neuro weeks 5-11
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
what is dysphagia?
feeding and swallowing difficulties
what are the phases of swallowing
oral preparatory phase (voluntary)
oral transport phase (voluntary)
pharyngeal phase (involuntary)
esophageal transport phase (involuntary)
what parts of the nervous system are involved in swallowing?
cortical
primary motor and somatosensory
subcortical
basal ganglia and limbic structures
brain stem
cranial nerces
what does the primary somatosensory system do for swallowing?
receives information about the movement of the jaw joints, muscles (tongue and soft palate), lips, bolus size
what do the subcortical areas do for swallowing?
may play a role in modifying and monitoring swallowing activity
what does the brainstem do in swallowing?
nucleus ambiguous
innervate the soft palate, pharynx, and larynx
nucleus tractus solitarius
sensory neurons related to taste
what do the cranial nerves do for swallowing?
trigeminal
motor: muscles of mastication
sensory: facial and mouth sensation
facial
motor: muscles of lip closure
sensory: taste, saliva production
glossopharyngeal
elevates the pharynx and larynx
taste in the posterior 1/3
vagus
innervates the larynx, pharynx, and soft palate muscles
sensory feedback from the pharynx and larynx
hypoglossal
muscles of tongue
what are the motor patterns in swallowing/chewing?
voluntary
complex, purposeful actions
learnt with practice
rhythmic
combines voluntary and reflexive
Onset and termination are voluntary
Once initiated, reflexive and repetitive
e.g. chewing (depending on the central pattern generator)
reflex
involuntary, rapid
e.g. cough/gag
triggered by a stimulus
what is the swallowing central pattern generator
located in the medulla and involves motor cranial nerves
creates a swallowing pattern/reflex
what occurs in the gag reflex?
stimulus from the glossopharyngeal nerve
muscular response from the vagus nerve
occurs in the pharyngeal stage of swallowing
what occurs in the oral preparatory stage of swallowing?
lip closure using the facial nerve
manipulation of the bolus via
lateral jaw movement (trigeminal)
lateral tongue movement (hypoglossal)
elevation of tongue and soft palate resting against the tongue
what occurs in the oral transit stage of swallowing?
oral cavity closed via tongue
food is moved back through the mouth with squeezing action
tongue forms a chute
mouth floor raises
tip of tongue reaches to palate
central area hollows
sides of the tongue elevate
what occurs in the pharyngeal stage of swallowing?
closing of airway while bolus moves through pharynx
requires sensory feedbakc to coordinate
what are the locations and functions of cortical speech production?
pre-motor cortex
planning
brocas area
planning
supplementary motor area
programming movement sequences
feeds correct motor instructions in the correct sequence
primary motor cortex
execution of speech
what are the functions of cranial nerves in speech?
trigeminal: muscles of mastication
facial: lip movement, articulation, and bilabial sounds
glossopharyngeal: pharyngeal closure and abnormal nasal airflow
vagus: elevation of soft palate during velopharyngeal closure
hypoglossal: muscles of tongue and articulation of lingual sounds (f and k)
what are the types of dysarthria (difficulty speaking)?
flaccid: LMN damage
spastic: bilateral UMN damage
dyspraxia/apraxia: impairment with planning or programming speech
what are the bases of speech?
phonation: voice production
resonance: air flow through oral or nasal cavities
articulation: production of speech sounds
prosody: features of speech
intonation
flow of speech
what does the the corticobulbar tract do for speech?
voluntary control of muscles for speech.
arises from primary motor cortex
passes through internal capsule
synapses at the LMN in the CN nucleus in the brainstem
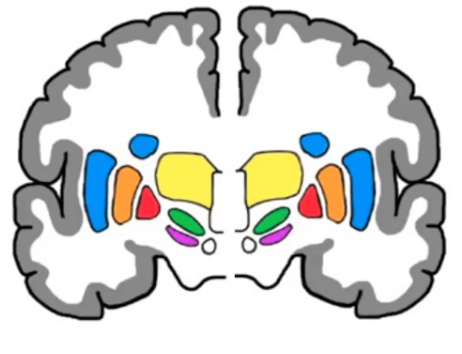
what are the grey matter structures of the basal ganglia?
caudate (striatum)
putamen (striatum)
gobulus palidus
internus (GPi)
externus (GPe)
subthalamic nucleus (STN)
substantia nigra
pars compacta (SNpc)
pars reticular (SNPR)
what are the steps of the direct pathway?
thalamus releases excitatory glutamate to motor cortex to stimulate movement
globus pallidus internus and substantia nigra pars reticula send GABA to thalamus, inhibiting glutamate release
motor cortex sends information about movement through glutamate to the striatum
excited striatum releases inhibiting GABA into the GPI and SNPR, preventing GABA from being sent to the thalamus
thalamus is able to continue sending excitatory glutamate to motor cortex
movement is facilitated
substantia nigra pars compacta sends dopamine to the striatum, modulation the direct pathway
what are the steps of the indirect pathway?
GABA sent from globus pallidus externus to the subthalamic nucleus inhibits glutamate release from subthalamic nucleus
cerebral cortex sends excitatory information to striatum
striatum sends inhibitory signals to the globus pallidus externus, preventing GABA from being sent to the subthalamic nucleus
cerebral cortex sends excitatory signals to the subthalamic nucleus
subthalamic nucleus sends excitatory signals to the globus pallidus internus and substantia nigra pars reticula
GPE and SNPR send GABA to the thalamus
thalamus is inhibited, and can no longer send glutamate to the motor cortex
movement is inhibited
substantia nigra pars compacta sends dopamine to the striatum, modulating and inhibiting indirect pathway
what are the pathways used to send information from the thalamus to the cortex and from the substantia nigra pars compacta to the striatum?
corticothalamic tract
nigrostriatal tract
what are the basal ganglia loops?
goal directed behaviour loop (non-motor)
social behaviour loop (non-motor)
emotion loop (non-motor)
reward direct
motor loop (motor)
what does the basal ganglia do for movement control?
regulates desired and inhibits undesired movements
voluntary movement, postural muscles, rhythmic movements
sends information back to motor cortex via thalamus
regulates muscle tone and force
how does the basal ganglia motor loop travel?
cortico-basal ganglia-thalamic loop
what are the pathways of the basal ganglia?
hyperdirect pathway (irrelevant)
direct: allows movement
indirect: prevents undesired movement
what are the cortical layers of the cerebellum?
molecular: few axons
purkinje cells: single row of huge cells
granular layer: numerous packed neurons
what are the peduncles of the cerebellum and what do they do?
Connect the rest of the CNS
Superior cerebellar peduncle: in the midbrain, efferent fibres via thalamic nuclei to the cortex
Middle cerebellar peduncle: in the pons, afferent fibres to the cerebellum from the cerebrum
inferior cerebellar peduncle: in the medulla, afferent and efferent
afferent from the spinal cord, vestibular apparetus
efferent to vestibular nuclei and reticular formation
what supplys the cerebellum with blood?
basilar artery giving rise to
anterior inferior cerebellar artery (AICA)
superior cerebellar artery (SCA)
posterior inferior cerebellar artery (PICA)
what does the cerebellum play a role in?
maintaining posture and balance - through inputs from vestibular, makes postural adjustments
coordination of voluntary movement - coordinates timing and force
motor learning - fine tunes motor programs
cognitive function
what are the cerebellum functional areas?
spinocerebellum (vermis)
vestibulocerebellum (floccolonodular)
cerebrocerebellum (lateral hemispheres)
what does the spinocerebellum/vermis functional area do?
input
movement commands from cortex
activity levels of spinal cord neurons
movement or postural adjustment from proprioceptors
plays a role in making anticipatory, corrective, and responsive adjustments
what does the vestibulocerebellum/floccolondular area do?
input
ipsilateral vestibular apparatus
ipsilateral vestibular nuclei in the brainstem
output
vestibular nuclei and reaches motor neurons via vestibulospinal tracts
role in head movement and position
what does the cerebrocerebellum/lateral hemisphere area do?
input
cerebral cortex via pontine nucleus
output
motor and premotor cortex via dentate and motor thalamus
role in timing movements, planning movements, and coordination of voluntary movement (influences corticospinal, brainstem, and rubrospinal tracts)
what is cerebellar ataxia?
sudden inability to coordinate muscle movement due to disease or injury to the cerebellum
can be genetic or non-genetic
Purkinje and granule cells are vulnerable to alcohol damage
what is spinocerebellar ataxia type 1?
autosomal dominant disease that causes loss of purkinje and granule cells
occurs in 3rd-4th decade of life
what are the differences between cerebellar ataxia and sensory ataxia?
cerebellar ataxia
caused by structural of functional change to cerebellum
results in ataxic movements
sensory ataxia
caused by structural or functional change to the sensory nerves
results in interruption of sensory feedback
results in ataxic movements
what are the tests to distinguish sensory and cerebellar ataxia?
rhombergs test: stand with feet together and balance for 30 secs. compare with eyes opened and closed
sensory: patients should be stable with eyes open and unstable with closed
cerebellar: unstable both open and closed
finger nose test: patients index finger to their nose and then to examiners finger quickly and accurately
sensory: signs of ataxia when eyes closed
cerebellar: signs of ataxia both open and closed eyes
what are the types and location of dysmetria (inaccurate size of movement)?
hypermetria: overshoots target
hypometria: undershoots target
damage to spinocerebellum
what is an intention tremor and where does it occur?
involuntary, oscillatory movement
spinocerebellum
what is dysdiadochokinesia and where does it occur?
difficulty with rapid alternating movements (e.g. finger tapping)
spinocerebellum
what is ocular dysmetria and where does it occur?
eyes not able to be moved accurately to target
vestibulocerebellum
what is nystagmus and where does it occur?
involuntary oscillation of the eye
vestibulocerebellum
what is movement decomposition and where does it occur?
difficulty of movement in which gestures are broken into individual segments instead of being executed smoothly
spinocerebellum
what is ataxic dysarthria and where does it occur?
change in force, timing, range, and direction of movement of the articulators that gives a very slurred “drunk” sounding presentation
cerebrocerebellum
what is ataxic gait and where does it occur?
variability in walking pattern, increased risk of falls, slow speed
spinocerebellum
I SKIPPED WEEK 8 UNTIL SMELL- GO OVER AGAIN PLS
what are the steps of olfaction?
air passes through the olfactory epithelium mucous
odour dissolves into mucous
odour reaches olfactory receptor cells
odour binds to surface of cilia
unmyelinated olfactory axons bundle together to create olfactory nerve
olfactory bundles penetrate the cribiform plate, travelling to the olfactory bulb
olfactory receptor neurons in the bulb synapse with second olfactory neuron
output neurons from bulb project to olfactory tract, projecting to range of areas
what are the disorders of smell called?
anosmia: loss of smell
hyposma: decreased sensitivity to smell
what are the structures associated with taste?
receptor cells sit together, forming tastebud
chemical change in receptor cell pushes a neural impulse
neural impuls cranial nerves
facial: transmits anterior 2/3 of tongue
glossopharyngeal: transmits posterior 1/3
vagus: transmits from epiglottis
sensory information from cranial nerves is transmitted to solitary nucleus in the solitary tract of the brainstem
second neuron in pathway transmits information to the thalamus
final neuron synapse in the gustatory cortex
what is a loss of taste called?
ageusia
what makes up the fibrous/tunic layer of the eye?
sclera: white part
provides attachment for extra-ocular muscles
cornea: transparent structure
what makes up the vascular layer of the eye?
choroid: capillary network of blood vessels
ciliary body muscles: muscles, processes, and suspensory ligaments alter lens shape
iris
pupillary dilator muscle (smooth muscle, sympathetic)
pupillary constrictor muscle (parasympathetic)
what makes up the inner layer of the eye?
retina: houses photoreceptors
rods: low light, no colour
cones, high light, colour
fovea
centre of macula
highest concentration of cones
site of sharpest vision
macula: centre of your retina,
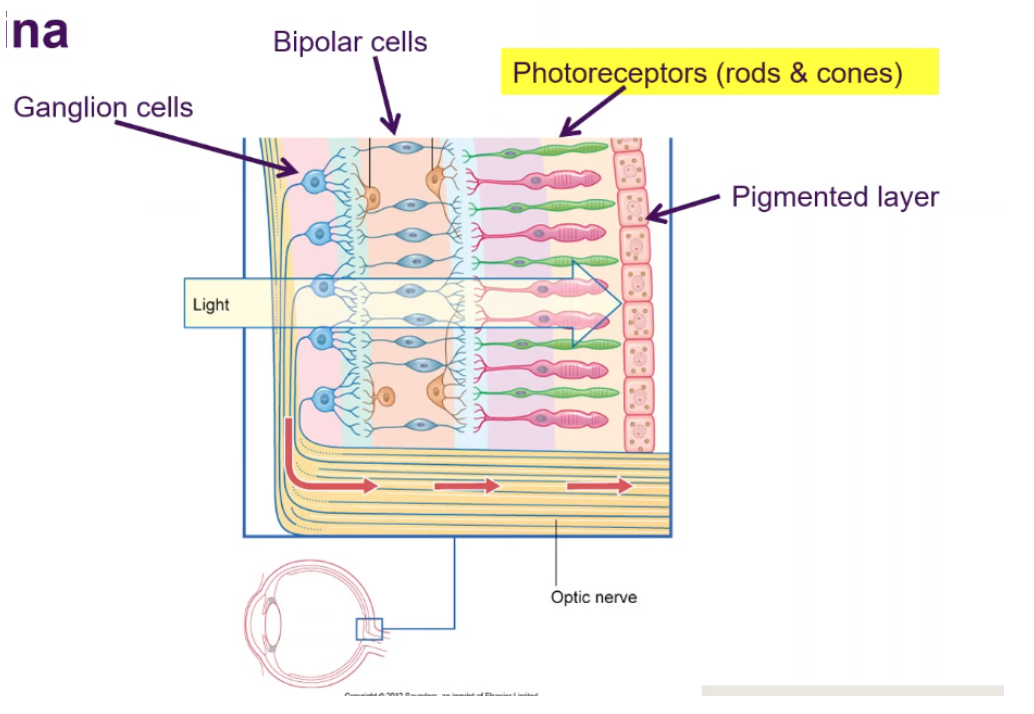
how does the retina work?
pigmented epithelium that absorbs light that is passing through
Photoreceptor cells synapse with bipolar cells
bipolar cell synapses with ganglion cells, which then become the optic nerve, which leaves the retina
blind spot occurs in the area where the retina meets the optic nerve (no light sensitive cells in this location)
what are the rectus muscles of the eye?
superior: elevate cornea
inferior: lower cornea
medial rectus: adduct eye
lateral rectus: abduct eye
what are the oblique muscles of the eye?
superior oblique: elevation and abduction
inferior oblique: depression and abduction
what is the process of the visual pathway?
optic tract travels from eye to lateral geniculate nuclei
lateral geniculate synapses with next neuron, which travels to the primary visual cortex (PVC looks for shape, size, texture)
information is subsequently sent to secondary visual cortex
information from left visual field is being projected to nasal side of left side, and temporal side of right side
at the optic chiasm, the information swaps to the other side of the brain
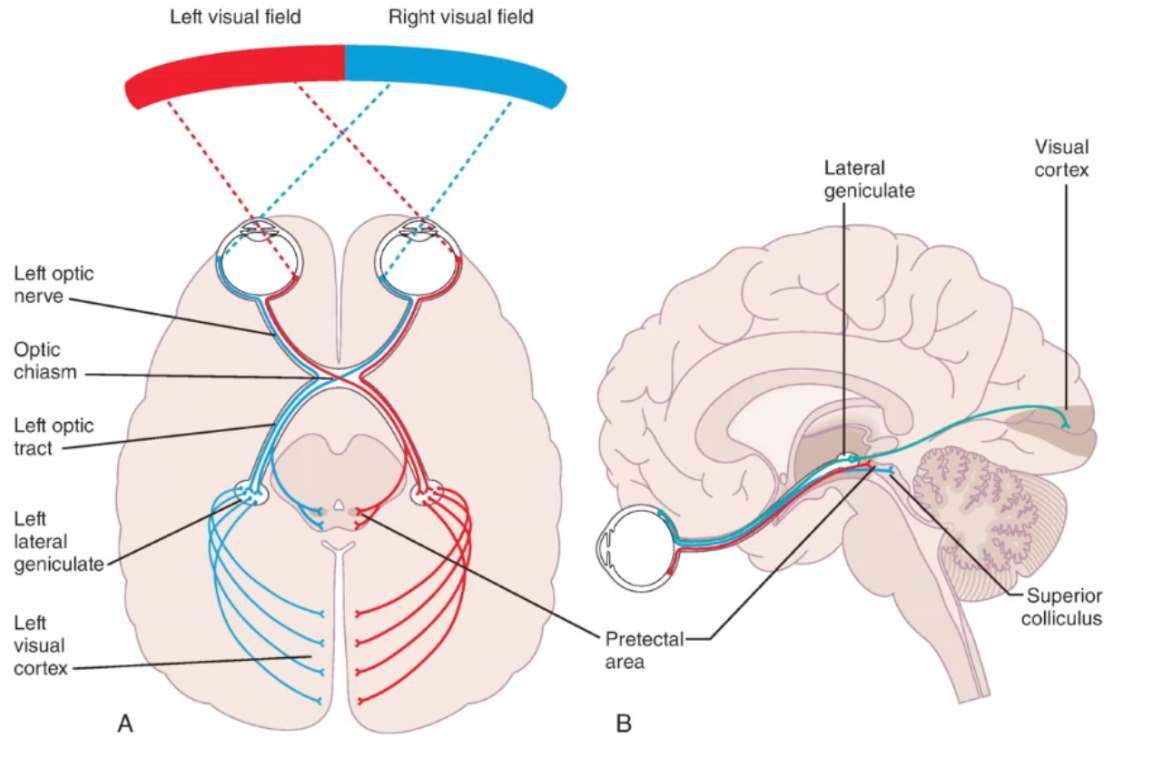
what are the types of blindness?
lesion at optic nerve of right eye: no vision in right eye
lesion at optic chiasm: vision impaired on lateral side of vision
lesion behind optic chiasm: vision lost on contralateral side of body
lesion far back, hasn’t cut the entire visual pathway: vision lost at contralateral bottom quarter of the body
what are the 3 bases of somatosensation?
proprioception: information from musculoskeletal system
exteroception: information from the skin (superficial or cutaneous)
interoception: information from internal organs (stretch of bladder or stomach)
what are the types of receptors?
nociceptors: pain
thermoreceptors: temperature
chemoreceptors: respond to water soluble and libid soluble substances dissolved in body fluids
mechanoreceptors: sensitive to stimuli that distort their plasma membrane
what are the muscoloskeletal receptors?
muscle spindles: within skeletal muscle belly
intrafusal fibres respond to muscle stretch
golgi tendon organ: found in tendons in musculotendionous junction
detect force/muscle tension created during contraction
joint receptosrs: respond to mechanical deformation of joint capsules and ligaments
what are receptive fields?
cutaneous areas of skin that leads to activity in neuron
large receptive fields cover a large area with low sensitivity
small receptive fields cover a small area precisely
small fields help the brain locate where a stimulus is felt with precision
what are the primary sensory neurons?
neurons that take in somatosensory information from skin, muscles, joint capsules, and viscera
PSN cell bodies are housed in the dorsal root ganglion (bipolar nerve)
what are the brodmanns area of the primary somatosensory cortex?
area 3: nerve fibres carrying proprioceptive information
areas 1 and 2: nerve fibres carrying information about texture, size, and shape
what is the brodmann’s area and function of the secondary somatosensory cortex?
area 40
recieves connections from the primary
responds to stimuli bilaterally
less precision than primary
what are the brodmanns area of the somatosensory association cortex?
areas 5 and 7
receives synthesised connections from the primary and secondary cortices
Neurons respond to several types of inputs
involved in complex associations
stereogenesis and haptic perception
what are the types of ascending somatosensory tracts?
conscious relay
divergent relay
non-conscious relay
what are conscious relay tracts and where are their neurons?
transmit information about the location and type of stimuli with high fidelity
1st order neuron: cell body in dorsal root ganglion, travels into spinal cord/brainstem
2nd order: cell body in spinal cord/brainstem, axon decussates to the contralateral thalamus
3rd order: cell body in thalamus, axon travels up to primary sensory cortex (via internal capsule)
what are the neurons of the dorsal column medial lemniscus tract?
1st order: enters and ascends through dorsal column of spinal cord
2nd order:
cell bodies located in nucleus gracilis or cuneatus of spinal cord
axons decussate in spinal cord and ascend to thalamus
3rd order: cell bodies located in thalamus send their axons to the cortex via the internal capsule
synapse to cells in the primary somatosensory cortex corresponding to the body area they originated from
what are the neurons of the spinothalamic tracts?
1st order: brings information into the posterior horn of the spinal cord
2nd order:
cell bodies in the posterior grey area of the spinal cord
axons of the secondary neurons cross at the midline and ascend from the spinal cord to the thalamus
3rd neuron: cell bodies in thalamus, project via thalamus to the primary somatosensory cortex (via internal capsule)
what are the nuclei of the brainstem responsible for intaking information from the trigeminal nerve?
mesencephalic nucleus: unconscious proprioception from muscle spindles of the face
excessive biting, receives information about stretch from muscles of mastication
main sensory nucleus: touch, vibration, 2 point discrimination, fine touch, conscious proprioception senses
spinal nucleus: pain, temperature, and crude touch
what are the order of neurons that intake sensation from the face?
1st order: trigeminal ganglion
2nd order: transmit information to thalamus
3rd order: thalamus to cortical areas

what do divergent tracts transmit?
slow aching pain
information transmission is not localised, and is transmitted to many locations in the brainstem and cortex
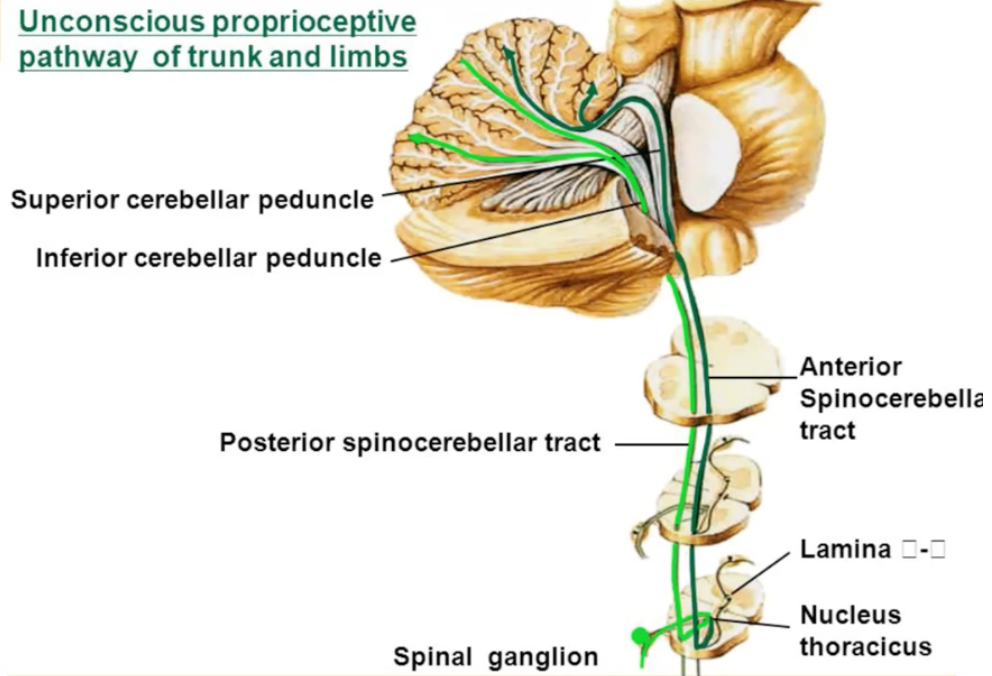
what do unsconscious relat tracts transmit?
spinocerebellar tract
unconscious movement-related information in the cerebellum
proprioceptive and sensory
what occurs with complications of the dorsal column medial lemniscus and the spinothalamic tract?
DCML: loss of proprioception and fine touch
hemisection of spinal cord: ipsilateral loss below level of lesion
somatosensory cortex lesion: contralateral sensory loss
STT: loss of pain and temp sensation
hemi section: contralateral loss below level of lesion
somatosensory cortex: contralateral sensory loss
what is nociception?
the neural process of encoding noxious stimuli (neural)
what is noxious stimuli?
a stimulus that is damaging or threatens damage to normal tissue
what is pain?
perception of an aversive or unpleasant sensation arising from a specific region of the body (perception)
what are the physiological processes of nociception?
transduction: conversion of noxious stimulus into an action potential in peripheral terminals of sensory fibres
conduction: passage of action potentials from periphery along axons towards the CNS
transmission: the synaptic transfer of input from one neuron to another
perception: when the sensation is perceived by the brain
what are the tacts for the transmission of pain?
spinothalamic: fast and slow pain, (A delta fibres)
spinoreticular: slow, dull pain (C delta)
reticular formation: responsible for emotion and behavuoural responses to pain
trigeminal pathway: pain from face
spinal trigeminal pathway is for pain
cell body for first order neuron is in trigeminal ganglion
travels to medulla (decussation of 2nd order neuron)
what are the characteristis of A delta fibres?
myelinated
fast, sharp, localised pain
lateral spinothalamic tract
what are the characteristics of C fibres?
unmyelinated
slow, dull, aching or burning
poor localisation
emotional and motivation aspects of pain
what are the classifications of pain?
acute
up to 6 weeks
associated with tissue damage
sub-acute
4-12 weeks
secondary issues with tissue healing (inflammation, infection)
chronic/persistent
continues past regular healing
3-6 months
what are the types of pain?
nociceptive: actual or threatened damage to non-neural tissue
e.g. post-op pain, injury
neuropathic: abnormal neural activitiy secondary to disease, injury, or dysfunction of nervous system
related to lesion of neural tissue
e.g. compressed nerve, phantom limb pain, MS related pain
nociplastic: pain arises from altered nociception despite no clear evidence of stimulus
no tissue damage or lesion on neural tissue
usually associated with chronic pain conditions such as fibromyalgia, low back pain, tension headaches
what is modulation of pain?
alterations to pain signals that may amplify or dull them
The same stimulus can elicit different responses in different scenarios
what is sensitisation?
an increase in responsiveness of nociceptive neurons to their normal input, and/or recruitment of a response to normally sub-threshold stimuli
can be peripheral or central
what are the types of pain sensitisation?
allodynia: pain resulting from a stimulus that does not normally cause pain
dysasthesia: unpleasant abnormal sensation, whether spontaneous or evoked
Hyperalgesia: increased response to a stimulus that normally is painful
what are the analgesia systems?
endogenous opioid system: excretion of natural, pain relieving chemicals
descending inhibition: a message sent down the brain and spinal cord that blocks incoming pain messages
gate control theory: non painful stimuli prevent pain messages in the spinal cord from reaching the brain
what is aphasia?
impaired ability to understand or produce speech
caused by damage to the cortical areas in the left hemisphere (broca’s and Wernicke’s)Broca’s
what is the flow of information during conversation?
primary auditory cortex - auditory discrimination
secondary auditory cortex - classification of sounds (language vs sounds)
wernickes area - auditory comprehension/word retrieval
subcortical connections - link wernickes and brocas area
brocas area - understanding syntax, instructions for language output
oral region of sensorimotor cortex - cortical output to speech muscles
what occurs during wernicke’s aphasia?
loss of blood flow to superior temporal gyrus (MCA)
impairment in receptive language
fluent verbal output
frequent word errors
can use made up words
impairment naming and repetition
what occurs during broca’s aphasia?
loss of blood flow to broca’s and surrounding inferior frontal gyrus by left MCA
limited verbal output
good auditory comprehension
repetition usually poor
can co-occur with motor-speech disorders (e.g. dysarthria)
what occurs during conduction aphasia?
legion to cortical region supramarginal gyrus and white matter pathways of arcuate fasciculus
fluent speech with relatively intact receptive language
poor repetition
phonemic errors in spoken output
naming difficulties
awareness of errors
what occurs during global aphasia?
extensive damage to frontal, temporal, and parietal regions
severe receptive and expressive impairments
almost totally absent speech
may be able to express through facial expression, intonation, and gesture
what are the 3 domains that cause cognitive communication disorders?
Memory: formation of records of new experiences and the use of the information to guide subsequent activities
Attention: the concentration of awareness/focus on some phenomenon to the exclusion of other stimuli
executive functionExecutive:
what is consciousness?
having subjective experiences and awareness of self and environment
can be influenced by meditation, medication, mental health conditions
what are the aspects of consciousness?
arousal
attention
selection of object and attention
motivation and initiation
what are the modulators associated with consciousness?
serotonin: general arousal
norepinephrine: attention
acetylcholine: selection of the object of attention, based upon goals
dopamine: motivation, motor activity, cognition
what is orienting attention?
the ability to locate specific sensory information from among many stimuli
e.g. locating the traffic light whilst driving