OPT 311 Large Pupils
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What are some etiologies with the muscle (non-neurological) causing a large pupil?
posterior synechiae
ocular trauma
angle closure glaucoma = also vomiting, cornea edema
What are some etiologies with the NMJ causing a large pupil?
parasympatholytic drops like tropicamide = inhibits constriction = fixed to light
sympathomimetic drops like phenylephrine = promotes dilation = still some constriction
Jimson weed alkaloid ingested = causes atropine intoxication = "corn pickers pupil"
denervation supersensitivity

Recall that with a fixed, dilated pupil, we can differentiate whether it's an afferent or efferent problem using which test?
indirect APD test results being either...
(+) APD means afferent problem
(-) APD means efferent problem
What is denervation supersensitivity causing a large pupil?
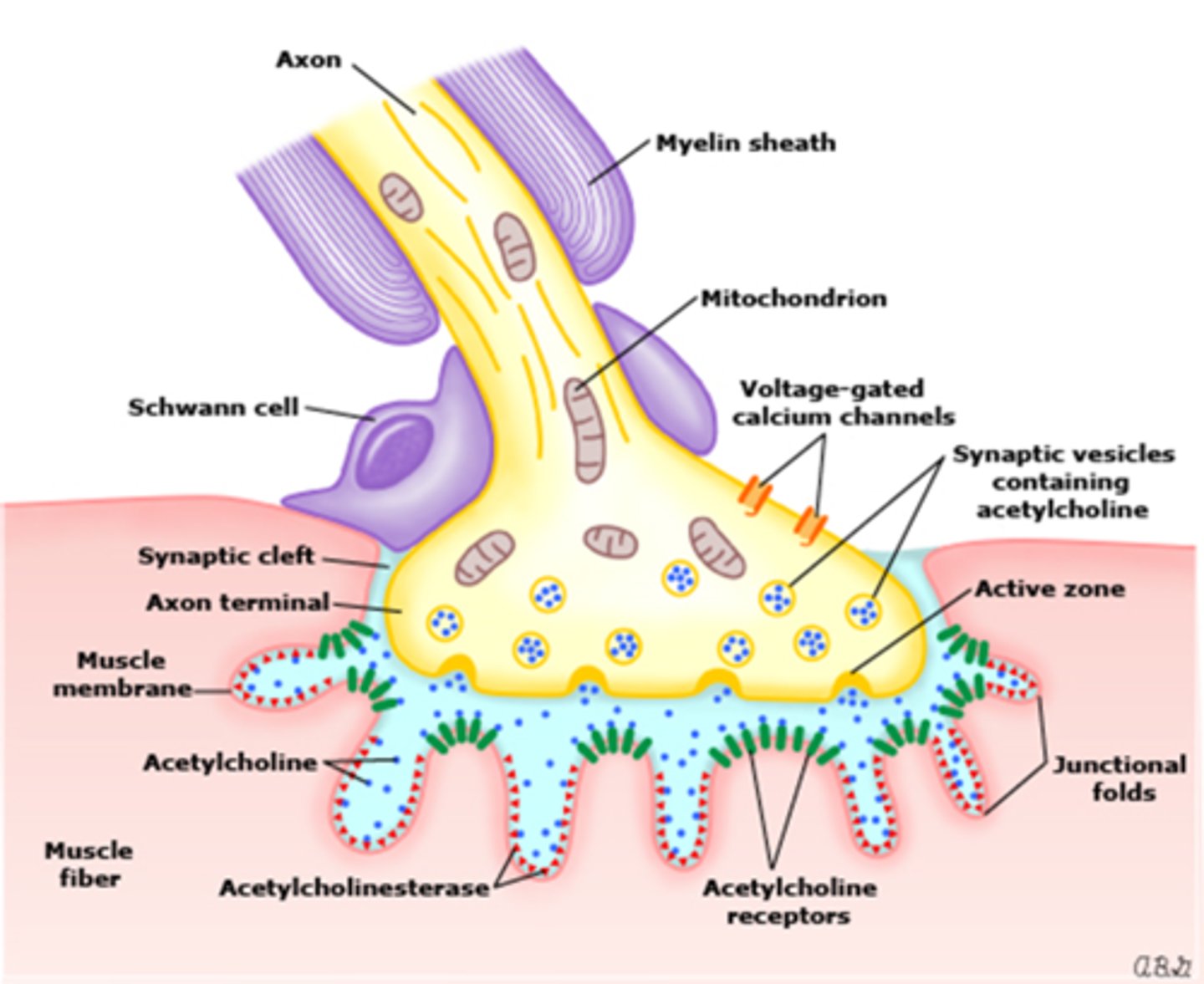
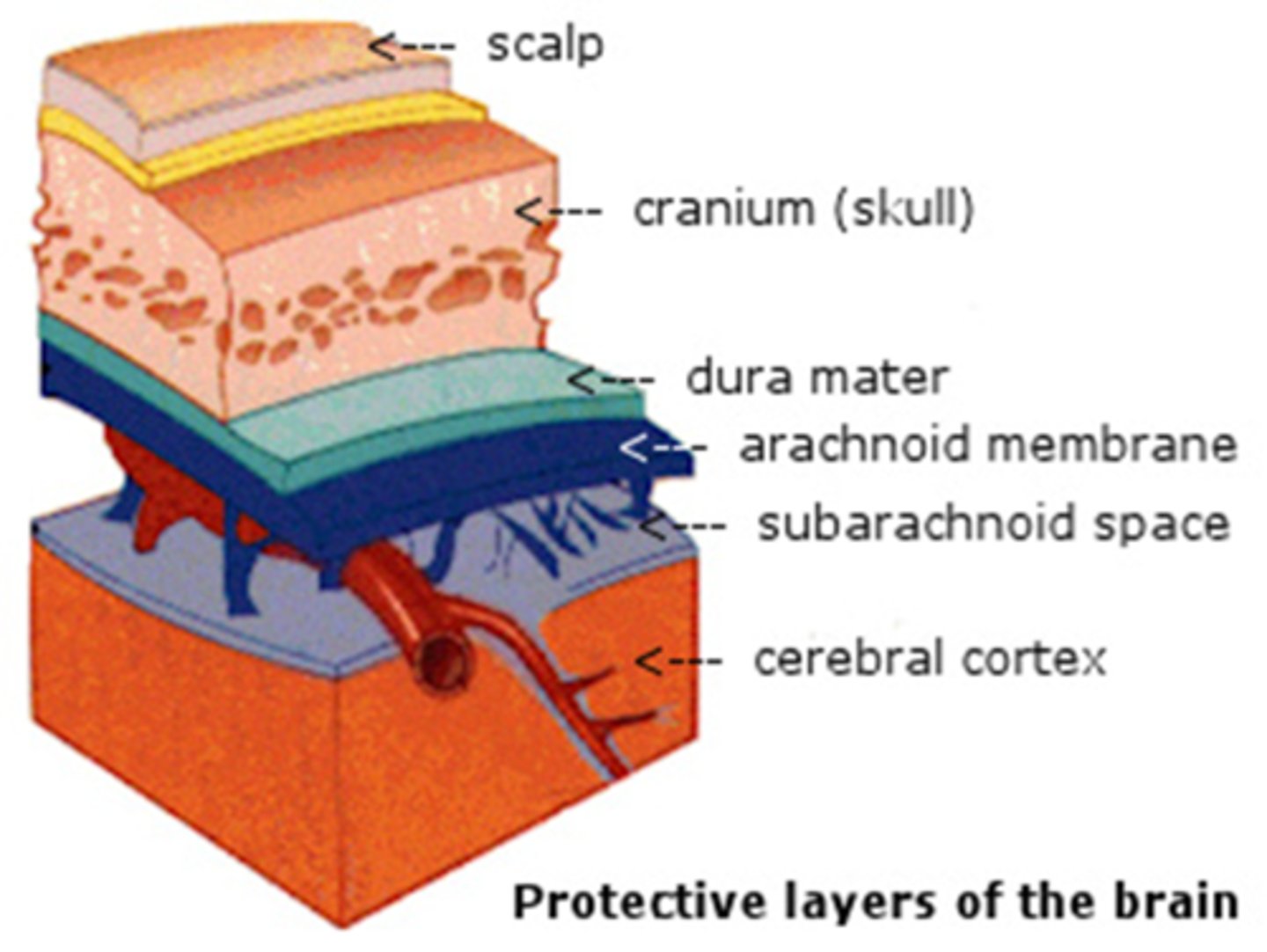
defect in parasymp fibers that travel with CN III = reduced ACh released at NMJ = sphincter mm does not receive ACh stimulation = sphincter mm becomes super-sensitive to low [ ] of any ACh-like neurotransmitter
![<p>defect in parasymp fibers that travel with CN III = reduced ACh released at NMJ = sphincter mm does not receive ACh stimulation = sphincter mm becomes super-sensitive to low [ ] of any ACh-like neurotransmitter</p>](https://knowt-user-attachments.s3.amazonaws.com/abddf32b-a71a-4ce8-9de5-0cce2f5f8e46.jpg)
Denervation supersensitivity of the iris sphincter mm is the basis for which test?
pilocarpine 0.125% test OU
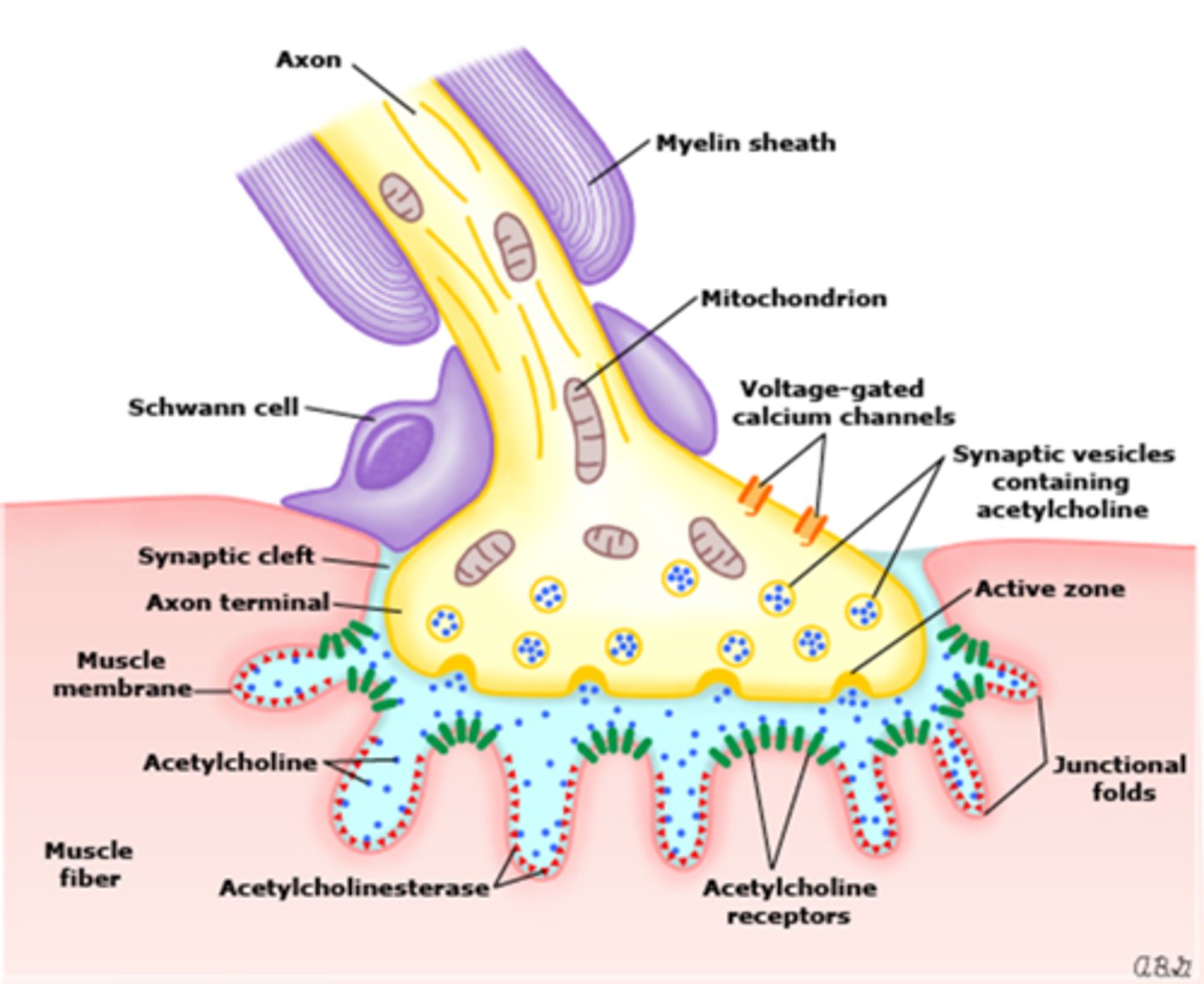
How does a normal eye respond to the 0.125% pilocarpine test?
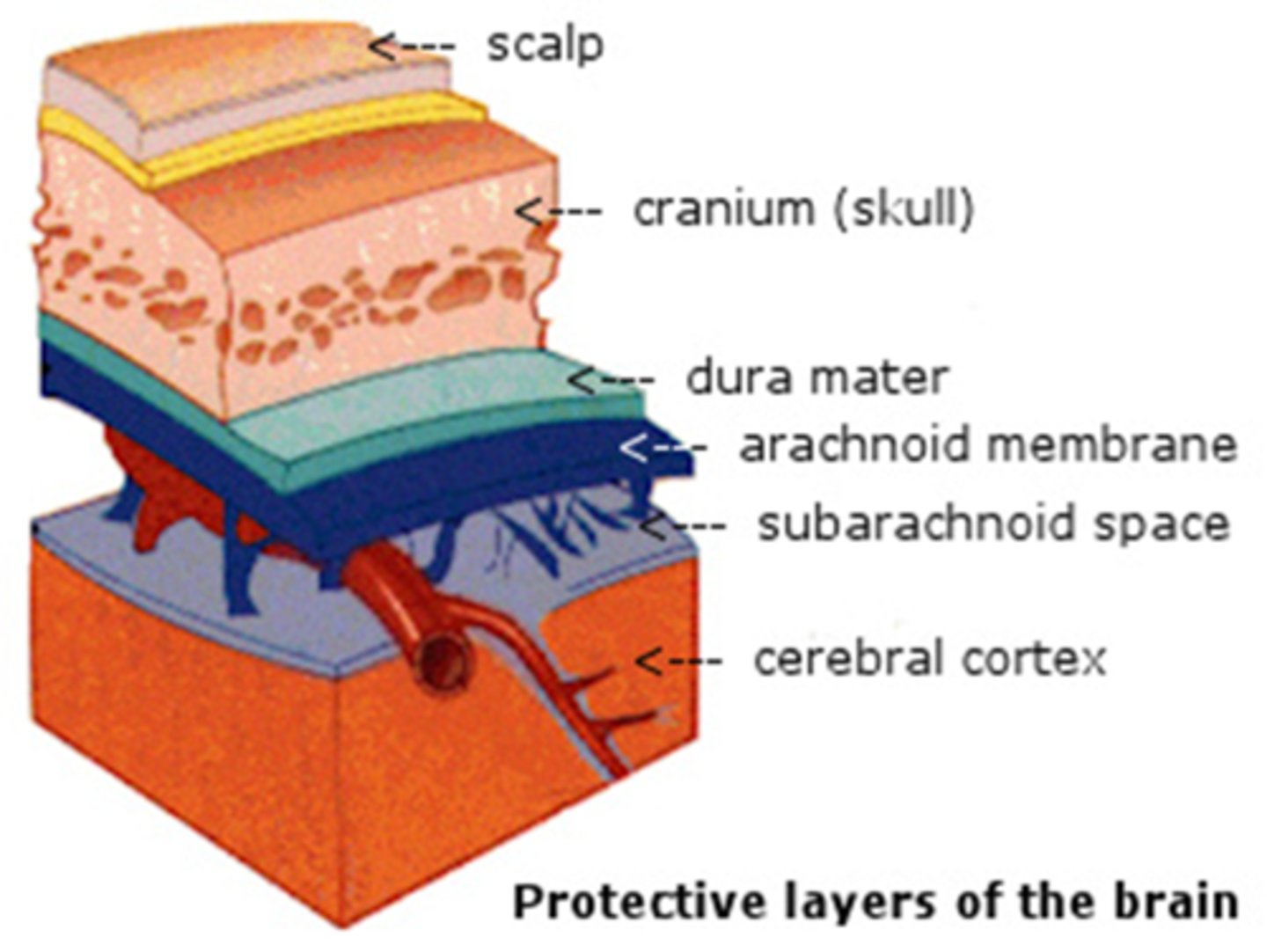
lots of ACh being released at NMJ = sphincter mm stimulated by a normal amount of ACh = sphincter mm will NOT respond to low [ ] of ACh
![<p>lots of ACh being released at NMJ = sphincter mm stimulated by a normal amount of ACh = sphincter mm will NOT respond to low [ ] of ACh</p>](https://knowt-user-attachments.s3.amazonaws.com/e25150e9-fcc5-4928-9cd1-15791573faca.jpg)
How does a pharmacologically dilated eye respond to the 0.125% pilocarpine test?
ACh receptors blocked = adding ACh-like drops such as pilocarpine will NOT induce constriction of the sphincter mm
When is it typically okay to put pharmacological testing drops in the pt's eye when presenting with a large pupil?
as long as you have R/O a CN III palsy
Ex) A 38-year old woman presents with a severe HA, a fixed, dilated pupil for 2 days, no ptosis, alignment in primary gaze, and no ASeg inflam. What tests should you do? Can you do pharmacological testing?
indirect APD test to confirm no afferent problem with CN II
eyelid function to confirm no ptosis
EOM to confirm no palsy
ask about chemicals that could have entered the eyes
pharmacolgoical supersensitivity test would be okay to do
Ex) A 72-year old man presents with a fixed, dilated pupil noted this morning, RUL ptosis, ocular misaligment in primary gaze, and no ASeg inflam. What tests should you do? Can you do pharmacological testing?
ask about pain/diplopia
indirect APD test to confirm no afferent problem with CN II
eyelid function to confirm no ptosis
EOM to confirm no palsy
screen other CN
pharmacolgoical supersensitivity test would NOT be okay to do

Ex) A 19-year old woman presents with a large pupil OS that has a sluggish direct response. OS pupil is larger in light and smaller in dim light. There is no ptosis, eyes are aligned, and no signs of ASeg inflam. What tests should you do? Can you do pharmacological testing?
indirect APD test to confirm no afferent problem with CN II
eyelid function to confirm no ptosis
EOM to confirm no palsy
iris motility observed with SLE
deep tendon reflexes
ask if always present, accom issues
pharmacolgoical supersensitivity test would be okay to do

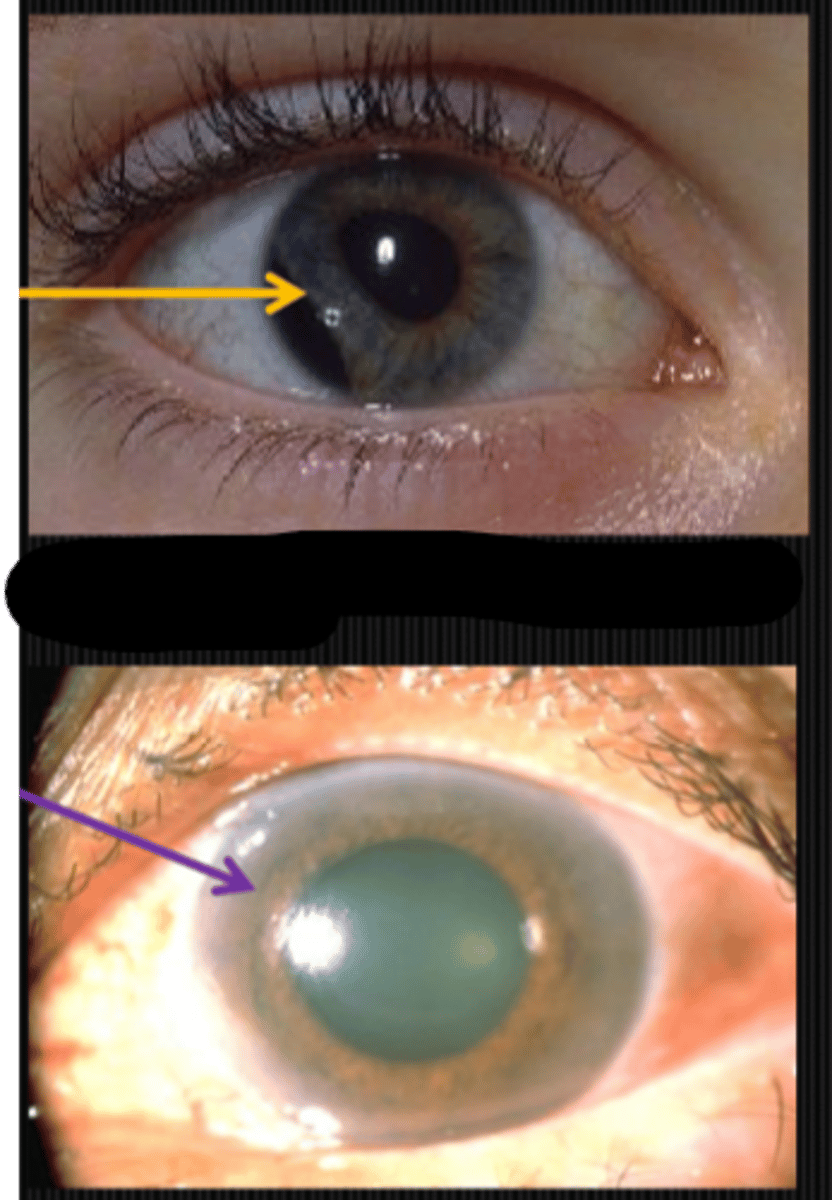
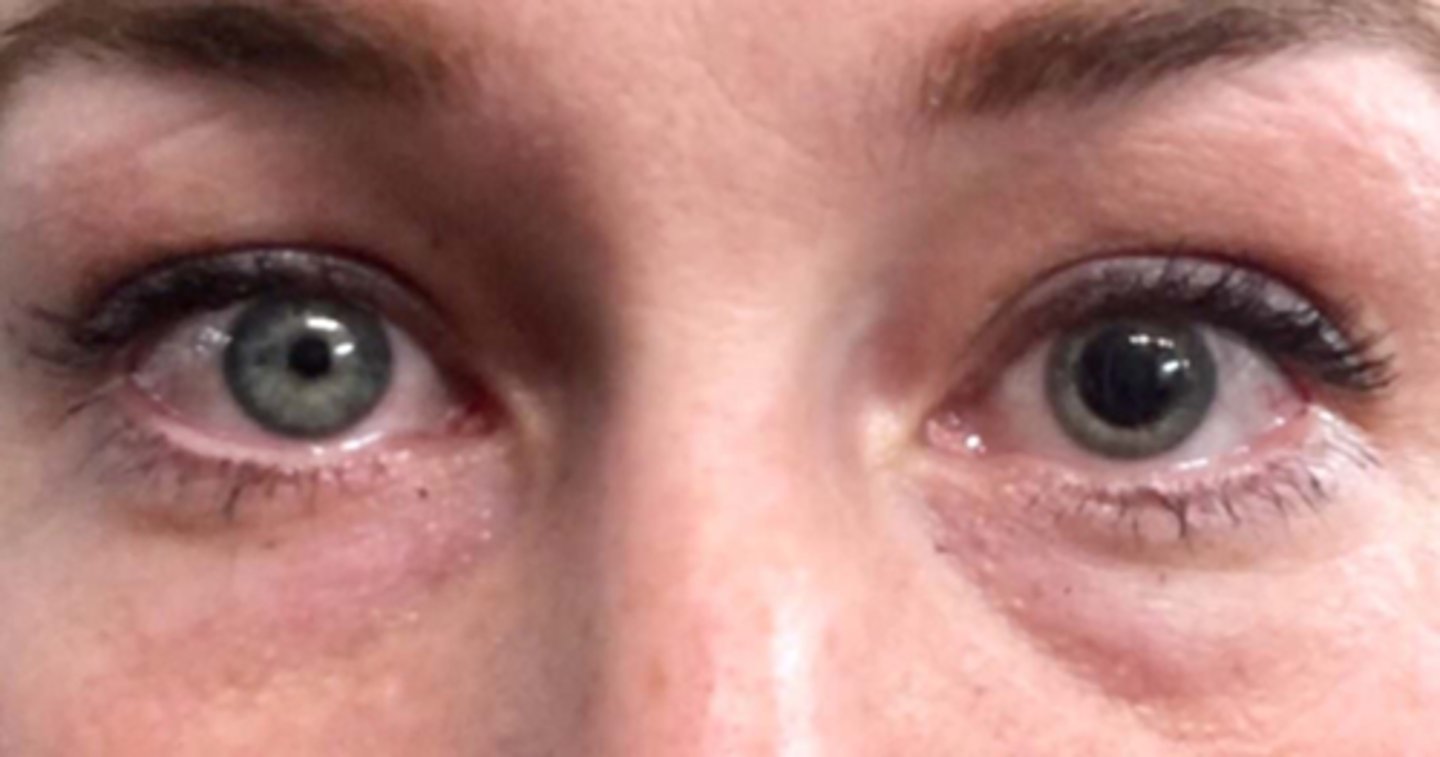
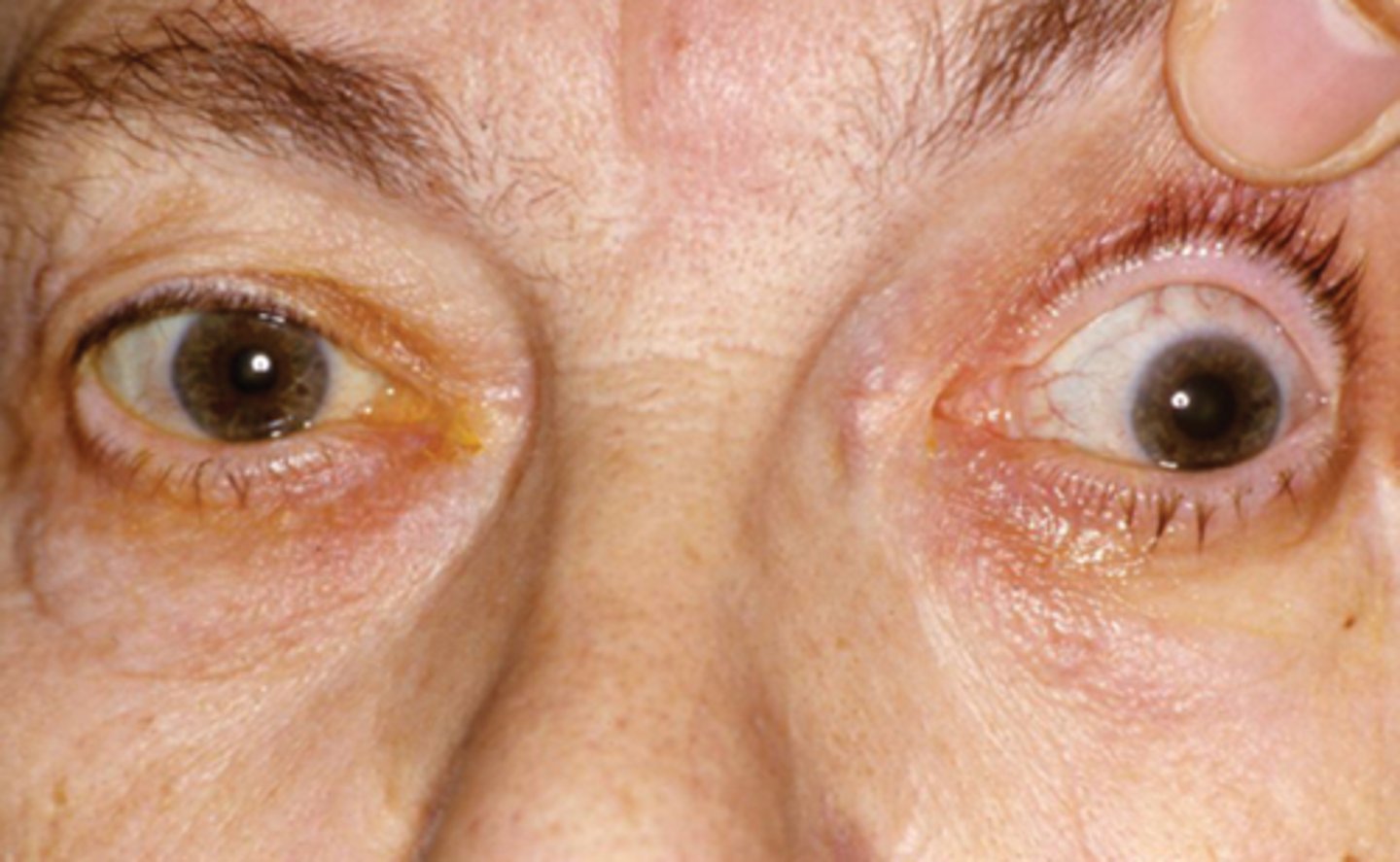
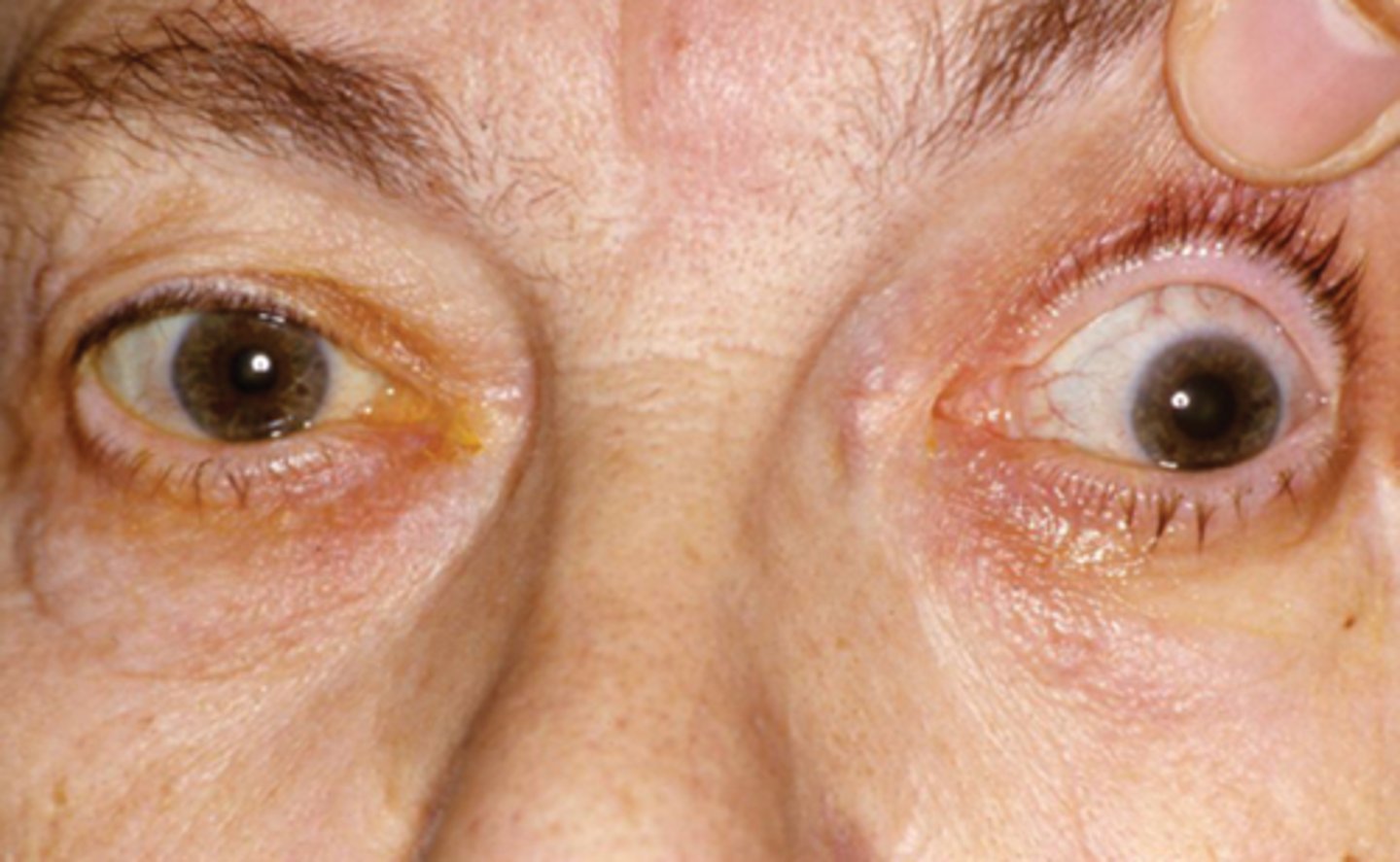
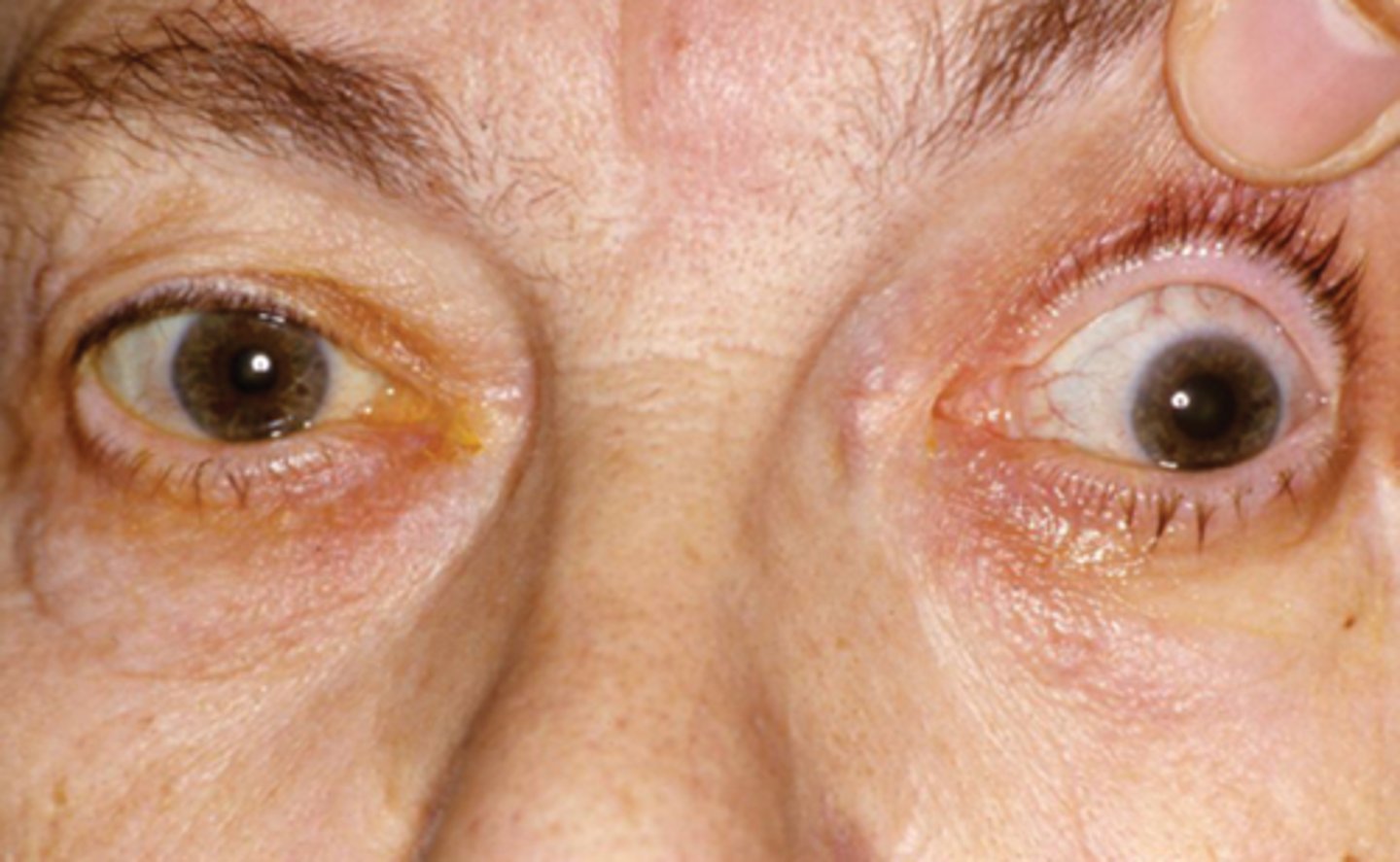
What 1/3 etiology with the nerve causing a large pupil is shown here?
tadpole pupil = sympathic irritation/spasm of iris dilator with unknown etiology = dilator pulls on sectoral area of pupil for 1-2 weeks
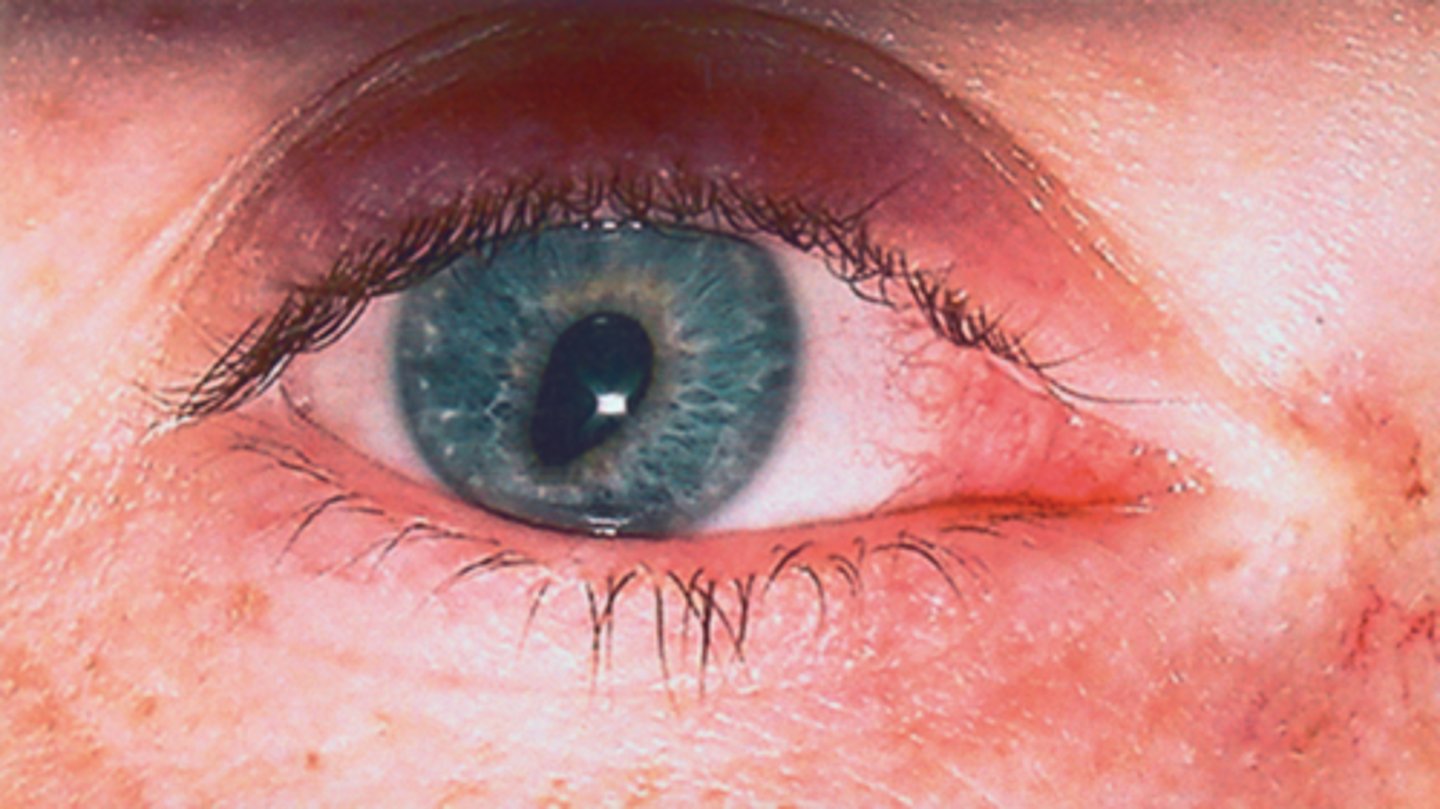
What 2/3 etiology with the nerve causing a large pupil is shown here?
tonic pupil (see tonic pupil Quizlet set)
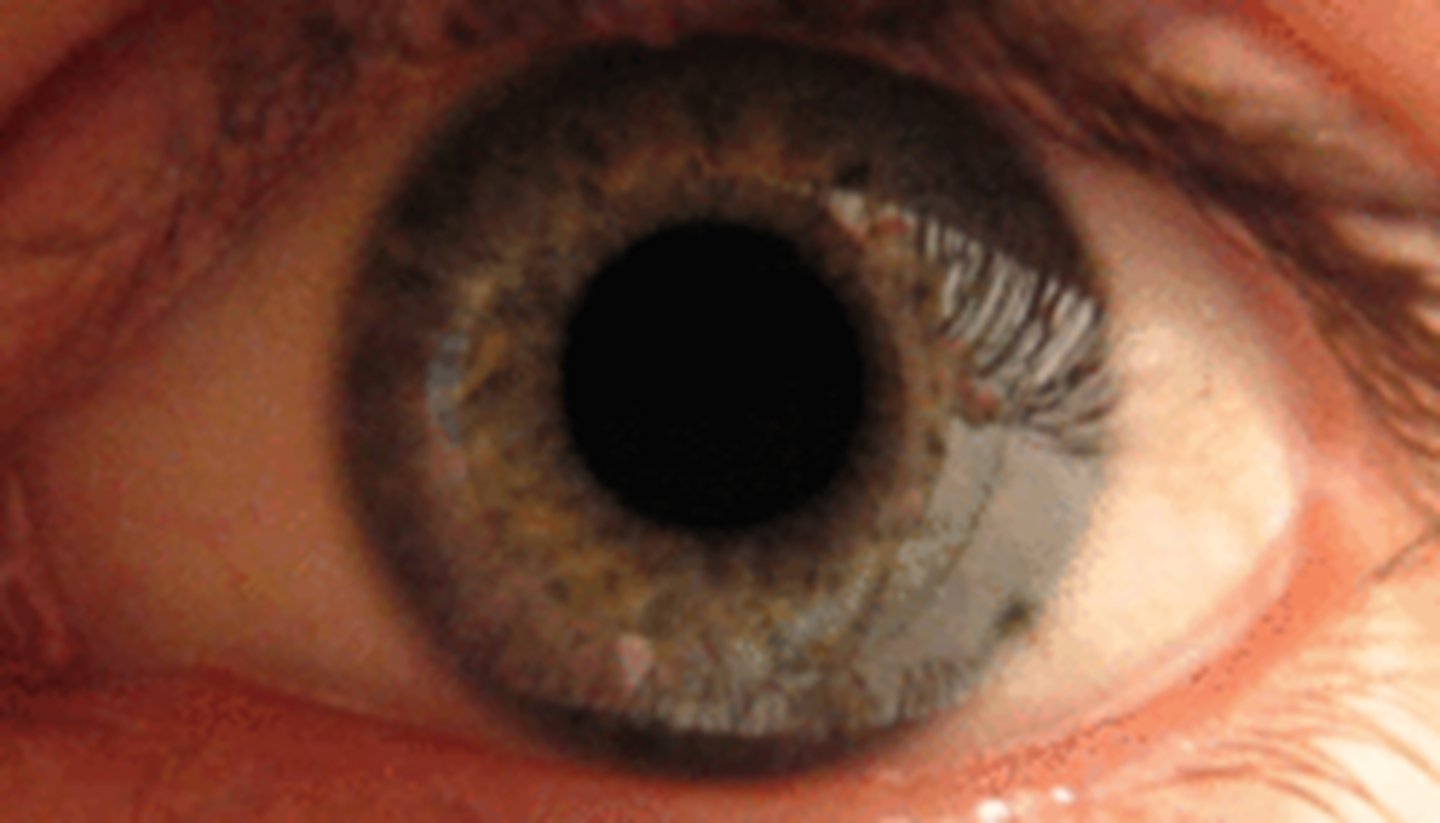
What 3/3 etiology with the nerve causing a large pupil is shown here?
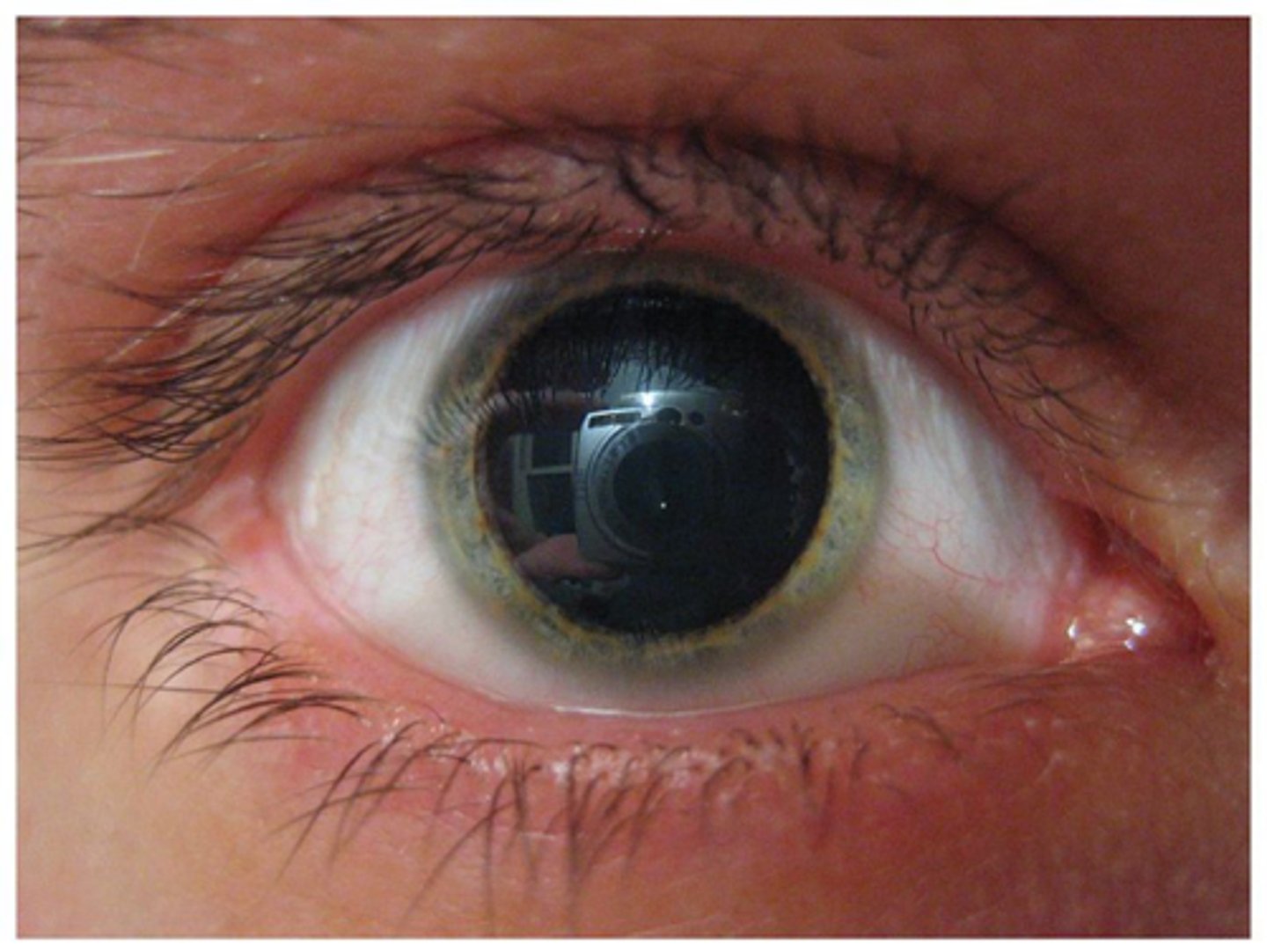
CN III palsy = parasymp issue
What is meant by an isolated CN III palsy?
ONLY affecting CN III and not affecting any other CN (need to do a CN screening exam to R/O other CN issues)
What is meant by a complete CN III palsy? 2 factors.
complete CN III palsy = pupil involved, total ptosis
incomplete CN III palsy = pupil spared, partial ptosis
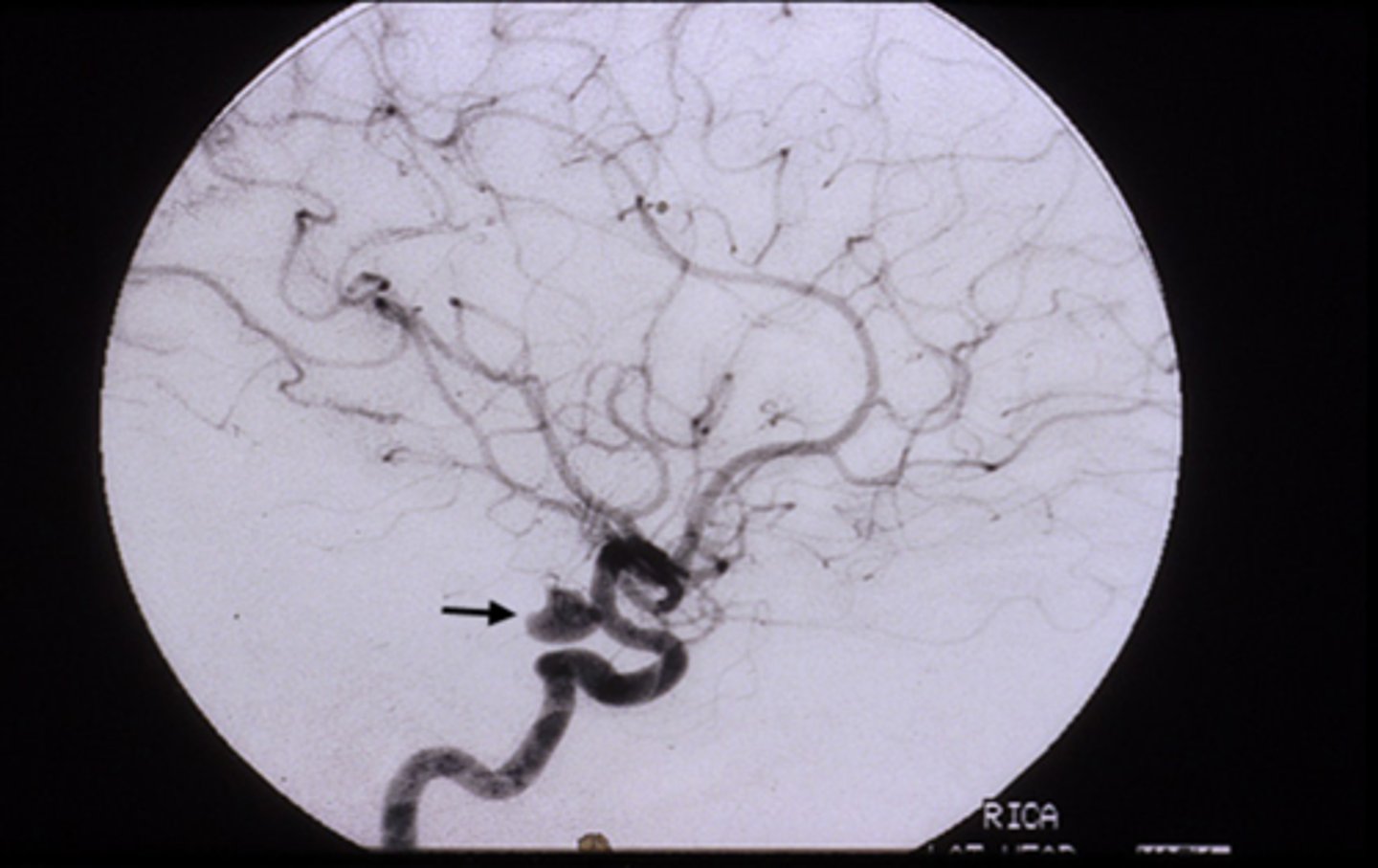
What is the difference between the cause of an isolated pupil-involved vs pupil-sparing CN III palsy?
fixed, dilated pupil (esp if painful like HA) = anuerysm at the junction of the ICA and posterior communicating artery
pupil-sparing (may or may not be painful like eye pain) = diabetes or ischemic vascular etiology
NOTE: can change from pupil-sparing to pupil-involved if it is an aneurysm
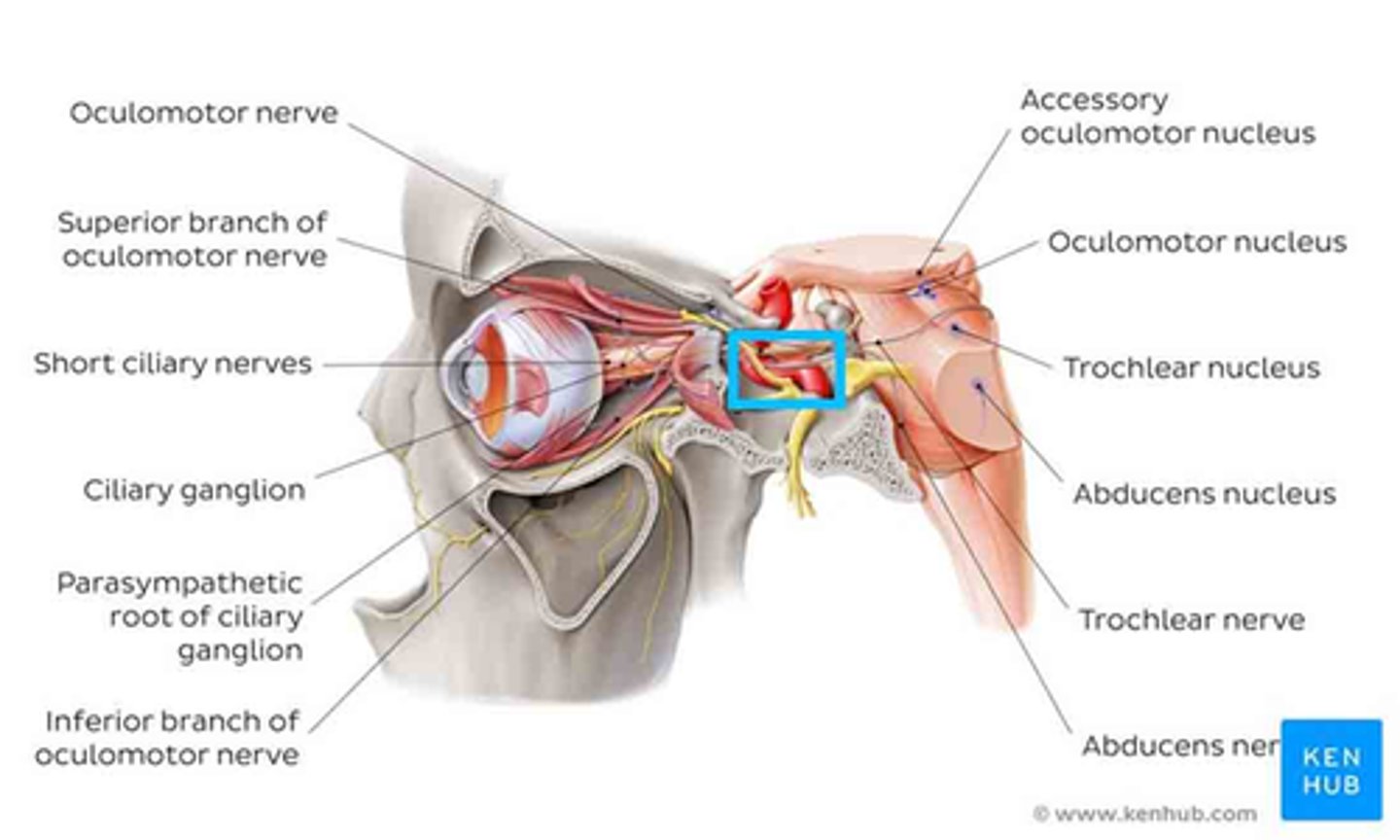
Explain the anatomy of the pupillomotor vs EOM fibers in the CN III.
pupillomotor fibers travel around the circumference of CN III
EOM fibers travel within the core of CN III
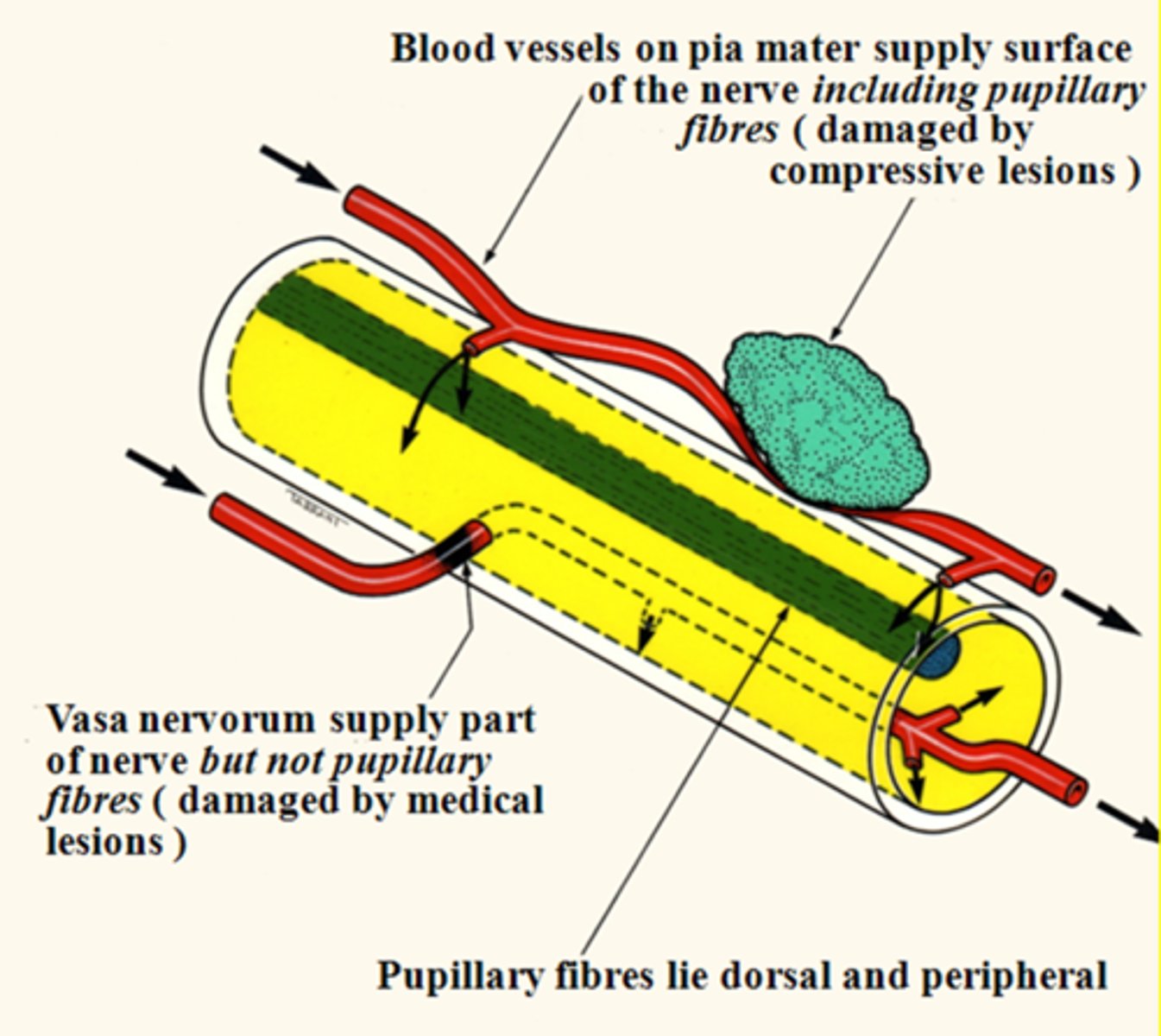
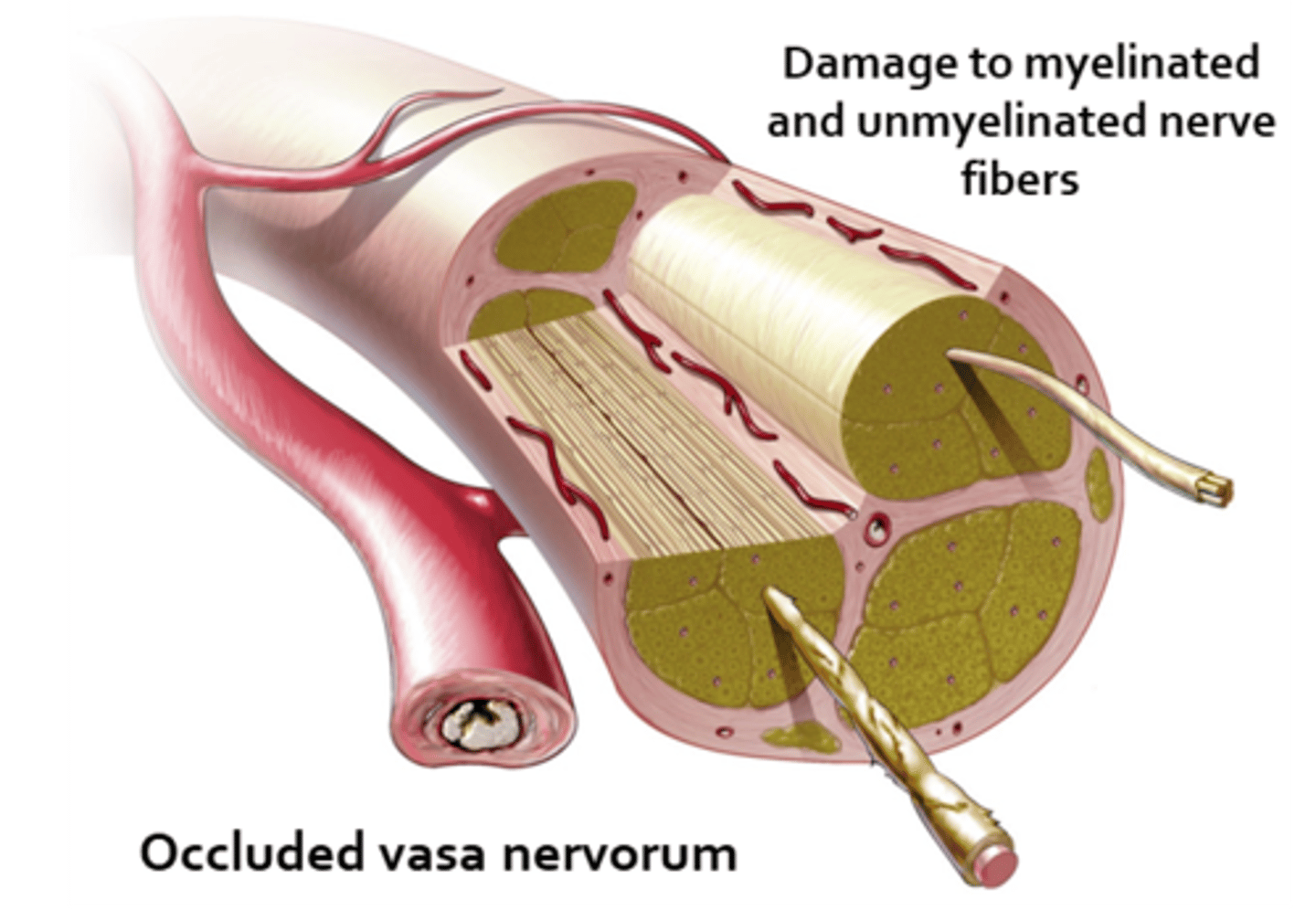
Why are most pupil-spared CN III palsies the result of DM or vascular etiologies?
vasa nervorum occlusion = infarcation of these small BV = focal areas of demyelination in the nerve core, while the outer pupillomotor fibers are spared
Where is the most likely location of the lesion in a CN III palsy (eye is down and out, ptosis) with a pupil that is larger in bright light, smaller in dim light?
cavernous sinus bc this is where the parasymp, symp, and CN III fibers are close together
BRAINSTEM PROBLEMS causing large pupils
BRAINSTEM PROBLEMS causing large pupils
What is Uncal syndrome?
fast expanding mass, hemorrhage, tumor = increased ICP = brainstem compression and herniation down into foramen magnum (fatal!) = fixed, dilated pupil
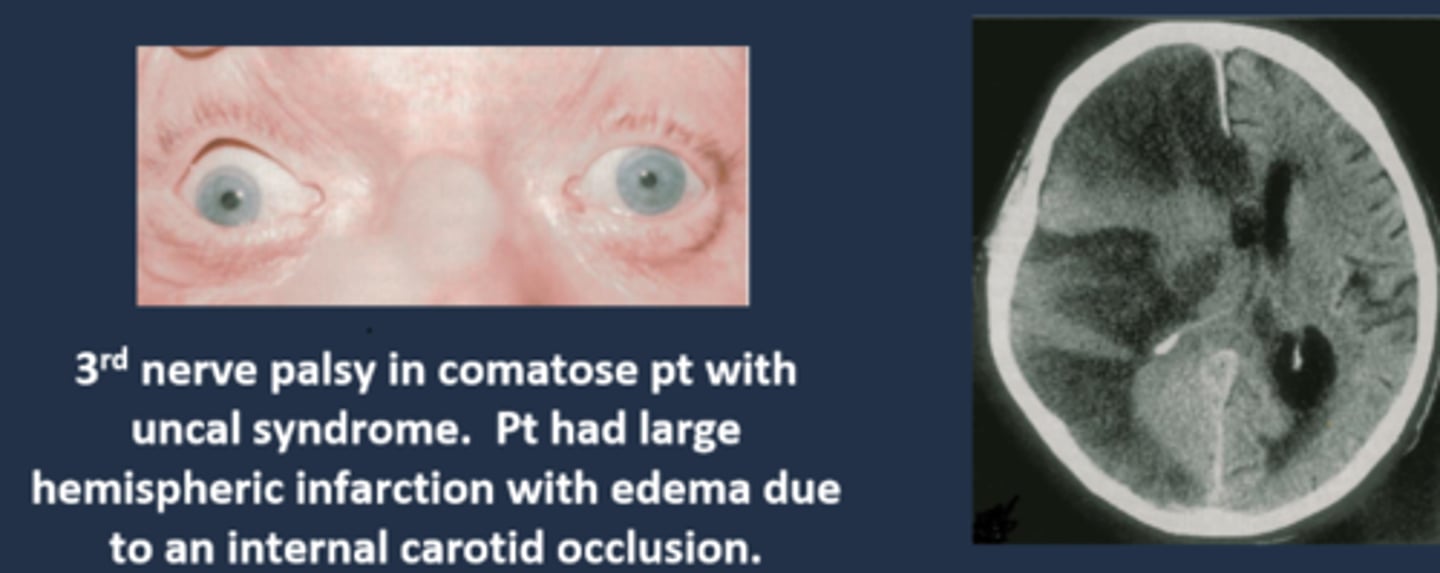
What do we call the fixed, dilated pupil seen in Uncal syndrome?
Hutchinson pupil
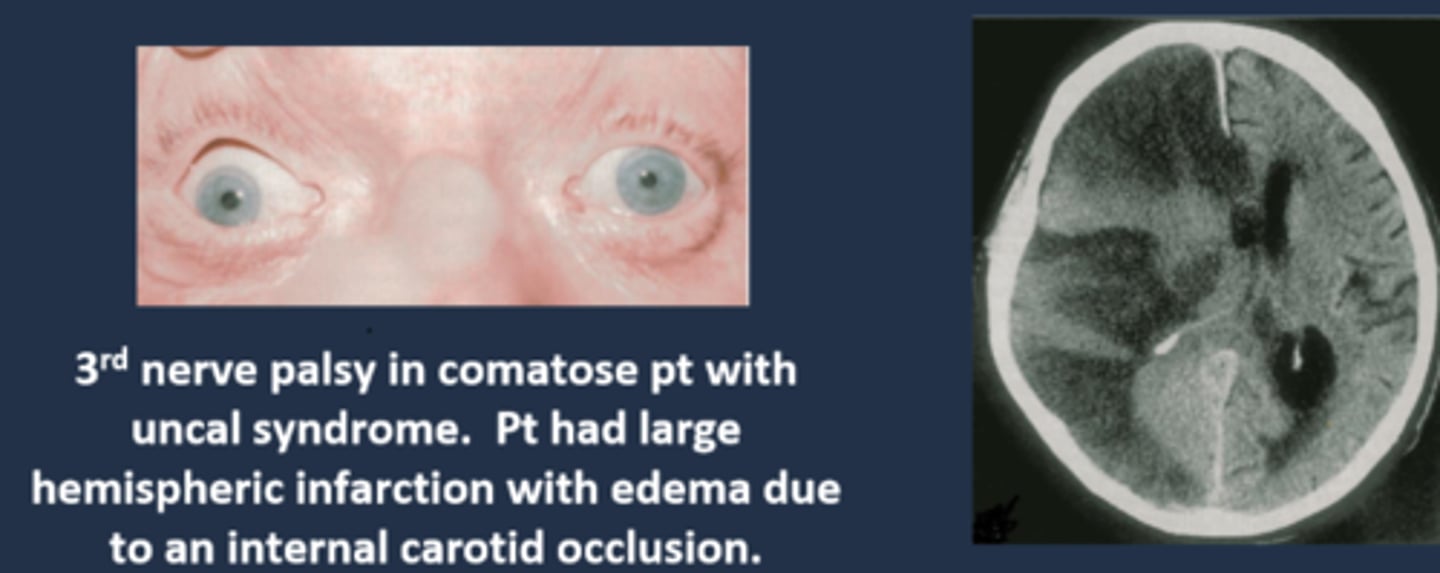
Explain the progression of the Hutchinson pupil seen in Uncal syndrome.
1. miotic pupil due to initial cerbreal edema
2. ipsilateral dilated pupil due to expanding mass on that side
3. bilateral fixed and dilated pupils eventually
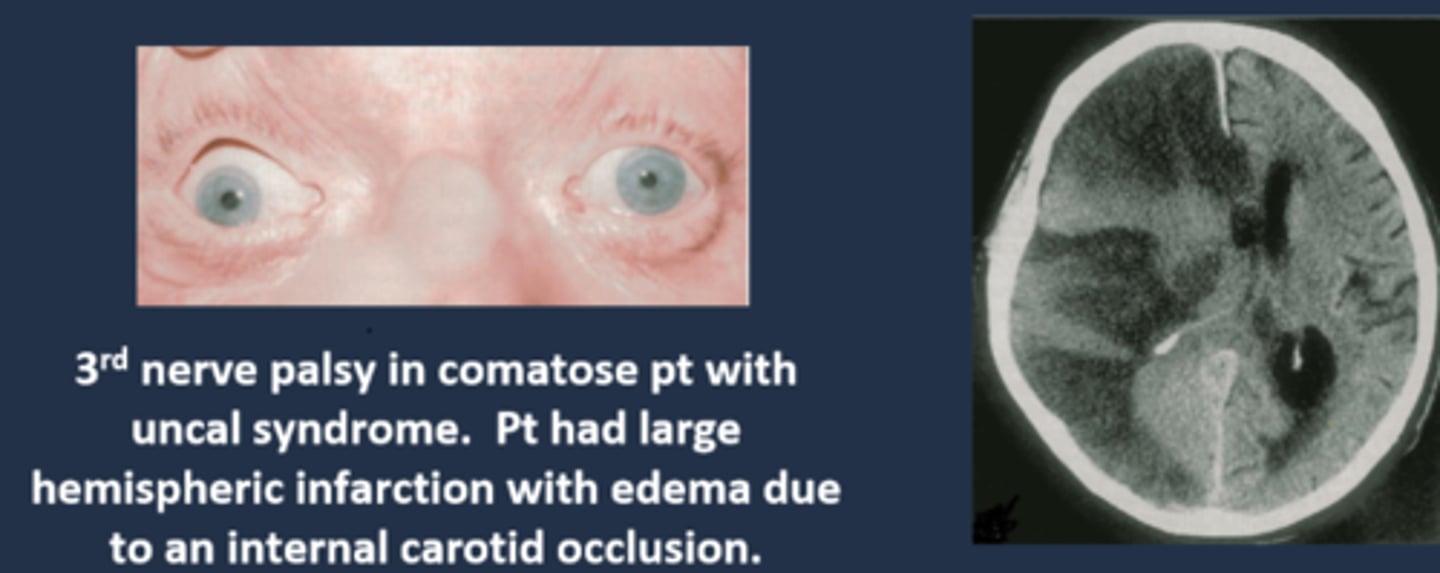
What are 3 other ocular signs of Uncal syndrome?
bilateral papilledema bc of increased ICP (bilateral even if only 1 pupil involved)
homonymous hemianopsia bc posterior cerebral arteries are occluded by mass = calcarine cortex ischemia
EOM paralysis = diplopia but mostly very late in the disease
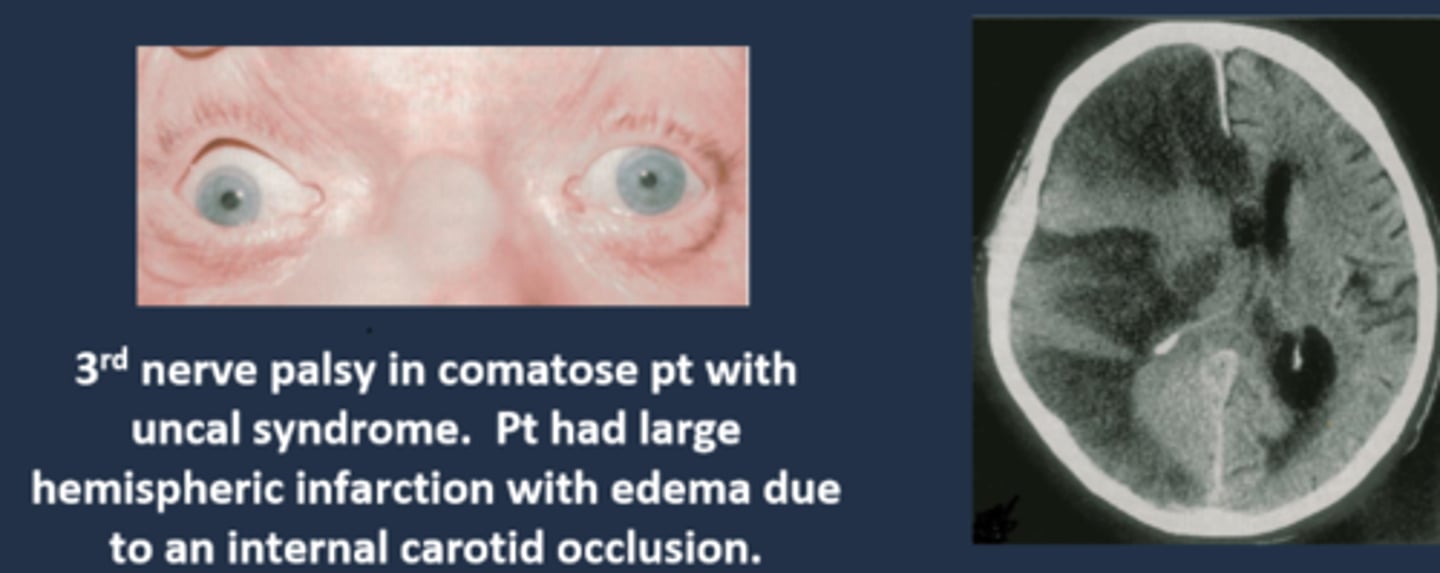
What are some other S/S of Uncal syndrome?
HA
confusion
somnolence (sleepy)
coma
tenderness over clot region
Cheyne-Stokes respiration = forced breathing, deep and shallow, periods of no breath
overall, pt's will be very ill and presenting to the ER (or you should send them to ER immediately!)
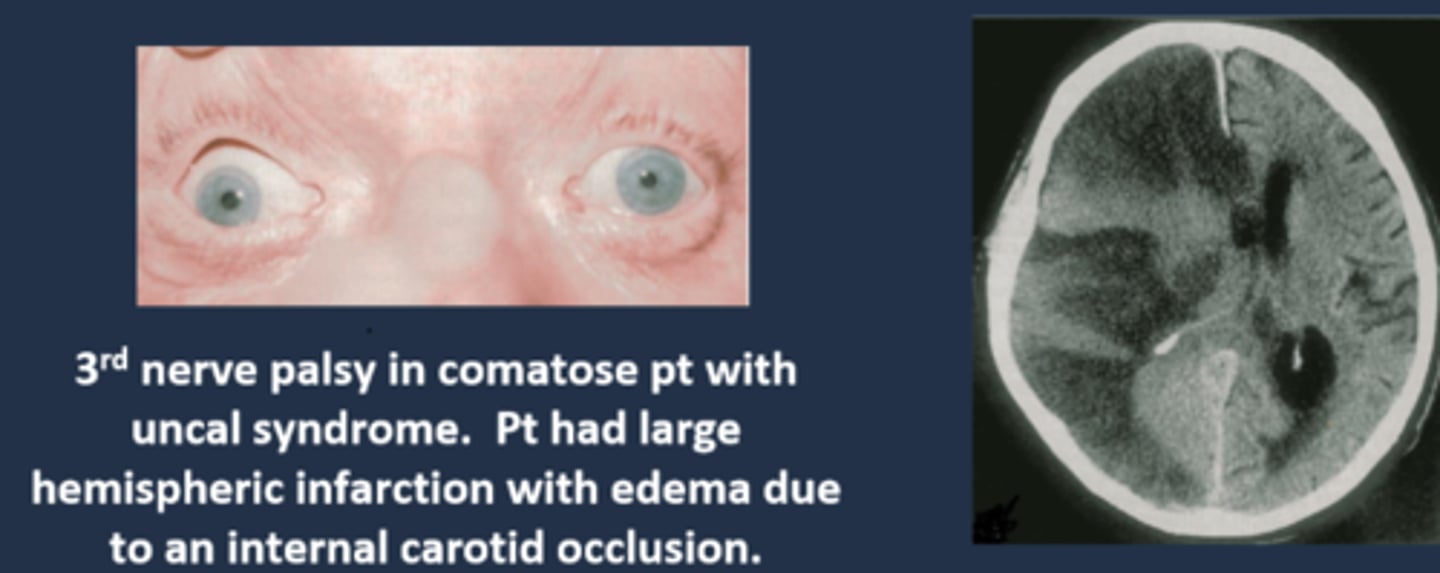
What is the most common cause of Uncal syndrome?
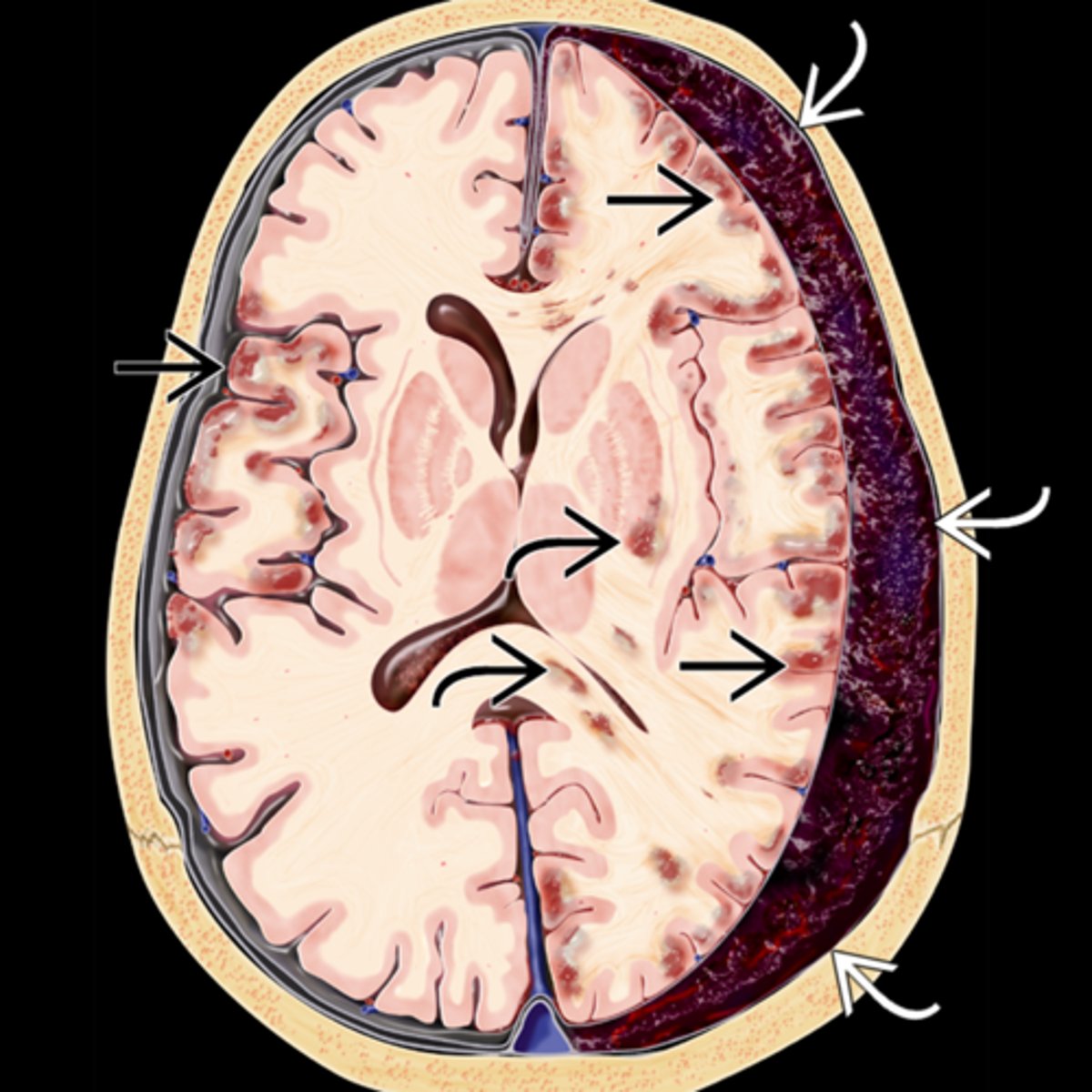
chronic subdural hematoma from head trauma esp in inebriated pt's
What are some less common causes of Uncal syndrome?
extradural hematoma from injury
subdural hematoma from drugs
Explain the series of a events that causes a subdural hematoma, Uncal syndrome, and eventually death.
trauma = brain moves ant to post = cerebral veins in subdural space rip = blood fills subdural space = fibrous dura and arachnoid mesothelium beneath create a sac around the cot = sac breaks = blood enters brain = pt is sick and dies
Where is the Uncal region, affected in Uncal syndrome?
uncas of parahippocampal gyrus (inferior area of temporal lobe) = lateral to the brainstem = lateral to CN III in brainstem
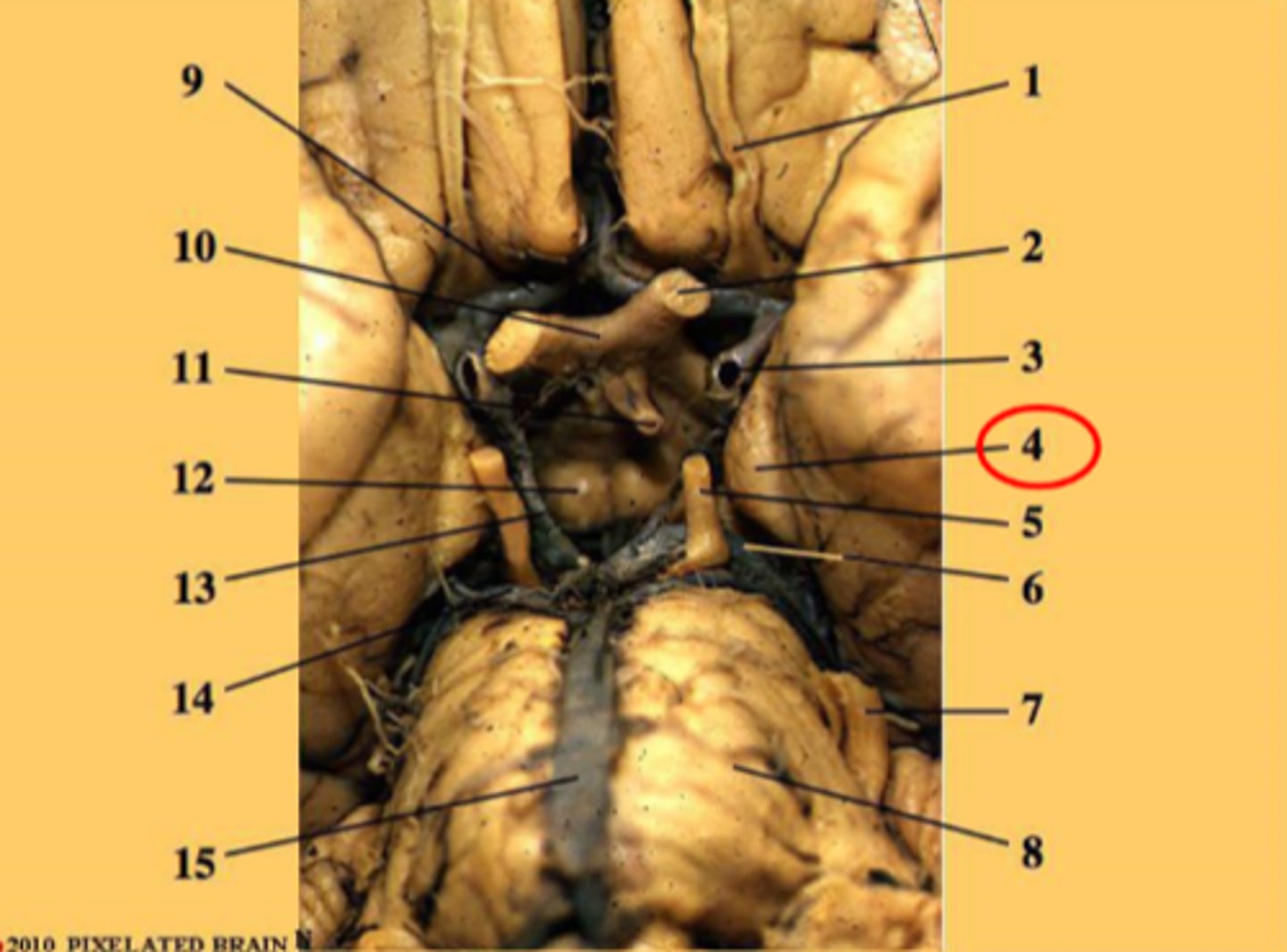
Explain how the Uncal region can affect CN III in Uncal syndrome.
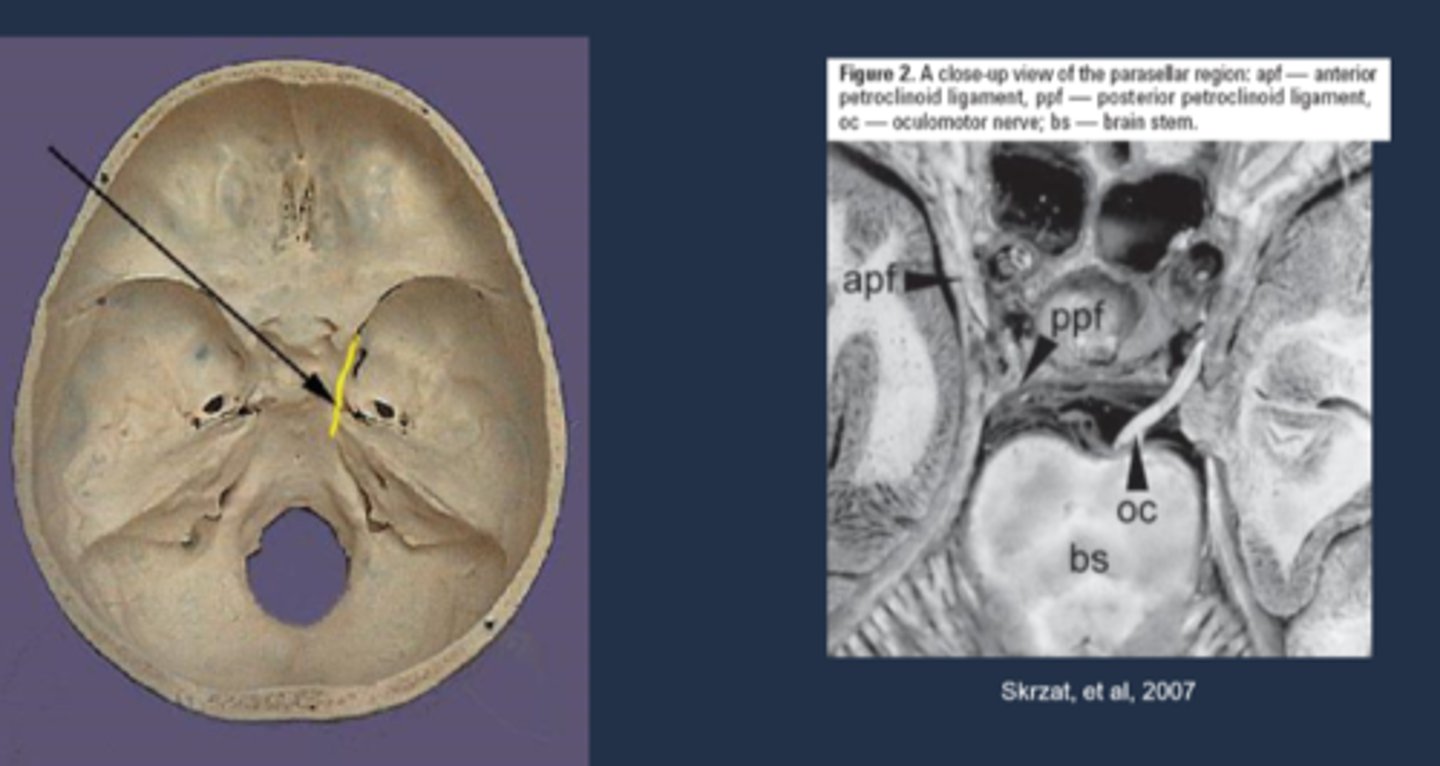
CN III leaves brainstem = pupillomotor fibers move dorsomedially = uncus herniates = compresses CN III dorsomedially against petroclinoid ligament and dorsum sellae = pupil is blown
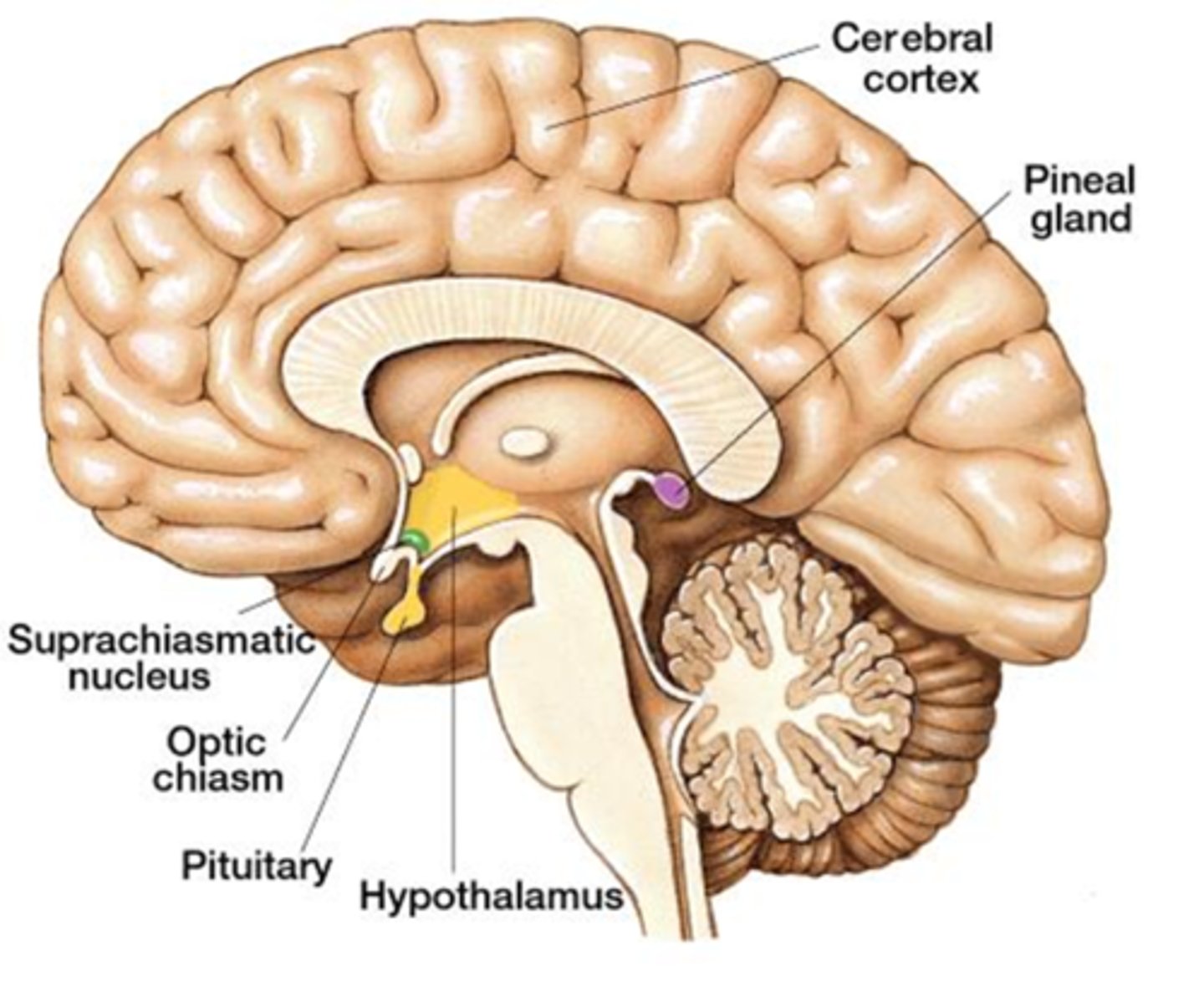
What is Parinaud's (dorsal midbrain) syndrome?
CNS lesion (tumor, MS, stroke, etc) causing compression on dorsal midbrain, affecting the...
superior colliculus = coordinating eye movement, convergence
MLF = vertical saccades
nucleus of Cajal = vertical gaze maintenance
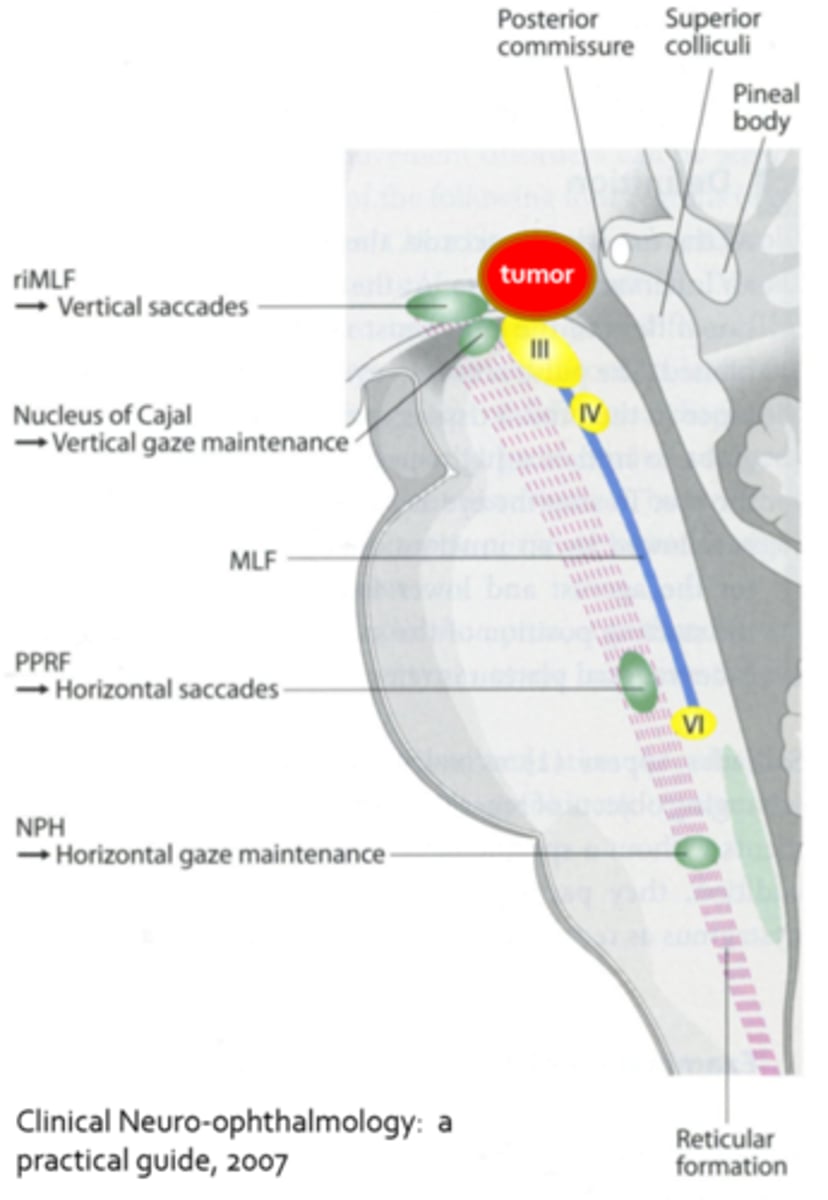
What pupil finding is seen in Parinaud's (dorsal midbrain) syndrome?
light-near dissociated pupils
What are 3 other ocular findings seen in Parinaud's (dorsal midbrain) syndrome?
convergence retraction nystagmus = eyes turn in and retract (pulse in and out) when trying to look up
lid retraction = Collier's sign
inability to make saccades upwards (pursuit ability lost later as well)
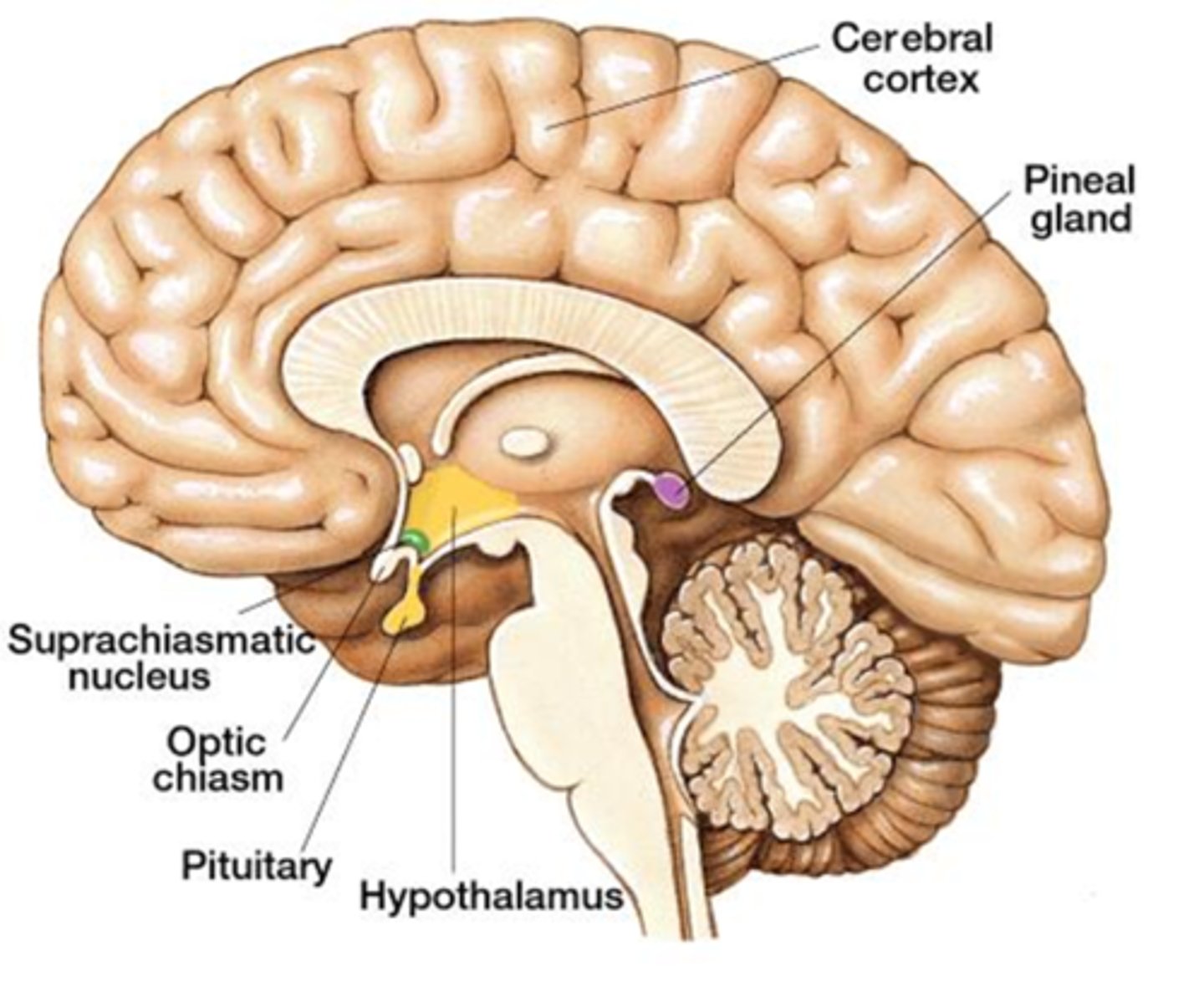
What is a very common cause of Parinaud's (dorsal midbrain) syndrome?
pineal gland tumor = would also show reduced melatonin and increased LH (precocious puberty)