Female Reproductive System - HUBIO
1/63
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
What are the functions of the female reproductive system?
Produce the eggs/oocytes (gametes)
Provides a site for fertilization of oocytes
Preparation for ad support developing embryo and fetus
Maintains nourishes developing fetus and removes waste products
Generates cyclical changes: Menstrual cycle
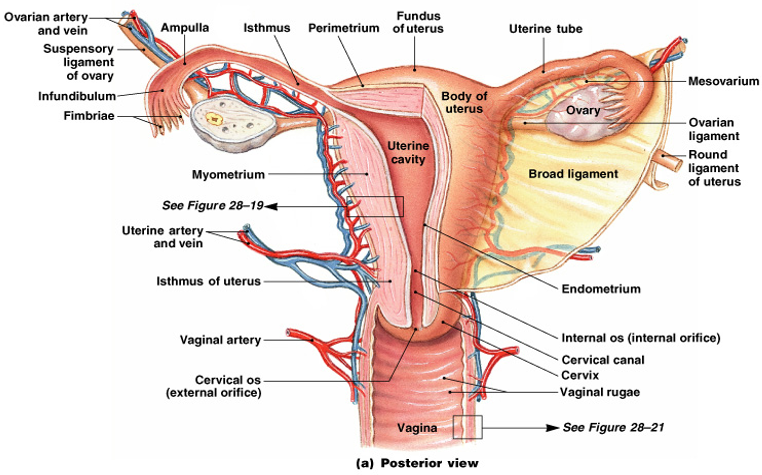
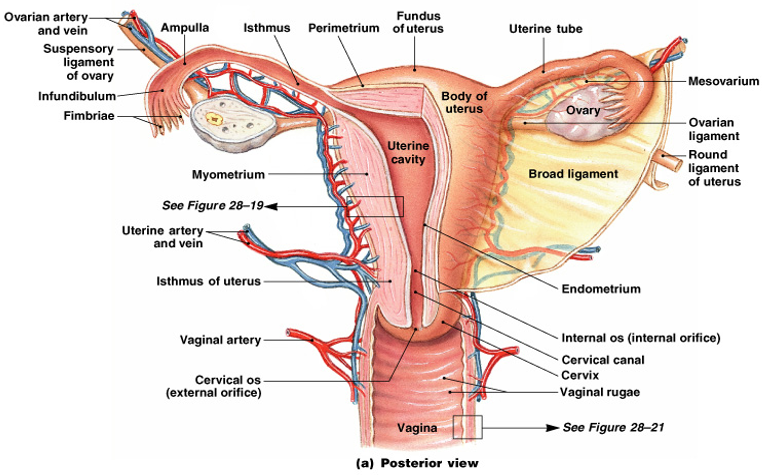
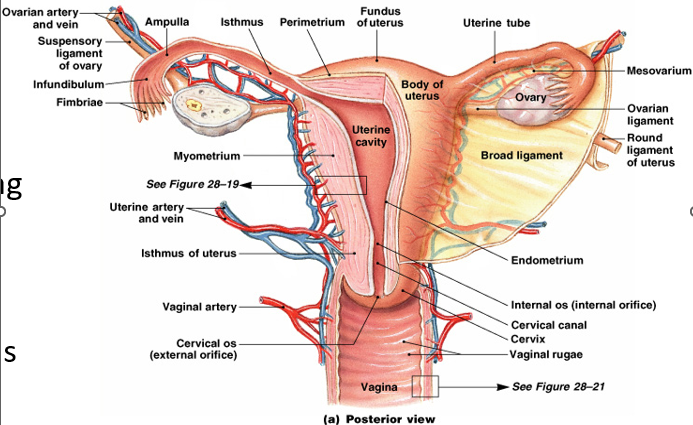
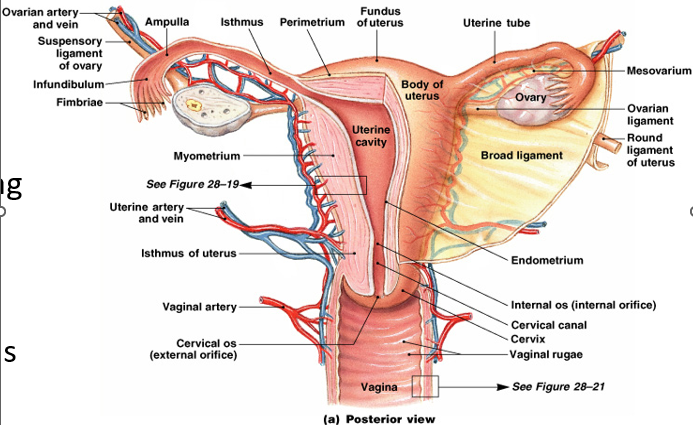
What is the vagina?
A tubular muscular organ that extends from the uterus to outside the body. It has muscular rugae (folds) that enable expansions to receive erect penis and a passage for delivery of children (birth canal). It also provides an outlet for uterine secretions and the menstrual cycle.
What is the outer vaginal wall called?
Adventitia (Fibrous Layer)
What is the middle vaginal wall called?
Muscularis (Muscular Layer)
What is the inner vaginal wall called?
Mucosa (Mucosal Layer)
What is the Fallopian Tube (Oviduct)?
It is an open ended tube leading from the uterus to the ovary. It is composed of a mucosa layer containing columnar epithelium and a muscularis layer. The terminal ampulla possess fimbriae that are ciliated.
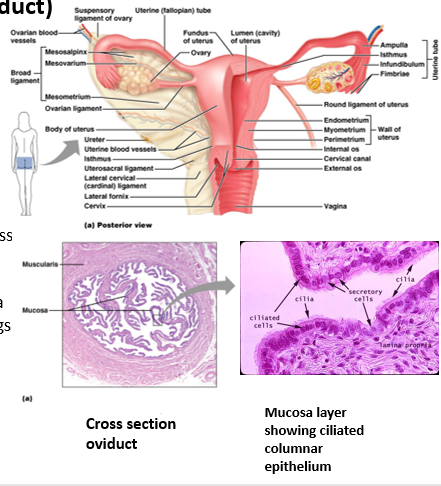
What is the purpose of the Cilia on the Fimbriae?
Beat rapidly to provide a current to direct ovulated eggs into the oviduct.
What is the main function of the Oviduct?
It is the location where fertilization typically occurs.
What is the Uterus?
A hollow, thick-walled organ located in the pelvis anterior to the rectum and posterior to the bladder. The entrance to it from the vagina is the cervix.
What is the function of the Uterus?
Receives, retains and nourishes the developing embryo.
What is the Outer layer of the Uterus called?
Perimetrium (serous membrane)
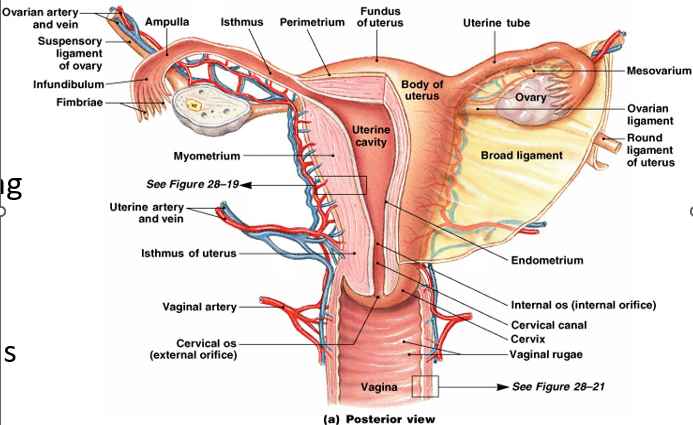
What is the Middle layer of the Uterus called?
Myometrium
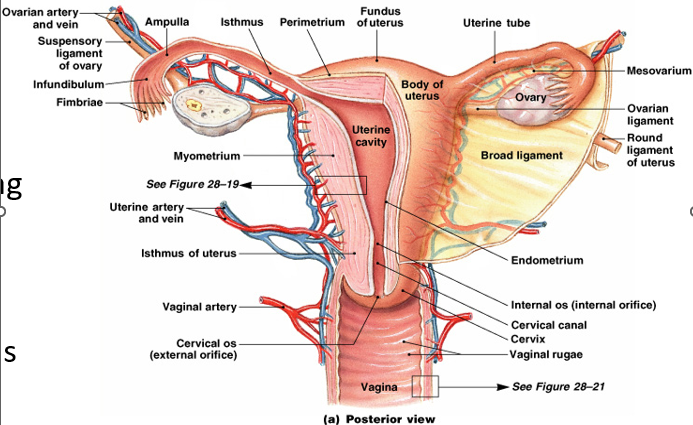
What is the Inner layer of the Uterus called?
Endometrium (mucosal lining)
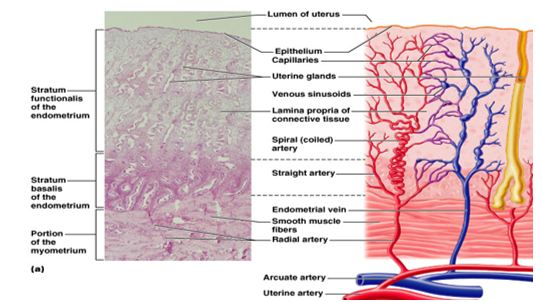
What are the 2 layers of the Endometrium?
Stratum Basalis - a permanent basal layer.
Stratum Functionalis - the luminal layer. This layer alters with the menstrual cycle, in preparation for the embedding of an embryo. It is shed if no embryo implantation occurs. Uterine glands secrete substances for embryo and extraembryonic tissue survival.
What holds the Ovaries in place?
Mesentery and Ligaments (broad, suspensory, and ovarian)
What is the innervation of Ovaries?
Sympathetic and Parasympathetic
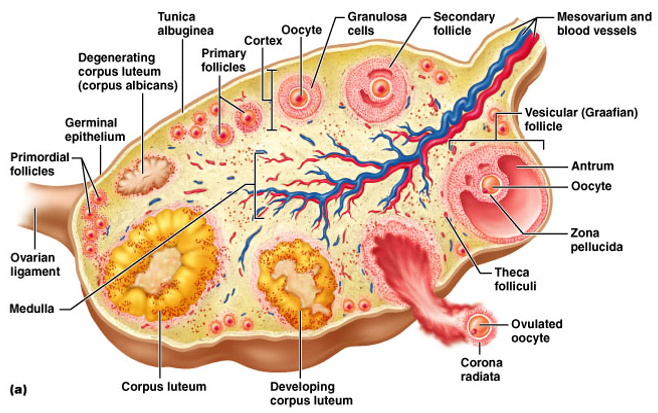
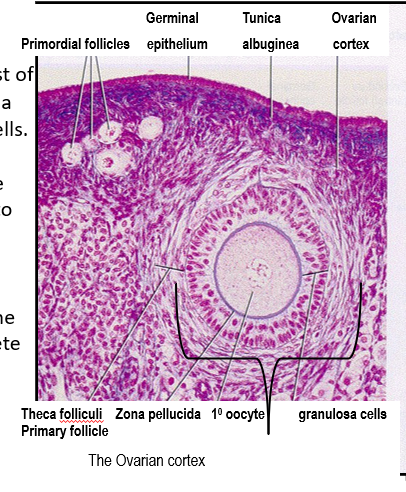
What is the structure of the Ovary?
Each pair of it is enclosed in a dense irregular connective tissue called the tunica albuginea. Beneath this capsule is the cortex, which contains the oocytes within ovarian follicles. The innermost medulla consists of loose connective tissue, blood vessels, lymphatics and nerves.
Oogenesis
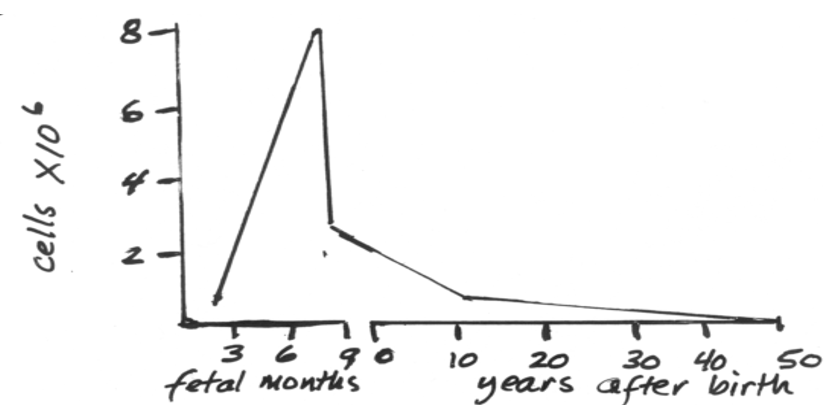
In human females, ovarian follicles develop about 105 days after conception. By birth, the ovaries contain about 2,000,000 oocytes. All are in Prophase I of meiosis, where they will remain until individual oocytes begin to mature at puberty. The maximum number of oocytes is determined prior to birth and the rapid decline of viable oocytes happens after 35 years of age.
What are Ovarian follicles?
They consist of an oocyte surrounded by a single layer of follicular cells. Later in development, the follicular cells multiply into several layers, known as granulosa cells. Granulosa cells nourish the oocyte and begin to secrete Estradiol as the follicle enlarges.
Phases of an Ovarian Follicle
As the 1° oocyte develops, the follicle’s granulosa cells multiply.
During the next phase, a cavity develops within the mass of granulosa cells, filling with follicular fluid.
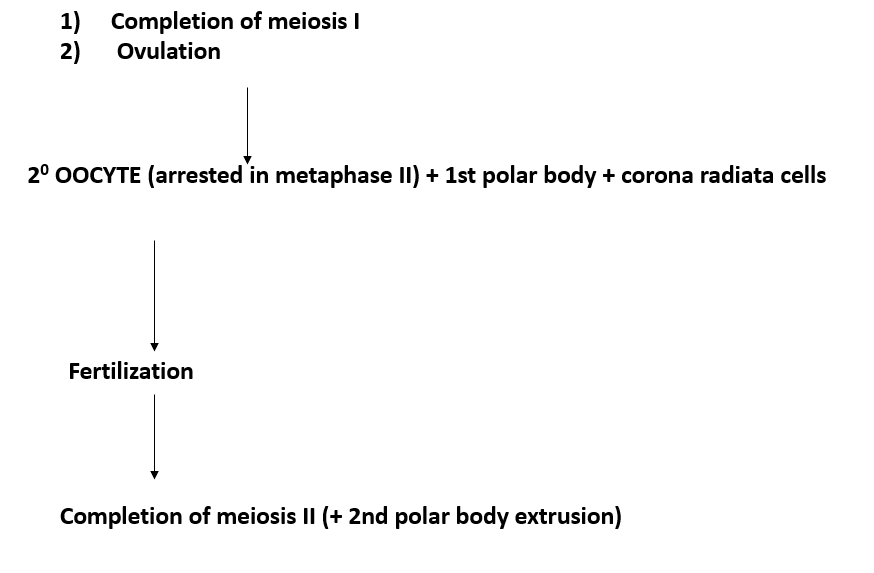
The 1st meiotic division occurs during this time. Cells surrounding the 2° oocyte are corona radiata. This is now a Graafian follicle.
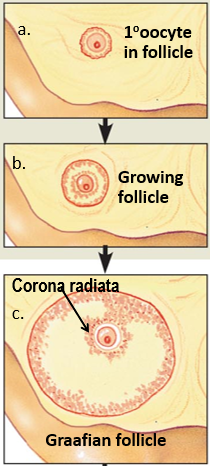
Phases of an Ovarian Follicle Continued
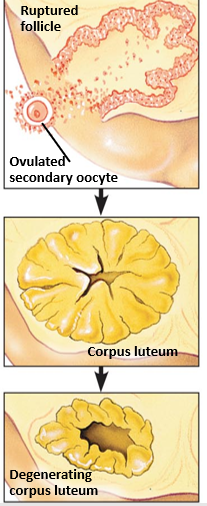
The Graafian follicle ruptures, releasing the 2° oocyte and the corona radiata.
The Corpus Luteum is the remnant of an ovulated mature follicle. It produces Estradiol, Relaxin, Progesterone, and Inhibin.
If implantation does not occur the Corpus Luteum degenerates into fibrous tissue the corpus albicans.
What happens before Ovulation?
Fimbriae, ciliated cells at the end of the Oviduct, move closer to the ovary. Their movement sweeps the oocyte into the oviduct. Once an oocyte is released from an ovary, it is transported via a fallopian tube (oviduct) to the uterus.
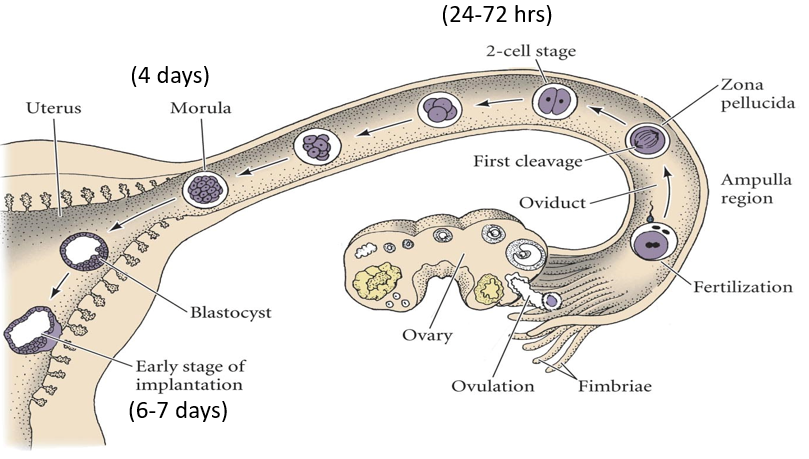
Where does fertilization happen if it occurs?
In the ampulla of the oviduct, and the embryo develops in the uterus.
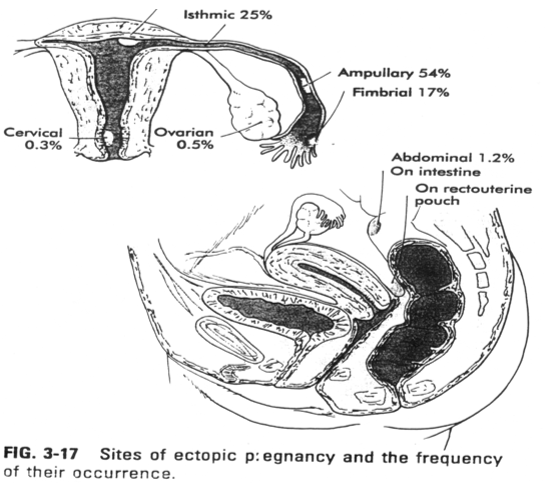
Ectopic Pregnancy
It is when an oocyte remains in the pelvic cavity or fallopian tube and is fertilized and begins development there.
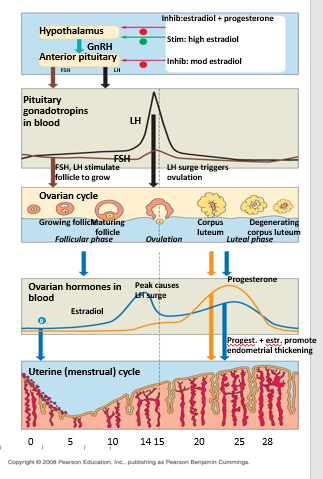
Menstrual Cycle
It is when the uterus prepares for implantation of an embryo. It begins from the first increase of uterine lining and ends when it shed. The average length is 28 days.
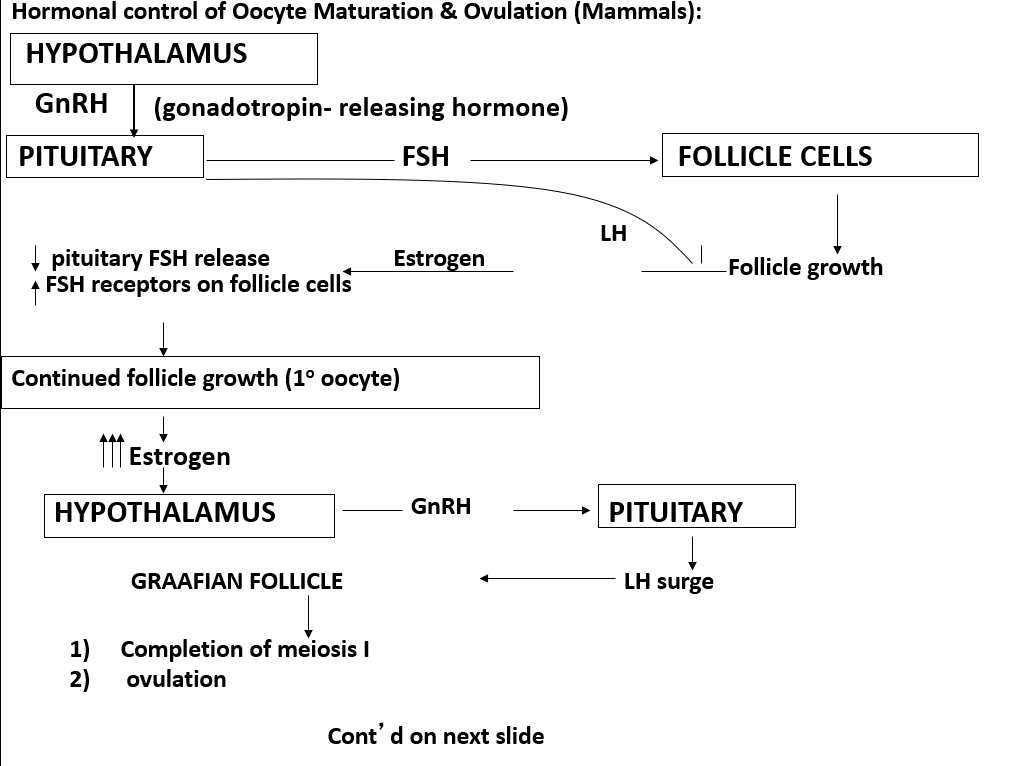
Gonadotropic releasing hormone (GnRH)
It is released by the hypothalamus and travels to the anterior pituitary gland, stimulating the release of follicle stimulating hormone, FSH, and luteinizing hormone, LH.
Follicle Stimulating Hormone (FSH)
Stimulates growth of an ovarian follicle.
Estradiol
It is the primary hormone released by the ovarian follicle.
Progesterone
It acts synergistically with estradiol to prepare the uterus for implantation.
What hormones are released by the Corpus Luteum?
Estradiol, progesterone, inhibin and relaxin
Inhibin
High levels inhibit LH and FSH.
Relaxin
Remodels collagen, increasing elasticity of pelvic joints and tissues of birth canal.
What happens when you have an increase in estradiol and progesterone?
GnRH is inhibited and therefore LH and FSH are also inhibited.
What happens when there is a slight increase in the level of estradiol?
FSH and LH are inhibited.
What happens when there are high levels of estradiol?
GnRH is stimulated and the FSH and a dramatic burst of LH.
Follicular phase: days 1-14 of the cycle
What happens on Day 1 of the follicular phase?
A slow increase in FSH starts follicle maturation. The follicle slowly enlarges, forming a swelling on the ovary wall. Usually, several follicles begin maturation; one develops faster than the others, secreting estradiol and inhibin. The slight increase in estradiol decreases FSH production and halts the development of other follicles. Occasionally, two follicles achieve codominance. If both are fertilized, fraternal twins are produced. As the primary follicle grows, estradiol production increases rapidly, stimulating the release of GnRH and causing a burst of LH at mid-cycle.
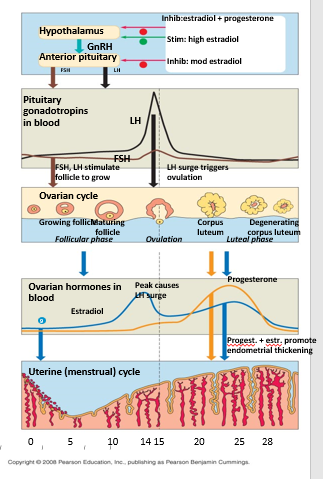
What happens on Day 14 of the follicular phase?
The follicle releases the secondary oocyte due a sudden surge of LH.
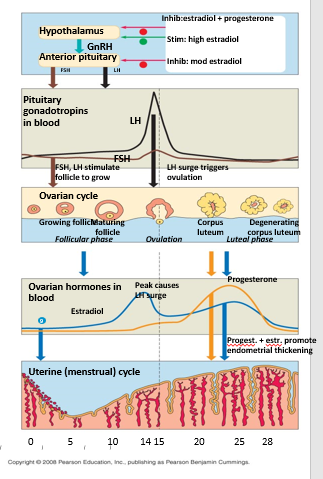
What happens int he luteal phase (Days 14- 28)?
After ovulation, LH stimulates the empty follicle to develop into corpus luteum. The corpus luteum secretes estradiol, progesterone, inhibin and relaxin. Estradiol and progesterone act together to support development of the uterine lining for possible implantation.
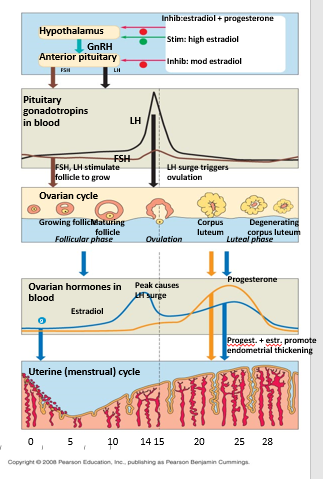
What happens during the menstrual phase?
The combination of estradiol and progesterone inhibits GnRH secretion, and therefore, LH and FSH. Decreased LH eventually causes atrophy (degeneration) of the corpus luteum, decreasing estradiol and progesterone. This causes the breakdown of the uterine lining (a.k.a menstruation). If the oocyte is fertilized, regression of the corpus luteum is averted because embryonic tissue is producing chorionic gonadotropic hormone. The maintenance of the corpus luteum continues the level of estradiol and progesterone, preventing the breakdown of the endometrium.
What happens during the menstrual phase of the Endometrial phases?
LH decreases, causing the corpus luteum to degenerate, decreasing estradiol and progesterone. The uterine lining breaks down. Day 1-5.
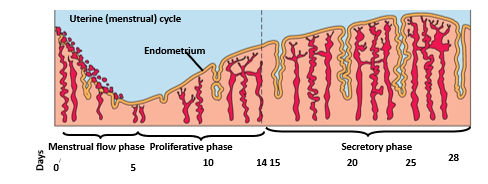
What happens during the proliferative phase of the Endometrial phases?
As granulosa cells begin secreting increasing amounts of estradiol, the lining grows. Day 6-14.
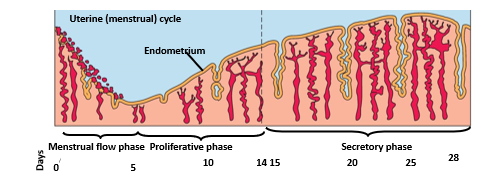
What happens during the secretory phase of the Endometrial phases?
Increased estradiol and progesterone cause the endometrium to become more vascular and glandular, and encourage glycogen deposition. Day 15-28
What is Endometriosis?
It is when some of the endometrium relocates to the abdomen, attaching to an organ and tapping into the neighboring blood supply. Each month under the stimulus of hormones, it will increase and then break down.
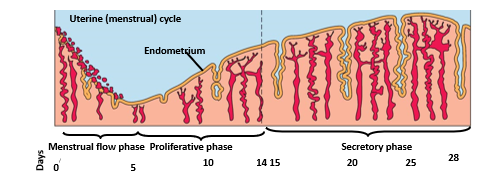
What happens if implantation occurs (Day 7-9)?
Some trophectodermal cells fuse to form syncytia. These syncytia proliferate and invade the endometrial extracellular matrix. The former trophectodermal cells, now called cytotrophoblastic cells, migrate between the syncytia followed by the fetal stroma. This will lead to the formation of the placental villi.
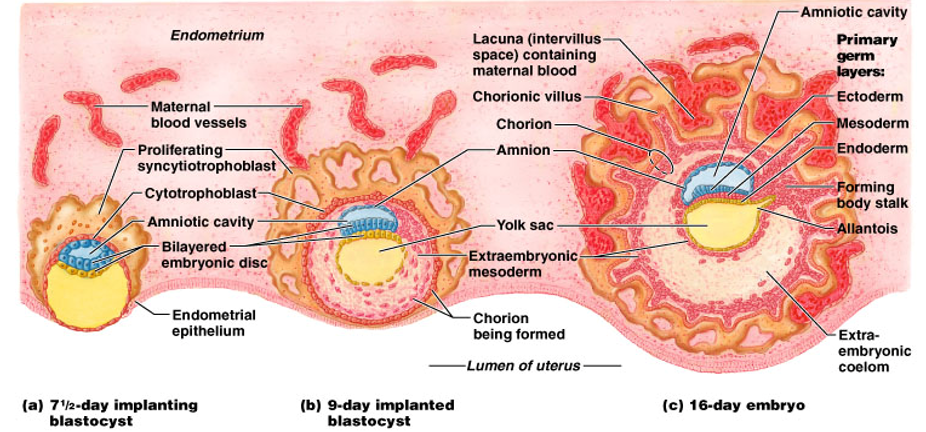
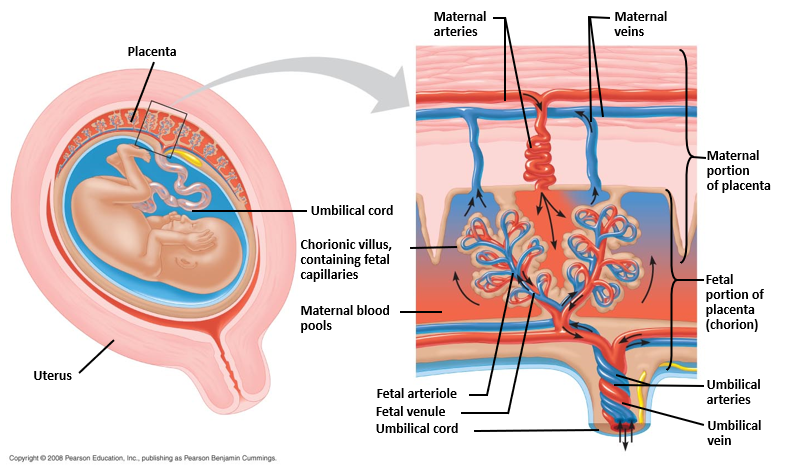
Fetal and Maternal Blood Circulation
The placenta is derived from the embryo and facilitate oxygen, nutrient and waste exchange. It begins to function around 5 weeks of development. The umbilical veins and arteries enter the capillary bed of the chorionic villus while maternal blood forms pools between the chorionic villus. Exchange is similar to that of a lung. Additionally since fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin – oxygen is stripped out from the maternal blood pools.
Reasons for Spontaneous Abortion and Miscarriage
Implantation of the embryo does not occur
Insufficient amounts of HCG to prevent the continuation of the menstrual cycle
Early developmental defects prevent embryonic development from proceeding
Insufficient amounts of progesterone production result in thinning and breakdown of the uterine lining
Abnormal implantation
Abnormal placenta
NB: Estimates are that 70% of fertilized eggs get miscarried, and about 30% of implanted eggs miscarry.
How long do sperm and oocytes live for?
Sperm live a maximum of 72 hours; oocytes:12-24 hours. Therefore, intercourse must occur within 72 hrs pre-, or 24 hrs post- ovulation to conceive.
What is a time barrier method of birth control?
Rhythm (tracking your menstrual cycle to predict ovulation)
What are mechanical barrier methods of birth control?
Condoms and Diaphragms
What are chemical barrier methods of birth control?
Creams, foams and spermicidal jellies (these are often not reliable alone so they are often used with a diaphragm)
What are oral contraceptive methods of birth control?
Synthetic estrogen and progesterone-like substances. They disrupt the normal pattern of GnRH release, preventing the LH surge needed for ovulation. Very effective, but possible side effects ( high blood pressure, nausea, etc.)
What is injectable contraception?
Intramuscular injection of progesterone derivative that prevents ovulation for 3 months.
What are contraceptive implants?
What is a Intrauterine device (IUD)?
A device placed in the cervix uterine cavity to interfere with implantation and block sperm movement by thickening cervical mucous. Some also secrete progestogen.
What are surgical methods of birth control?
Vasectomy and tubal ligation.
What does a morning after pill (RU486) do?
Binds to progesterone receptors; uterine proliferation ceases.
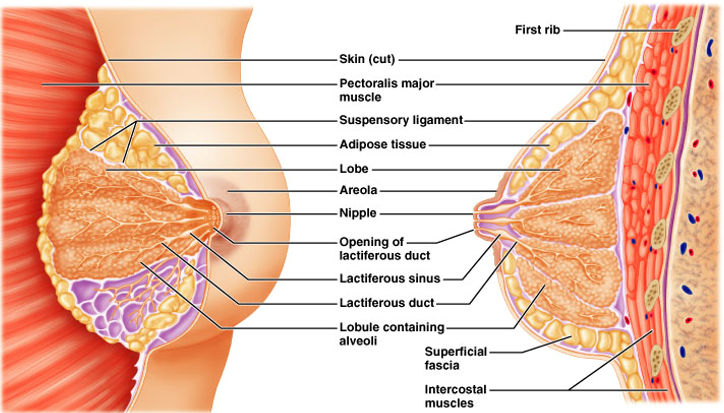
What are Mammary glands (breasts)?
They are modified sweat glands that typically only work in lactating females. They produce milk to feed the baby.
They respond to hormone stimulation (primarily prolactin and oxytocin from the pituitary).
The nipple is surrounded by a pigmented ring of skin, the areola
Mammary glands consist of 15-25 lobes
Each has a distinct compound alveolar gland opening at the nipple
Separated by adipose and suspensory ligaments
Smaller lobules composed of tiny alveoli or acini
— Like bunches of grapes
— Walls: simple cuboidal epithelium of milk-secreting cells
— Don’t develop until half-way through pregnancy (ducts grow during puberty)
Milk passes from alveoli through progressively larger ducts
— Largest: lactiferous ducts, collect milk into sinuses
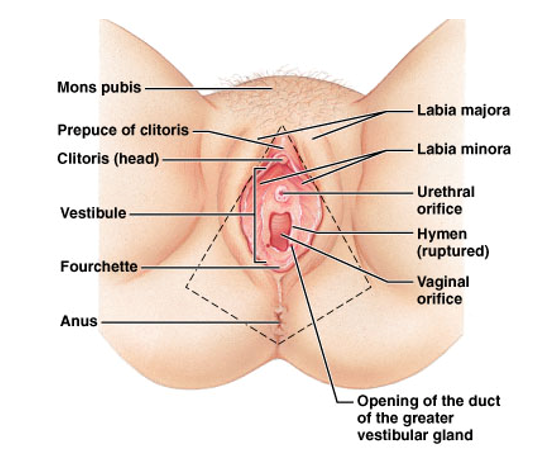
External Female Genitalia (Vulva)
Mons pubis
Labia majora
Labia minora
Vestibule
Clitoris
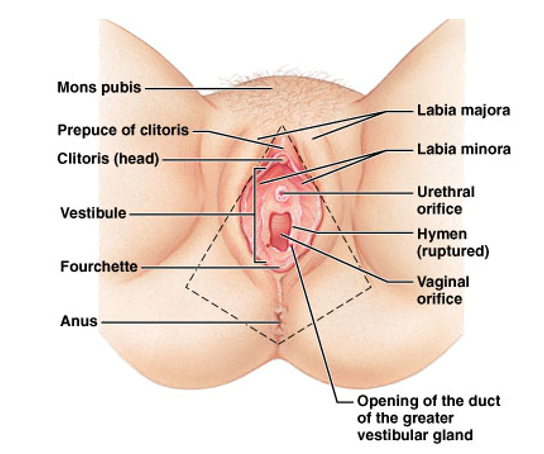
Mons Pubis
Fatty pad over pubic symphysis (hair develops after puberty)
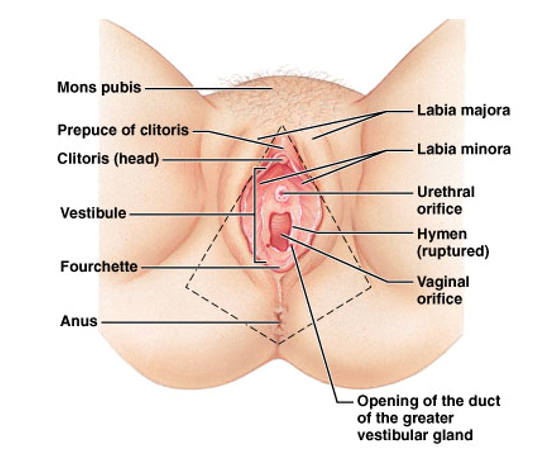
Labia majora
Long fatty hair-covered skin folds.
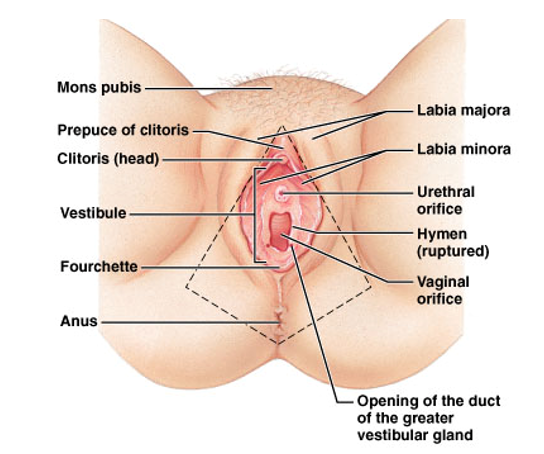
Labia minora
Thin, hairless, folds enclosing vestibule
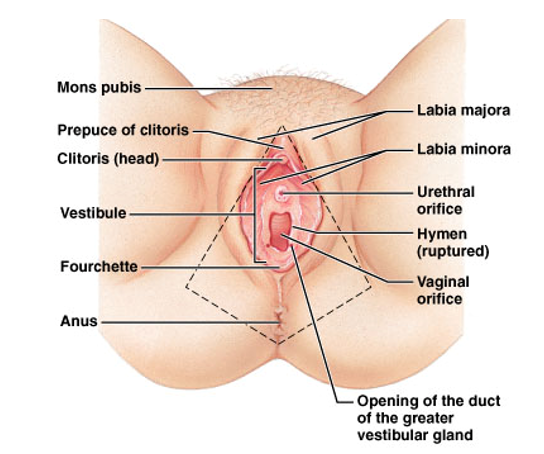
Vestibule
Houses external openings of the urethra and vagina
Urethra is anterior (drains urine from bladder)
Baby comes out of the vagina
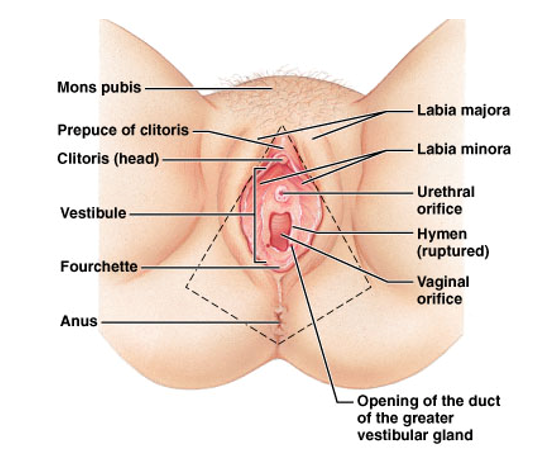
Clitoris
Anterior, homolog of penis (sensitive erectile tissue)