MLS 5202 Unit 7,8,9 Exam
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
List the body sites at which anaerobes are found as normal flora.
· Intestinal tract
· Urethra
· Vagina
· Oral cavity and upper respiratory tract
· Skin and mucus membranes
Name the genus that is the most abundant group of bacteria in the intestinal tract and oral cavity
Bacteroides
Name the organism that accounts for 43% of all clinical anaerobic isolates
Bacteroides
List 5 groups of anaerobes that together account for 2/3rds of infections
Bacteroides fragilis group
Porphyromonas and Prevotella
Fusobacterium nucleatum
Clostridium perfringens
ANA cocci
Give the ratio of anaerobes to aerobes in the G.I. tract, and the percentage of anaerobic bacteria found in the oral and nasal regions.
· Ratio (aerobes to anaerobes in GI tract): 1 to 1000
Define endogenous and exogenous infections.
· Endogenous: originates from one's own flora
· Exogenous: comes from the outside
Name the genus of the anaerobic organism that is responsible for the majority of exogenous infections and give the reason why it is able to survive as an exogenous organism.
· Clostridium
· The can form spores
Define polymicrobial infection and why anaerobes are less likely to be the sole organism in an infection.
· Endogenous infections where other NF "join in on the fun"
· Anaerobes are less likely to be the sole organism involved in infection because there could be other involved.
Recognize examples of conditions that predispose a patient to anaerobe-associated diseases
· Human or animal bites
· Aspiration of oral contents into lungs after vomiting
· Tooth extraction, oral surgery, traumatic puncture wound to oral cavity
· GI tract surgery or traumatic puncture
· Genital tract surgery or traumatic puncture
· Introduction of soil into wound
List the indications of anaerobic infections
· Infection near a mucosal surface
· Infection persists despite aminoglycoside therapy
· Foul odor, large quantity of gas
· Black color or brick red florescence
· Macroscopic sulfur granules
· Gram stain
List three metabolic pathways found in bacterial species and list the final electron acceptors of each.
· Respiration: inorganic compounds (usually oxygen)
· Anaerobic respiration: Nitrate (NO3), Sulfate (SO4), CO2
· Fermentation: acids and alcohols
Define the following terms: obligate aerobe, aerotolerant anaerobe, microaerophilic anaerobe, obligate, moderate, strict anaerobe, facultative anaerobe, capnophile
· obligate aerobe: grows only in the presence of O2
· aerotolerant anaerobe: unable to multiply in more than 2-8% O2
· microaerophilic aerobe: requires lower concentration of O2 - 2 to 10%
· obligate, moderate, and strict anaerobe:
Obligate: grows only in the absence of O2
Moderate: same as aerotolerant
Strict: cannot multiply in more than 0.5% O2
· facultative anaerobe: can use O2 if present, but can also grow anaerobically (most human pathogens)
· capnophile: grows in 5-10% CO2
List the gases and their percentages in the following laboratory incubator environments:
· air: 21% O2 and 0.03% CO2 (79% N2)
· microaerophilic:
· CO2: about 15% O2 and 5-10% CO2
· anaerobic systems: 0% - 0.5% O2
5-10% H2
5-10% CO2
80-90% N2
Define the term free radical (information also on Pg. 7-9) & the effect they can have on proteins, DNA, lipids, etc.
molecules that have an extra electron or too few electrons
Free radical cause damage to proteins, DNA and lipids because they are looking to give or take electrons from other sources. They denature DNA and proteins and damage the phospholipid bilayer because of this.
Creates a cascade of free radicals (one takes and electron from another and now the one taken from is a free radical).
Describe the specific effects free radicals can have on molecules that they come in contact with, and how many free radicals are produced each day in a typical human.
They take away or give an extra electron. A typical human cell produces 1 trillion toxic free radicals a day.
Give the name of the term for accumulated damage due to oxygen free radicals.
Oxidative stress
Describe what happens to our bodies ability to fight free radicals as we age.
Our ability to fight free radicals decreases as we age
Give the name of the body's natural defense against oxidative stress and list 3 examples and where they are found outside the body.
Antioxidants. Fruits, vegetables, and melatonin.
List and describe, in detail why O2 is so toxic to humans and to anaerobes.
· Oxygen is toxic to humans because it produces free radicals and toxic oxygen derivatives that cause cellular damage.
· Oxygen is toxic to anaerobes because the more anaerobic the bacteria the fewer enzymes and pathways the organism has to deal with oxygen.
List two enzymes that serve to eliminate free radicals and their toxic products, and list general relationships to these enzymes and different bacterial requirements for oxygen.
· Catalase and superoxidase dismutase
o Strict aerobe: catalase, superoxidase dismutase
o Facultative anaerobe: catalase, superoxidase dismutase
o Microaerophile: small amts of catalase, superoxidase dismutase
o Aerotolerant anaerobes: small amts of catalase, superoxidase dismutase
o Strict anaerobe: neither catalase or superoxidase dismutase
Give the chemical reaction a cell can use to eliminate toxic hydrogen peroxide.
2H2O2 --------> 2H2O + O2 (Catalase)
Describe why an aspirate is preferred to a swab for anaerobic specimen collection.
· An aspirate is preferred to a swab because there is no exposure to oxygen compared to a swab (exposed to O2 during collection)
Define PRAS in terms of transport and culture media
· PRAS (pre-reduced anaerobically sterilized transport and culture media).
List the steps involved in the proper set up of an anaerobic jar using a Gas-Pak system,
Plates are put into container
Gas pack envelope is placed inside container with indicator strip.
Container is closed.
What are the final atmospheric conditions for Gas-Pak system?
Generates CO2 and H2
Reduces O2 to 0.2%
Raises H2 and CO2 to 5-10%
o the QC method is used to indicate anaerobic conditions within the jar, and
If the indicator strip is white you're alright, if its blue you're screwed.
Aerotolerance test
Duplicate plates are used, one in the ANA chamber and one in the CO2.
Check for growth at 24-48hrs
Special potency antimicrobial disks (know specific susceptible and resistant patterns for various genera covered)
Reported as susceptible or resistant: Vancomycin (5 micro g), Colistin (10 micro g), Kanamycin (1 micro g), SPS (Sodium polyanethol sulfonate)
Reported as tolerant or susceptible: Nitrate disk, bile disk
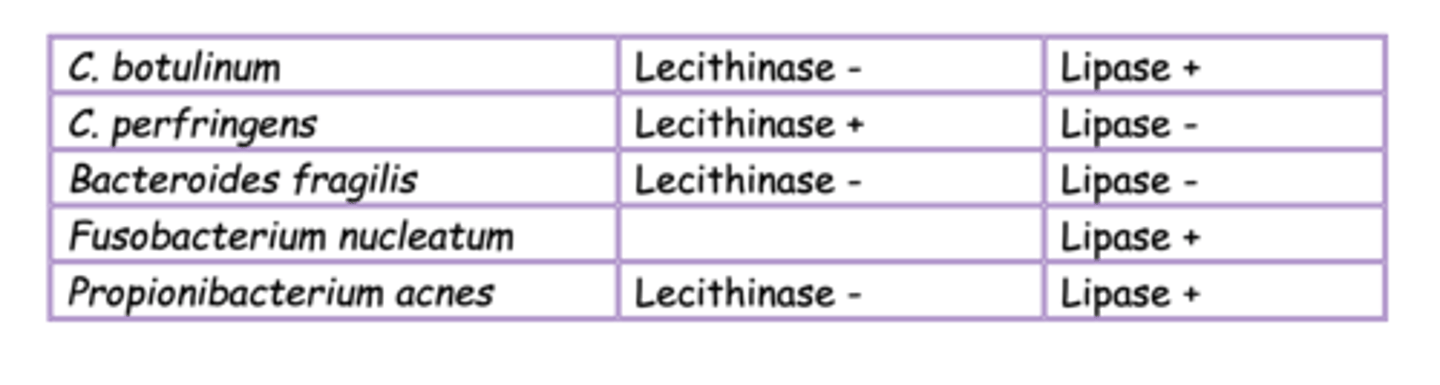
Egg yolk agar reactions (know specific results for various genera covered)
Biochemical ID systems (list one commercial system)
Analytical Profile Indentification (API)
GLC (define the term chemical fingerprint)
Gas liquid chromatography. A chemical footprint is specific chemicals that come up on GLC spectra that can help identify organisms.
Anaerobic Gram Negative Rods
Bacteroides
• Fusobacterium
• Porphyromonas
• Prevotella
Anaerobic Gram Positive Rods – sporeformers
• Clostridium
Anaerobic Gram Positive Rods – non sporeformers
• Actinomyces
• Propionibacterium • Bifidobacterium
• Eubacterium
• Lactobacillus
• Mobiluncus
Anaerobic Cocci
• Gram positive: Peptostreptococcus
• Gram negative: Veillonella
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: · Bacteroides fragilis
o Most abundant group of bacteria in intestinal tract, oral cavity, vagina
o Gram stain: short G neg pleomorphic rods
o Resistant to K, V, C
o Grows on KVLB agar
o Bile tolerant on BBE
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Fusobacterium nucleatum and F. mortiferum
NF in URT, GI tract, urethra
Gram stain: Fusobacterium nucleatum: G neg long thin tapered rods
F. mortiferum: G neg globular swellings and bizarre shapes (pleomorphic forms)
Vancomycin: R
Kanamycin: S
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification:
Porphyromonas and Prevotella spp.
NF in the oral cavity
Gram stain: G neg pleomorphic rods
Bile sensitive / pigmented species group
Prevotella melaninogenica: pigment is enhanced on KVLB (resistant to K and V). Black to brown pigment Brick red florescence (woods lamp) Porphyromonas asaccharolytica: NG on KVLB (R to V and C) SBA – brown to black pigment Fluorescence (woods lamp)
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Clostridium perfringens, C. histolyticum, C. tetani, C. botulinum, and C. difficile
Clostridium perfringens: Normal intestinal flora of humans (causes endogenous infections) Gram stain: large G pos box car rods (cultures older than 6hrs may stain variable) SBA ANA: Aerotolerance test Colony morphology: large irregular margins Special potency disks: CL (resistant), K (S), V (S) Egg Yolk agar: lecithinase pos, lipase neg Reverse CAMP: S. agalactiae instead if S. aureus streaked down the middle.
C. histolyticum
C. tetani: Exogenous in origin Intestinal flora of humans and animals (25%) Gram stain: G pos tennis racquet shape
C. botulinum: Gram stain: G pos bacillus
C. difficile: NF in 5-10% of the population Tox A and B ELISA CCFA agar: cycloserine, cefoxitin, fructose Gram stain: large Gram pos rods, box cars
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Actinomyces israelii
NF of oral oropharynx and vagina
Gram stain: G pos branching filaments
Sulfur granules: macroscopic colonies seen in abscesses
Slow growing: 1-2 weeks
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Propionibacterium acne
Predominant NF of skin and NF of colon
Common contaminant of blood cultures
Lipase: pos
Gram stain: pleomorphic G pos rods. Referred to as ANA diphtheroids
Catalase: pos
Spot indole: pos
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Mobiluncus spp., Bifidobacterium spp., Eubacterium spp., Lactobacillus spp.,
Bifidobacterium spp., Eubacterium spp., Lactobacillus spp: NF of GI tract and NF of vagina Low virulence Sometimes found in polymicrobial infections Gram stain: G pos rods
Mobiluncus spp: NF of vagina May play a role in bacterial vaginosis Curved G pos rods (stains G neg)
For each of the following anaerobic genera, list the normal flora sites (if any), and specific methods of lab identification: Peptostreptococcus anaerobius, and Veillonella spp.
Peptostreptococcus anaerobius: NF of oral cavity, colon, vagina Gram stain: G pos cocci in chains Sensitive to SPS: Sodium Polyanethol Sulfonate GLC: isocapronic acid
Veillonella spp: NF of oral cavity Gram stain: small G neg cocci
Veillonella parvula
List the primary media that could be used for anaerobic specimens (including aerotolerance test media).
· Aerotolerance test: SBA and CHOC
· Egg yolk agar
· BBE (bacteroides bile esculin)
· KVLB (Kanamycin, Vancomycin, Laked blood)
· CCFA (cycloserine, cefoxitin, fructose)
· PEA
· SBA
Explain the utility of thioglycollate broth with the recovery of anaerobic bacteria.
Nonselective for cultivation of anaerobes as well as facultative anaerobes and aerobes
Identify the major divisions of mycobacteria and the species associated with each.
1. Mycobacteria Tuberculosis complex
a. M. tuberculosis
b. M. bovis
c. M. africanum
2. Nontuberculous Mycobacteria (NTM)
a. M. avium-intracellulare complex
i. Opportunistic pathogen in AIDS patients
ii. 30-50% infection rate
iii. Disseminated infection, can occur in all organs
b. M. leprae – leprosy
Define MAC in terms of mycobacterial species and how its affect individuals with AIDs.
· MAC: M. avium-intracellular complex
· Opportunistic pathogens
· Mostly infect immunocompromised
· AIDS patients: 30-50% infection rate, disseminated infection, can occur in all organs
· Ubiquitous in nature (found just about everywhere)
Diagram and compare the cell wall of mycobacteria to Gram negative and Gram positive bacteria.
· Mycobacteria have a think layer of mycolic acid above the arabinogalactan and peptidoglycan layer.
List and explain the advantages and disadvantages of the mycobacterial cell wall.
· Contributes to environmental survival of the organism
· Protects from host defenses
o Intracellular parasite
· Resistant to most antibiotics
· Makes it difficult for cell to get nutrients in
o 2-6 weeks to form a visible colony on lab media
Compare the generation time of M. tuberculosis, rapid and slow growers to that of E. coli.
· M. tuberculosis: 20hrs
· Rapid growers: 12hrs
· Slow growers: 24hrs
· E. coli: 20 mins
List the staining procedures that are used for mycobacteria, describe the steps of the two acid fast stains, explain the advantage of the auramine-rhodamine fluorochrome stain.
· Ziehl-Neelsen stain
o Primary stain - carbolfuchsin
§ Heat with Bunsen burner until steams
§ Then sit for 5 mins
o Decolorize with 0.5% HCL / 70% ethanol - 3 mins
o Counterstain with methylene blue for 1 min
o Mycobacteria - reddish bacteria
o View with 100x oil lens
· Kinyoun stain
o Same as Ziehl-Neelsen but not heated
o View with 100x oil
§ 300 fields or 15mins to call negative
· Auramine-rhodamine fluorochrome stain
o More sensitive than carbolfuchsin stains
o Require fluorescence microscope / filter
o Yellow green rods / black background
§ Viewed with 40x objective
Explain the basis of the Runyon classification scheme used for NTM. Name and define the two categories of pigment production used to classify mycobacteria.
· Runyon classification: Four groups based on pigment and growth rate
· Two categories:
o Photochromogens: produce pigment only in the presence of light
o Scotochromogens: produce pigment in light or dark
Explain the safety precautions that are required when processing a possible mycobacterium specimen, and explain the digestion and decontamination procedure and explain why each step is necessary.
· Sputum cultures collected in special containers to prevent aerosols
· All requests must be clearly designated:
o Culture for AFB
o Culture for mycobacterium
· Must be processed with
o Face shield
o Biohazard hood- level 3
o Mycobacteria labs have negative pressure
· Processing procedure for sputum samples
o Digestion
§ Liquify sample
§ Digest proteinaceous material
§ N-acetyl-L-cysteine (NALC) - mucin (mucous)
o Decontamination
§ Kills non-mycobacterial organisms prior to plating
§ 2% NaOH - kills off most NF and some mycobacterium
o Centrifugation and concentration
List examples of specialized media used for mycobacteria.
· Lowenstein-Jensen (others)
o Fresh whole eggs, potato flour, glycerol + malachite green
· Middlebrook agar 7H10
o Serum albumin
· Middlebrook broth 7H9 + others
o BACTEC systems - Becton Dickinson Diagnostic
List the general methods used to identify of mycobacteria.
· Growth rate and pigmentation
· Biochemical tests
· HPLC - mycolic acid profile
· DNA probes
List the species that cause TB, the number of people infected worldwide, and then describe the symptoms and possible outcomes of TB infection. List the term that is commonly used to describe the patient wasting away.
· Species that cause TB: M. tuberculosis, M. bovis, M. africanum
· Number of people infected worldwide: 1.7 billion
· Symptoms of pulmonary TB
o Low grade fever
o Night sweats
o Fatigue
o Anorexia (low appetite) and weight loss
o Symptoms similar to pneumonia – chronic persistent cough
o Consumption: patient wasting away
Explain how a TB skin test is done, what PPD stands for, what is used as a confirmation if the test is positive.
· The skin test is done by injecting the PPD intradermally. You are not looking for redness but for a raised hard area.
· If the patient is hypersensitive there will be a 10-33mm zone
o This indicates that you have a TB infection or have been exposed to TB.
· If pos, confirm with a culture or chest x-ray
· PPD: Purified Protein Derivative
Name the vaccine that is used to prevent TB, and its three letter abbreviation.
· BCG: Bacille Calmette-Guerin
List the drugs that are used to treat individuals with TB.
· Isoniazid (INH) + rifampin and others
List the nontuberculosis mycobacteria species, along with the site and type of infection that each causes.
· Mycobacteria causing pulmonary infections
o Mycobacterium kansasii
§ Found in water
o Mycobacterium avium complex (MAC) (M. avium, M. intracellulare)
§ Grouped together because they are hard to differenitiate
· Mycobacteria causing non-pulmonary infections
o Mycobacterium fortuitum – causes soft tissue infections
§ Rapid grower < 7 days and grows on MacConkey plates
o Mycobacteria marinum – causes salt and fresh water skin infections usually from open wounds in the skin
o Mycobacteria scrofulaceum – causes cervical lymph infections where lymph nodes on neck swell up
· Mycobacterium leprae
o One of the oldest recorded disease
o Also known as Hanses disease after G.A, Hansen who first identified M. leprae in 1873
o 70% of cases come from India, Indonesia, Myanmar.
o Two forms: tuberculoid leprosy, lepromatous leprosy
o Only bacteria to attack peripheral nerves in humans.
o Incubation can be up to 10 years before symptoms appear
o Very curable
o Cannot be cultured and grows best in armadillo footpads
For the following clostridia spp., describe their respective diseases, symptoms, toxins produced, treatment and prevention: Clostridium perfringens
o Intestinal flora of humans. Endogenous infections
o Food poisoning: caused by type c strain. Enterotoxin producing strain. Rich meats and stews. Severe abdominal pain and often bloody diarrhea.
o Necrotic inflammation of small intestine
o Fatal without treatment
o Gas gangrene: myonecrosis. Also caused by C. histolyticum.
o Exotoxin (Alpha toxin) cause tissue necrosis and large amounts of foul smelling gas.
o Treated with debridement of necrotic tissue, hyperbaric O2, antisera against alpha toxin, antimicrobials (to a lesser degree).
For the following clostridia spp., describe their respective diseases, symptoms, toxins produced, treatment and prevention: C. tetani
o Causes tetanus
o CNS toxin: causes continuous excitation of motor neurons in spinal cord. Sustained contractions occur in spastic paralysis.
o Can be prevented with vaccine
§ Dtap: infants and children
§ Tdap: one time dose for adolescents and adults
§ Td: children and adults
For the following clostridia spp., describe their respective diseases, symptoms, toxins produced, treatment and prevention: C. botulinum
o Causes botulism by ingesting preformed toxin
o Toxin in the most poisonous substance known. It's a neurotoxin that binds to cranial nerves.
o Prevents acetylcholine
o Death by paralysis of diaphragm
o Can be prevented by boiling contaminated food or adding a nitrate additive
For the following clostridia spp., describe their respective diseases, symptoms, toxins produced, treatment and prevention: C. difficile
o Antibiotic-Associated Enteritis: inflammation of the intestinal tract which leads to diarrhea
o Pseudo membrane colitis: fibrous pseudo membrane that covers the mucosa of the colon.
o Toxin A: enterotoxin
o Toxin B: cytotoxin
§ Both can be detected using an ELISA test
o CCFA agar: cycloserine, cefoxitin, fructose
o Gram stain: large Gram pos rods box cars
Compare the effect of the toxin from C. tetani to the C. botulinum toxin.
C. tetani: CNS toxin causes excitation of motor neurons in spinal cord
C. botulinum: Binds to cranial nerves and prevents release of acetylcholine
Describe the hemolytic reaction of C. perfringens
Double zone of beta hemolysis. Inner zone is complete and outer zone is partial.
Describe the use of CCFA and its components
CCFA agar is used for the ID of C. difficile. It contains cycloserine, cefoxitin and fructose.
List 3 etiological factors in the development of acne
Increased serum production, hypercornification of follicle ducts, and altered metabolism of cutaneous microflora such as Propionibacterium acnes.
Explain how P. acnes is involved in the formation of blackheads
P. acnes produces lipases that hydrolyze sebum triglycerides to free fatty acids. The free fatty acids or their oxidation products may be involved in the formation of blackheads
List two other organism that are also normal flora of the sebaceous follicles
Staphylococci and yeasts
Know the resistance to special potency disks for each genus
o Fusobacterium: vancomycin
o Preveotella: vancomycin and kanamycin
o Porphyromonas: vancomycin and colistin
o Bacteroides: kanamycin, vancomycin, colistin and tolerant to bile disk
o Clostridium: colistin
o Peptostreptococcus anaerobius: SPS disk
Define obligate intracellular parasite.
· Organisms that can only reproduce inside of their host cell
List and describe the unique characteristics of Chlamydia.
· Once thought to be a virus
· Must be grown in tissue culture
· Once thought to be a n energy parasite
o Cannot make its own ATP
o Parasite: two organisms living together, one physically dependent
· No peptidoglycan in cell wall
· Unique development cycle
o Elementary bodies (EB)
o Cell wall enables organism to survive outside host for limited time
o Infects cells that line conjunctiva, respiratory tract. Urogenital tract and rectum.
Describe the developmental cycle, and name the two forms or bodies involved in the cycle.
· Tiny cocci called Elementary bodies
· Large pleomorphic reticulate bodies
· Cycle:
o EB enters host cell by triggering its own endocytosis,
o Once inside endosome it turns into a RB
o RB replicates rapidly into multiple RB's
o Once an infected vesicle becomes full on RB's it becomes an inclusion vesicle. 21hrs after infection the RB's convert back to EB's
o About 19hrs after RB's are converted to EB's they are releases and are able to infect new cells
List and describe the diseases associated with C. trachomatis
o Trachoma: chronic inflammation of conjunctiva
§ Mechanical damage to cornea, results in scarring and vision loss
o Chlamydia: STD – genital infection
§ Very contagious
§ 85% of females are asymptomatic and 25% of males are symptomatic
§ Females: slight vaginal discharge, inflammation of cervix, dysuria
§ Males: Urethral discharge, inflammation of epididymis, dysuria
o Neonatal pneumonia
o Inclusion conjunctivitis
§ ½ to ¼ of infants born to mothers purulent discharge in the eye
§ Doesn’t lead to blindness, treated with tetracycline or erythromycin (eyedrops).
o Lymphogranuloma venereum (LGV)
§ Rare genital infection
§ Small sores on genitals, fever, headahe
§ Swelling of ulceration of lymphatic tissue around groin area
· C. psittaci
List and describe the diseases associated with C. psittaci
o Birds to humans, causes pneumonia called psittacosis
o Major reservoir is psittacine birds: parrots, parakeets, pigeons
List and describe the diseases associated with
o Mild pneumonia (difficult to diagnose)
§ Atypical
§ 90% asymptomatic
o Recent evidence suggests that chronic infection with C. pneumoniae puts people at risk for atherosclerosis or heart attacks
o High incidence of C. pneumoniae in atherosclerotic lesions near the heart compared to a near absence of the organism in health arterial tissue
o Attaches to lining of coronary arteries
o Causes damage and promote plaque build up
o Treatment with antimicrobials may reduce heart attacks
Describe the general characteristics of the rickettsial organism, general mode of transmission and general effect of an infection on the human body.
· Strict intracellular parasite
· Transmitted by ticks, fleas, lice etc
· Penetrate skin and quickly move into the blood stream damaging capillaries and causing decrease in permeability
· Swelling of vessels causes rash. Also affects blood vessels of heart, lungs and kidnerys
· Symptoms include severe headache, malaise, fever and rash. Severe infections can lead to cardiovascular collapse.
· Rash is called centrifugal maculopapular rash (three categories)
o Centripetal
o Centrifugal
o Generalized
· Gram negative rod
List the diseases and vector associated with the following rickettsial species: R. rickettsii, R. akari, R. prowazekii, and R. tsutsugamushi.
· R. rickettsii
o Rocky mountain spotted fever
o Dog tick in east – wood tick in the west
o Most cases are in eastern U.S.
· R. akari
o Rickettsial pox
o Mouse mites
o Mild fever and rash
· R. prowazekii
o Lice
o Epidemic typhus
o Higher fever, rash, cardiovascular collapse
o 75% death rate
· R. typhi
o Endemic typhus (murine typhus)
o Fleas to rodents
o Southern Gulf coast states especially Texas
o Milder form of typhus, rarely fatal
· R. tsutsugamushi
o Mites
o Asia and southwest pacific
o Milder form of typhus
o The new species designation is orientia
Describe the characteristics and diseases of Coxiella burnetii, Mycoplasma pneumoniae, and Ureaplasma.
· Coxiella burnetii
o Obligate intracellular parasite but can survive outside host
o Spreads without vector – aerosols are breathed into lungs
o Zoonotic disease of sheep, goats and cattle
§ Occupational hazard
o Causes flu like symptoms along with some rickettsial like symptoms without rash. Fever, headace, malaise, nausea and vomiting
o Q fever
· Mycoplasma pneumoniae
o NF in oropharynx
o Produces atypical pneumonia – “walking pneumonia”
o Mild and difficult to treat – self limiting
o Community acquired infection
§ Leading cause of pneumonia in college students and military
o Diagnosis made serologically through ELISA, Florescent antibody (FA), or PCR.
o Treatment not really required but can shorten illness
· Ureaplasma urealyticum
o Associated with UTI however does not cause symptoms
o NF of urethra or vagina of sexually active men and women
o ½ of all people with 5 or more lifetime sexual partners are colonized
· Know the resistance to special potency disks for each genus
o Fusobacterium: vancomycin
o Preveotella: vancomycin and kanamycin
o Porphyromonas: vancomycin and colistin
o Bacteroides: kanamycin, vancomycin, colistin and tolerant to bile disk
o Clostridium: colistin
o Peptostreptococcus anaerobius: SPS disk