia treatments
exposure therapy
may be paired w SSRI or something for the anxiety
many different forms, but often in a fear hierarchy
imagination, observation, virtual reality, viewing, touching, experiencing, etc
Social anxiety disorder (SAD)
level of fear of social situations that leads to impairment
in education, employment, family relationships, marriage/romantic relationships, and friendships
DSM-5 criteria:
marked and persistent fear of one or more social or performance situations
fear of being scrutinized or embarrassing oneself
feared situations are avoided or endured with great distress
fears significantly interfere with funcitoning
subtypes of social anxiety disorder
specific: 1-3 feared situations
most common form is fear of public speaking
ex: eating in public, performing in public, etc
generalized: 4+ feared situations
ex: eating in public, using bathroom, parties, maintaining conversations, meeting strangers, etc
prevalence of Social anxiety disorder
lifetime: 12.1%
12 month prevalence: 6.8%
rates higher in women (15.5%) than men (11%)
early age of onset: childhood to mid-adolescence
high comorbidity w other anxiety disorders, and depression
etiology (risk factors) of Social anxiety disorder
genetic risk:
tendency toward high negative affect or low positive affect (—or—) low extraversion and high neuroticism levels
environmental risk factors:
bullying in childhood — directionality unknown
childhood neglect / abuse
parenting style: maternal overprotection
Cognitive behavioral theory of Social Anxiety Disorder (Rapee and Heimberg)
thoughts = “i’m not good enough”
feelings = sadness and loneliness
behaviors = avoidance of social situations
beliefs: negative self-evaluation; being liked is fundamentally important
behaviors of hyper-vigilance
hyper-vigilance in social anxiety disorder
heightened attention to signs of social threat / cues in the social environment
hyperaware
eye-tracking studies show that ppl w generalized social anxiety disorder are constantly scanning ppls faces a lot more than others
treatment — social anxiety disorder
medication:
SSRI often prescribed need a constant treatment for the anxiety
sometimes benzodiazepines
psychotherapy:
group or individual CBT is most supported
attention bias retraining
cognitive behavioral therapy:
cognitive restructuring
social exposures
fear hierarchy
work up towards higher feared situations
panic attack symptoms
**note: symptoms must peak in 10 minutes
palpitations
sweating
trembling or shaking
sensations of shortness of breath
feeling of choking
chest pain
nausea
dizziness
derealization
fear of losing control
numbness
fear of dying
chills / flushes
relationship between panic attack and panic disorder
first attack frequently follows distress of highly stressful life circumstances
many adults who experience a single panic attack do not develop a panic disorder
20% of college students have attack, but don’t develop disorder
how you respond to the initial attack dictates whether or not one develops the disorder
DSM-5 criteria for panic disorder
recurrent, unexpected panic attacks
sudden, overwhelming experience of terror or fright
more focused than anxiety
“false alarm”
common in other anxiety disorders too
at least one panic attack followed by 1 month (or more) of 1 (or more) of the following
persistent concern about having another attack
worry about the implications of the attack
significant change in behavior related to the attacks
DSM-5 criteria for agoraphobia — highly linked to panic disorder
anxiety about being in situations from which escape might be difficult or in which help might not be available if panic like symptoms develop
hallmark feature: these situations are avoided or else endured with distress
80-90% of diagnoses are female
range of severity associated w disorder
prevalence and course of panic disorders
lifetime prevalence = 3.5% of adult pop
twice as prevalent in females
chronic: 50% recover in 12 years
average age of onset = 23-24 years old
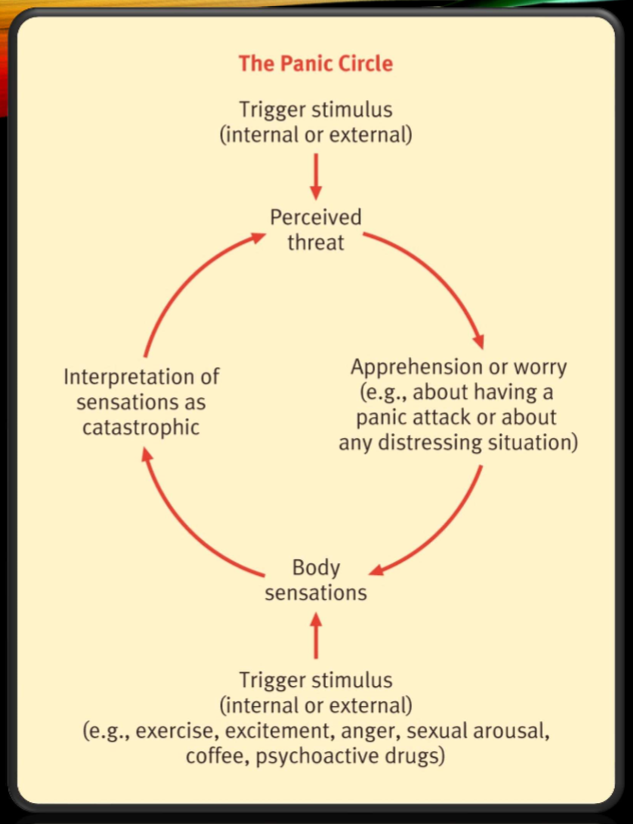
catastrophic misinterpretation — cognitive factors in panic disorder
panic attacks are triggered by internal stimuli
anxious mood leads to physiological sensations
narrowed attention and increased awareness of bodily sensations
person misinterprets bodily sensations as catastrophic event
“fear of fear”
the panic circle — cognitive factors in panic disorder
trigger stimulus → perceived threat → worry → bodily sensations → interpretation of sensations as catastrophic → go thru circle again
panic disorder treatment
85% of ppl w panic disorders show up repeatedly at emergency rooms
interoceptive exposure therapy: helps u revisit those feared internal stimuli that u experience in a panic attack —- (exposure to feared bodily sensations associated w panic)
cognitive therapy: target catastrophic automatic thoughts
psychoeducation
with treatment, 70-90% recover
** benzodiazepines make relapse more frequent :(
General anxiety disorder DSM-5 criteria
excessive anxiety and worry (apprehensive expectation) occurring more-days-than-not for at least 6 months, about a number of events or activities
person finds it difficult to control the worry
the anxiety and worry are associated with 3 or more of the following 6 symptoms (with at least some symptoms present for more-days-than-not for the past 6 months)
restlessness or feeling keyed up / on edge
being easily fatigued
difficulty concentrating or mind going blank
irritability
muscle tension
sleep disturbance (difficulty falling or staying asleep, or restless unsatisfying sleep)
causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
GAD vs MDD — differential diagnosis
must have evidence that GAD exists outside of depressed episodes
differential must be made, bc these two disorders are highly comorbid
GAD-specific symptoms (vs MDD)
worry
cognitive biases
intolerance of uncertainty (difficulty w ambiguous and uncertain possiblilities)
GABA / benzodiazepine receptor dysfunction
worry vs GAD
worry:
uncontrollable
negative emotional thoughts
concerned with possible future threats or dangers
usually verbal rather than visually expressed
when it becomes GAD:
frequency
control
range of topics
valence (how extreme it is)
prevalence and comorbidity of GAD
lifetime prevalence = 5.7%
age of onset: 31-33
GAD and MDD correlate 0.59-0.70 ——> high correlation
Tri-Partite model of mood and anxiety disorders
relates mood and anxiety disorders to broad underlying traits of positive and negative affect as well as autonomic arousal
negative affect (mood and anxiety)
positive affect (MDD only)
physiological hyper-arousal (anxiety specific)
GAD etiology:
cognitive = “intolerance of uncertainty”
difficulty with ambiguous and uncertain possibilities
biological:
GABA / benzodiazepine receptor dysfunction
treatments for GAD
medications:
SSRIs
benzodiazepines — effective but rarely prescribed bc side effects and addictiveness
CBT: new treatments that target avoidance of emotion:
self-monitoring
interpersonal and emotional processing therapy
antecedent cognitive reappraisal
target cognitive biases (overestimate likelihood of negative events and underestimate ability to cope)
mindfulness-based CBT for GAD
emotion regulation therapy
emotional awareness training — prevention of emotional avoidance
staying in present moment, stop behavioral avoidance, engage w emotions as they come