(22) Regulation of Extracellular Fluid Osmolarity
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
What is osmolarity? (units)
number of osmoles/L of water
What is the normal plasma osmolarity?
300 mOsm/L
When there is excess water in the body, is the extracellular fluid osmolarity more elevated or reduced?
reduced
(since more water = more dilute)
When there is a deficit of water in the body, is the extracellular fluid osmolarity more elevated or reduced?
elevated
(since less water = more concentrated)
What does the kidney do when there is excess water in the body? (low osmolarity)
excrete dilated urine
By how much can the kidney reduce the osmolarity of urine (i.e. dilute urine) in order to get rid of excess water?
3-6 fold
What does the kidney do when there is a deficit of water in the body? (high osmolarity)
reabsorb water and excrete concentrated urine
By how much can the kidney increase the osmolarity of urine (i.e. concentrate urine) in order to minimize water loss?
4 fold
When there is excess water in the body, is there a high or low urine output?
high (+ diluted)
When there is a deficit of water in the body, is there a high or low urine output?
low (+ concentrated)
If there is an excess of water in the body, this leads to a decreased extracellular fluid osmolarity. What happens to the secretion of ADH?
decreases
(since ADH promotes reabsorption of water, and we don't want anymore water)
If there is excess water in the body, the secretion of ADH is reduced or blocked. This [increases/decreases] the permeability of the late distal tubules and collecting tubules for water and results in a [dilution/concentration] of the urine.
decreases, dilution
The kidneys are able to adjust the osmolarity and volume of urine without affecting what other value?
solute excretion rate
(kidney does this by mostly just affecting water reabsorption or excretion)
As osmolarity decreases, does urine flow rate increase or decrease?
increase
(lower osmolarity = more water = more dilute urine to get rid of excess)
As osmolarity increases, does urine flow rate increase or decrease?
decrease
(higher osmolarity = less water = less urine but concentrated to minimize water loss)
What is the relationship between osmolarity and solute excretion rate?
as osmolarity changes, solute excretion rate remains constant
minimum volume of urine which must be produced in order to eliminate the necessary amount of solute (excess solute that we take in and don't need needs to be gotten rid of)
**on average, we need to eliminate 600 mOsm/day
obligatory urine volume
A patient's kidneys can concentrate urine up to 1200 mOsm/L. Using the usual minimum amount of 600 mOsm that needs to be excreted each day, how do you calculate the obligatory urine volume?
600 mOsm/1200 mOsm/L = 500 mL
If Dr. Donati was stranded on a desert island with his pet Australian hopping mouse Wilbur (???) and they were surrounded by ocean, why shouldn't Dr. Donati drink the saltwater?
would greatly increase the obligatory urine volume to make up for the excess solutes taken in
(salinity of sea water is 2400 mOsm/L, his kidneys can concentrate 1200 mOsm/L, so he would have to eliminate 2 L of fluid for every 1 L he drinks to eliminate the extra solute he took in from the saltwater)
If your obligatory urine volume was 1 L, keeping in mind that the average kidneys can concentrate 1200 mOsm/L, how much solute would you be excreting?
A. 1200 ml
B. 2000 ml
C. 600 ml
D. 500 ml
A
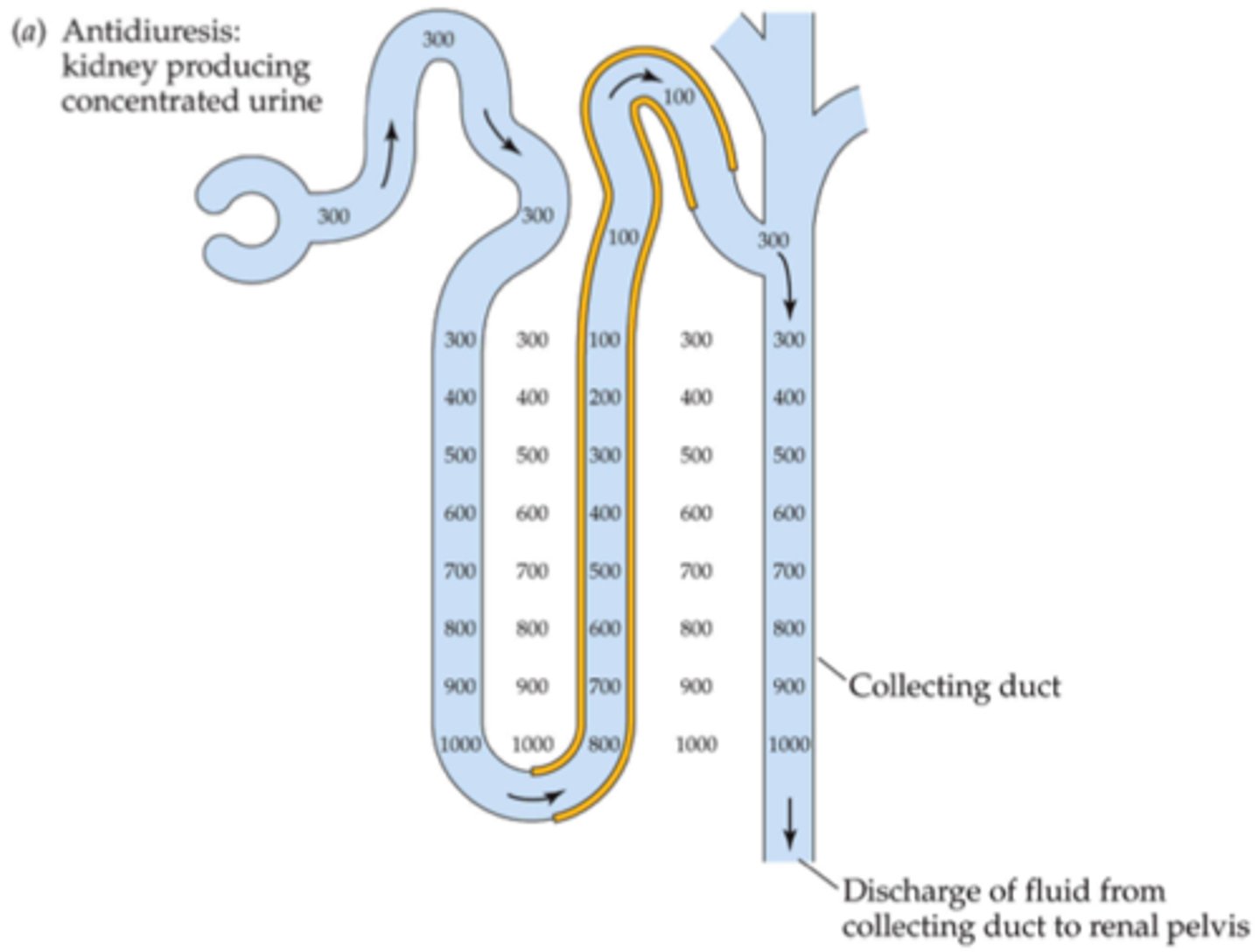
What are the 2 requirements for concentrating urine?
increased ADH, high osmolarity of renal medullary interstitial fluid
(water moves to area of high osmolarity, so more water will move outside the renal tubule into the interstitial fluid, and ADH will make the later tubules more permeable to that water)
Where is osmolarity of renal interstitial fluid higher: cortex or medulla?
medulla
(so things don't move passively out of the renal tubules unless there is this gradient)
phenomenon in which water and ions move in and out of the renal tubules and different parts of the tubular system
countercurrent mechanism
Is water transport out of the proximal tubule active, passive, or both?
passive
Is NaCl transport out of the proximal tubule active, passive, or both?
both
Is water transport out of the thin descending limb active, passive, or both?
passive
Is NaCl transport out of the thin descending limb active, passive, or both?
passive
Is water transport out of the thin ascending limb active, passive, or both?
none
(impermeable to water)
Is NaCl transport out of the thin ascending limb active, passive, or both?
passive
Is water transport out of the thick ascending limb active, passive, or both?
none
(impermeable to water)
Is NaCl transport out of the thick ascending limb active, passive, or both?
active
(has the secondary active Na/K/Cl symporter)
What part of the renal tubules can establish a 200 mOsm concentration gradient between the tubular lumen and the interstitial fluid?
thick ascending limb
Is water transport out of the cortical collecting tubule + medullary collecting duct active, passive, or both?
passive (mediated by ADH)
If the collecting tubule is permeable to water, then how does the osmolarity at the beginning relate to the osmolarity at the end of the collecting duct?
much higher at the end
Is NaCl transport out of the cortical collecting tubule + medullary collecting duct active, passive, or both?
active
Where is osmolarity reduced (i.e. diluted) the most?
thick ascending limb
(since solutes can move out but water can't)
When salt is actively transported out of the ascending limb of the loop of Henle into the interstitial fluid, that increases the osmolarity. Therefore, this induces what in the descending limb?
osmosis
process by which a progressively increasing osmotic gradient is formed in the interstitial fluid of the renal medulla as a result of countercurrent flow
involves the repetitive absorption of NaCl from the thick ascending limb and the continued inflow of new NaCl from the proximal tubules
countercurrent multiplication
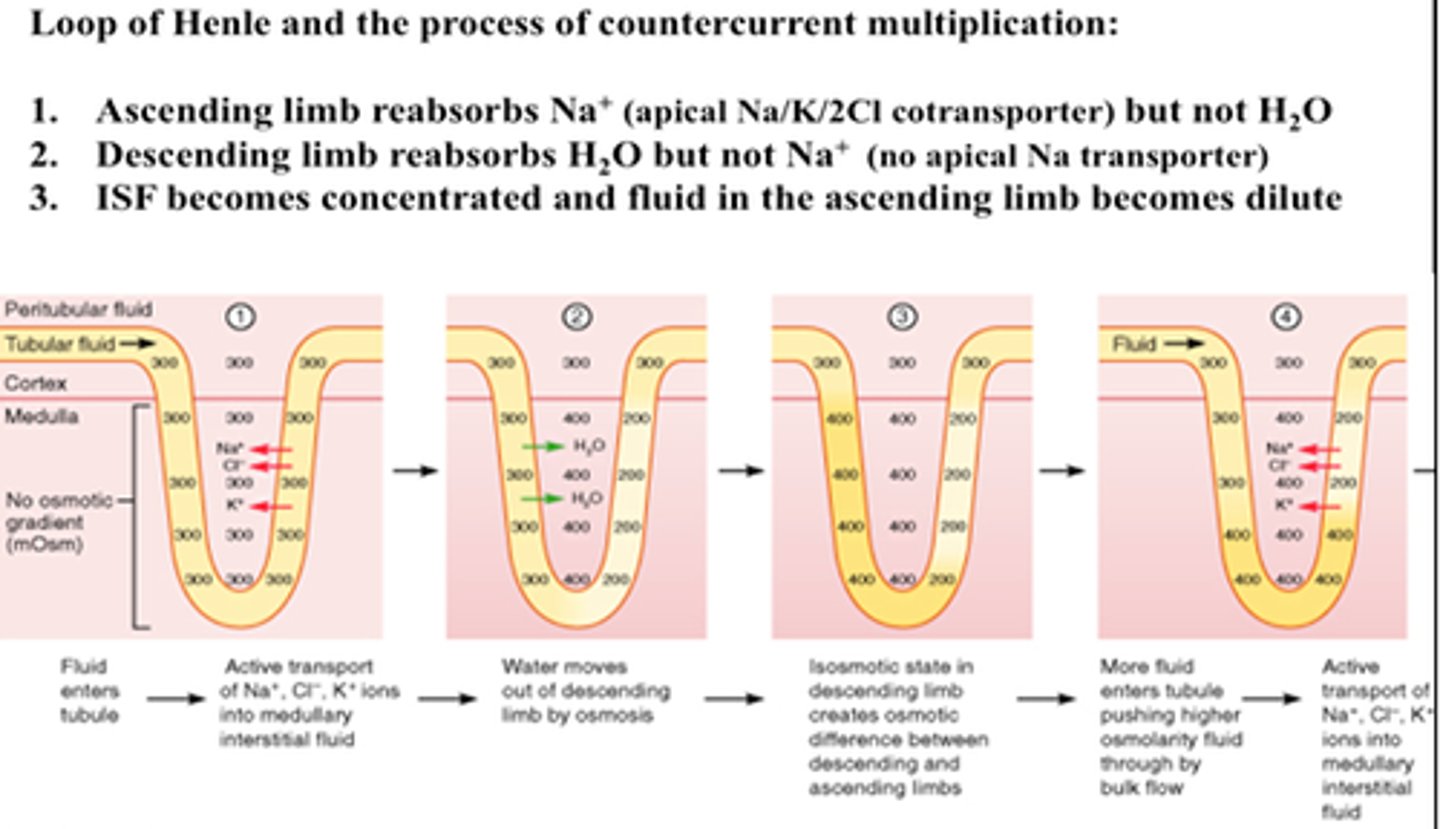
In the ascending limb of the loop of Henle, water cannot flow out due to lack of aquaporins, just salts. So then how can water enter interstitial fluid to prevent it from being too hyperosmotic?
diffuses out of descending limb
As Na+ continues to be reabsorbed in the thick ascending limb, water continues to be reabsorbed in the descending limb.
Does this create a high or low osmolarity in the medullary interstitial fluid? (compared to plasma)
high
As Na+ continues to be reabsorbed in the thick ascending limb, water continues to be reabsorbed in the descending limb.
Does this create a high or low osmolarity in the cortical interstitial fluid? (compared to plasma)
low
refers to the osmotic gradient in interstitial fluid from cortex to medulla, responsible for countercurrent multiplier system
**higher osmolarity at bottom of loop, lower at top
corticomedullary gradient
Where is urea initially passively reabsorbed? (about 50%)
proximal tubules
About 50% of urea is passively reabsorbed in the proximal tubules. What other part of the renal tubules absorbs the rest?
collecting ducts
About 50% of urea is passively reabsorbed in the proximal tubules, and the rest is absorbed in the collecting ducts. However, it is then secreted back into what parts again?
thin limbs (of loop of Henle)
About 50% of urea is passively reabsorbed in the proximal tubules, and the rest is absorbed in the collecting ducts. However, it is then secreted back into the thin limbs, and some of it gets trapped in the medullary interstitium. If there is excess, then that is excreted. Why is this cycle so important?
maintains high renal medullary osmolarity
Which nephrons have the peritubular capillaries all around: cortical or juxtamedullary?
cortical
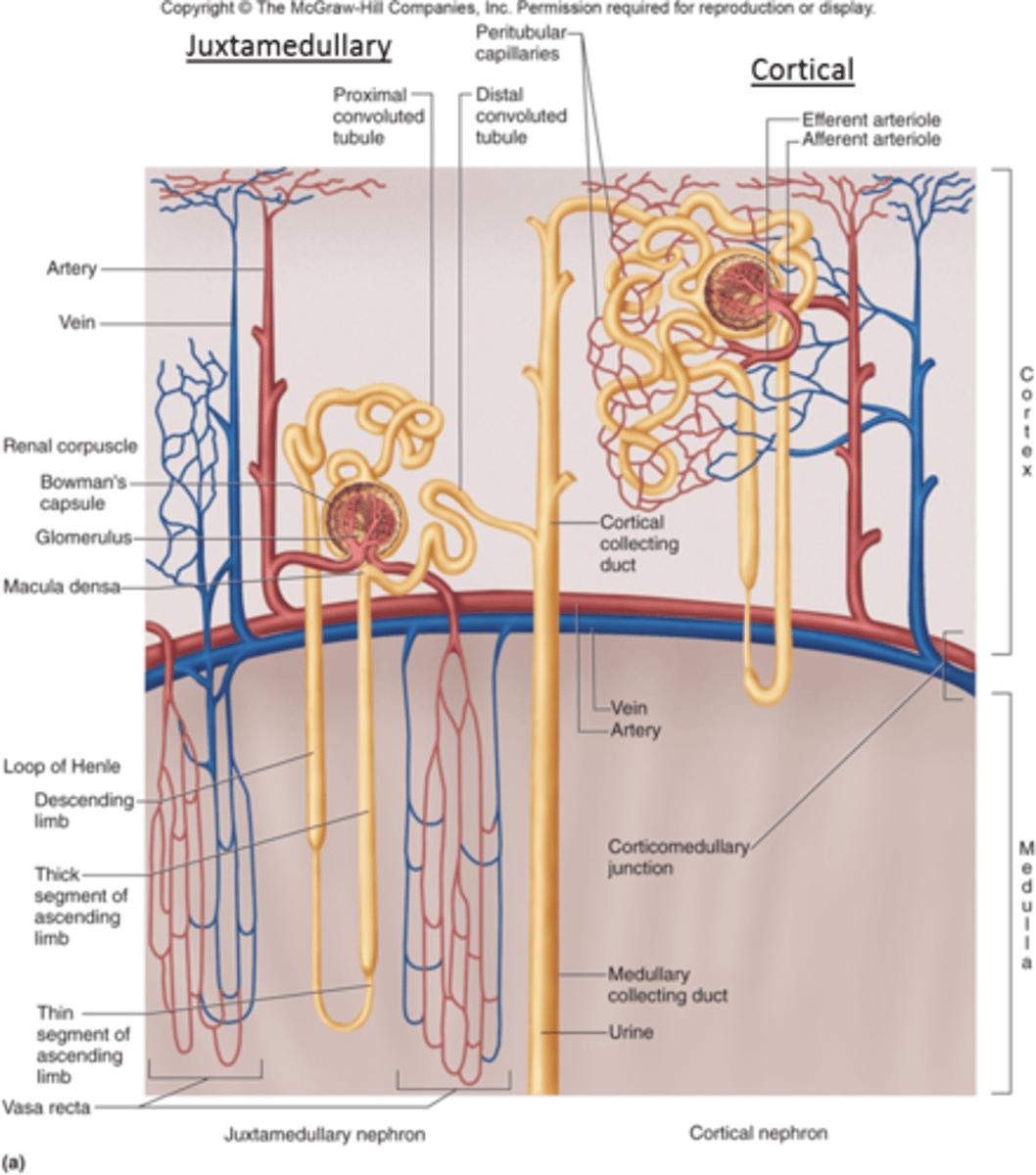
Which nephrons have the vasa recta: cortical or juxtamedullary?
juxtamedullary
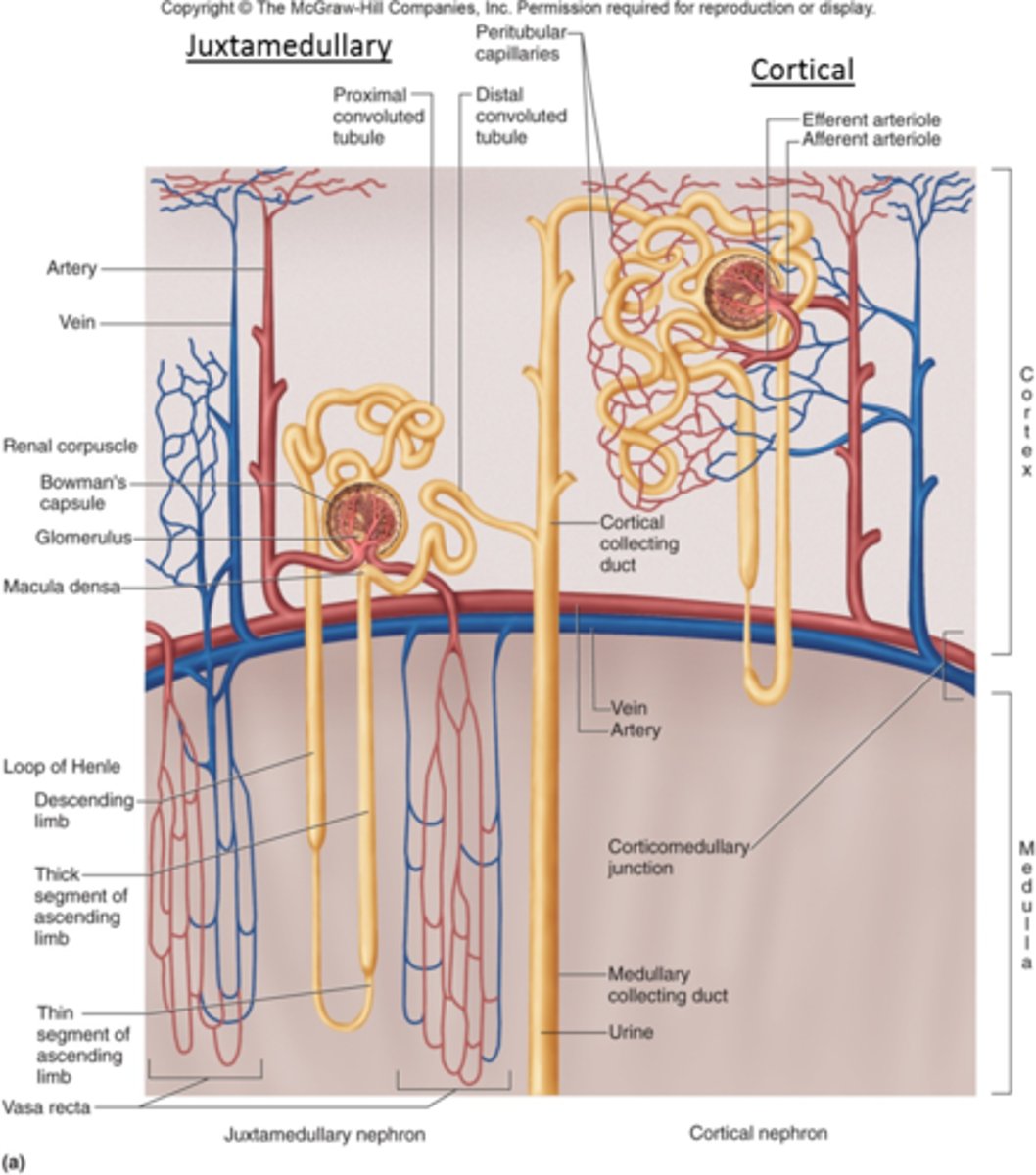
structure in juxtamedullary nephrons that picks up some of the water lost from thin descending limb and some of the solutes from the thick ascending limb, helping to maintain the constant gradient
**does not create high osmolarity - maintains it instead!
vasa recta
How does the vasa recta affect osmolarity?
maintains it (but does not create high osmolarity)
In the absence of ADH, are the late distal tubule and collecting tubules permeable or impermeable to water?
impermeable
In the presence of ADH, are the late distal tubule and collecting tubules permeable or impermeable to water?
very permeable
cells found in the hypothalamus that sense increases in osmolarity of extracellular fluid
when they're stimulated, they send signals to both the supraoptic and paraventricular nuclei, which synthesize ADH
osmoreceptors
Osmoreceptors stimulate the production of ADH in what part of the brain?
hypothalamus
Osmoreceptors stimulate the release of ADH in what part of the brain?
posterior pituitary
How does the kidney respond to feedback from ADH?
increases water reabsorption in late distal/collecting tubules
How does ADH affect urine osmolarity?
makes it more concentrated
(since it promotes water reabsorption)
Why is alcohol a diuretic?
blocks ADH
(therefore prevents water reabsorption)
Does elevated blood pressure increase or decrease ADH secretion? (via arterial baroreceptor reflex)
decrease
(reduce water reabsorption)
Does reduced blood pressure increase or decrease ADH secretion? (via arterial baroreceptor reflex)
increase
(promote water reabsorption)
Does decreased blood volume result in an increase or decrease in ADH secretion? (via cardiopulmonary reflex)
increase
(more water reabsorption = increased blood volume)
Does increased blood volume result in an increase or decrease in ADH secretion? (via cardiopulmonary reflex)
decrease
(less water reabsorption = decreased blood volume)
Is ADH secretion more sensitive to changes in osmolarity or blood volume?
osmolarity
(5% change in osmolarity has the same effect as 15% change in blood volume)
When ADH is present, do we produce diluted or concentrated urine?
concentrated
When ADH is absent, do we produce diluted or concentrated urine?
diluted
True or false: The diluting segment of the renal tubule (thick ascending) is ALWAYS impermeable to water, regardless of ADH effects.
true
Where is the thirst center found?
(thirst = conscious desire for water)
preoptic nucleus (hypothalamus)
Does increased osmolarity increase or decrease thirst?
increase
(take more fluid in to dilute it out)
Does decreased blood volume increase or decrease thirst?
increase
(take in more fluid to bring volume up)
Does decreased blood pressure increase or decrease thirst?
increase
(take in more fluid to bring pressure up)
Does increased angiotensin II increase or decrease thirst?
increase
(since angiotensin II is trying to raise BP)
Does decreased osmolarity increase or decrease thirst?
decrease
Does increased blood volume increase or decrease thirst?
decrease
Does increased blood pressure increase or decrease thirst?
decrease
Does decreased angiotensin II increase or decrease thirst?
decrease
Which portion of the renal tubules listed below is NOT permeable to water regardless of the presence of ADH?
A. proximal tubule
B. collecting duct
C. early distal tubule
D. thin descending Loop of Henle
C
When either the ADH or thirst mechanisms fail, the other normally can still control extracellular osmolarity and concentration of what ion?
Na+
If both the ADH and thirst mechanisms fail, how can we control extracellular osmolarity now?
we can't
Which statement is correct?
A. Water reabsorption is under control of vasopressin throughout the length of the nephron.
B. The ascending limb of the loop of Henle is always impermeable to water.
C. Vasopressin makes the distal and collecting tubules impermeable to water.
D. Fifteen percent of the filtered water osmotically follows the absorption of Na+ and other solutes in the proximal tubule.
E. Water reabsorption is passive in the early portions of the nephron but is active in the distal portions of the nephron.
B
The normal osmolarity of body fluids is ________ mOsm/liter.
A. 100
B. 200
C. 300
D. 450
E. 600
C