anemias lab med
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
a decrease in the total amount of RBCs and/or hemoglobin to carry oxygen to the body’s tissues
anemia
what big overarching causes can cause anemia
dec RBC production, blood loss, RBC destruction
what can cause a dec in RBC production leading to anemia
hormone imbalance (dec EPO, T3/T4)
nutritional deficiencies (dec iron, B12, or folate)
meds (chemo meds suppress bone marrow, NSAIDS
toxins (alc)
intrinsic bone marrow dysfunction
chronic disease (anything autoimmune, aplastic anemia, leukemia, other cancers, etc)
genetic disorders
what is the MAIN reason for dec RBC production
intrinsic bone marrow dysfxn
what can cause blood loss leading to anemia
trauma/surgery (duh)
heavy menstrual bleeding
GI bleeding (ulcers/polpys)
what can cause RBC destruction leading to anemia
hemolysis
intravascular mechanical, autoimmune, infections, or toxins (i.e sickle cell anemia, thasslemia, malaria, HIV, mono
extravascular destruction (more common)
genetic disorders
regular anemia sx
jaundice in skin/eyes, pale/cold skin, SOB, muscular weakness, change in stool color, fatigue, dizzy, hypotension, heart palpitations, inc HR, splenomegaly, hepatomegaly
severe anemia sx
fainting, chest pain, angina, heart attacks
reflex tests we do to eval any kind of anemia
peripheral blood smear
bone marrow biopsy
reticulocyte count (including immature reticulocyte fraction and reticulocyte hemoglobin content (CHr))
haptoglobin
bilirubin (esp seen in hemolysis)
direct antibody test (DAT) for autoimmune concerns
what is the most important test to do for anemia and why
reticulocyte count, bc reticulocytes are baby RBCs and seeing them tells us if theres an inc in RBC production/RBCs being put out too soon. indicator of bone marrow fxn to produce RBCs(tells if the problem is in the bone marrow or not)
a test measuring the number of reticulocytes in circulation. can be done as part of a CBC (manual/automated cell differential where reticulocytes stain slightly bluer than normal RBCs in wright-giemsa stain) or can be specifically stained for it
reticulocyte count
if we have lots of reticulocytes will our MCV (vol measure) go up or down
up bc reticulocytes are bigger and have more Hgb
if we have lots of reticulocytes will our MCHC (color measure) go up or down
down bc reticulocytes are more pale
what specific stains can we do to look at reticulocytes
brillian cresyl blue (BCB) or New methylene blue (NMB) (both target the RNA residues in reticulocytes)
% retics =
retic count / RBC count
(depends on the number of retics in circulation, number of RBCs, and retic maturation time)
what could a low reticulocyte count indicate
bone marrow failure/dysfxn (not producing enough RBCs)
what could a high reticulocyte count indicate
normal bone marrow fxn and the body compensating for anemia by making more RBCs (means either hemolysis or hemorrhage)
what time frame does reticulocyte count reflect changes in and whats it used for
reflects changes in the last 18-24hrs, used to determine the possible cause of an anemia or monitor
to correct for variance in reticulocyte maturation time in circulation and the total number of circulating RBCs what do we calculate
reticulocyte index (esp important for anemia pts bc it corrects to normal hematocrit and its dependent on Hgb level)
whats the formula for the reticulocyte index
retic index = observed retic count (%) X observed PCV/45
what does a low (under 2%) reticulocyte index indicate
bone marrow failure/dysfxn (not making enough RBCs)
what does a high (over 2%) reticulocyte index indicate
normal bone marrow fxn and the body compensating fro anemia by making more RBCs (aka anemia caused by hemorrhage/hemolysis)
a comparison between immature and mature reticulocytes in circulation (bc younger retics have more RNA)
immature reticulocyte fraction/ reticulocyte maturity index
a measure of reticulocyte Hbg content in real time and the equivalent to the MCH for reticulocytes
reticulocyte RET-He
measures the functional avaliability of iron during Hb synthesis and is the equivalent to MCHC for reticulocytes
CHr
what does dec reticulocyte RET-He/CHr mean
sensitive and early marker of iron-restricted erythropoiesis (can dec even more before iron def anemia develops)
strongest predictor of iron deficiency and iron deficient anemia in kids under 2yo
types of anemia based on RBC indicies (MCV and MCHC)
microsytic/hypochromic, normocytic/normochromic, macrocytic/hyperchromic (or normochromic)
small and pale RBCs with low MCV/MCHC and high RDW
microcytic-hypochromic anemia
most common cause of anemia
microcytic-hypochromic anemia
most common cause of microcytic-hypochromic anemia
iron deficiency (can be from not eating enough or malabsorbtion)
if pt w microcytic-hypochromic anemia has normal serum ferritin and serum iron % transferrin saturation what could be some possible other causes of the anemia
sideroblastic anemia (cant use iron right, will see basophilic stippling and iron builds up, may be sign of iron poisoning)
anemia of chronic disease (autoimmune, ferratin really high)
thalassemia (2nd most common cause of microcytic-hypochromic anemia, body cant make hemoblobin so MCV hellaaaaaa low)
a test that separates diff types of hemoglobin in the blood by electric current, used to investigate, dx, screen, and monitor abnormal hemoglobin disorders
hemoglobin electrophoresis
HgbS on hemoglobin electrophoresis =
sickel cell anemia
HgbC on hemoglobin electrophoresis =
hemolytic anemia
normal sized and normal colored RBCs, MCV, MCHC and RDW are in range
normocytic-normochromic anemia
most common cause of normocytic-normochromic anemia
anemia of chronic disease (esp in hospitalized pts)
abnormally large RBCs w more Hgb, high MCV and MCHC
macrocytic-hyperchromic anemia
what is the main cause of macrocytic-hyperchromic anemia
megaloblastic anemias (B12/folate deficiencies), also often will see hypersegmented neutrophils
test that measures the amount of MMA (organic byproduct of protein metabolism) and the higher the MMA is the lower the B12 is, helpful in early or mild B12 deficiency
methylmalonic acid
an amino acid byproduct of methionine metabolism (not used to bueld proteins),
homocysteine
when homocysteine is high (hyperhomocyteinemia) what does that mean
vit B6, B9, B12 deficiency (inc risk of stroke, coronary vasc disease, thrombus, osteoporosis, cognitive decline
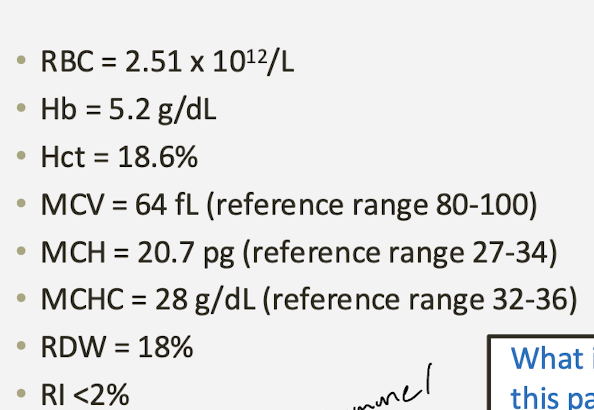
what does this pt have
microcytic, hypochromic anemia
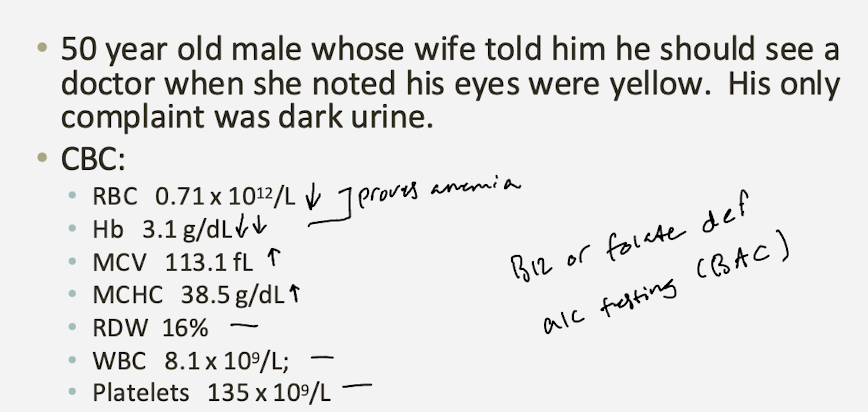
what does this pt have
macrocytic anemia
when RBCs are broken down or destroyed faster than theyre made, stimulates reticulocytosis, sometimes classified as normocytic-normochromic and can be sorted into intrinsic adn extrinsic type
hemolytic anemia
pos DAT =
autoimmune
high LDH =
cells getting broken down
RBC destruction due to defect within RBCs (membrane/enxyme/hemoglobin defect) thats usually inherited (sickel cell, G6PDH, thalassemia, hereditary spherocytosis, paroxysmal nocturnal hemoglobinuria)
intrinsic hemolytic anemia
RBC destruction caused by factors outside of RBC, often acquired (microangiopathic, autoimmune, trauma, meds, injury) gotta check liver and spleen
extrinsic hemolytic anemia
test that measures a protein produced by the liver and binds w free Hgb to present damage to tissues adn is removed from blood by liver/spleen
haptoglobin
low haptoglobin =
oxidative stress/damage to tissues (hemolytic anemia, liver disease, CVD, CA)
high haptoglobin =
inflammation, meds
test that detects if RBCs are coated w antibodies
direct antibody test
pos direct antibody test =
antibodies are present on RBCs, indicates autoimmune problem, associated w autoimmune hemolytic anemia , hemolytic disease of newbornm transfusion rxn, drug induced hemolysis
neg direct antibody test =
no antibodies on RBCs
excessive blood loss causing anemia, no signs of hemolysis on lab tests, past med hx and presentation is important bc may see fatigue, pallor, dizzy, SOBm tachycardia, cold hands and fet, dry mucous membranes, dec cap refil, easy bruising, or active bleeding
hemorrhagic anemia