hemostasis practical
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
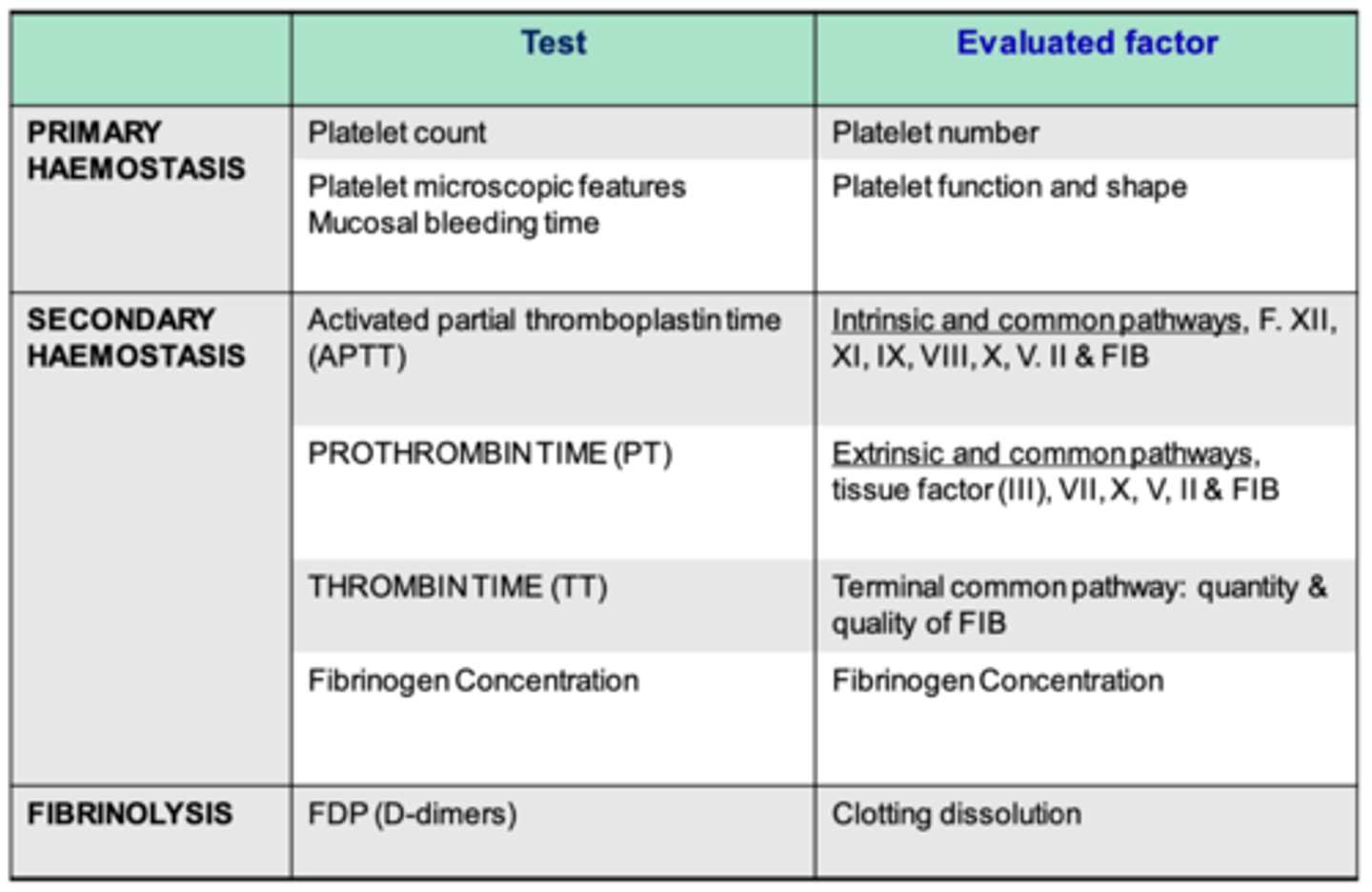
what tests/laboratory evaluation are used to evaluate primary hemostasis?
platelet count
platelet microscopic features
mucosal bleeding time

how can we evaluate the number of platelets an animal has?
platelet count
how do we evaluate the function of an animal's platelets?
mucosal bleeding time test
what laboratory tests/evaluations do we use to evaluate secondary hemostasis?
activated platelet thromboplastin time- intrinsic and common pathways
prothrombin time- extrinsic and common pathways
thrombin time- terminal common pathway
fibrinogen concentration
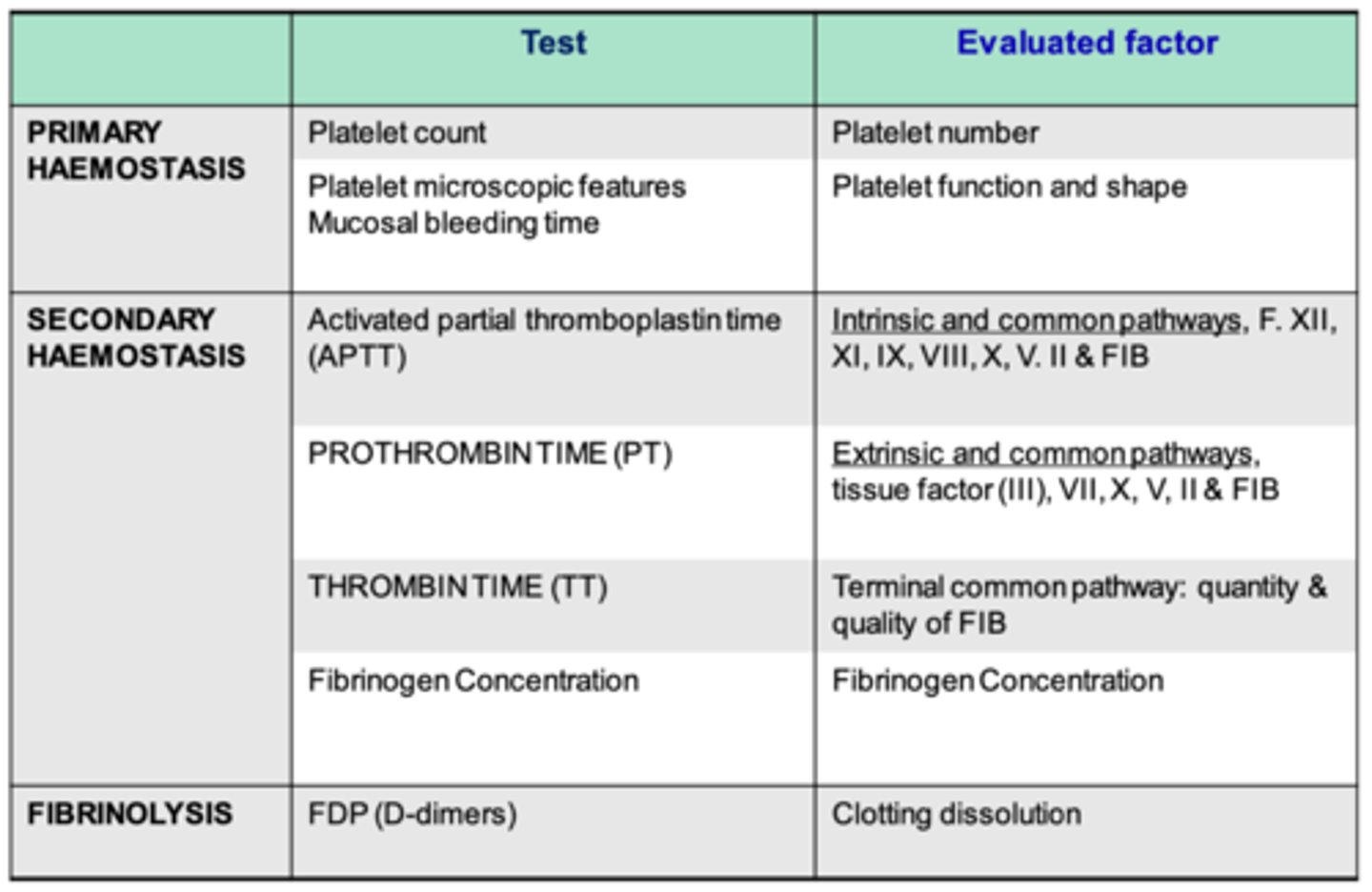
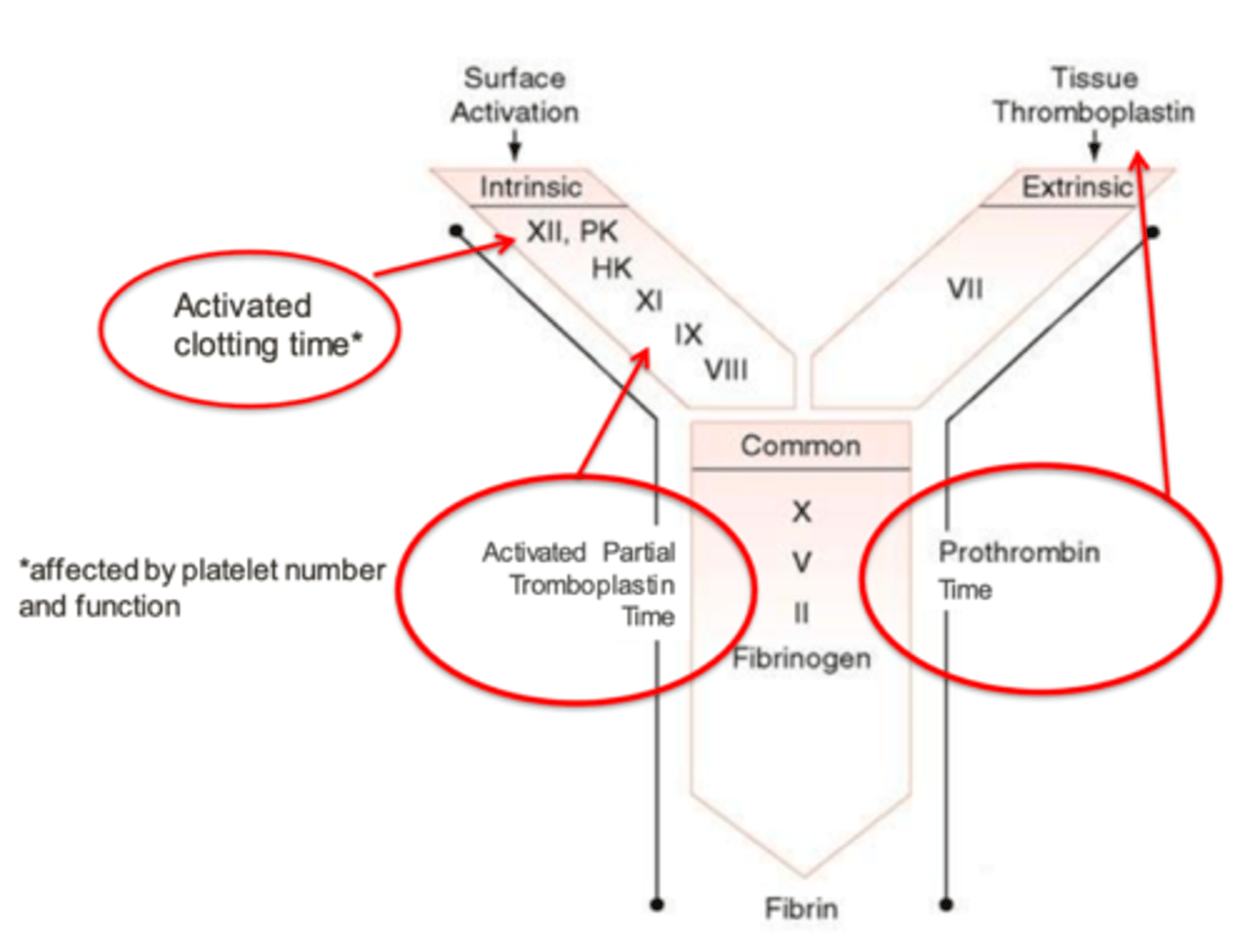
what is the activated partial thromboplastin time used to evaluate?
intrinsic and common pathways (factors XII, XI, IX, VIII, X, V, II, and FIB)
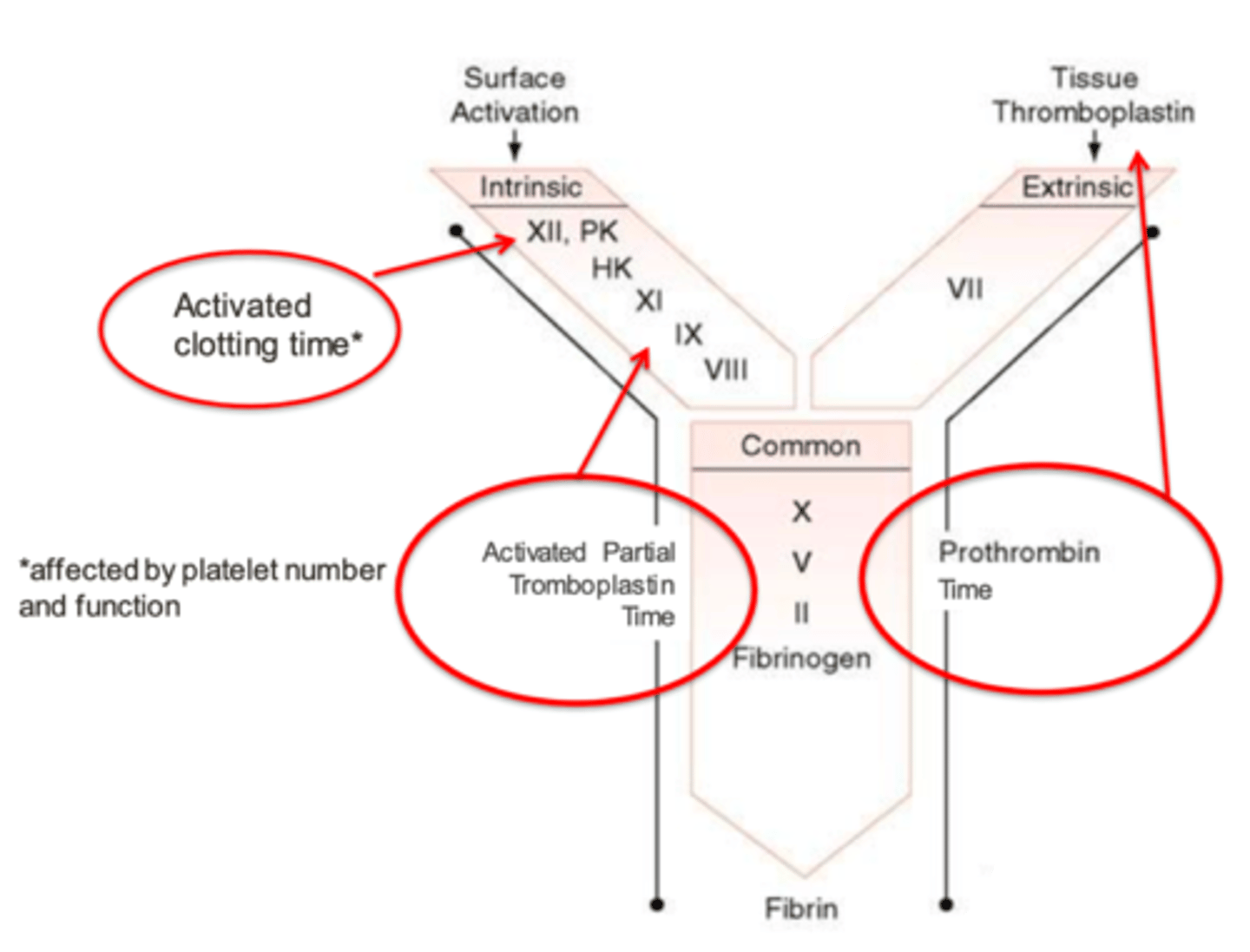
what is the prothrombin time test used to evaluate?
extrinsic and common pathways (factors III, Vii, X, V, II, and FIB)
what is the thrombin time test used to evaluate?
the terminal common pathway (the quantity and quality of fibrinogen)
what test do we use in the lab to evaluate the clotting dissolution?
FDP (D-dimers)
what does the platelet count give us information about?
if the patient has thrombocytopenia or thrombocytosis
how do we perform a platelet count?
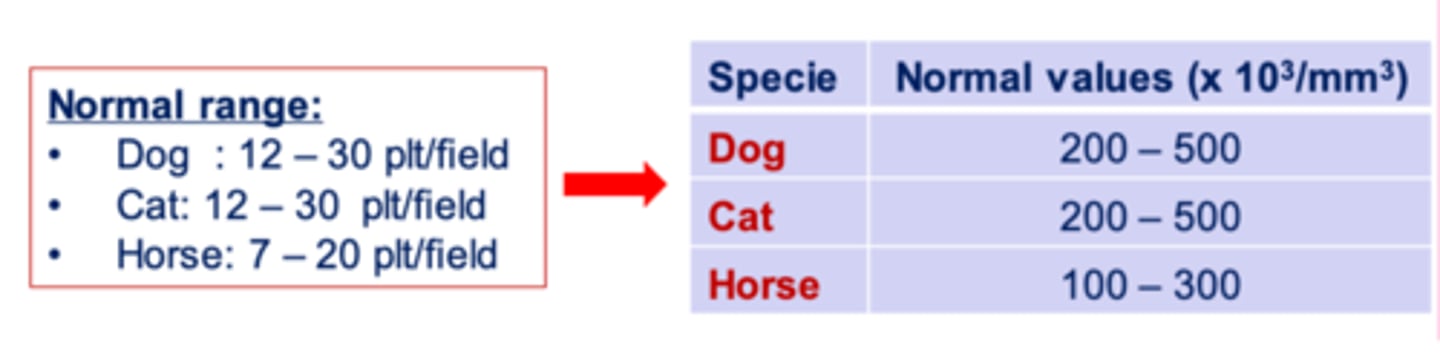
it can be either manual or automatic
manual: we do a blood smear using a sample with EDTA. we count the number of platelets per field, and then multiply this by 15,000.
if we perform a platelet count and the number is lower than the normal range for that species, we call this...
thrombocytopenia
if we perform a platelet count and the number is higher than the normal range for that species, we call this...
thrombocytosis
which is more common to see, thrombocytosis or thrombocytopenia?
thrombocytopenia
what are possible etiologies behind thrombocytopenia?
congenital (breed related)
increased platelet use: DIC, hemangiosarcoma
increased platelet destruction: immunomediated, infectious
low platelet production: BM disease, chemotherapy, FIV, FeLV, NSAIDs
if an animal has moderate thrombocytopenia (40-100 x10^3), what do we expect clinically?
possible bleeding
if a patient is spontaneously bleeding, what do we expect to see in their platelet count?
severe thrombocytopenia (less than 40 x10^3)
which is more reliable for counting the platelets in a blood sample- manual or automatic (with a machine)?
manual, using a blood smear
the automatic platelet counting machine is not very reliable
what are the possible etiologies behind thrombocytosis?
bone marrow disease
iron deficiency anemia
nephrotic syndrome
myeloidal metaplasia
trauma
FeLV, FIV
chronic inflammatory disease
neoplasia
aggregations of platelets are common in what species?
this causes what type of result in a platelet count?
cats; pseudothrombocytopenia
what is the best way for us to determine the platelet function (how well the platelets are working) in an animal?
performing a mucosal bleeding time test.
for this, we make an incisions on the mucosa of the upper lip (in small animals) or of the vagina (in cattle) and measure the amount of time it takes for it to stop bleeding.

what is the mucosal bleeding time?
it is a test we use to determine the functionality of the platelets.
for this, we make an incisions on the mucosa of the upper lip (in small animals) or of the vagina (in cattle) and measure the amount of time it takes for it to stop bleeding.
if the time is higher than normal, this indicates vascular abnormalities, lack of platelets, or defects of platelet function
if we test the mucosal bleeding time in a dog and it is 7 minutes, what do we predict?
this is too high. the normal range for dogs is under 4 minutes.
this indicates vascular abnormalities, lack of platelets, or defects of platelet function
what is the normal mucosal bleeding time of a horse?
10-14.5 minutes
what is the normal mucosal bleeding time of a dog?
less than 4 minutes
what is the normal mucosal bleeding time of a cat?
1-2.5 minutes
how do we determine the platelet function automatically (not using the mucosal bleeding time test)?
we have a machine that does this automatically. it stimulates capillary flow conditions, and counts the time needed for the platelets to tap the capillary hole in a membrane coated with collagen/epinephrine or collagen/ADP.
this allows us to evaluate platelet aggregations and adhesion to detect platelet disorders.

prothrombin time (PT) evaluates what pathways?
extrinsic (VII) and common (X, V, II, I)
if there is a high concentration of fibrin degradation products, this can indicate what etiologies?
DIC
intoxication by a vitamin K agonist
hepatic disease
hypofibrinogenemia can be caused by...
DIC
advanced liver disease
a decreased antithrombin III indicates....
DIC
severe hepatopathy
protein loss nephropathy
enteropathy
after laboratory tests, we see that an animal has a LOW platelet count and a high mucosal bleeding time. This indicates:
thrombocytopenia
after laboratory tests, we see that an animal has a HIGH prothrombin time and a high activated partial thromboplastin time. This indicates:
hepatopathy
an animal who has been intoxicated by a rodenticide will show what abnormalities in their lab results?
VERY high prothrombin time (PT) and activated partial thromboplastin time (APTT)
after laboratory tests, we notice these results:
low platelet count
high mucosal bleeding time
high prothrombin time
high activated partial thromboplastin time
low fibrinogen
what do we think this animal has?
DIC
an animal with Hemophilia A or B will have what abnormality in their laboratory results?
high Activated partial thromboplastin time (APTT)
the FIB (fibrinogen) evaluation helps us to evaluate what?
heparin in the lbood
hepatopathies (low FIB)
DIC (low FIB)
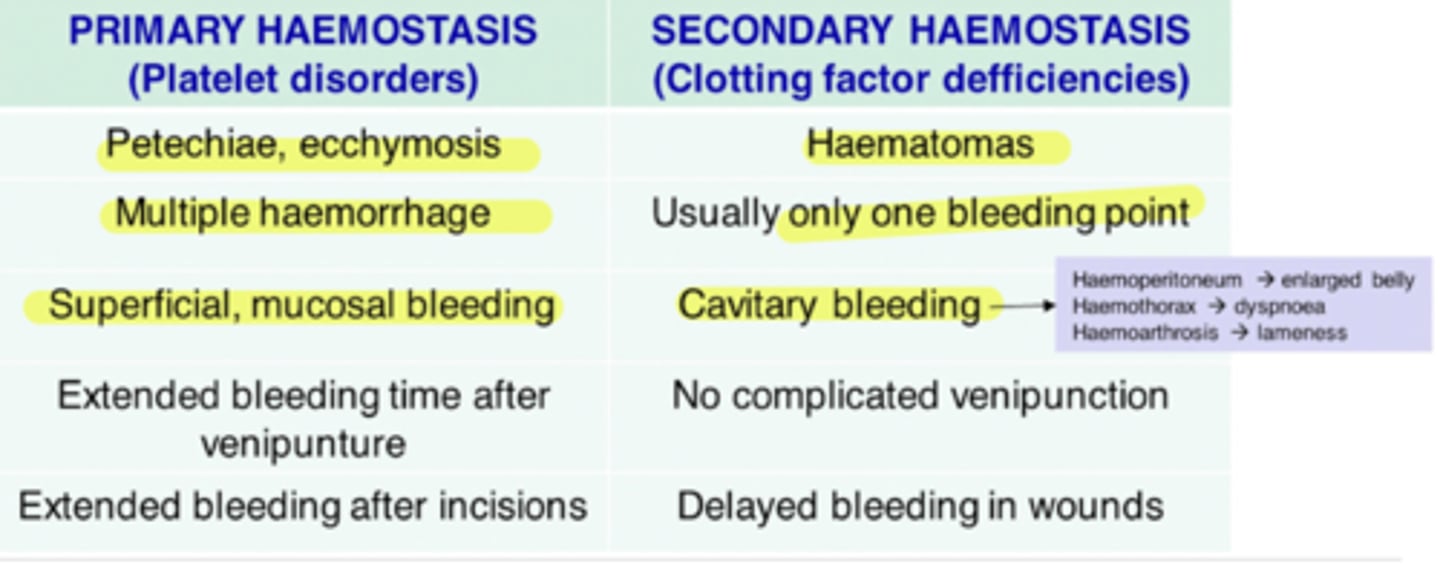
what are the clinical differences between a primary hemostasis disorder and a secondary hemostasis disorder?
primary: petechia, ecchymosis, multiple hemorrhage, superficial mucosal bleeding, longer bleeding after venipuncture and incisions
seconday: hematomas, only 1 bleeding point, cavitary bleeding, delayed bleeding in wounds
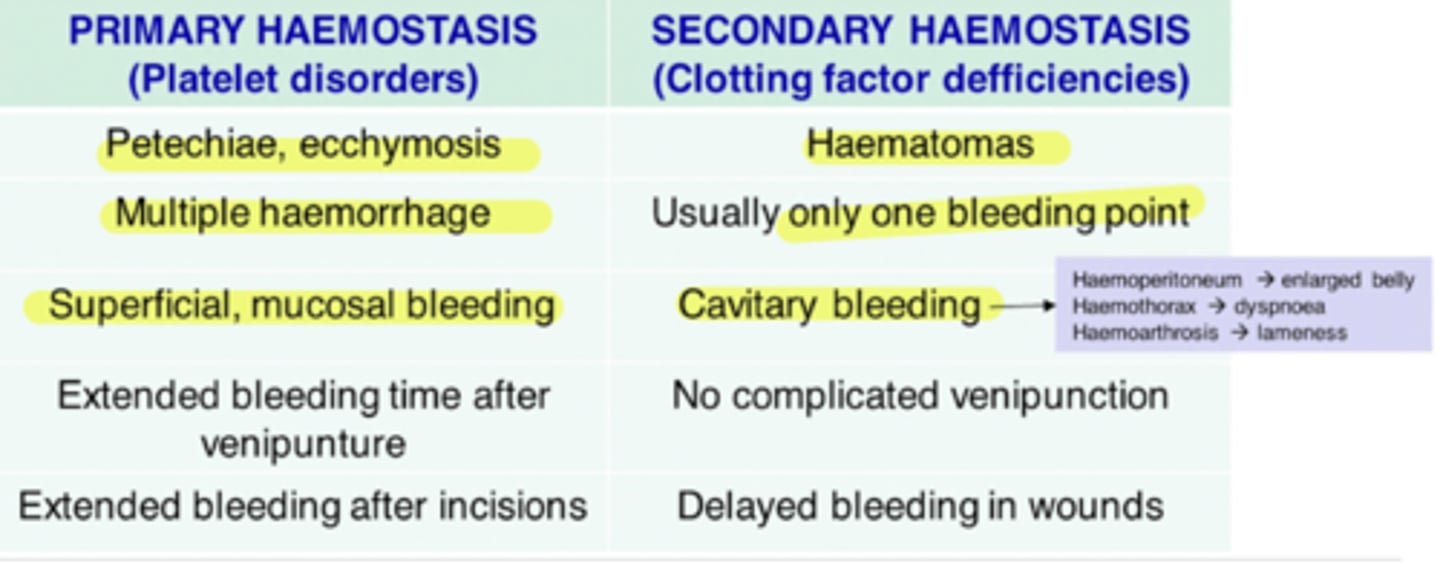
if an animal presents to us with petechia, ecchymosis, and superficial mucosal bleeding, do we suspect a problem with primary or secondary hemostasia?
primary
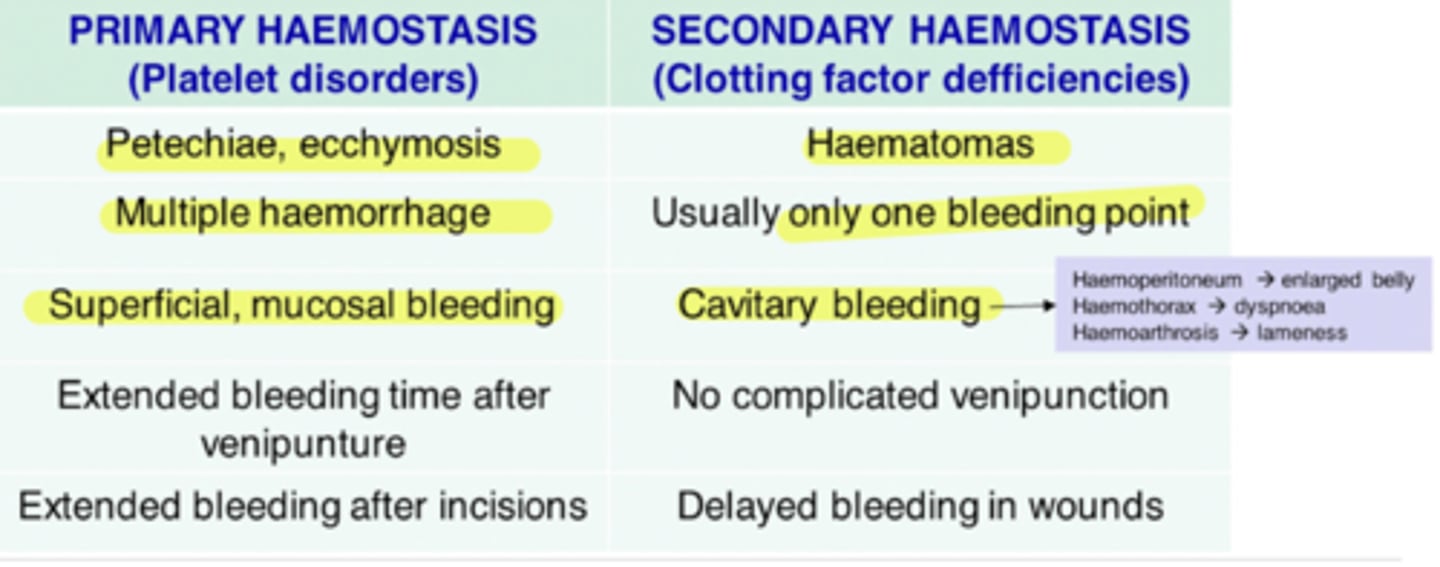
an animal with a problem with secondary hemostasia will have these clinical signs:
hematomas
one bleeding point
cavitary bleeding
delayed bleeding in wounds
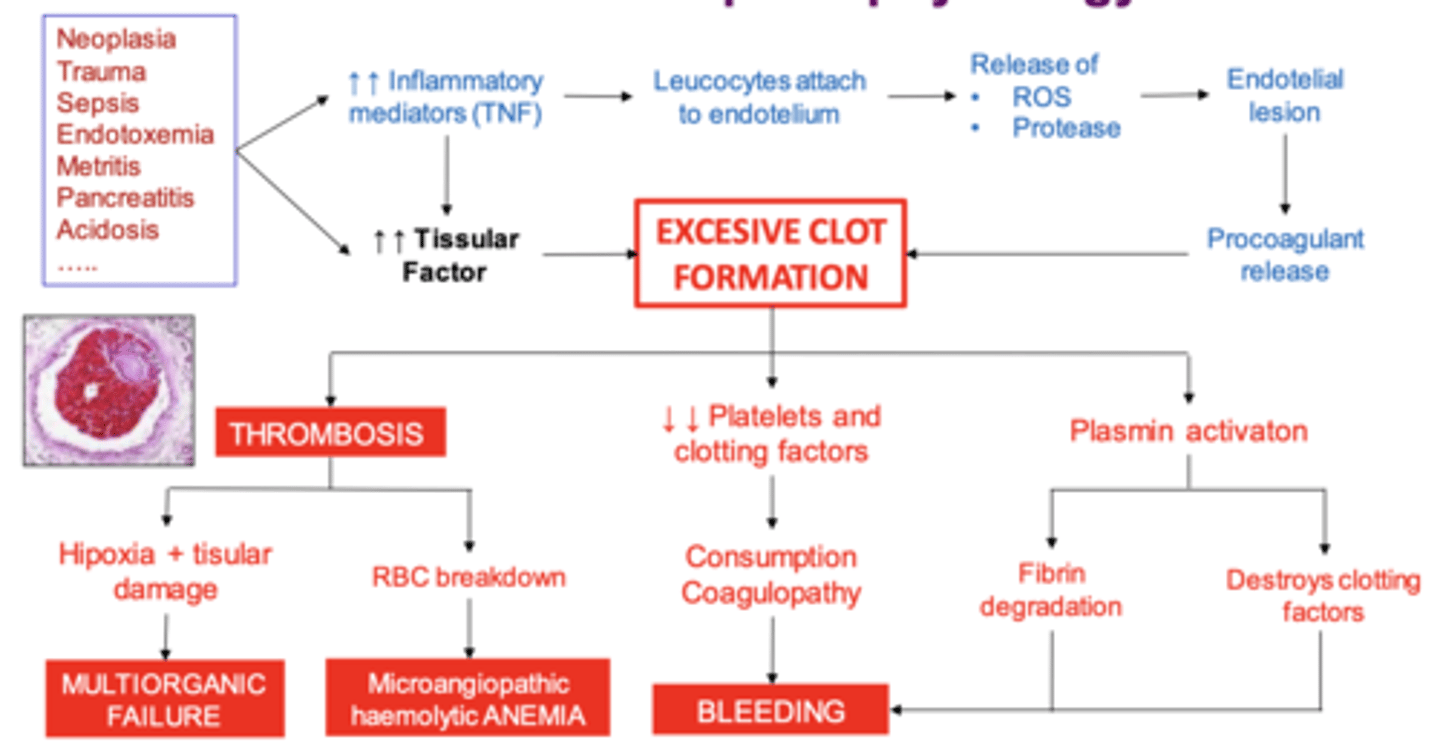
what are possible causes of DIC?
neoplasia
trauma
sepsis
endotoxemia
metritis
pancreatitis
acidosis
ETC (there are MANY)
explain the pathophysiology of DIC
1. initial cause
2. increased inflam. mediators and tissue factor
3. excessive clot formation
4. thrombosis, decreased platelets, plasmin activation
the thrombosis causes hypoxia and tissue damage, which causes multiorganic failure, as well as the breakdown of RBCs, which leads to anemia.
the decreased platelets and clotting factors and plasmin activated leads to bleeding
so at the same time, there is thrombosis and bleeding, causing damage to many organs in the body