CARDIO TEST 2
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Know the average age that MI’s occur in men and women.
- Men: 66 & Women: 72
Be familiar with the factors that can accelerate atherosclerosis.
- LDLs, high blood pressure, smoking, & high saturated fat intake
Be familiar with what information can be implied from having a high C-reactive protein
level.
- How much atherosclerosis is occurring in the vessels, high levels are linked to a 2.5-4.5x increased risk of CVD
Be able to distinguish between the various proteins and enzymes we discussed in class
and what processes they are associated with (e.g. homocysteine is a protein that is
associated with collagen and calcium buildup in arteries).
Proteins and enzymes related to cardiovascular health and their roles in processes like metabolism and tissue repair.
Know why aspirin is typically prescribed to CVD/CHD patients.
- Aspirin reduces platelet stickiness
• Be familiar with associated statistics on how exercise therapy can reduce total mortality
and CHD mortality (i.e. Odds’ ratio).
- OR = 0.76
Be familiar with the effects that regular moderate and vigorous intensity have on C-
reactive protein (Odds’ ratios, percentages).
- Moderate PA: OR= 0.85
- Vigorous PA: OR: 0.53
Be familiar with the results of the MRFIT study.
- On the 6 years follow up, 488 men out of 12,000 died.
- 75-220 kcal/day is the needed energy expenditure to reduce CHD risk in men
Be familiar with stroke rates across ethnic groups.
- Men: White- 35, Black- 55, Hispanic- 35 Asian- 35, Indian- 30
- Women: White- 35, Black- 45, Hispanic- 30, Asian- 30, Indian- 30
Be familiar with stroke risk in smokers, people who have high blood pressure, diabetics,
and people who engage in high amounts of physical activity.
- Smokers; 60% higher
- High BP; primary independent risk factor for stroke, men are 4x likely to have a stroke if they have hypertension (greater than 160/95), women RR = 4.2
- Diabetics; Stroke risk doubled, 25% higher in women vs men
- PA; 20-25% lower risk (RR 0.75-0.80)
Be familiar with the 3 main mechanisms of stroke and be able to identify each.
- Embolic: circulating blood clots in LV
- Lacunar: blockages of small arteries deep in the brain
- Thrombotic: abnormal regulation of hemostatic factors & fibrinolytic system, insufficient anticlotting proteins
Be familiar with the different stroke treatments we discussed in class (identification,
features of each).
- Alteplase: converts plasminogen to the proteolytic enzyme Plasmin, plasmin then breaks down clotting factors fibrin and fibrinogen, 50% success rate, must be administered within 4.5 hrs of symptom onset
- Thrombectomy: Clot removal that grabs the clot via imagine, used in patients with large artery occlusion within 24 hrs of a stroke, 70-90% rate of reperfusion
- Ischemic Conditioning: 3-4 short cycles (5 mins of inflation & 5 mins of deflation via tourniquet), stimulates adenosine & bradykinin (vasoD) to be released, 2 hours of brain protection, 12-24 hours of delayed protection and can continue for 48-72 hours
Be familiar with the results of the Harvard Alumni study regarding stroke risk.
- Inverse relation to self reported weekly energy expenditure
- Less than 500 kcal/wk = 6.5 per 10,000 person years
- 500-1,999 kcal’wk = 5.2 per 10,000 person years
- Greater than 2,000 kcal/wk = 2.4 per 10,000 person years
Be able to list the 5 most common signs of stroke.
- Sudden numbness/weakness of face, arm, or leg, especially on one side of the body
- Sudden confusion & trouble with speaking/understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, or loss of balance
- Sudden, severe headaches with no known cause
How many people with diagnosed hypertension take medication to manage the
condition?
- 2/3 of diagnosed people
Be familiar with the basic mechanisms of action of each antihypertensive drug we
discussed in class.
- ACE inhibitors: relax blood vessels by blocking ACE from producing angiotensin II a vasoC
- ARBs: Blocks Angiotensin II binding sites
- Calcium channel blockers: block calcium channels, reducing the calcium than can enter cells in heart/arteries = decrease in contraction strength & BP
- Beta blockers: Blocks binding sites for catecholamines on the heart
Be familiar with specific side effects of taking certain antihypertensive drugs we talked
about in class.
- Calcium channel blockers = increased heart failure rate by 38%
- ACE inhibitors: stroke increase by 15% and heart failure by 19%
Be familiar with the average blood pressure reductions typically seen in the different
antihypertensive drugs we talked about in class.
- ACE inhibitors: -7mmHg SBP
- Beta Blockers: -10mmHg SBP
- ARBs: -8mmHg SBP
- Calcium channel blockers: -11mmHg SBP
- Diuretic: -8mmHg SBP
Be familiar with the effects of acute aerobic exercise on total peripheral resistance.
- TPR by 27% and plasma norepi, by 20% in Px with mild HT for up to 90 mins post ExRx
- Decreased vascular resistance by 7%, Decreased plasma renin activity by 20%
• Be familiar with how much of a decrease in resting blood pressure is usually seen across
different interventions (the info is in the table on slide 25).
- Improved diet: 5 mmHg
- Aerobic ExRx: 4.6 mmHg
- Alchol Restriction: 3.8 mmHg
- Sodium Restriction: 3.6 mmHg
- Fish oil supps: 2.3 mmHg
• Be familiar with the results of the post exercise hypotension study by Padilla et al. we
talked about in class.
- Hypertensive Px see a 12-14 mmHg decrease in SBP post ExRx
Be familiar with how much of a decrease in blood pressure can be seen in hypertensive
patients as a result of regular dynamic resistance training.
- Decreases SBP by 2-7 mmHg
Decreases DBP by 3-5 mmHg
Be able to explain in detail the RAAS system of reactions and how it reduces blood
pressure
- (1) Renin acts on angiotensin
- (2) Renin converts angiotensin to angiotensin I
- (3) ACE converts Angio I to Angio II
- (4) Angio II binds to receptors on kidneys, brain, and arterioles
- (5) Increased sodium reabsorption & fluid release back into circulation, increased BP, increased release of Aldosterone
- (6) Angio II acts on brain by causing productuon of ADH
Be familiar with how risk of CHD changes due to changes in cholesterol
· For every 1% change in cholesterol there 2% change in CHD risk
· For every 1% change in LDL-C there is a 2-3% change in CHD risk
· For every 1 % change in HDL-C there is a 2% and 3% change in CHD risk for men and women
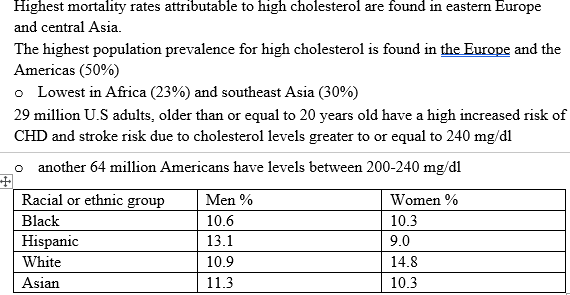
I. Be familiar with high cholesterol prevalence around the world and by ethnic group.
I. Be familiar with the process of how triglycerides are transported.
· Triglyceride- is a major form of biological fat
· Very low density lipo proteins (VLDL), are responsible for transporting triglyceride synthesized in the liver to adipose cells for storage.
I. Be familiar with how new HDL molecules are formed (important enzymes).
· Are secreted from the liver and intestines· Are secreted from the liver and intestines
Be familiar with the specific mechanisms that are thought to cause the cardioprotective effect of high HDL in the bloodstream.
· Inhibitions of LDL oxidation
o Paraoxanse 1 (PON1)
· Inhibition of adhesion molecules
Be familiar with the results of the Marathon study.
· Leisure time PA in men 20-60 years old was quantified and adjusted for age, alcohol consumption, smoking, and BMI. Cholesterol was then measured.
o Each 100kcal/day expended at an intensity > 7kcal/min = 2.09 mg/dl in
HDL
o Intensity equal to 9.5-12 kcal/min were associated with lower levels of total
cholesterol and triglycerides.
Be familiar with the typical cholesterol reductions seen from chronic aerobic exercise training
Triglyceride | 10 | 8% decrease
| 140 to128 |
Total –c | 10 | 4 % decrease
| 212 to 204 |
Ldl-c | 10 | 5% decrease
| 138 to 132 |
hdl-c | 10 | 4.5% decrease
| 45 to 47 |
I. Be familiar with the specific mechanism thought to increase HDL formation from a single exercise session.
· High intensity exercise
I. What is the primary cause of dyslipidemia in most people?
· Are single polygene mutations
o Overproduction and defective Clearence of triglycerides and LDL cells
o Underproduction and excessive clearance of HDL cells
· Secondary cause
o Excessive salt and fat intake
o Dietary cholesterol and fat intake
o Diabetes
o Alcholol overuse
o Kidney and liver disease
o Some hypertension and hiv drugso Excessive salt and fat intake
o Dietary cholesterol and fat intake
o Diabetes
o Alcholol overuse
o Kidney and liver disease
o Some hypertension and hiv drugs