Cell injury and death
1/63
Earn XP
Description and Tags
gen. pathology dmd3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
What are the causes of cell injury?
oxygen deprivation
chemical agents
infectious agents
immunologic reactions
genetic defects
nutritional imbalance
physical agents
aging
What is hypoxia?
oxygen deficiency
interferes with aerobic oxidative respiration
pneumonia, anemia, or carbon monoxide poisoning is what type of condition?
hypoxia
what is the most common cause of hypoxia?
ischemia
what are some chemical agents that can cause cell injury or death?
-glucose
-salt
-oxygen
what are some infectious agents that can cause cell injury or death?
bacteria
fungi
protozoans
what are some immunologic reactions that can cause cell injury or death?
autoimmune reactions against own’s tissues and allergic reactions
what are some genetic defects that can cause cell injury or death?
congenital malformations in Down syndrome, hemoglobin S and sickle cell anemia, deficiency of functional proteins, and damage or misfolded DNA.
what are some nutritional imbalances that can cause cell injury or death?
protein-calorie insufficiency, vitamin deficiencies, excess of animal fat, etc.
what are some physical agents that can cause cell injury or death?
-trauma
-extreme temperatures
-radiation
-electric shock
-sudden change in atmospheric pressure
what is cellular senescence
a state where cells stop dividing but remain metabolically active (aging)
-diminished ability to respond to damage
cellular injury results from?
functional and biochemical abnormalities in one or more of several essential cellular components.
What are some essential cellular components?
mitochondria
cell membrane
protein synthesis
cytoskeleton
genetic apparatus
What are the importance of ATP
oxidative phosphorylation and glycolytic pathway
What causes ATP depletion?
-reduced supply of oxygen and nutrients
-mitochondrial damage
-actions of some toxins
What happens when there is an increase pf cytosolic Ca2+
it activates a number of enzymes with potentially deleterious cellular effects
phospholipases causes?
membrane damage
proteases break down both?
membrane and cytoskeletal proteins
endonucleases for?
DNA and chromatin fragmentation
adenosine triphosphatases hastes?
ATP depletion
increased intracellular Ca2+ levels results in the induction of?
apoptosis
depleting extracellular Ca2+ delays?
cell death after hypoxia and exposure to some toxins
what are free radicals?
chemical species with a single unpaired electron in an outer orbital; highly reactive
what is oxidative stress?
excess of free radicals
what is reperfusion?
the restoration of blood flow to a tissue or organ that has been deprived of circulation (ischemia)
plasma membrane can be damaged by?
-ischemia
-microbial toxins
-lytic complement components
-physical and chemical agents
what is autophagy
lysosomal digestion of cell’s own components
survival mechanism during nutrient deprivation
what is heterophagy
cell ingests substances from the outside for intracellular destruction
what are residual bodies
undigested debris persistent within the cell
examples of residual bodies
lipofuscin pigments
carbon particles
tattoo pigments
what is hemosiderin
a hemoglobin-derived granular pigment that is golden yellow to brown and accumulates in tissues when there is a local or systemic excess of iron
iron is normally stored within?
apoferritin
apoferritin forms?
ferritin micelles
large aggregates of ferritin micelles are seen as?
hemosiderin pigment
hemosiderosis is?
a condition characterized by the excessive accumulation of hemosiderin, an iron-storage complex, in tissues.
if there is an impressive accumulation of systemic hemosiderosis what happens?
the iron pigment does not damage the parenchymal cells or impair organ function
what is pathologic calcification?
the abnormal deposition of calcium salts, together with smaller amounts of iron, magnesium, and other minerals
when calcification occurs in dead or dying tissues it is called?
dystrophic calcification
deposition of calcium salts in normal tissues called?
metastatic calcification
when does dystrophic calcification occur?
occurs in the absence of calcium metabolic derangements
metastatic calcification reflects derangement in ?
in calcium metabolism (hypercalcemia)
true or false
necrotic cells are unable to maintain membrane integrity, and their contents often leak out
true
the enzymes responsible for digestion of the cell are derived from?
lysosomes
what are the patterns of tissue necrosis?
coagulative necrosis
liquefactive necrosis
gangrenous necrosis
caseous necrosis
fat necrosis
fibroid necrosis
tissue necrosis in which the component cells are dead but the basic tissue architecture is preserved for at least several days
coagulative necrosis
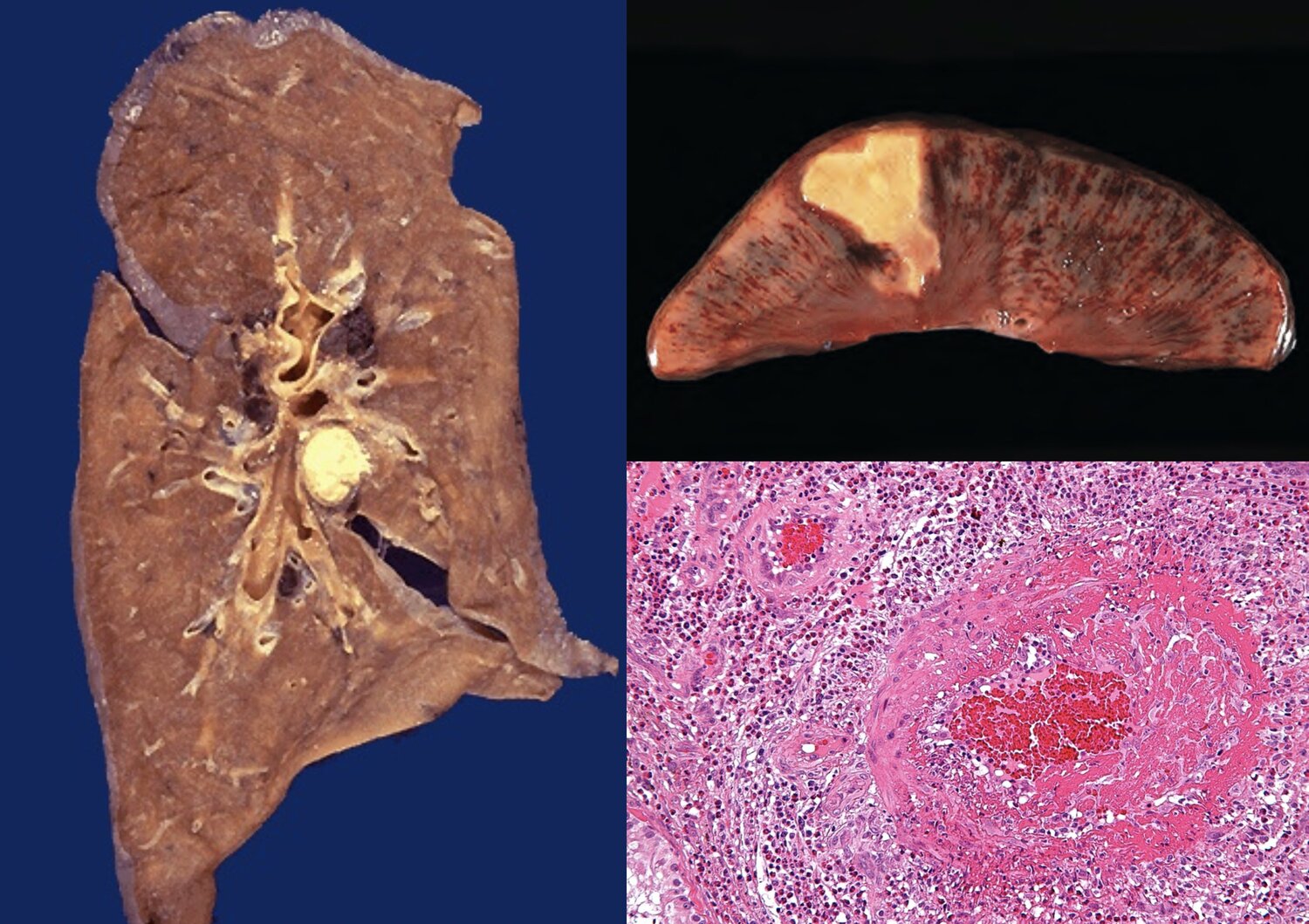
coagulative necrosis is characteristics of infarcts in all solid organs except?
the brain
areas of tissue that have undergone necrosis due to a blockage in the local blood supply, leading to a lack of oxygen and nutrients
infarcts
a type of necrosis where the necrotic tissue is transformed into a liquid or viscous mass, often due to enzymatic digestion
liquefactive necrosis
necrosis seen in focal bacterial or fungal infections
liquefactive necrosis
hypoxic death of cells within the central nervous system often evokes…
liquefactive necrosis
true or false
liquefaction digests the dead cells partially
false
liquefaction completely digests the dead cells
if liquefactive necrosis was initiated by acute inflammation what happens to the material?
the material is frequently yellow = pus
necrosis that is the result from the loss of blood supply and has undergone coagulative necrosis involving multiple tissue layers
gangrenous necrosis
gangrenous necrosis is usually applied to?
a limb (usually lower leg)

gangrenous necrosis and liquefactive action is called
wet gangrene
necrosis characterized by a cheese-like appearance of the affected tissue; yellow-white
caseous necrosis

necrosis most often in foci of tuberculous infection
caseous necrosis
on microscope caseous necrosis appears as?
a collection of fragmented or lysed cells with an amorphous granular appearance
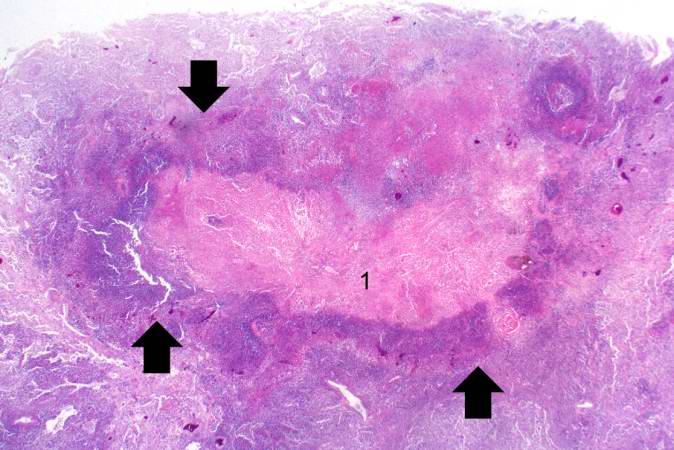
caseous necrosis often enclosed within a distinctive inflammatory border called?
granuloma
a special form of necrosis usually seen in immune reactions involving blood vessel
fibrinoid necrosis
deposits of immune complexes together with fibrin that leaked out of vessel resulting in a bright pink and amorphous appearance in H&E stains called?
fibrinoid
what is the programmed destruction of cells during embryogenesis
apoptosis
cell death kind involving endometrial cell breakdown in menstruation
apoptosis
kind of cell death regression of lactating breast after weaning
apoptosis