7. Adaptive Immunity
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
What is adaptive immunity also known as?
Adaptive immunity is also known as acquired immunity, immune response, or simply immunity.
What cells are involved in adaptive immunity?
Adaptive immunity involves lymphocytes and antibodies.
When is adaptive immunity activated?
Adaptive immunity is activated after the secondary line of defense (the inflammatory response).
How does the speed of adaptive immunity compare to the second line of defense?
Adaptive immunity is slower than the second line of defense (inflammatory response).
What does adaptive immunity provide?
Adaptive immunity provides long-term security against reinfection.
What does it mean that adaptive immunity is inducible?
Adaptive immunity is inducible, meaning lymphocytes and antibodies must be produced in response to an infection.
How is adaptive immunity specific?
Adaptive immunity is specific because lymphocytes and antibodies are tailored to the infecting microbe.
How is adaptive immunity long-lived and systemic?
Adaptive immunity provides long-term protection against specific infections and acts throughout the body.
What does it mean that adaptive immunity has memory?
Adaptive immunity has memory, allowing for an immediate response if the body is reinfected by the same pathogen in the future.
What is active immunity?
Active immunity is when the body is exposed to an antigen, either naturally (infection) or through immunization (vaccine), prompting the immune system to produce antibodies and memory cells.
What is passive immunity?
Passive immunity occurs when preformed antibodies or T cells are administered, providing temporary protection without the body having to produce its own antibodies.
Can you provide an example of active immunity?
An example of active immunity is immunization, such as the Hepatitis A vaccine, which stimulates the body to produce its own antibodies.
Can you provide an example of passive immunity?
An example of passive immunity is the administration of antibodies in cases like the Ebola outbreak in Dallas, where preformed antibodies were given to help fight the infection.
What is clonal diversity in the immune response?
Clonal diversity refers to the production of a wide variety of T and B lymphocytes before birth, ensuring that the immune system can recognize and respond to a vast array of antigens.
Where do B and T lymphocytes mature?
B lymphocytes mature in the bone marrow, while T lymphocytes mature in the thymus.
What is antigen recognition?
Antigen recognition is the process by which lymphocytes (B and T cells) identify foreign substances (antigens) through specific receptors on their surfaces.
What is clonal selection?
Clonal selection is the process by which an antigen activates a specific lymphocyte, causing it to proliferate and form a clone of cells that are specific to that antigen.
What is the role of antigen processing and presentation?
Antigen processing and presentation involves the breaking down of antigens into smaller pieces that are displayed on cell surfaces, allowing immune cells like T cells to recognize and respond to the antigen.
Clonal diversity
before infection
create diverse immature cells
bone marrow and thymus
many different B and T cells
Clonal selection
after infection
activate specific immune cells
lymph nodes, spleen, bloodstream
expansion of the right B or T cell for the infection
What is the generation of clonal diversity?
It is the process by which the immune system produces all necessary receptor specificities to recognize a vast array of antigens.
Where does the generation of clonal diversity take place?
It occurs in the primary (central) lymphoid organs—thymus and bone marrow.
What is the result of the generation of clonal diversity?
It produces immature but immunocompetent T and B cells, meaning they can recognize antigens but require activation.
When does the generation of clonal diversity primarily occur?
It primarily occurs before birth, in the fetus.
Where does B cell development occur?
In the bone marrow, where B cells undergo production, proliferation, and differentiation.
Where do B cells go after developing in the bone marrow?
They travel to lymphoid tissue and reside there as immunocompetent cells.
secondary organs
How many antigens can each B cell respond to?
Each B cell responds to only one specific antigen.
Where does T cell development occur?
In the thymus, the central lymphoid organ for T cell development.
What is the key feature of developing T cells?
They develop antigen-specific T cell receptors (TCRs).
Where do T cells go after leaving the thymus?
They travel to and reside in lymphoid tissue as mature immunocompetent cells.
secondary organs
What initiates clonal selection?
Clonal selection begins when T and B cells interact with an antigen.
What must happen before T and B cells can respond to an antigen?
The antigen must first be processed and presented by antigen-presenting cells (APCs).
What is the result of B cell activation during clonal selection?
B cells differentiate into active antibody-producing plasma cells.
What happens to T cells during clonal selection?
T cells differentiate into effector cells, such as T cytotoxic cells.
What three conditions must be met for antigen processing and presentation to occur?
The antigen must be of the appropriate type.
Lymphocytes must be prepared to recognize the antigen.
The antigen must be presented appropriately.
What is the first step in clonal selection?
Processing and presentation of antigens by antigen-presenting cells (APCs).
What specialized molecules are involved in antigen processing?
Major histocompatibility complex (MHC) molecules.
Where are major histocompatibility complex (MHC) molecules found?
On the surface of all human cells except red blood cells (RBCs).
What are MHC molecules called in humans?
Human leukocyte antigens (HLAs).
What cells are MHC I molecules presented on
All nucleated cells and platelets
Is MHC I endogenous or exogenous?
Presents endogenous antigen
What cells to MHC I molecules recruit
Recruits CD8 Tc Cells
What cells are MHC II molecules presented on
Expressed only on antigen-presenting cells (APC’s):
macrophages
dendritic cells
B cells
Is MHC II endogenous or exogenous?
Presents exogenous antigen
What cells to MHC II molecules recruit
Recruits CD4+ Th Cells
Mnemonic
A good way to remember the difference between MHC class I and MHC class II
molecules is by using the "8 Rule" and understanding their function:
1. The "8 Rule" (Multiplication Rule)
• MHC I × CD8 = 8 → MHC class I interacts with CD8+ T cells (Cytotoxic T cells).
• MHC II × CD4 = 8 → MHC class II interacts with CD4+ T cells (Helper T cells).
2. Who Presents What?
• MHC I = 1 letter = All nucleated cells → Presents endogenous antigens (e.g.,
viruses, cancer proteins).
• MHC II = 2 letters = Only APCs (Antigen-Presenting Cells) → Presents
exogenous antigens (e.g., bacteria, fungi).
3. Pathway Mnemonics
• MHC I → "I’m infected" → Presents intracellular pathogens (virus-infected cells)
to CD8+ cytotoxic T cells.
• MHC II → "Help me too" → Presents extracellular pathogens (phagocytosed
bacteria) to CD4+ helper T cells
What happens when an immunocompetent B cell encounters an antigen for the first time?
B cells with specific B cell receptors (BCRs) are stimulated to differentiate and proliferate.
What does a differentiated B cell become?
A plasma cell.
What is the function of a plasma cell?
A plasma cell acts as a factory for antibody production.
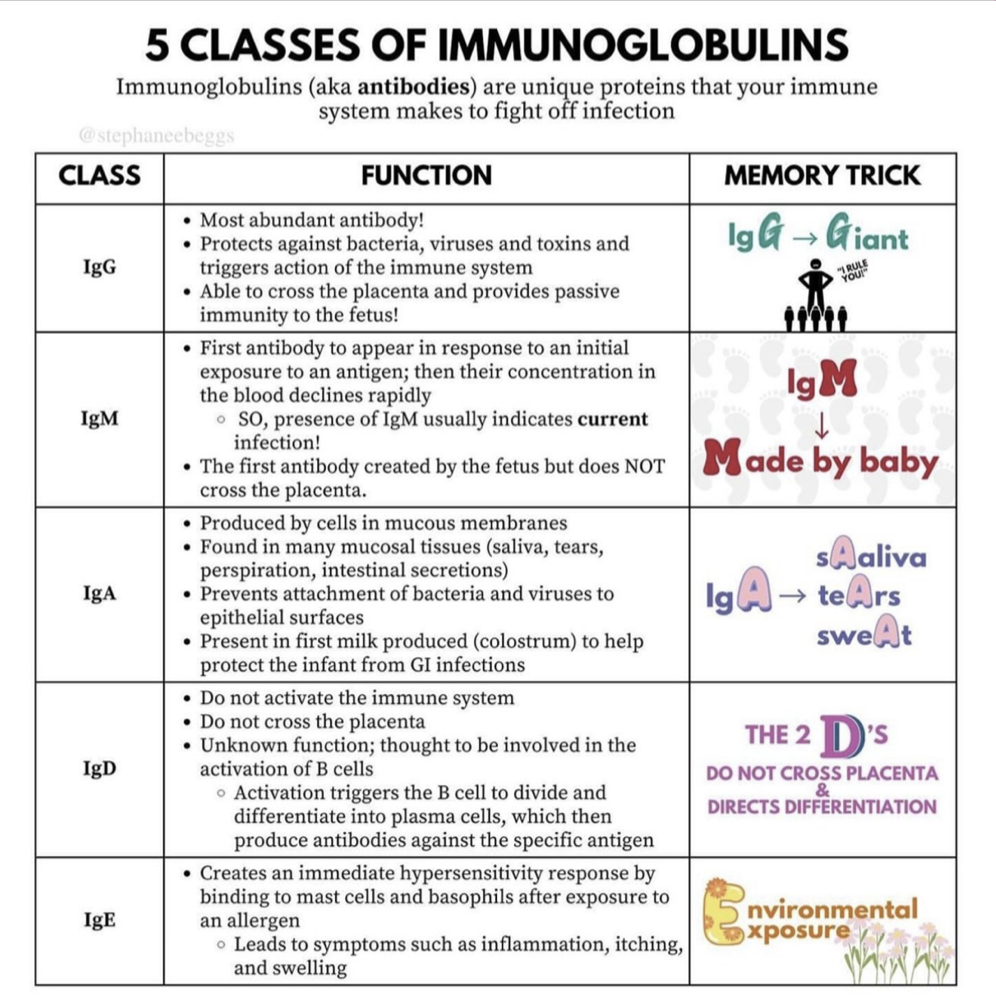
What are the five classes of antibodies produced by plasma cells?
IgG, IgM, IgA, IgD, and IgE.
What is an antigen?
A molecule that can bind with antibodies, T cell receptors, or B cell receptors.
How can the entry route of an antigen vary?
Antigens can enter the body through intravenous, intradermal, or oral routes.
What genetic factor can influence antigen response?
Atopy (a genetic predisposition to allergic diseases).
a parent who has very bad allergies may pass that down to their kid
What other factors can affect an immune response to antigens?
Nutrition, concurrent disease, and drugs.
What allergy is penicillin related to?
Shellfish allergy (due to a shared chemical base).
What are immunoglobulins?
Immunoglobulins (antibodies) are proteins produced by plasma cells that help fight infections.
What is another name for immunoglobulins?
Antibodies (the terms are interchangeable).
Where are immunoglobulins produced?
Plasma cells (which originate from B cells).
What are the five types of immunoglobulins?
IgG, IgA, IgM, IgD, IgE (Tip: GAMED or G-MADE).
Do all immunoglobulins have the same structure and function?
No, each type has a different structure and function.
What is the most abundant immunoglobulin?
IgG (80%-85% of total antibodies).
What is the main function of IgG?
It provides most of the protective activity against infections.
How does IgG help newborns?
IgG is transported across the placenta and protects the infant for the first 6 months of life.
Ways to remember IgG
great
general
guard
goo goo ga ga
Where is IgA found?
In blood and bodily secretions (e.g., saliva, tears, mucus, and breast milk).
What is the function of the secretory piece in IgA?
It protects IgA from enzyme degradation, allowing it to function in mucosal immunity.
How to remember IgA
airways
alimentary (GI)
anti-adhesion
What is the largest immunoglobulin?
IgM is the largest of the immunoglobulins.
When is IgM first produced?
IgM is the first antibody produced during the primary immune response to an antigen.
When does IgM synthesis begin?
IgM is synthesized during fetal life.
Ways to remember IgM
massive
main (main immune response)
macro
What is known about the function of IgD?
There is limited information on the function of IgD.
What is the concentration of IgD in the blood?
IgD is found in low concentrations in the blood.
Where is IgD primarily located?
IgD is primarily on the surface of developing B lymphocytes, acting as an antigen receptor.
Ways to remember IgD
differentiation (differentiates B cells)
development (crucial role In development of B cells)
defense
Which immunoglobulin is the least concentrated in circulation?
IgE is the least concentrated of all immunoglobulin classes in circulation.
What is the primary function of IgE?
Defends against large parasites and mediates allergic responses.
How does IgE help protect against parasites?
IgE initiates an inflammatory reaction to attract eosinophils.
Why is IgE associated with allergies?
When produced against harmless environmental antigens, IgE triggers allergic reactions.
Where are the Fc portions of IgE bound?
The Fc portions of IgE are bound to mast cells.
Ways to remember Ige
allergEES
eisonphils
emergency (parasites)
help chart
How does an antigen bind to an antibody?
The antigen fits into the antigen-binding site of the antibody with specificity and is held there by chemical interactions.
What ensures the specificity of antigen-antibody binding?
The unique shape of the antigen-binding site on the antibody ensures specificity.
What type of interactions hold the antigen in place within the antibody?
Chemical interactions such as hydrogen bonds, ionic bonds, and Van der Waals forces.
What are the main functions of antibodies?
To protect against infection through both direct and indirect actions.
What are the direct antibody actions for protection?
Neutralization: blocks binding
Agglutination: helps clump particles together, making them easier to identify and remove from suspension.
Precipitation: making insoluble so it cannot be processed
What are the indirect antibody actions for protection?
Inflammation, Phagocytosis, Complement system activation.
How is the degree of antibody protection assessed?
By an antibody titer.
look at diagrams on charts
What is T cell activation in clonal selection?
T cell activation occurs when an antigen binds to specific T cell receptors (TCR) on a T cell, triggering its response.
What happens when an antigen binds to a T cell receptor (TCR)?
The binding of an antigen to the TCR activates the T cell, which can then undergo clonal expansion and differentiation.
What is one function of T cells after activation?
Activated T cells can directly kill foreign or abnormal cells, such as precancerous cells.
How do T cells assist other immune cells?
Activated T cells can help activate or assist other immune cells, enhancing the immune response (to then kill them)
What role do memory cells play in T cell clonal selection?
Memory cells are formed after T cell activation, providing long-term immunity by remembering the antigen for faster responses in future exposures.
How do different types of Th cells arise?
Different types of Th cells arise through different signaling events, with differentiation dependent on the cytokines involved.
What is the role of Th1 cells?
Th1 cells help develop Tc cells, contributing to cell-mediated immunity.
What do Th2 cells do?
Th2 cells help develop B cells, which are involved in humoral immunity.
What is the function of Th17 cells?
Th17 cells activate macrophages, playing a role in inflammation and defense against pathogens.
What is the role of Treg cells in the immune response?
Treg cells limit or suppress the immune response, helping to prevent excessive inflammation and autoimmunity.