Ch. 6 Pt 1 Corticospinal Tract & Other Motor Pathways
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
Review: key tips for localizing clinical lesions (motor and sensory)
1) crossover (decussation) of a pathway
2) somatotopy of different body parts in the cortex and tracts
3) practice drawing tracts and somatotopic representation in the brain and spinal cord
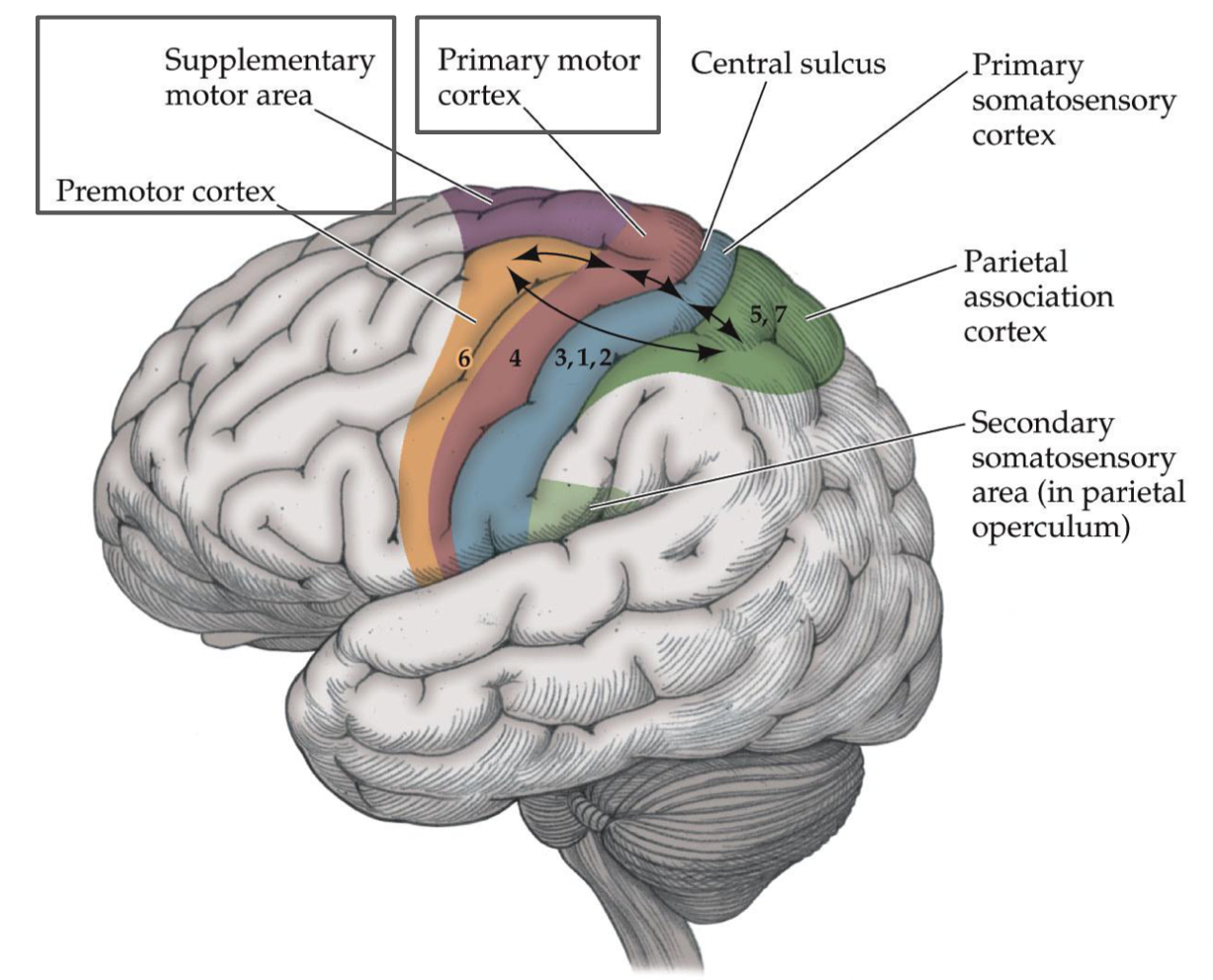
Review: What does the primary motor cortex (PMC, Area 4) control in the body? What deficits would occur if there was a lesion?
controls movement on the contralateral side of the body
- lesion: motor deficits on contralateral side
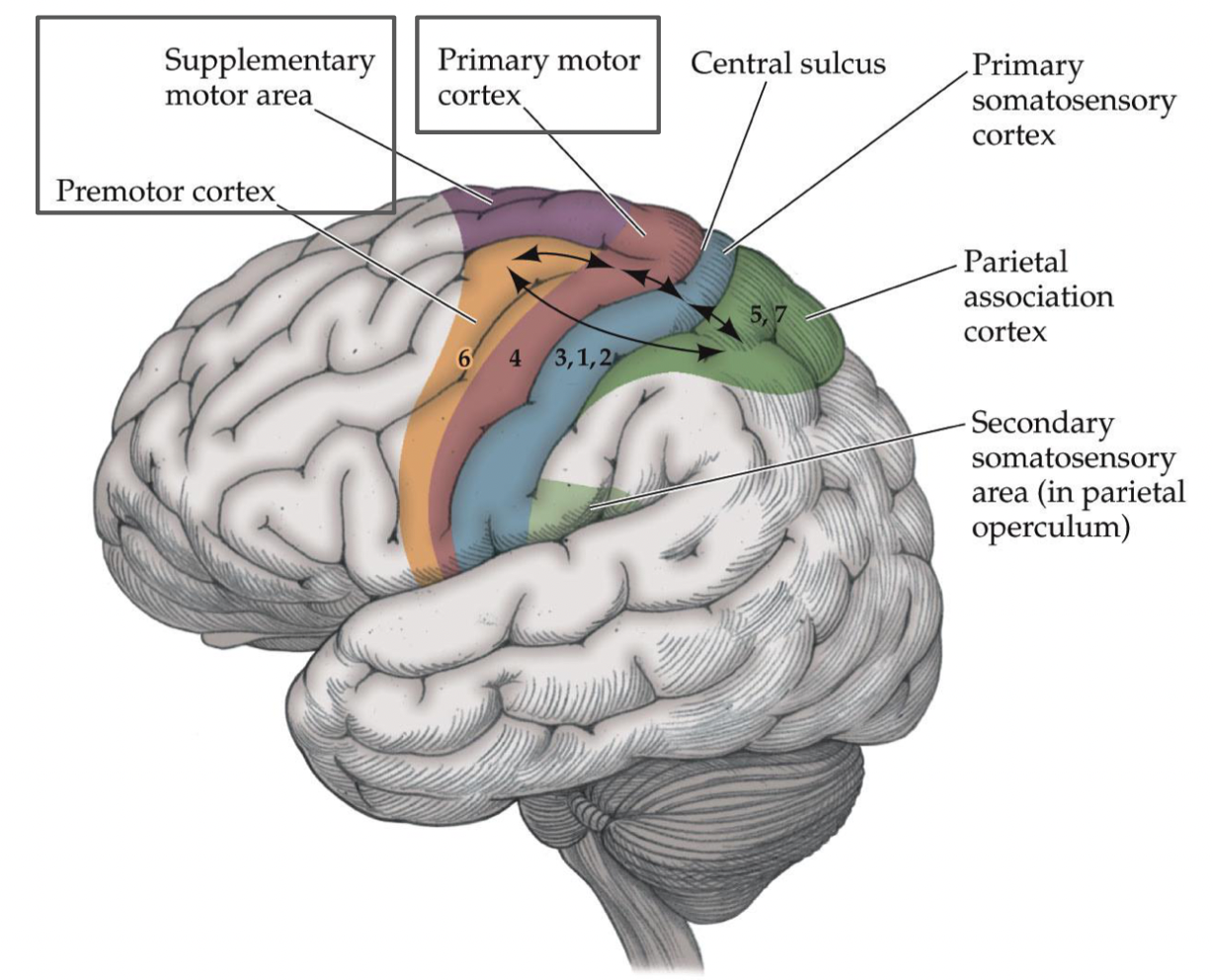
Review: supplementary motor area (area 6) and premotor cortex (area 6) location? What type of movement planning are they involved in? What deficits occur with a lesion? What connections exist between motor and sensory areas?
- anterior to primary motor cortex
- involved in higher-order movement planning and project to PMC
- lesions: deficits in movement planning
- reciprocal connections also exist b/w motor and sensory areas
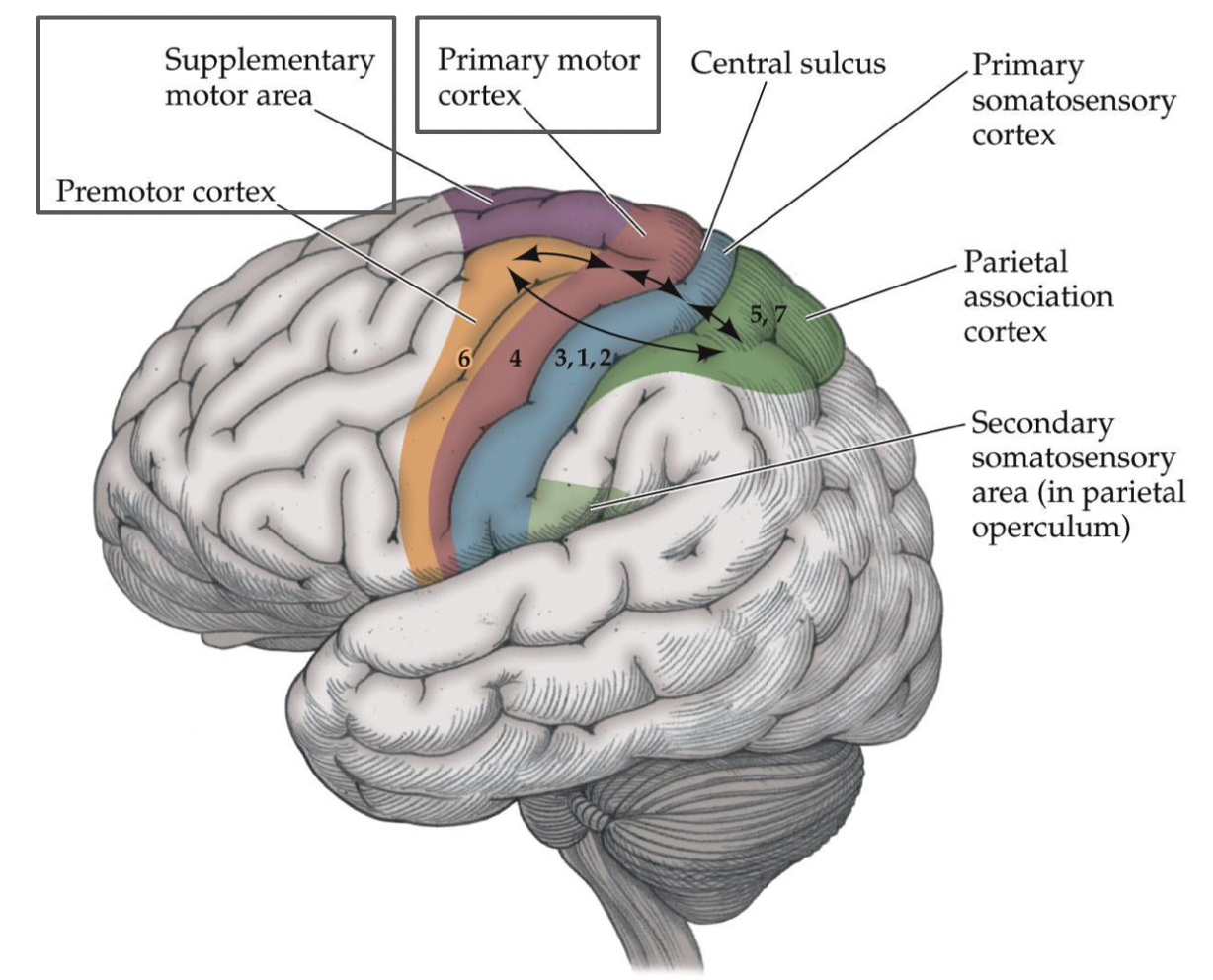
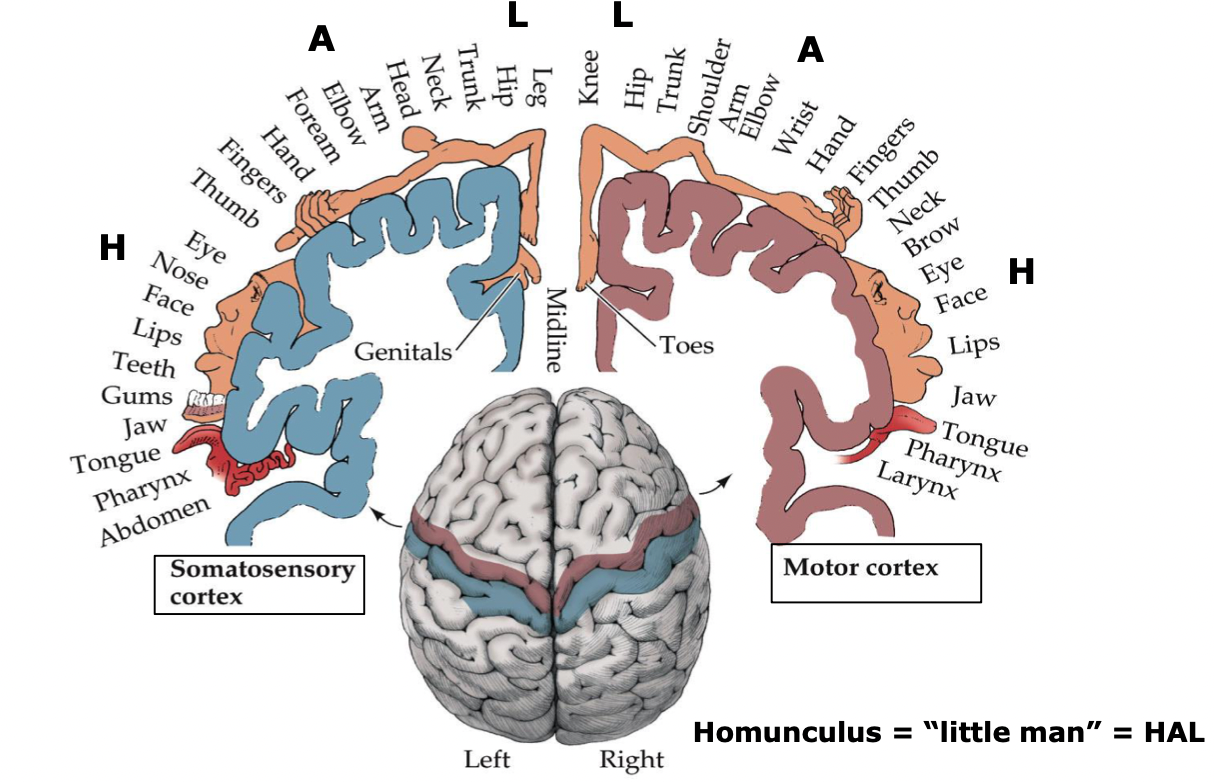
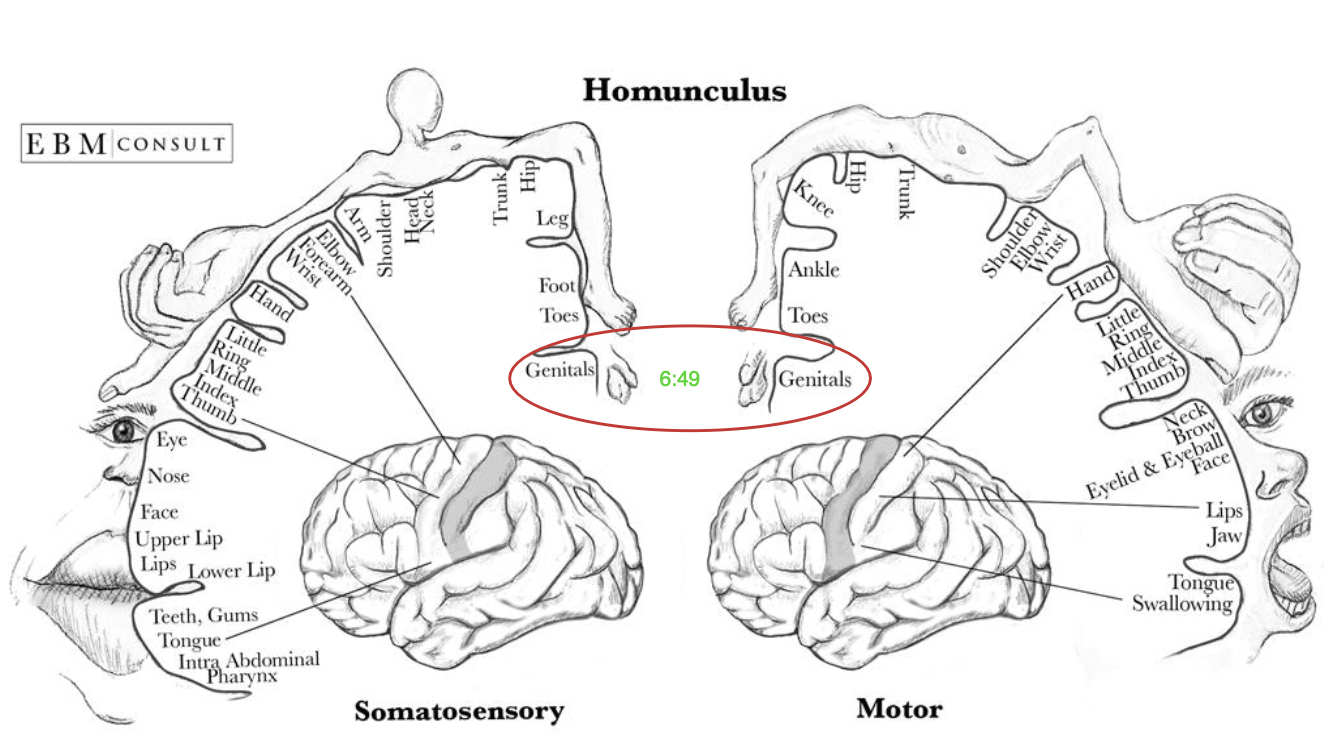
Motor and sensory cortex and their pathways exhibit what type of organization?
somatotopic organization
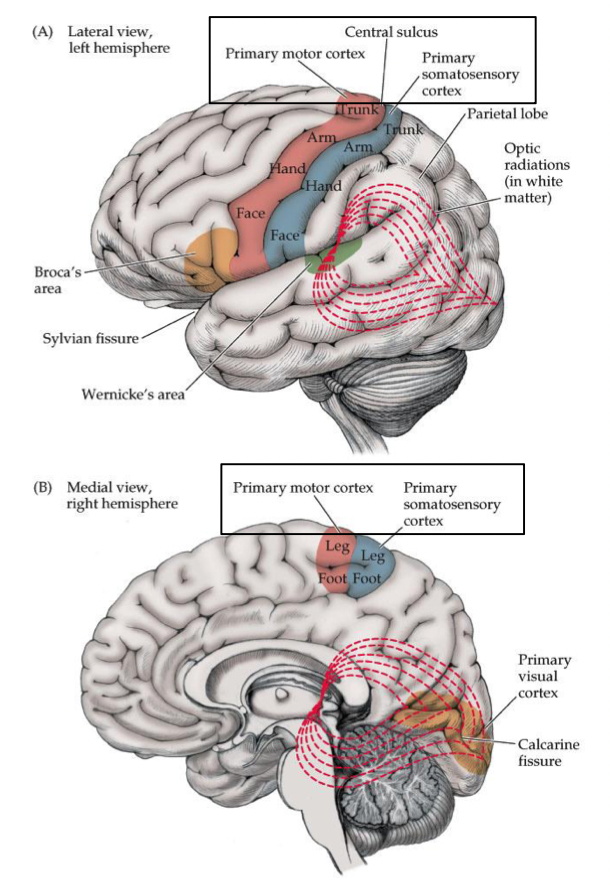
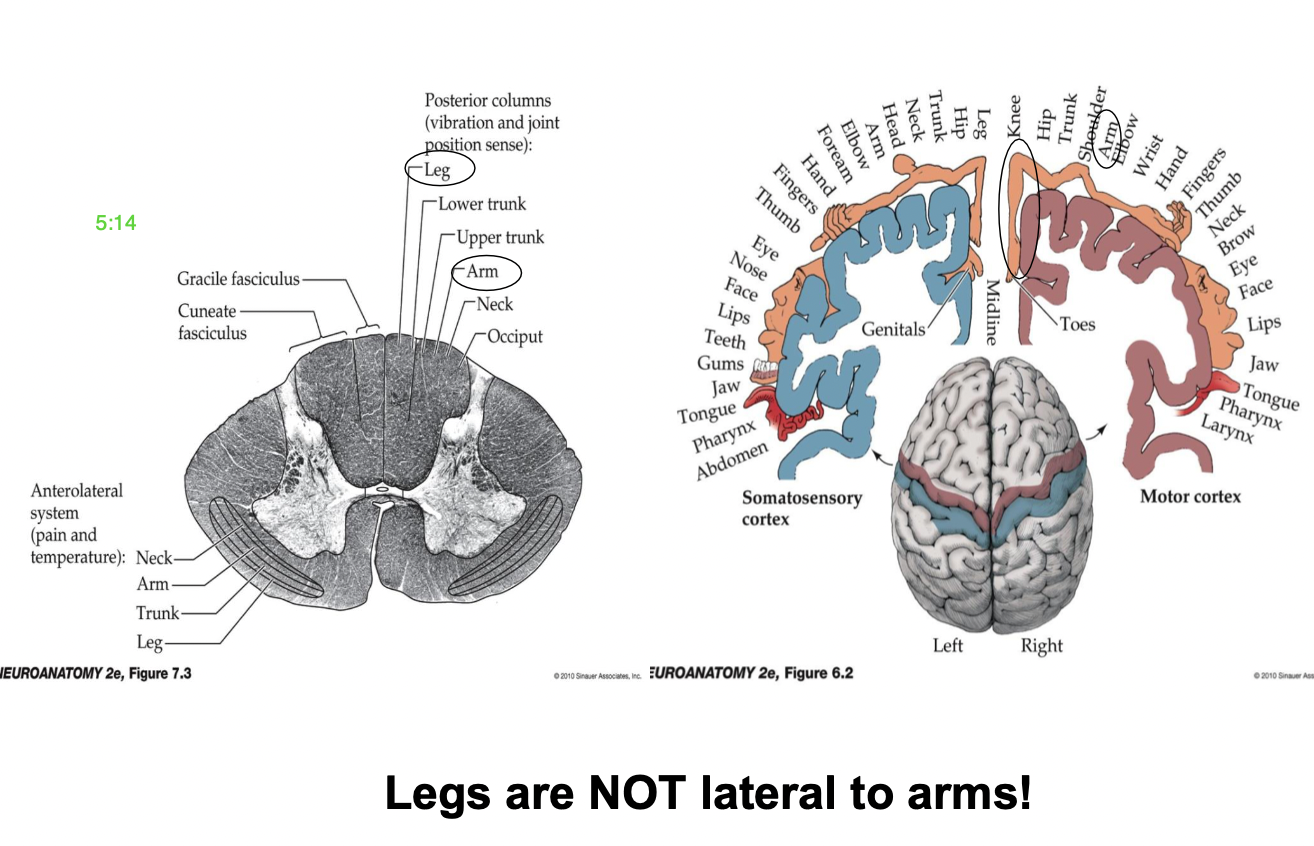
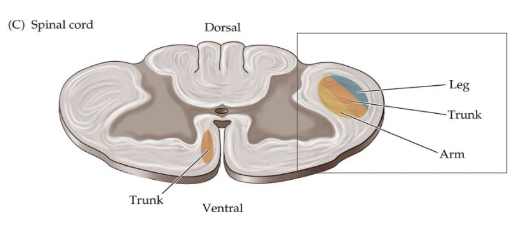
How do motor and sensory pathways maintain their organization? Where are the lower extremities located?
- maintain a rough somatotopic organization along their entire length
Lower extremities = Lateral
The legs are lateral to the arms with two exceptions:
1) primary motor and primary somatosensory cortex
2) dorsal (posterior) columns
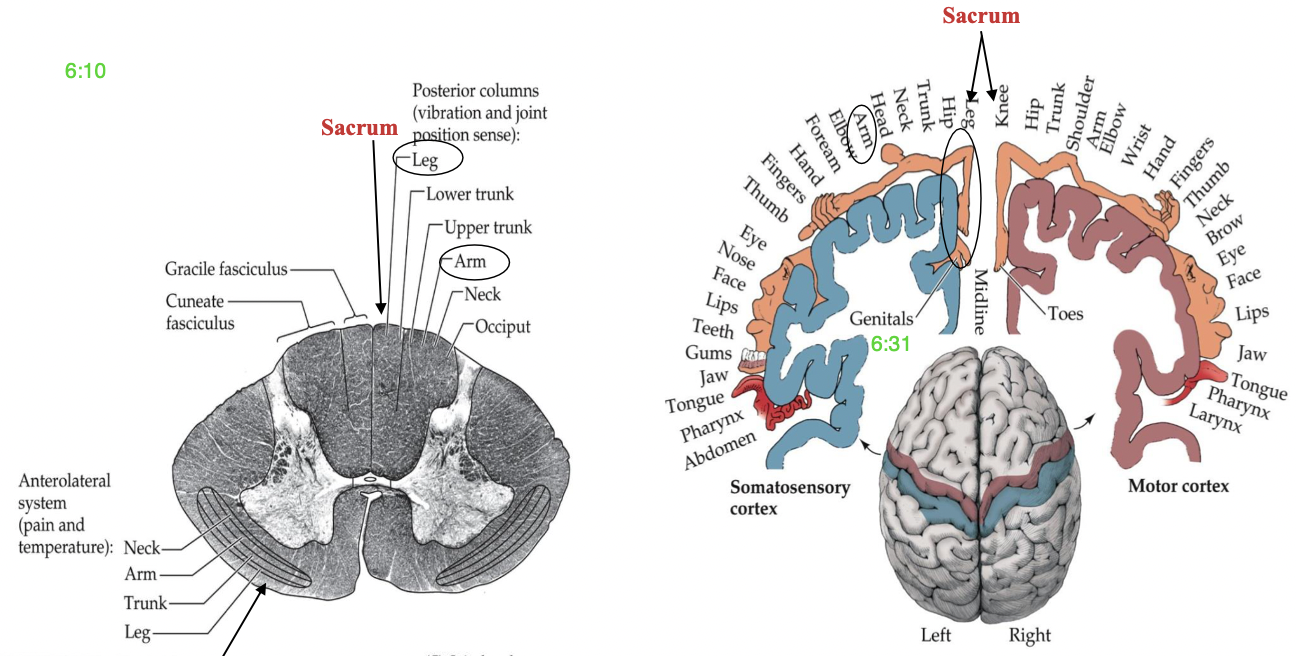
Where is the sacrum located in the posterior columns and somatosensory/motor cortex (homunculus)?
in the midline between leg and knee, near “genitals”
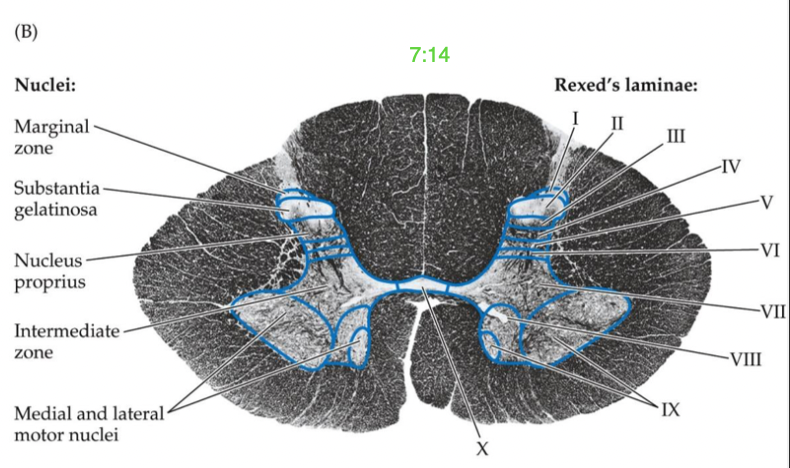
What is gray matter? What is it divided by?
- neuron cell bodies
- divided by functional groups of nuclei called laminae
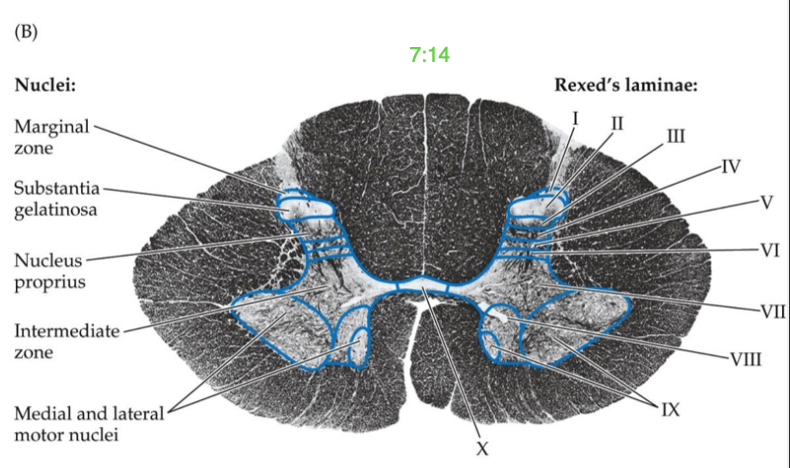
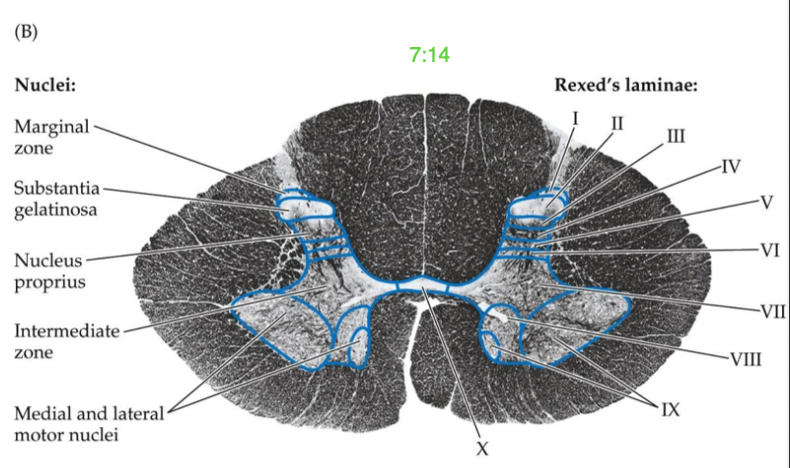
What is the ventral/anterior horn? Which laminae are involved?
motor nuclei (motor neuron pools [MNP])
Laminae VIII-IX (outgoing skeletal muscle innervation)
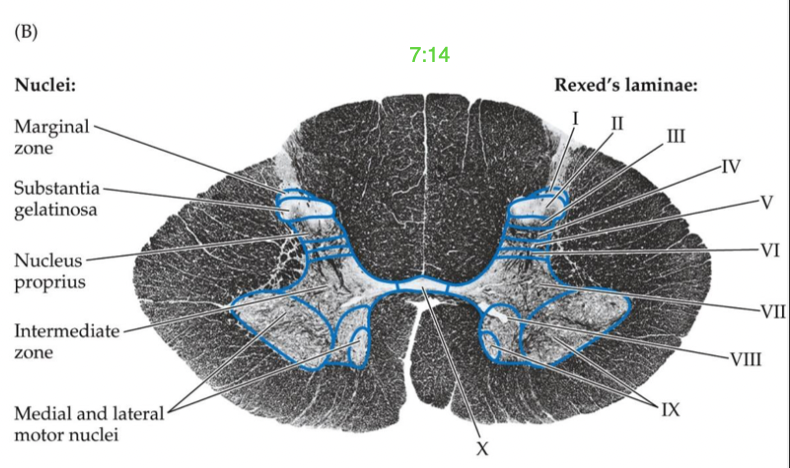
What is the dorsal/posterior horn? Which laminae are involved?
sensory nuclei
Laminae I-VI (incoming sensory information)
Where is the intermediate zone in between? What laminae is involved? (2)
in between the ventral/dorsal horns
Laminae VII: visceral functions
Laminae X: gray commissure - axons crossover to other side of SC
What is white matter? What do ascending and descending axons surround? What tracts does it form?
- myelinated axons
- ascending/descending axons surround gray matter
- form motor and sensory tracts/fasciculi
What is the entry point of sensory axons in the spinal cord?
dorsolateral sulcus
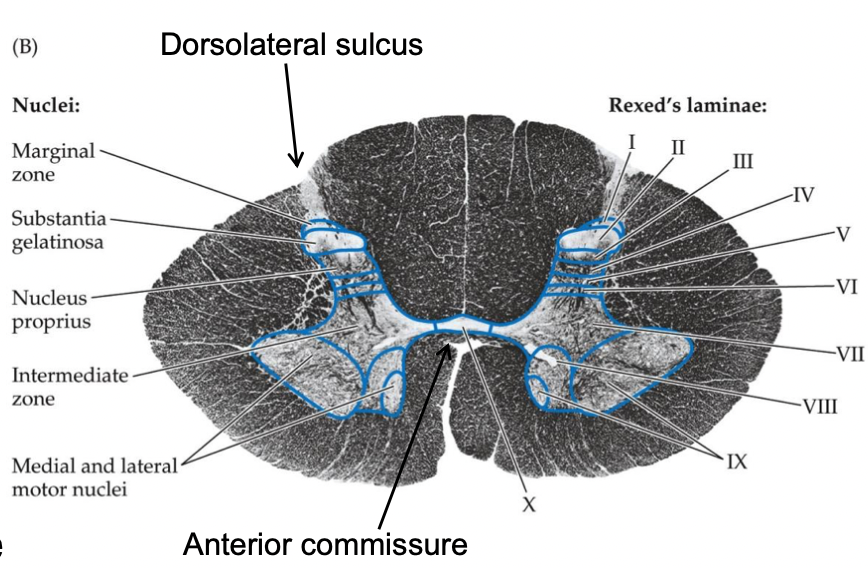
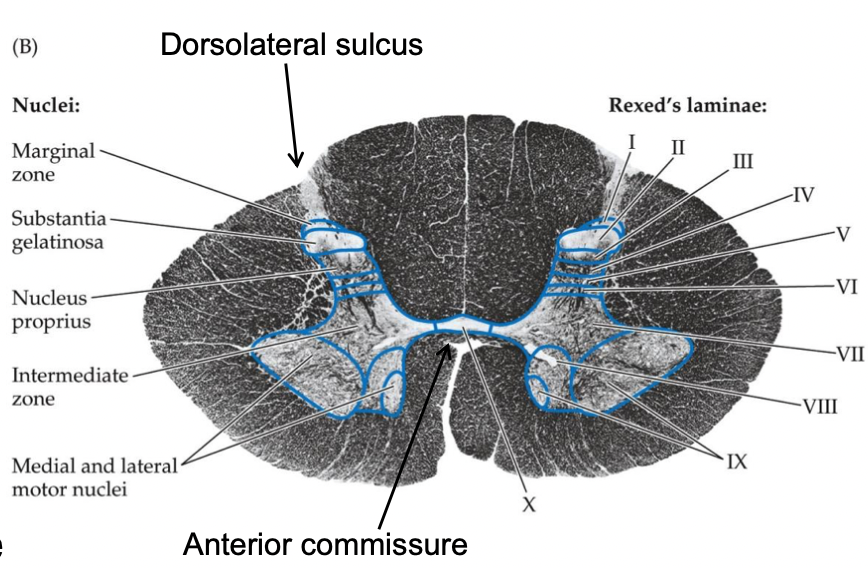
What is the anterior commissure?
decussation of spinothalamic tract axons
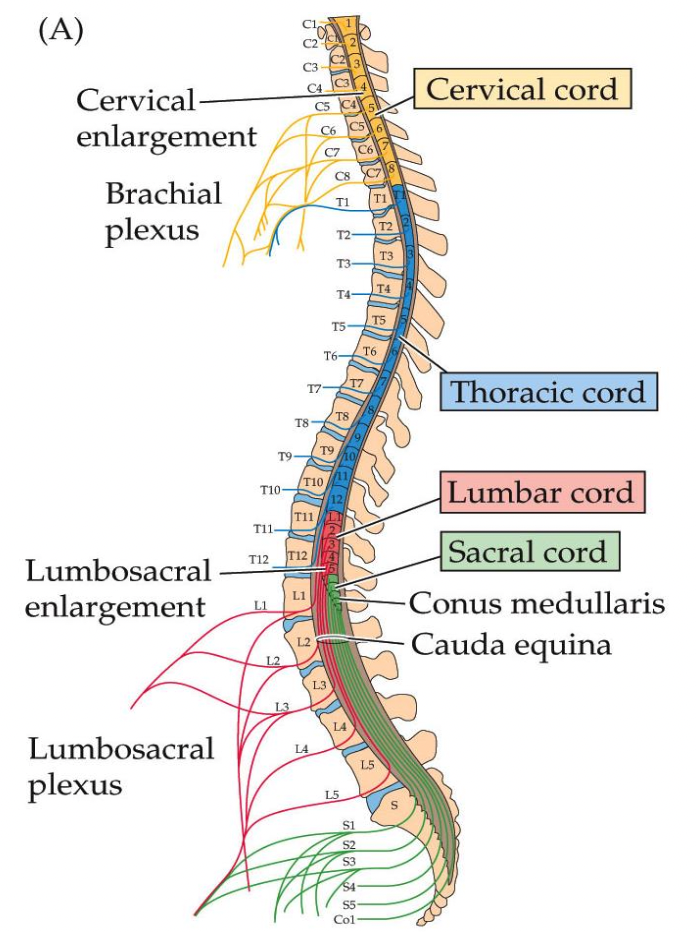
What are the levels of the cervical and lumbosacral enlargements?
cervical enlargement: ~C3-T1
lumbosacral enlargement: ~L1-S2
In the two enlargements of the spinal cord, where is there more motor nuclei? Why?
more motor nuclei in the ventral horns for the innervation of the arms and legs
there are more in the cervical/lumbar enlargement because there are so many cells bodies for the start of LMNs to go out and innervate the muscles of the arms and legs
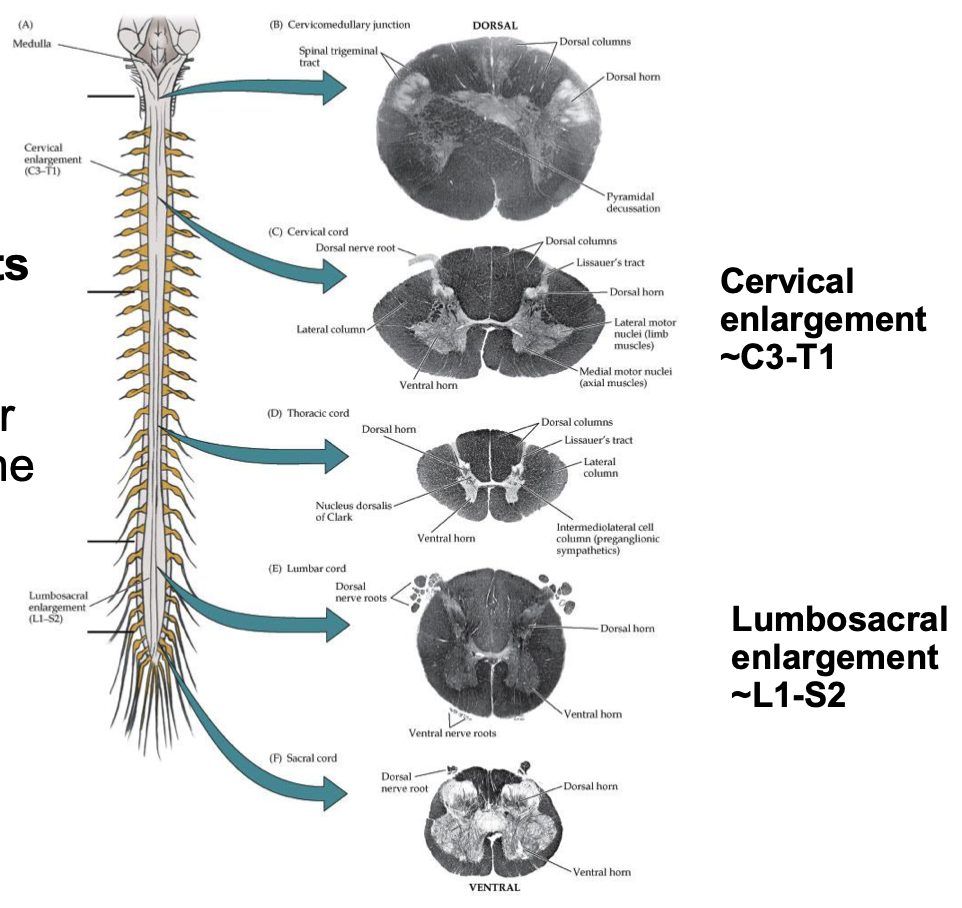
Why is there more white matter at cervical levels compared to lumbosacral levels?
- Most of the ascending fibers have already entered the spinal cord (almost arrived at the brain, the final stop)
- Most of the descending fibers (motor neuron pathways) have NOT started to peel off yet to innervate the LMNs
How much of the spinal cord does the anterior spinal artery make up?
ventral, lateral ~2/3 of spinal cord
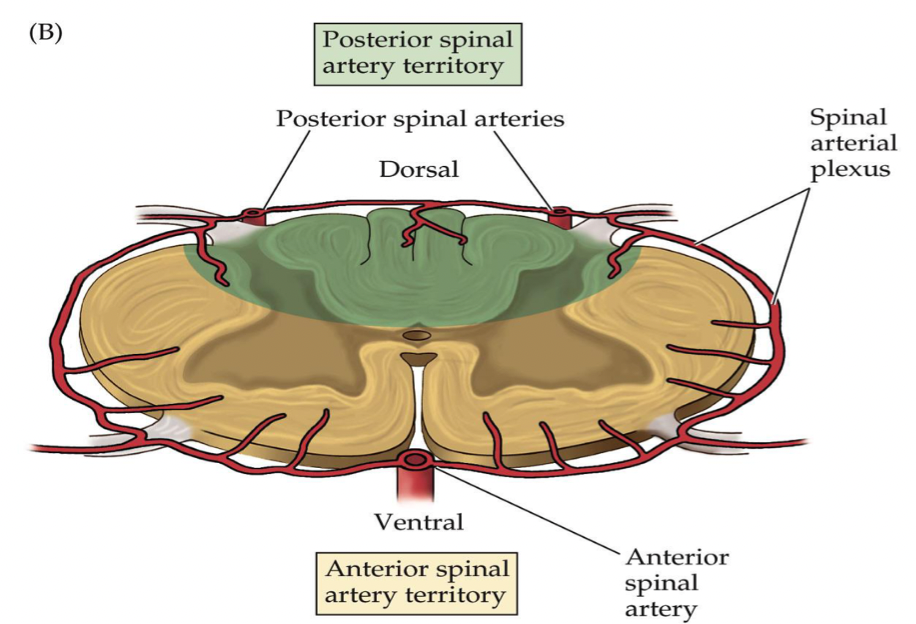
How much of the spinal cord does the posterior spinal artery make up? What does is form surrounding the spinal cord?
dorsal, midline ~1/3 of spinal cord
forms a spinal artery plexus
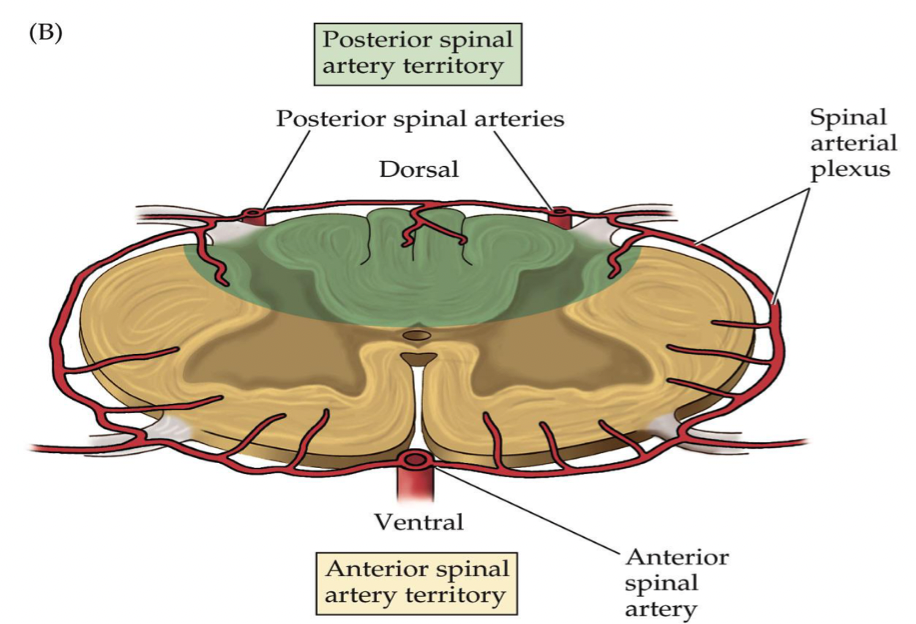
What arteries also assist with supplying the spinal cord inferiorly?
several radicular arteries (off aorta)
What is the influence of basal ganglia and the cerebellum on the motor system? What do they not have a direct connection to?
- provide a major, indirect influence on the motor system
- no direct connections to LMNs (does not synapse directly)
What is the mechanism that the basal ganglia and cerebellum use to refine motor output? Which pathways are activity adjusted?
- use of feedback systems/loops
- feedback loops adjust activity in the descending motor pathways
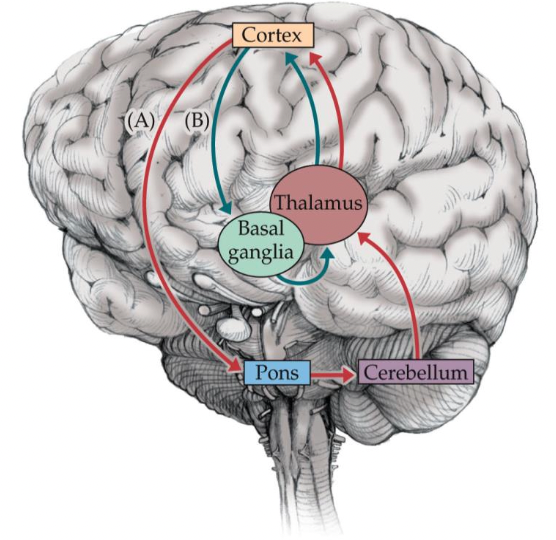
In the feedback loops of basal ganglia and cerebellum, what inputs are received, and where are outputs sent?
- receive major inputs from motor cortex about planned movement
- send outputs through thalamus (second snoop in town) to influence motor cortex
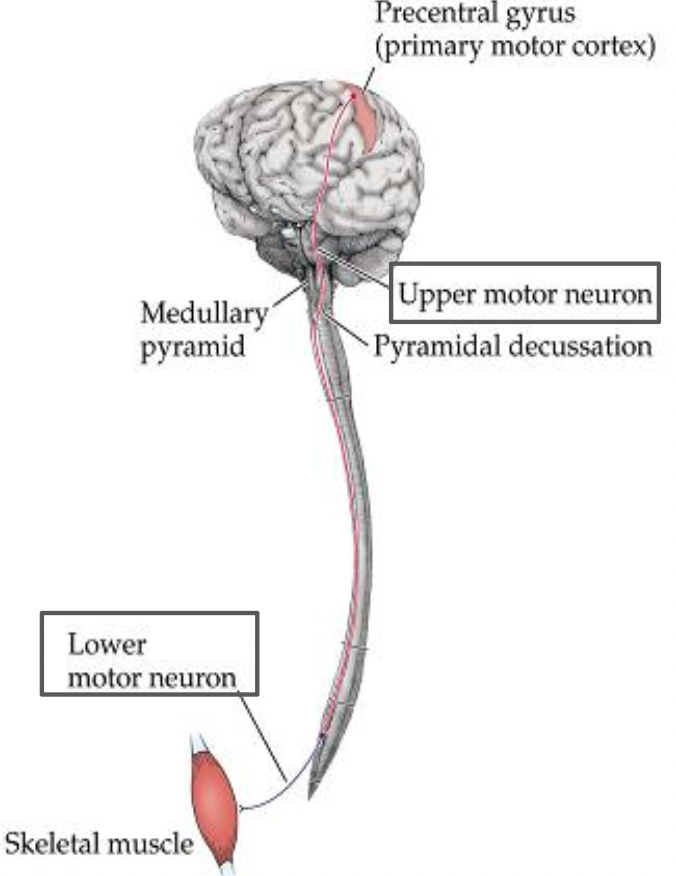
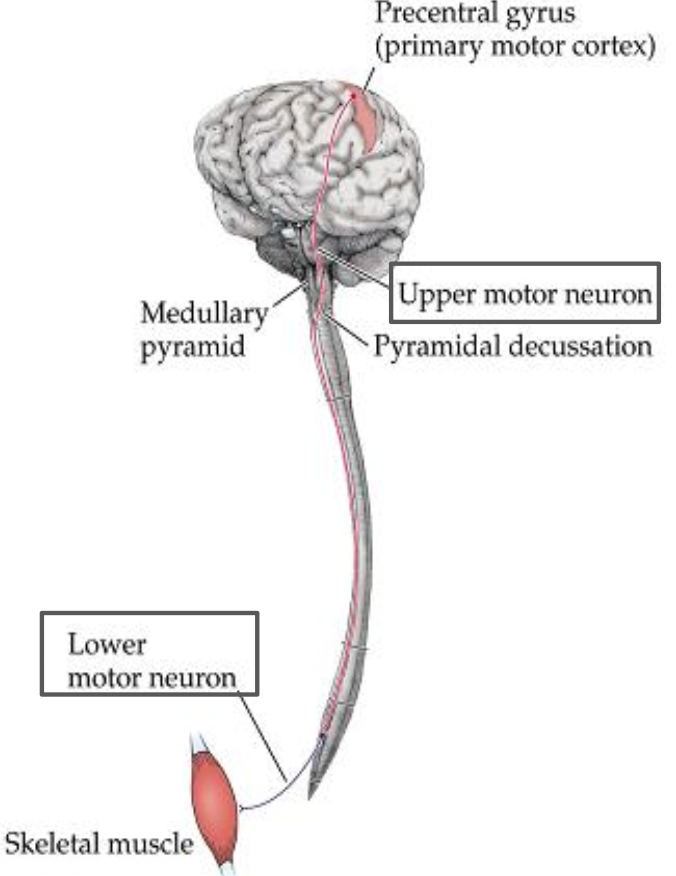
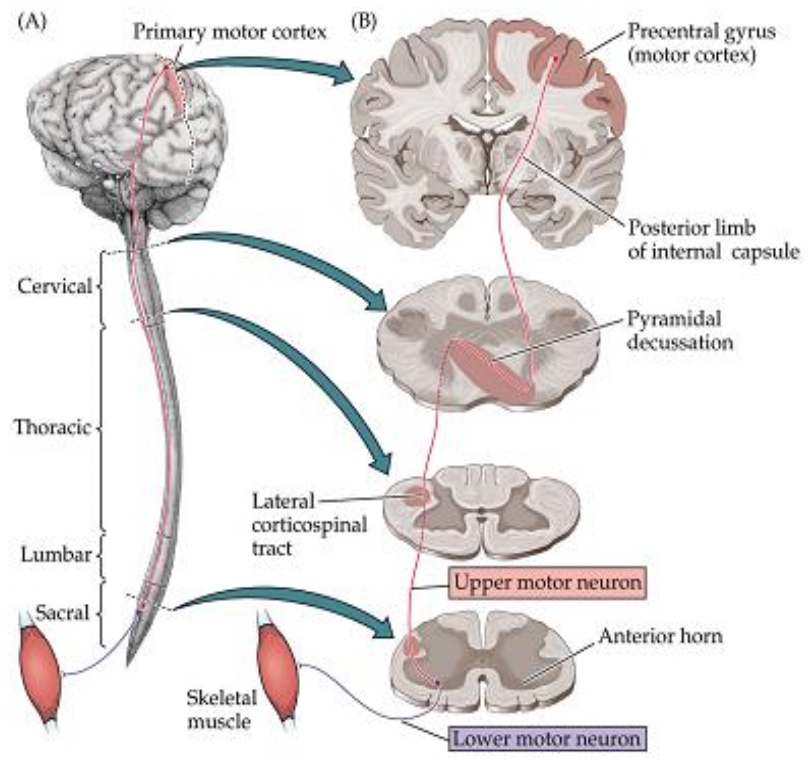
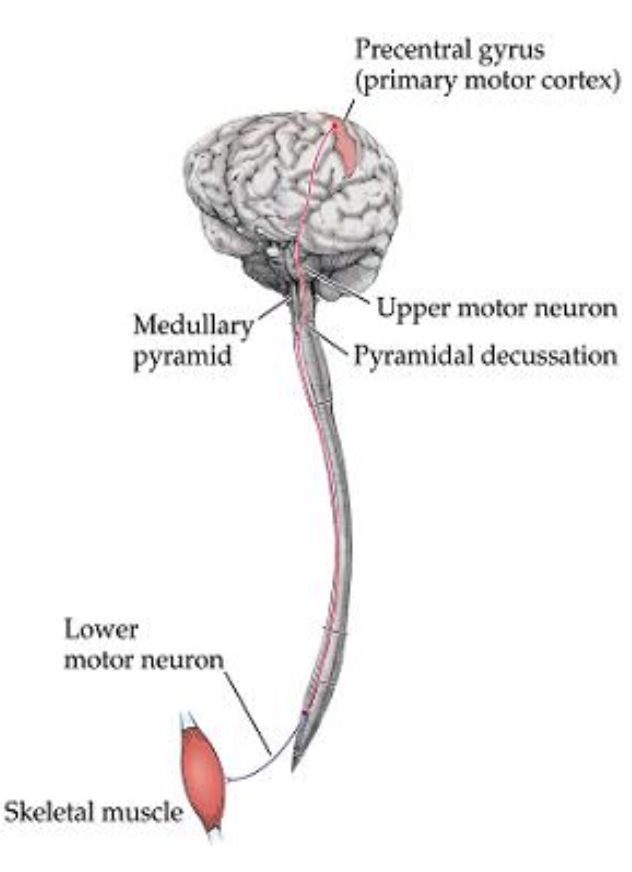
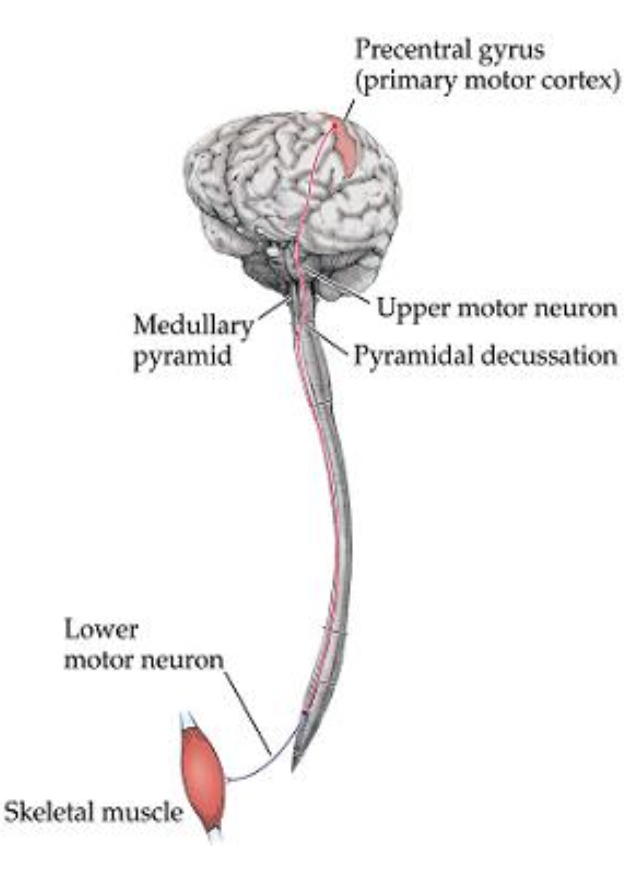
Motor pathways: Where do upper motor neurons (UMN) project from? down to where?
motor neuron that projects from cerebral cortex (precentral gyrus) down to spinal cord or brainstem to synapse onto LMN
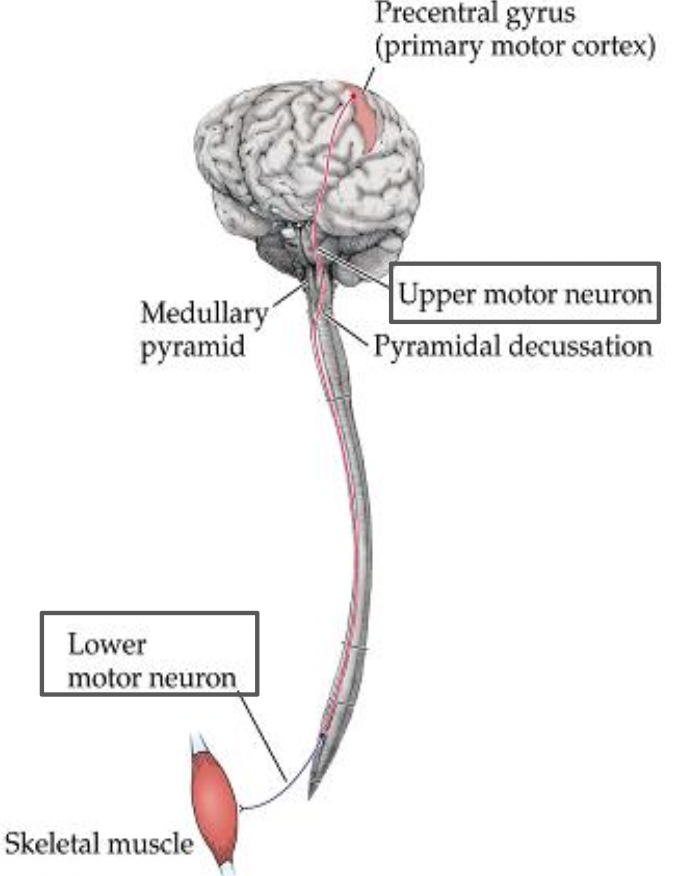
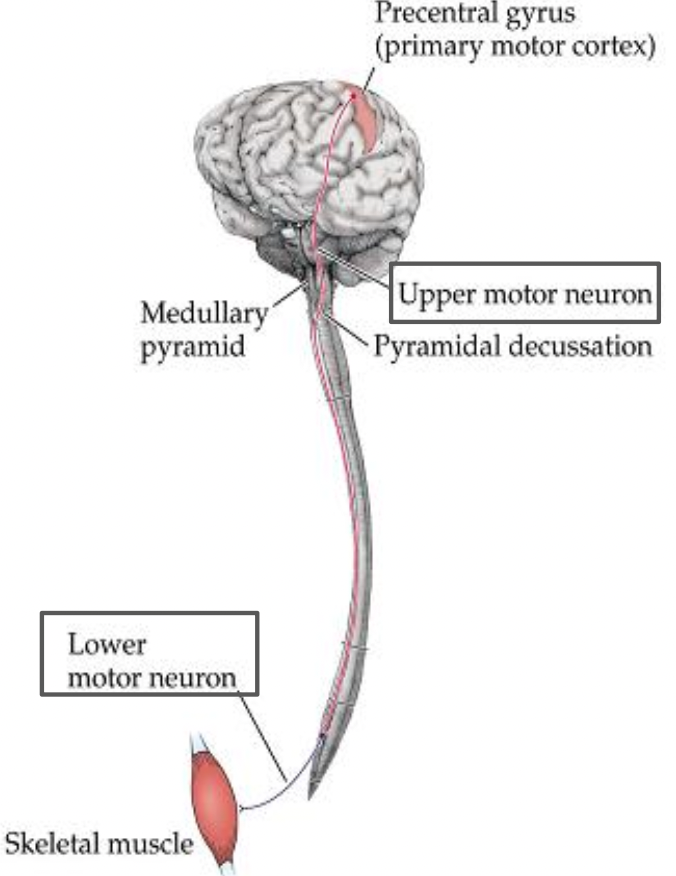
Motor pathways: Where are lower motor neurons (LMN) located? Where does it project out to?
motor neuron located in anterior horn of gray matter of spinal cord (or brainstem, if cranial nerve) that projects out to striated muscle
What neurons are LMNs composed of?
What should these not be confused with?
composed of alpha motor neurons - largest neurons in the SC
* do not confuse w/ gamma motor neurons - associated w/ muscle spindle to increase sensitivity to stretch *
What are tracts generally named according to? Give an example using the corticospinal tract.
tracts are generally named according to the origin and termination
e.g. corticospinal tract - originates in cortex and terminates in spinal cord
descending motor tracts from the cortex (UMNs) influence motor output by synapsing on LMNs
What are the descending motor pathways/systems categorized into?
based on the location in the SC
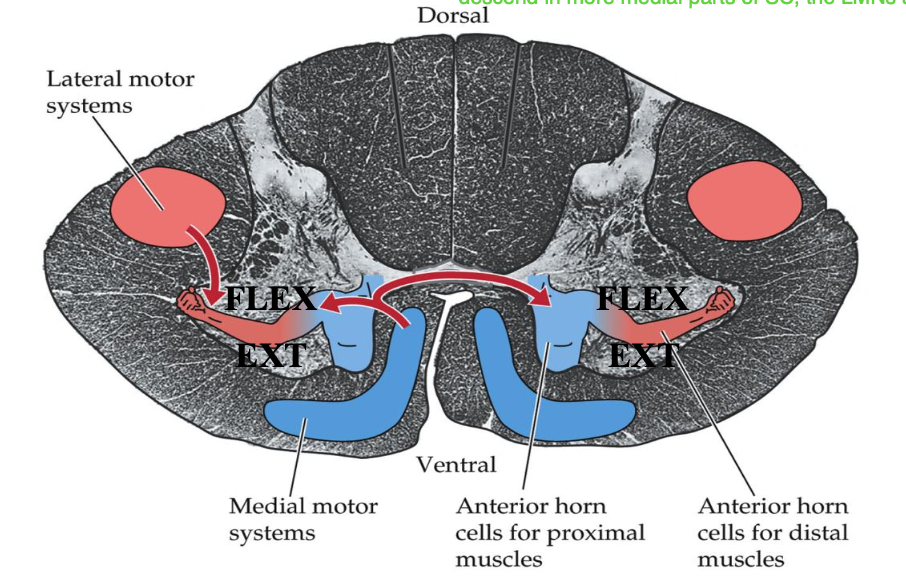
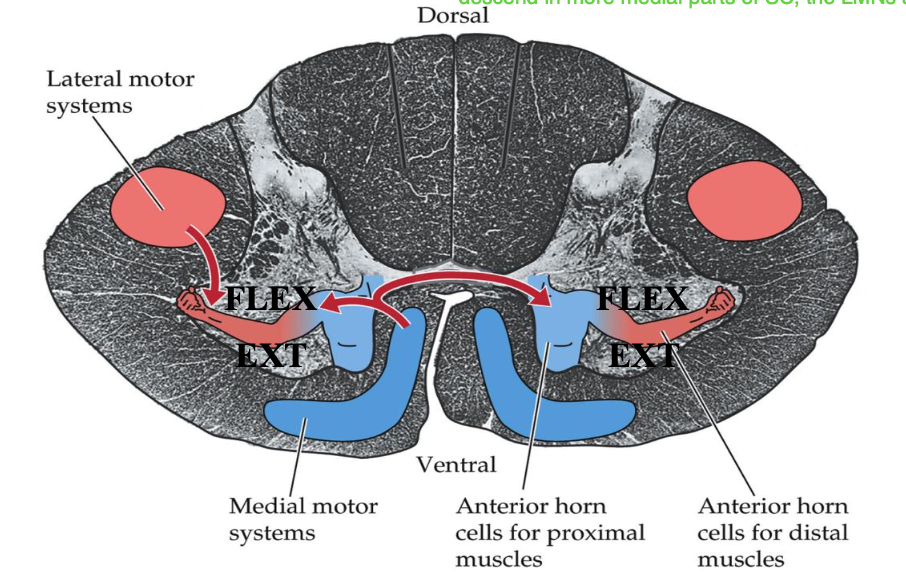
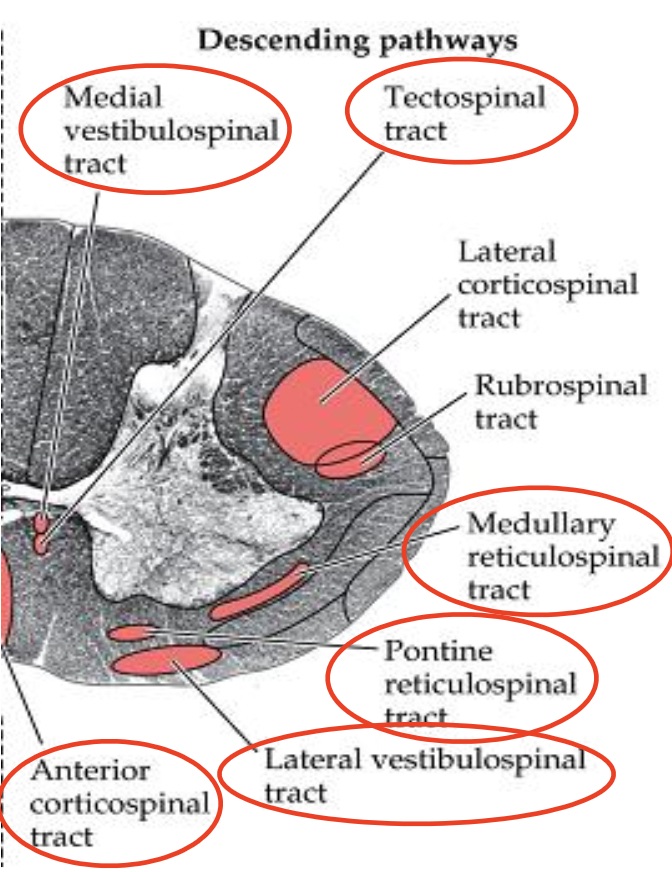
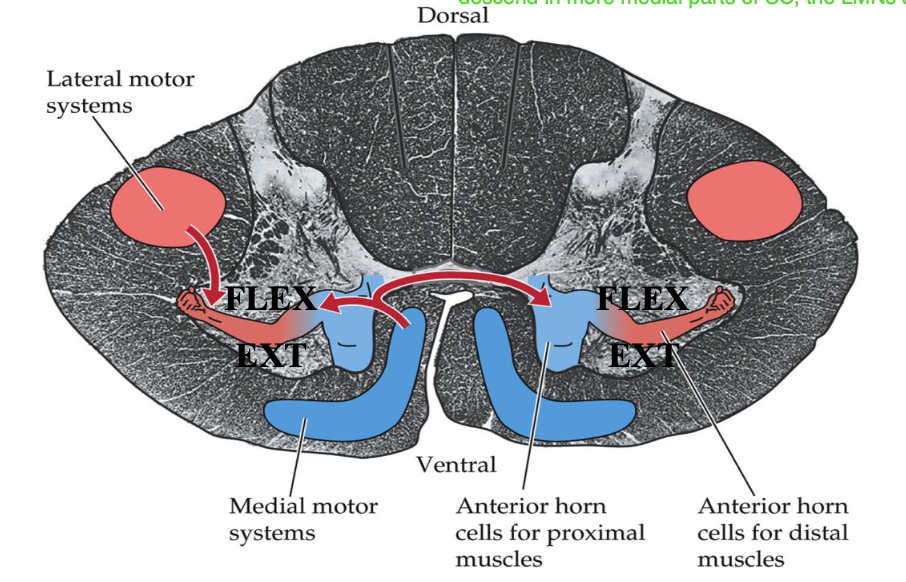
Where are lateral motor pathways located in the SC? What are the two pathways?
located in the lateral portion of the SC to synapse on lateral motor nuclei in the anterior horn (distal musculature)
1) lateral corticospinal tract
2) rubrospinal tract
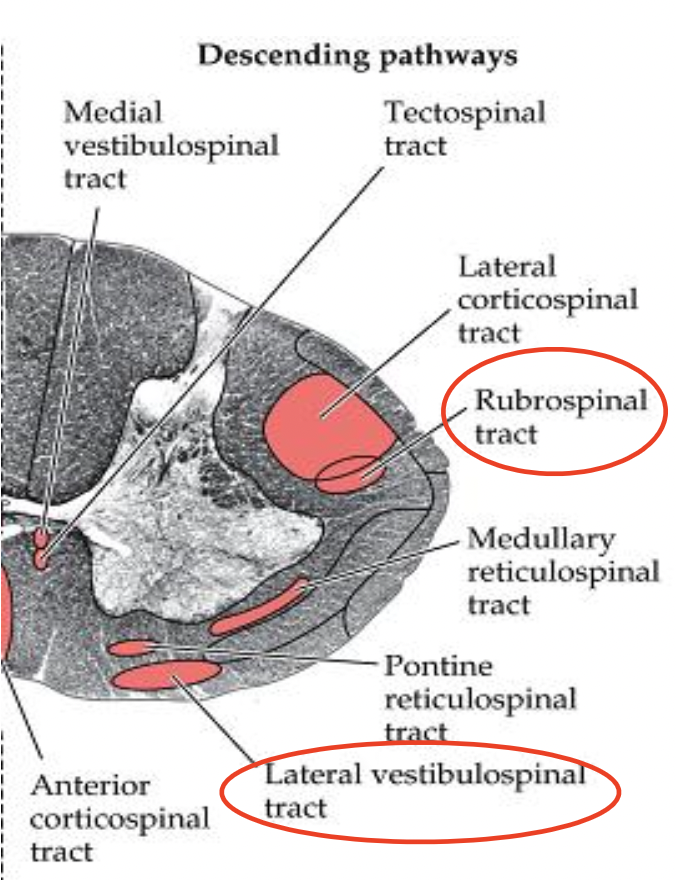
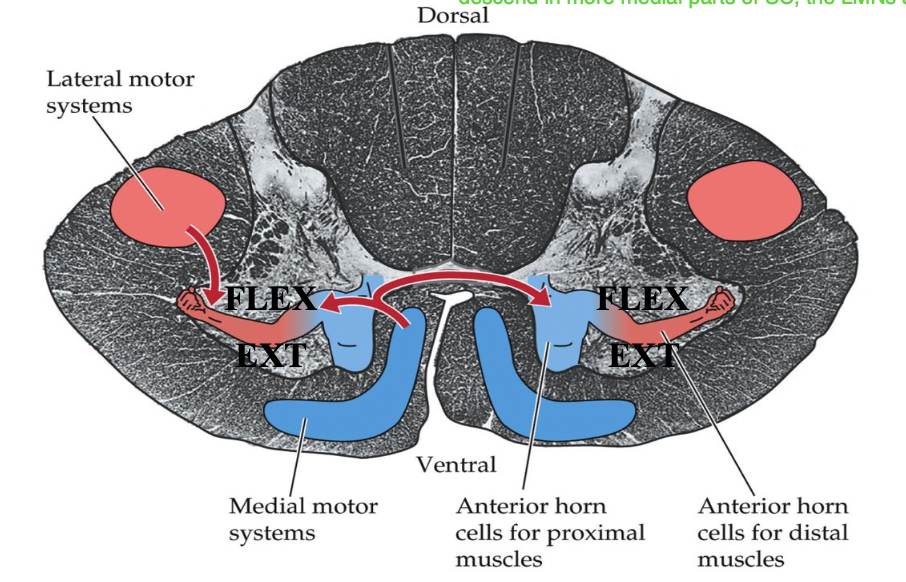
Where are medial motor pathways located in the SC? What are the four pathways?
located in the medial portion of the SC to synapse on medial motor nuclei in anterior horn (proximal musculature)
1) anterior corticospinal tract
2) vestibulospinal tract
3) reticulospinal tract
4) tectospinal tract
In the motor pathways, for more organization, where are extensor muscles usually located in the ventral horn? flexor muscles?
extensor muscle: anterior in the ventral horn
flexor muscle: posterior in the ventral horn
Lateral motor pathways - Lateral corticospinal tract:
site of origin?
site of decussation?
levels of termination?
function?
site of origin: primary motor cortex and other frontal and parietal areas
site of decussation: pyramidal decussation, at the cervicomedullary junction
levels of termination: entire cord (predominantly at cervical/lumbosacral enlargements)
function: movement of contralateral limbs
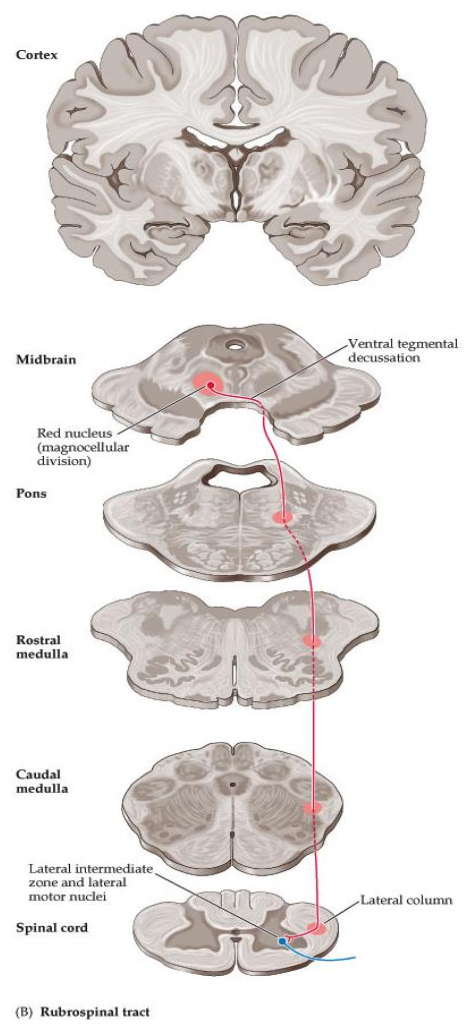
Lateral motor pathways - Rubrospinal tract:
site of origin?
site of decussation?
levels of termination?
function?
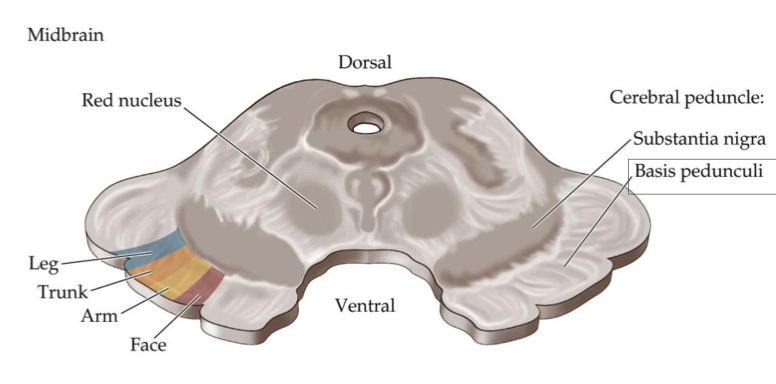
site of origin: red nucleus, magnocellular division
site of decussation: ventral tegmental decussation, in the midbrain
levels of termination: cervical cord
function: movement of contralateral limbs (function is uncertain in humans)
What is the most clinically important descending motor pathway? What does this tract control?
lateral corticospinal tract aka pyramidal tract aka corticospinal tract
- controls voluntary movements of the extremities (distal movements) on the opposite side of the body
In the lateral corticospinal tract, what is fractionation? What is this important for?
- ability to activate muscles independently of other muscles
- important for fine motor tasks
How many neurons are involved in the lateral corticospinal tract?
two neuron system/pathway
- UMN and LMN
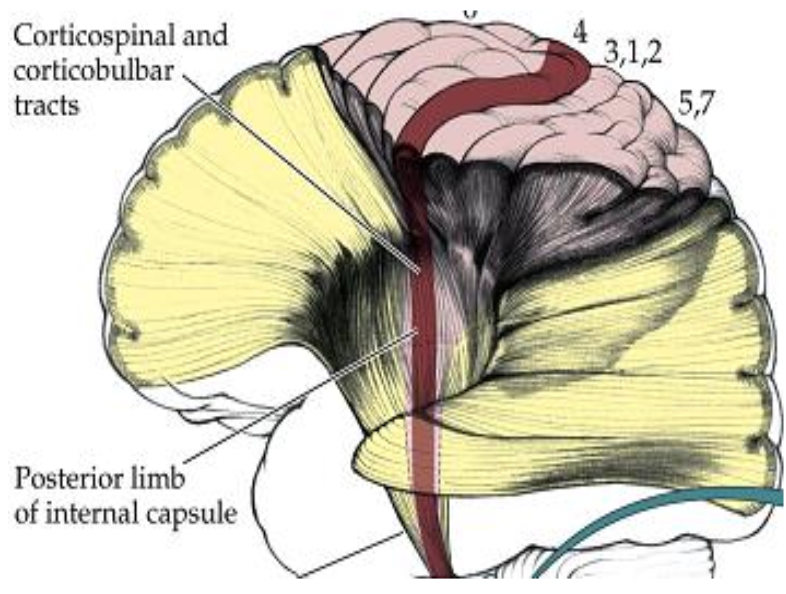
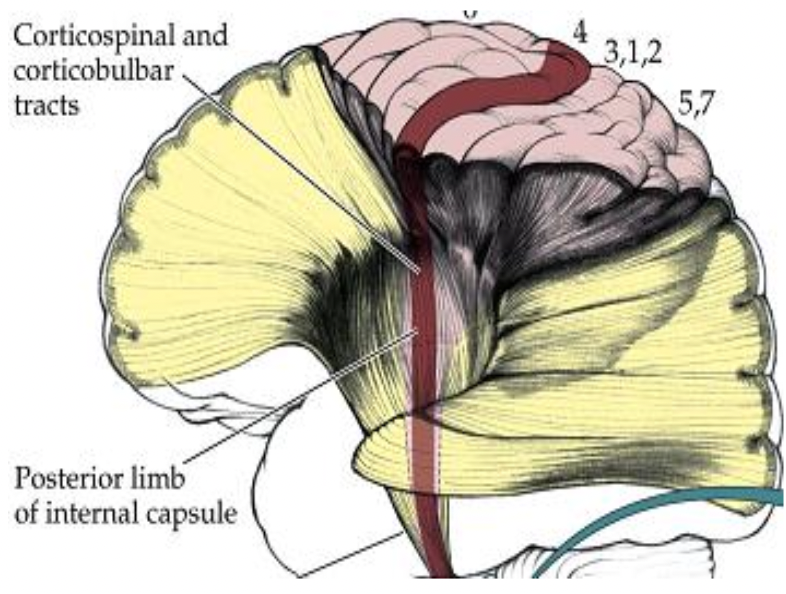
Where do majority of the corticospinal tract (CST) axons originate?
primary motor cortex (area 4) - precentral gyrus
In the corticobulbar tract, these are neurons from the ___ that synapse on motor neurons CN in the ____ to provide motor function to the ___.
In the corticobulbar tract, these are neurons from the CST that synapse on motor neurons CN in the brainstem to provide motor function to the face.
Why are the CST and corticobulbar tract sometimes described together?
since function of the corticobulbar tract is similar to the CST, and since it travels w/ the CST to the brainstem (CN nuclei) to innervate muscles in the face
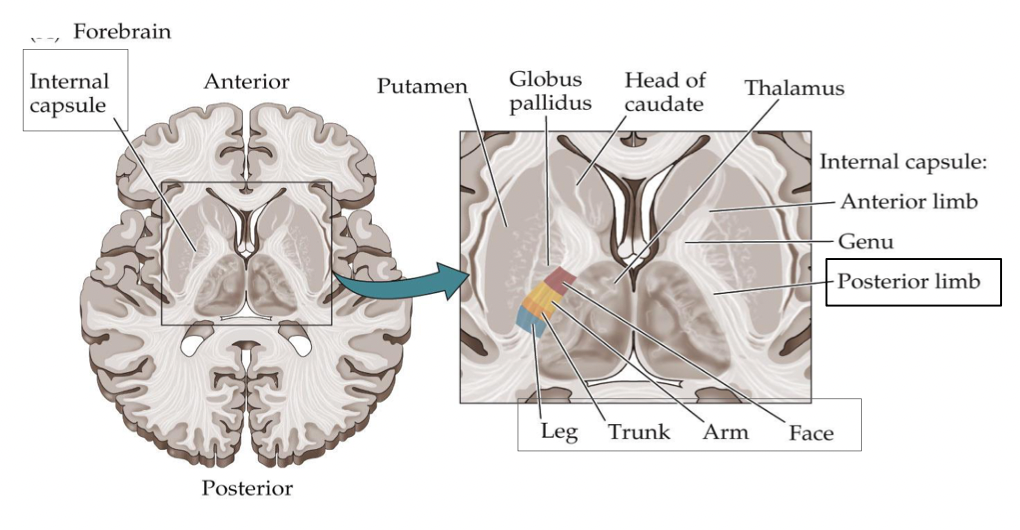
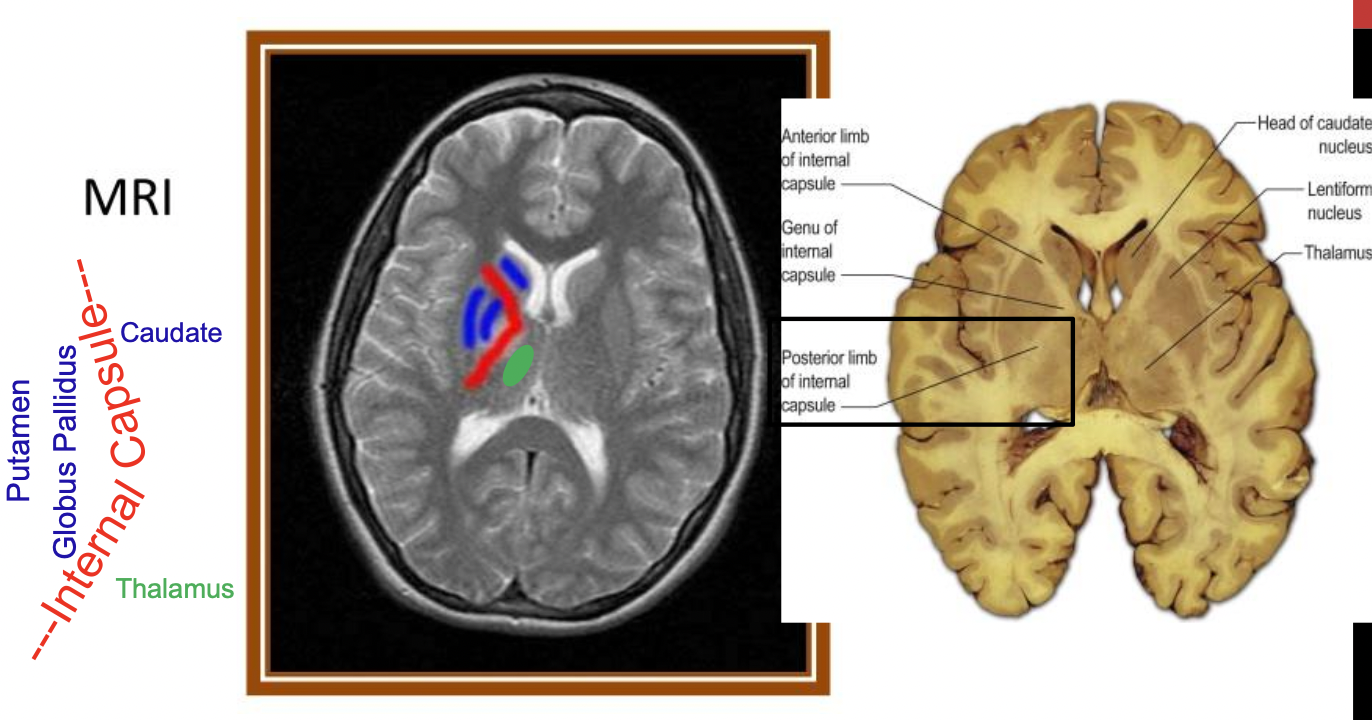
Where does the CST descend through first? What does it exhibit here?
first, CST descends through the internal capsule in the posterior limb
- exhibits somatotopy: this is not one of the two exceptions, so LE is going to be more lateral
After the internal capsule, where does the CST descend through?
through the midbrain
- middle 1/3 of the (anterior cerebral peduncle)
- exhibits somatotopy: lower extremities = more lateral, NOT one of the two exceptions
After the midbrain, where does the CST continue to descend?
in the ventral/anterior pons
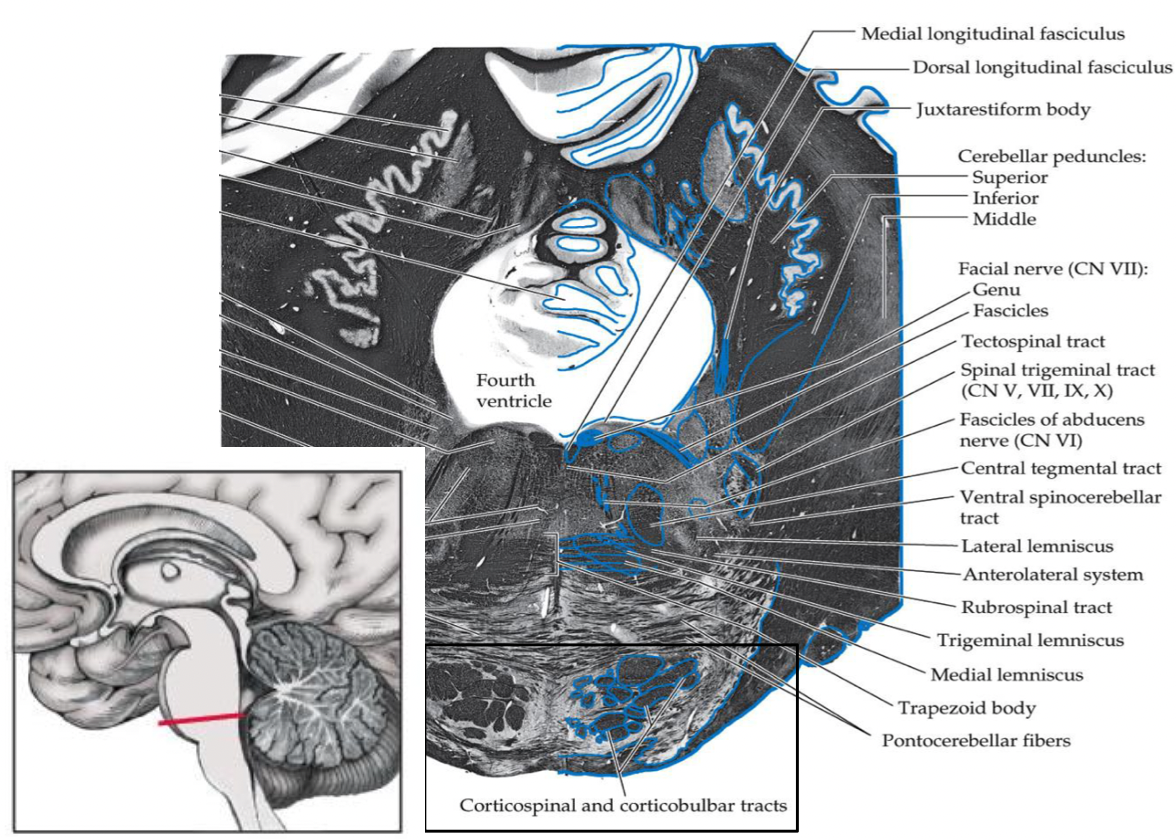
After the anterior pons, where does the CST descend through?
through the medulla - forms the medullary pyramid
At the inferior medulla, how much of the axons crossover? Where do they crossover? What is this the level of?
~85-90% of the axons crossover to the contralateral side at the pyramidal decussation (at the level of the cervicomedullary junction)
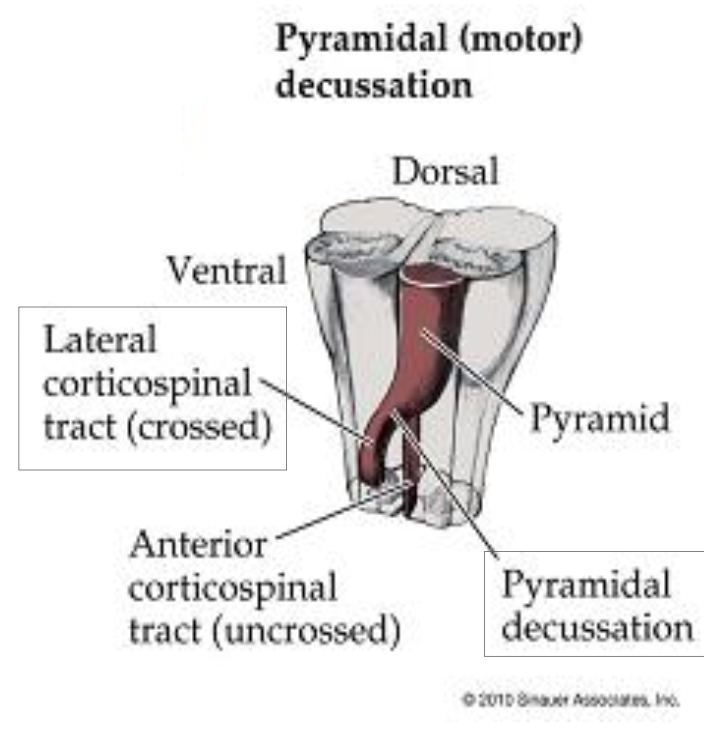
After the medulla, where does the CST descend?
in the lateral portion of the spinal cord
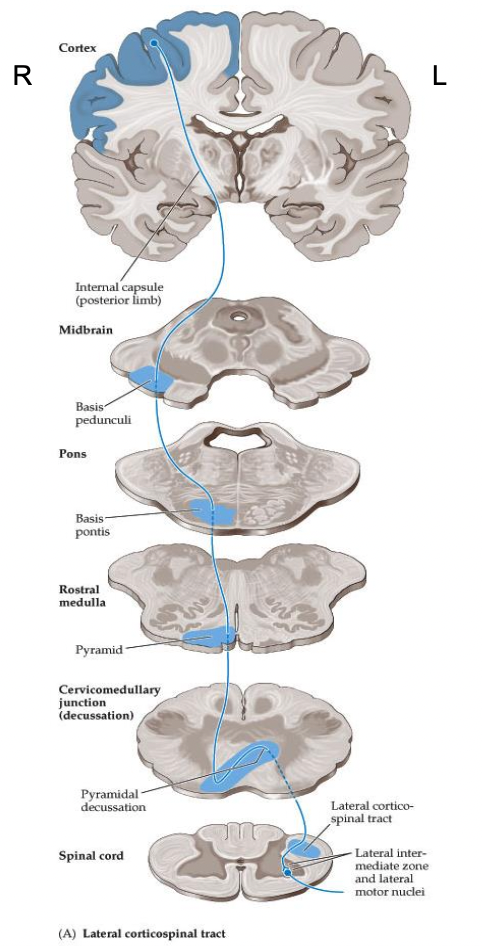
Where does the CST enter to synapse on LMNs? What is this responsible for?
enters the anterior horn to synapse on LMNs
- responsible for movement of contralateral limbs
L cortex controls R sided musculature of the body, vice versa
A lesion to the left CST in the spinal cord would affected which side of the body?
L side, because it has already crossed in the medulla
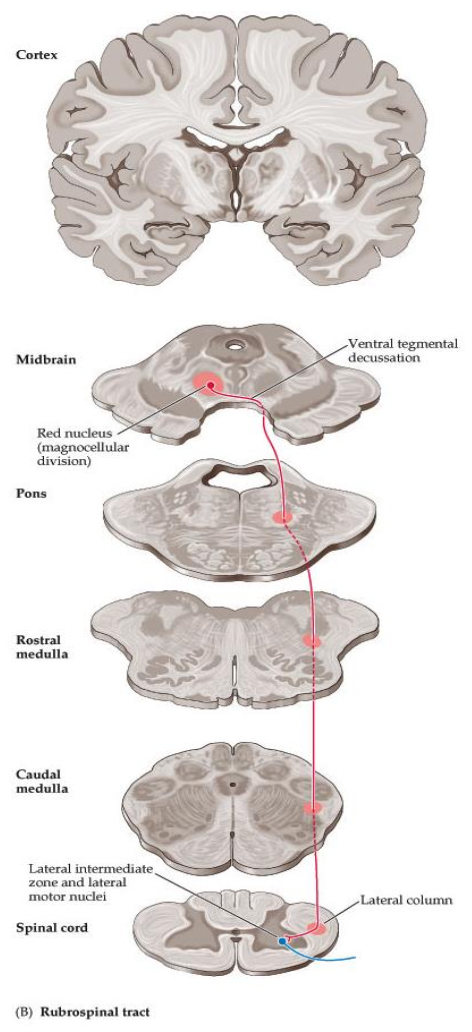
Where does the rubrospinal tract originate? Where does it cross over? Where does it descend to and enter to synapse?
Originates in red nucleus of the midbrain
Crosses over right away to the contralateral side at the ventral tegmental decussation
Descends in the lateral spinal cord to then enter the anterior horn to synapse on lower motor neurons
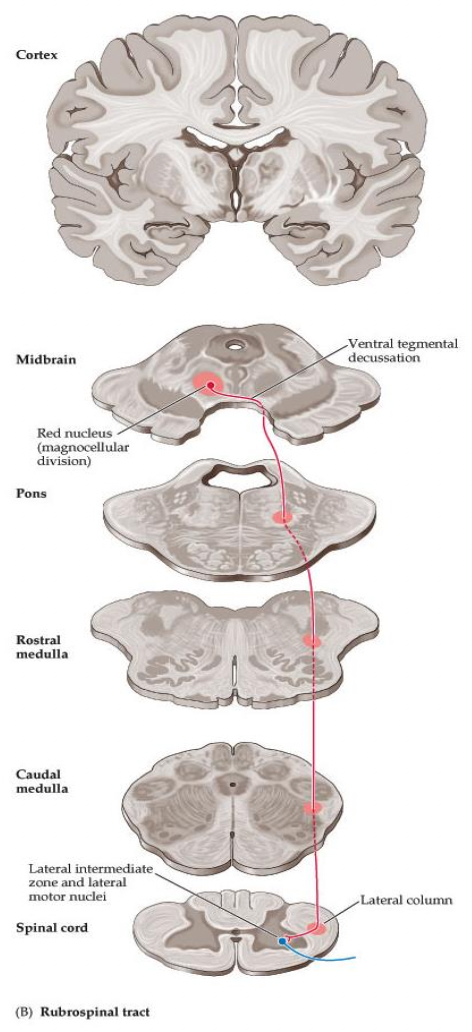
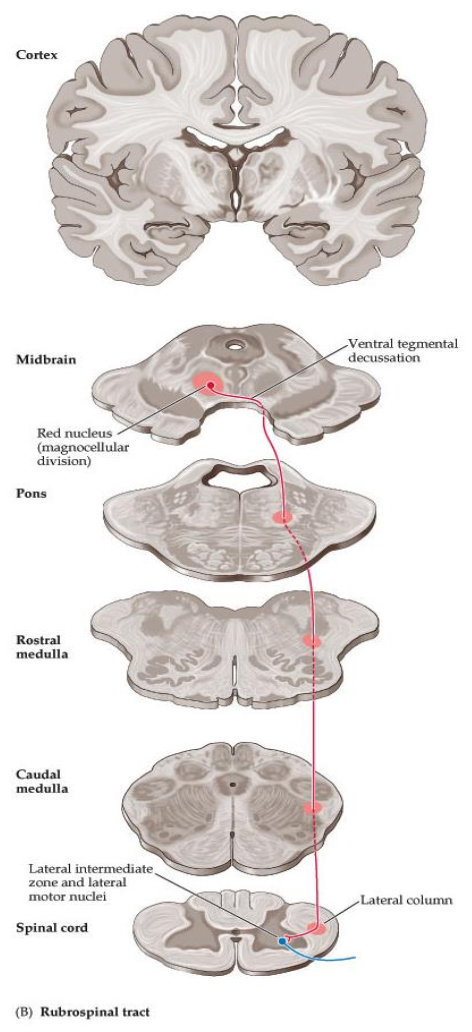
Where does the rubrospinal tract end? What movements does it control? How much contribution does it have to muscle control?
Ends in cervical spinal cord (UE movement)
Controls contralateral upper extremity distal musculature
Small tract, making a minor contribution to muscle control (uncertain in humans)