Antibiotics
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
1.) Use of broad-spectrum antibiotics may cause an overgrowth of
a) viruses
b) parasites
c) hair
d) fungi
a) viruses
b) parasites
c) hair
d) fungi
2.) Your patient, Mr. Grace, reports taking isoniazid, rifampin, and pyrazinamide. Your patient is MOST likely being treated for which of the following conditions?
a) Endocarditis
b) Tuberculosis
c) HIV
d) Tonsillitis
a) Endocarditis
b) Tuberculosis
c) HIV
d) Tonsillitis
3.) An overgrowth of which of the following organisms is responsible for an antibiotic-associated diarrhea?
a) Clostridium difficile
b) Porphyromonas gingivalis
c) Staphylococcus aureus
d) Mucobacterium tuberculosis
a) Clostridium difficile
b) Porphyromonas gingivalis
c) Staphylococcus aureus
d) Mucobacterium tuberculosis
4.) A patient being treated for periodontal disease complains of a metallic taste. The drug that is causing the condition is:
a) Clindamycin
b) Metronidazole
c) Tetracycline
d) Augmentin
a) Clindamycin
b) Metronidazole
c) Tetracycline
d) Augmentin
5.) A two year old boy has an abscess related to tooth K and requires antibiotic therapy. With this information alone, which drug would be contraindicated?
a) Zithromycin
b) Penicillin
c) Tetracycline
d) Clindamycin
a) Zithromycin
b) Penicillin
c) Tetracycline
d) Clindamycin
6.) Patients may require antibiotic prophylaxis if they have which of the following conditions? CHOOSE 4
a) Prosthetic hip replacement
b) Congenital heart disease
c) Hypercholesterol
d) HBA1C below 8
e) Previous infective endocarditis
f) HBA1C above 8
g) Congestive heart failure
h) Cardiac arrhythmia
a) Prosthetic hip replacement
b) Congenital heart disease
c) Hypercholesterol
d) HBA1C below 8
e) Previous infective endocarditis
f) HBA1C above 8
g) Congestive heart failure
h) Cardiac arrhythmia
7.) Which of the following antiinfective agents is bacteriostatic, but may be bactericidal at higher dose levels?
a) Clindamycin
b) Metronidazole
c) Penicillin
d) Rifampin
a) Clindamycin
b) Metronidazole
c) Penicillin
d) Rifampin
8.) Which of the following medications can reduce the effectiveness of oral contraceptives?
a) Amoxicillin
b) Azithromycin
c) Erythromycin
d) Penicillin
e) All of the above
a) Amoxicillin
b) Azithromycin
c) Erythromycin
d) Penicillin
e) All of the above
9.) Mrs. Slocum presents with swelling and pain associated with an abscessed #6. She is being treated for rheumatoid arthritis with methotrexate. Which antibiotic would NOT be contraindicated?
a) Clindamycin
b) Amoxicillin
c) Penicillin
d) Augmentin
a) Clindamycin
b) Amoxicillin
c) Penicillin
d) Augmentin
10.) Which of the following antibiotics produces an exaggerated sunburn in a patient who has a brief exposure to sunlight while taking? CHOOSE 3
a) Tetracycline
b) Doxycycline
c) Levaquin
d) Vancomycin
e) Azithromycin
f) Metronidazole
a) Tetracycline
b) Doxycycline
c) Levaquin
d) Vancomycin
e) Azithromycin
f) Metronidazole
11.) When there are multiple species of bacteria causing an infection, which type of antibiotic would be used?
a) Narrow spectrum
b) Broad spectrum
c) Narrow and broad spectrums together
d) Any antibiotic would do
a) Narrow spectrum
b) Broad spectrum
c) Narrow and broad spectrums together
d) Any antibiotic would do
12.) A bacteriostatic antibiotic and a bacteriocidal antibiotic can be taken together
a) True
b) False
a) True
b) False
13.) Mrs. Fleming has been taking penicillin for a large endodontic abscess on #5. After a few days she notices that she has developed a vaginal yeast infection. This is an example of:
a) An unrelated infection
b) A different infection due to the endodontic abscess
c) A secondary infection
d) A superinfection
a) An unrelated infection
b) A different infection due to the endodontic abscess
c) A secondary infection
d) A superinfection
14.) A patient is allergic to penicillin and requires antibiotic premedication to prevent infective endocarditis. Which one of the following antibiotics would be the drug of choice?
a) Amoxicillin
b) Erythromycin
c) Clindamycin
d) Tetracycline
a) Amoxicillin
b) Erythromycin
c) Clindamycin
d) Tetracycline
15.) Arestin belongs to which class of antibiotics?
a) Tetracyclines
b) Penicillins
c) Quinolones
d) Macrolides
a) Tetracyclines
b) Penicillins
c) Quinolones
d) Macrolides
16.) Which of the following antibiotics are not recommended for use in dentistry? (CHOOSE 3)
a) Vancomycin
b) Tetracyclines
c) Macrolides
d) Aminoglycosides
e) Penicillins
f) Sulfonamides
a) Vancomycin
b) Tetracyclines
c) Macrolides
d) Aminoglycosides
e) Penicillins
f) Sulfonamides
17.) An antibiotic-associated severe gastrointestinal problem is referred to as:
a) gastritis
b) fungal infection
c) antibiotic resistance
d) pseudomembranous colitis
a) gastritis
b) fungal infection
c) antibiotic resistance
d) pseudomembranous colitis
18.) From the following list, select the drugs associated with intrinsic tooth staining in children younger than 8 years of age
a) erythromycin
b) minocycline
c) metronidazole
d) doxycycline
e) clindamycin
f) tetracycline
a) erythromycin
b) minocycline
c) metronidazole
d) doxycycline
e) clindamycin
f) tetracycline
Name five potential adverse effects that may result from antibiotic therapy:
a.
b.
c.
d.
e.
Name five potential adverse effects that may result from antibiotic therapy:
a. bacterial resistance
b. GI effects (nausea, vomiting, diarrhea)
c. Allergic reactions
d. Superinfections
e. photosensitivity
A bactericidal antibiotic is one that _______ bacteria whereas a bacteriostatic antibiotic __________ bacteria.
A bactericidal antibiotic is one that kills bacteria whereas a bacteriostatic antibiotic inhibits bacteria.
______________ is an enzyme that breaks down the ___________ ring on penicillin and can be produced by the bacteria ____________________. Amoxicillin is combined with ___________ acid to form the drug ____________ which is resistant to the effects of the enzyme.
Beta-lactamase is an enzyme that breaks down the beta-lactam ring on penicillin and can be produced by the bacteria Staphylococcus aureus. Amoxicillin is combined with clavulanic acid to form the drug Augmentin which is resistant to the effects of the enzyme.
Pseudomembranous colitis is caused by the bacteria ___________________ and is associated with all antibiotics, especially _____________ and can possibly be prevented by taking _____________________ along with the antibiotic.
Pseudomembranous colitis is caused by the bacteria Clostridium difficile and is associated with all antibiotics, especially Clindamycin and can possibly be prevented by taking Lactobacillus acidophilus (a probiotic) along with the antibiotic.
Allergies to penicillin are seen in about ___ % of the population and there is a cross-hypersensitivity between penicillin and ______________.
Allergies to penicillin are seen in about 10% of the population and there is a cross-hypersensitivity between penicillin and cephalosporins.
TRUE or FALSE: Clindamycin (Cleocin) is safe for patients with gastrointestinal issues.
FALSE
Name two precautions/directions with tetracyclines:
a.
b.
Name two precautions/directions with tetracyclines:
a. do not take with milk, dairy products, iron, magnesium-containing products, or antacids
b. wait ≥ 2 hours before/after taking lipid-lowering drugs to take tetracyclines
Who must not be prescribed tetracyclines?
pregnant women
children ≤ 8 yrs
Name two precautions with metronidazole (Flagyl):
a.
b.
Name two precautions with metronidazole (Flagyl):
a. NO alcohol
b. NO anticoagulants (e.g. Warfarin)
List the four antibiotics that treat TB disease:
a.
b.
c.
d.
List the four antibiotics that treat TB disease:
a. Isoniazid (INH)
b. Rifampin (RIF)
c. Pyrazinamide (PZA)
d. Ethambutol (EMB)
What is pyridoxine and why must it be taken with isoniazid?
Pyridoxine is Vitamin B6. It must be taken with isoniazid to prevent a pyridoxine deficiency which can cause peripheral neuropathy.
List four issues that have helped create antibiotic resistance:
a.
b.
c.
d.
List four issues that have helped create antibiotic resistance:
a. delayed tx (diagnosis wasn’t made early enough, inadequate doses of antibiotic were initially given, wrong antibiotic)
b. pt discontinued the drug early
c. pt took leftover antibiotics
d. pt missed doses
What are the potential issues with the drug methotrexate and antibiotics? Why?
Concurrent use of methotrexate and penicillins can lead to a potentially fatal interaction. Penicillin competes with methotrexate in the kidneys for excretion, leading to toxic levels of methotrexate (it has a narrow therapeutic index).
Which antibiotics cause photosensitivity/phototoxicity?
tetracyclines (doxycycline, minocycline, tetracycline)
fluoroquinolones (ciprofloxacin, levofloxacin, ofloxacin)
sulfonamides (sulfamethoxazole-trimethoprim (Bactrim))
Clindamycin is bacteriostatic at _____ mg and _____________ at 300 mg.
Clindamycin is bacteriostatic at 150 mg and bactericidal at 300 mg.
Antiinfective Agents Definitions
Antiinfective Agents: substances that act against or destroy infections; can come from ANY SOURCE (made by a microorganism OR developed in a chemistry laboratory) and can inhibit or kill a VARIETY of organisms such as bacteria, protozoa, and viruses
Antibacterial Agents: substances that destroy or suppress the growth or multiplication of bacteria; can come from any source (made by a microorganism OR developed in a chemistry laboratory); only affects BACTERIA
Antibiotic Agents: chemical substances produced by MICROORGANISMS that have the capacity, in diluted solutions, to destroy or suppress the growth or multiplication of organisms or prevent their action
Bactericidal: the ability to KILL bacteria; IRREVERSIBLE effect
Bacteriostatic: the ability to INHIBIT or RETARD the multiplication or growth of bacteria; REVERSIBLE effect (remove contact with agent → bacteria are still able to grow and multiply)
Antimicrobial Agents: substances that destroy or suppress the growth or multiplication of microorganisms
Antifungal Agents: substances that destroy or suppress the growth or multiplication of fungi
Antiviral Agents: substances that destroy or suppress the growth or multiplication of viruses
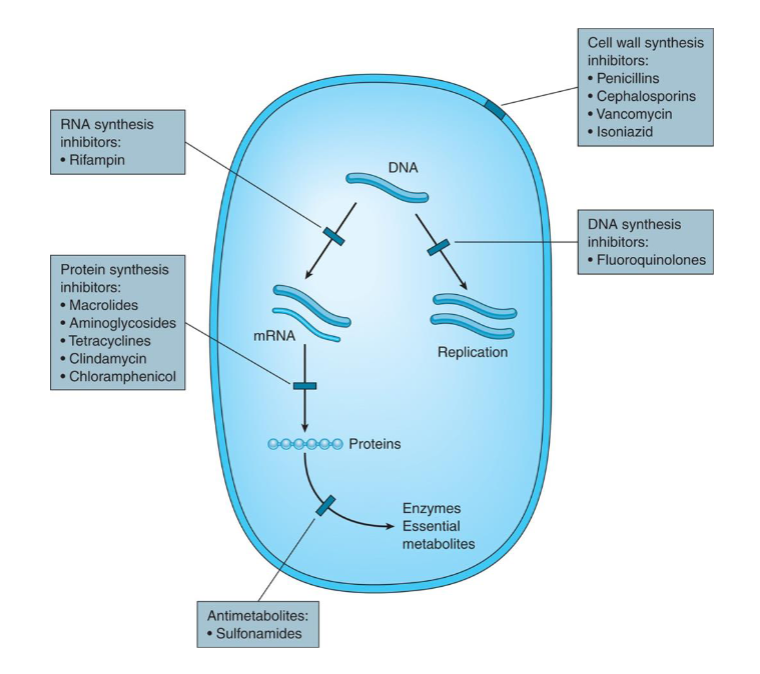
Antibiotics
Antibiotic Agents: chemical substances produced by MICROORGANISMS that have the capacity, in diluted solutions, to destroy or suppress the growth or multiplication of organisms or prevent their action
.
Types:
Bactericidal: the ability to KILL bacteria; IRREVERSIBLE effect
Cell-Wall Synthesis Inhbitors:
Penicillins
Cephalosporins
Vancomycin
Isoniazid (INH)
Bacteriostatic: the ability to INHIBIT or RETARD the multiplication or growth of bacteria; REVERSIBLE effect (remove contact with agent → bacteria are still able to grow and multiply)
DNA synthesis inhibitors
RNA synthesis inhibitors
Protein synthesis inhibitors
Antimetabolites
Spectrum of Activity:
Narrow spectrum
Broad spectrum
Extended spectrum
.
Adverse Effects:
bacterial resistance to the antibiotic: bacteria will continue to multiply, grow, and survive in the presence of concentrations of an antibiotic that are usually lethal to organisms
inherent antibiotic resistance: bacteria are naturally resistant
acquired antibiotic resistance: bacteria have adapted and evolved resistance
Spontaneous Mutation
Genetic Exchange: bacteria share genetic information with each other via transduction, transformation, or bacterial conjugation
Active Efflux: efflux pumps allow microorganisms to regulate their internal environment by pumping toxic substances out of the cell; key mechanism of gram (-) bacteria
Epigenetics: external modifications to DNA that turn genes on/off; affects how the cell reads genes but does not change the DNA sequence itself; means “above” or “on top of” genetics
possible causes:
1. treatment resistance: “doctor-induced resistance” causing a delay in tx bc the diagnosis wasn’t made early enough, inadequate doses were initially given, the wrong antibiotic was given
2. misuse resistance: pt did not take as directed, pt did not take on prescribed schedule, pt missed doses, pt discontinued the drug early, pt took left-over antibiotics
3. overuse/overprescription of antibiotics
Superinfections: the overgrowth of an organism that was not present when the treatment of an infection began; infection imposed upon another infection due to the overgrowth of normal flora (GI tract, oral cavity, respiratory tract, vaginal area) or the eradication of microorganisms that are part of the normal flora, usually associated with prolonged antibiotic use and broad-spectrum antibiotics; can cause overgrowth of candidiasis and can cause stomatitis or glossitis
GI issues: direct/indirect irritation caused by an imbalance in the normal GI flora, resulting in nausea, vomiting, and/or diarrhea; may be avoided by taking probiotics such as Lactobacillus acidophilus (ex: antibiotic-associated pseudomembranous colitis caused by overgrowth of Clostridium difficile)
allergic reactions
photosensitivity: certain antibiotics (and diuretics, retinoids, and BC pills) can make the skin sensitive to the sunlight by interacting with UV light to create toxic or inflammatory reactions in skin cells; symptoms: severe sunburn, blistering, rashes
tetracyclines: doxycycline, minocycline, tetracycline
fluoroquinolones: ciprofloxacin, levofloxacin, ofloxacin
sulfonamides: sulfamethoxazole-trimethoprim (Bactrim)
drug interactions
Indications for Antibiotics
acute odontogenic/orofacial infections
prophylaxis against IE
prophylaxis for pts at risk for infection because of immunocompromise (DM with HbA1C >8, immunosuppressant drugs, transplant pts)
periodontal therapy:
systemic antibiotics are used in conjunction with periodontal debridement and/or surgery (e.g. Grade C periodontitis, NPDs)
topical antimicrobial agents (e.g. Arestin, aka minocycline HCl) used for localized periodontitis
endodontic therapy:
endodontic lesion WITH soft tissue swelling AND systemic involvement (fever, lymphadenopathy, cellulitis) or spread of infection (NOT indicated in an uncomplicated endodontic infection / well-localized soft tissue swelling WITHOUT systemic signs of infection)
prophylaxis for postsurgical infection
peri-implantitis:
infections associated with bone loss and/or suppuration (NOT indicated in peri-implant mucositis → use chlorhexidine gluconate instead)
Antibiotic Families
Bactericidal:
Penicillins
only 2 penicillins used in dentistry: Penicillin VK & Amoxicillin (and Augmentin)
NO METHOTREXATE → toxicity
cell wall synthesis inhibitors (beta-lactam ring)
Cephalosporins
good for bone penetration
10% cross allergenicity with penicillins
cell wall synthesis inhibitors (beta-lactam ring)
Nitroimidazoles: Metronidazole (Flagyl)
Metronidazole + Amoxicillin → useful against Aa and Pg in rapidly-progressing (Grade C)/nonresponding periodontitis, NPDs
found in GCF
NO ALCOHOL, LITHIUM, ANTICOAGULANTS (WARFARIN)
Quinolones (Fluoroquinolones)
off-label use for periodontitis, most common use: chronic bronchitis
.
Bacteriostatic:
Macrolides
Azithromycin (Zithromax): periodontal disease (concentrates in phagocytes for good penetration into tissues)
Erythromycin & Clarithromycin are CYP3A4 INHIBITORS → increased blood levels of certain drugs
Tetracyclines
concentrates higher in GCF than in blood → used for periodontal disease
contraindicated in pregnant women / children ≤ 8 yrs
.
Both Bactericidal & Bacteriostatic:
Lincomycins: Clindamycin
dose dependent: 300mg bactericidal, 150mg bacteriostatic
penetrates well into GCF → off-label use for periodontitis and dental infections
PSEUDOMEMBRANOUS COLITIS
.
NOT Used in Dental Medicine:
Sulfonamides
Vancomycin
Aminoglycosides
Beta-Lacam and Penicillin Resistance
Penicillins & Cephalosporins are potent bactericidal agents that contain a beta-lactam ring. The beta-lactam ring interferes with bacterial cell wall synthesis.
method of action: inhibits one or more of the penicillin-binding proteins (PBPs) (the enzymes involved in the synthesis of the bacterial cell wall and in maintaining its integrity via cross-linkages/transpeptidases) → no cell wall → internal part of bacterial cell is vulnerable to outside environment → lysis (cell rupture) → death
Beta-Lactamase (penicillinase): bacterial enzymes that cleave the beta-lactam ring, rendering penicillin ineffective and causing penicillin resistance
95% of Staphylococcus aureus produce beta-lactamase
Augmentin: Amoxicillin + clavulanic acid → prevents the penicillin beta-lactam ring from being destroyed by the beta-lactamase enzyme
Penicillins
method of action: bactericidal (cell wall synthesis inhibitors via beta-lactam ring)
discovered by Sir Alexander Fleming
administration: oral or parenterally (NEVER topical due to allergic reaction)
spectrum of activity: primarily effective against gram (+) cocci and bacilli bacteria (Streptococcus pneumoniae) and some gram (-) bacteria
Narrow-spectrum: natural penicillins
Penicillin V & Penicillin G
not very effective against gram (-) bacteria because penicillin can’t penetrate their thick lipopolysaccharide coat
Broad-spectrum
Aminopenicillins (amoxicillin and ampicillin) & antipseudomonal penicillins (piperacillin, ticarcillin)
more effective against gram (-) bacteria
Pharmacokinetics:
Absorption: primarily absorbed from duodenum, but depends on acid stability in the stomach; absorption is greatest when taken on an empty stomach (exception: amoxicillin which can be taken with food); all penicillins must be taken with a full glass of water to increase absorption from the GI tract
Penicillin VK: absorbed orally (acid stable)
Piperacillin & Ticarcillin: injected to bypass the stomach (not acid stable)
Elimination: excretion by kidneys (note: dosage must be reduced in those with renal failure)
Indications:
Penicillin VK & Amoxicillin: the only 2 penicillins used in dentistry for mild-mod odontogenic infections
Penicillin VK: mild-mod endodontic, periodontic, and odontogenic infections
Amoxicillin: more serious infections (broad-spectrum); effective against Peptostreptococcus (found in perio sites)
Augmentin (amoxicillin + clavulanic acid): used for resistant strains of bacteria, especially for perio pts that are refractory to tx, NPDs, and some surgeries (especially sinus lifts)
Penicillin Adverse Effects and Drug Interactions
Adverse Effects:
allergic reactions occur in <10% of the population
pseudomembranous colitis
GI upset (most common adverse effect causing nausea, vomiting, diarrhea; oral penicillins may be taken with a probiotic like Lactobacillus acidophilus)
superinfection
Drug Interactions
Penicillin + bacteriostatic antibiotic (i.e. tetracyclines, erythromycins) → space the two antibiotics so they are not given concurrently
Oral contraceptives → may render oral contraceptives ineffective (estrogen undergoes enterohepatic circulation and needs bacteria in the gut to break it down before it reabsorbs; penicillin prevents this causing poor absorption of estrogen and rendering the oral contraceptive ineffective)
Food → increases breakdown of penicillin in the stomach
Probenecid (gout tx) → decreases renal elimination of penicillins
Pregnancy/Nursing (Category B)
Methotrexate → potentially fatal interaction due to toxic levels of methotrexate (low TI); penicillin and methotrexate compete in the kidneys for excretion, leading to a buildup of methotrexate and toxicity
Cephalosporins
method of action: bactericidal (cell wall synthesis inhibitors via beta-lactam ring)
similar beta-lactam ring as penicillins
Indications:
NOT used for dental infections due to high $
skin, bone, genitourinary, and respiratory tract infections; otitis media, acute prostatitis
great for bone penetration
Adverse Effects: similar to penicillins
NOTE: There is a 10% cross-hypersensitivity reaction with peniciliins (aka: 10% of people allergic to penicillin will also be allergic to cephalosporins). → BOARD QUESTION
Nitroimidazoles: Metronidazole (Flagyl)
method of action: bactericidal
spectrum of activity: effective against obligate or strict anaerobes (like subgingival bacteria)
Indications:
Metronidazole + amoxicillin → useful against Aa and Pg in rapidly progressing (grade C) periodontitis, NPDs, and nonresponding periodontitis
found in GCF
Adverse Effects:
GI upset (okay with food)
metallic taste
dry mouth
dark urine
okay in renal disease; dark urine does not indicate any effects on the kidneys
Drug Interactions:
alcohol → disulfiram-like reaction causing headache, nausea, vomiting
NO alcohol, including alcohol mouth rinse!
lithium → causes toxicity
anticoagulants (warfarin) → increased bleeding
okay with antiplatelets
Quinolones (Fluoroquinolones)
method of action: not actually an antibiotic (synthetically produced); antimicrobial
spectrum of activity: broad spectrum antimicrobial effective against facultative gram (-) anaerobes
indications:
CHRONIC BRONCHITIS (majority of dental pts taking quinolones)
allergy to penicillin
periodontitis (off-label)
bacterial sinusitis, acute bacterial chronic bronchitis, pneumonia, skin infections, bacterial conjunctivitis (eye drops), UTIs
adverse effects:
phototoxicity, dizziness, convulsions, headaches, hallucinations, joint/cartilage damage (esp. Achillies’s tendon!)
Ciprofloxacin should NOT be given to children
drug interactions:
Warfarin
theophylline (antiasthma med)
caffeine
dairy products (Ca), sodium bicarbonate (NO AIR POLISHING), iron, antacids (Mg, Al) → reactive metals with strong binding affinity cause delayed absorption of quinolones
*take these products 4 hours before/2 hours after taking quinolones
ex: Ciprofloxacin, Levaquin
Macrolides
mechanism of action: bacteriostatic — inhibits protein synthesis within bacterial cell (prevents multiplication)
spectrum of activity:
Erythromycin: gram (+) bacteria and some gram (-) strains; NOT used for perio/endo infections bc it cannot penetrate gram (-) cell walls
pharmacokinetics:
absorbed primarily in duodenum
widely distributed to most body tissues (except the brain)
concentrates and metabolizes partly in the liver
primarily excreted unchanged via bile
indications:
Azithromycin (Zithromax): periodontal disease (concentrates in phagocytes such as PMNs and macrophages which contributes to their distribution into inflamed periodontal tissues in greater amounts than in plasma); good penetration into tissues
upper and lower respiratory tract infections, pharyngitis, tonsilitis, community-acquired pneumonia, gonorrhea, skin infections, otitis media, acute pelvic inflammatory disease Legionnaires’ disease, chlamydia
adverse effects:
Hepatic dysfunction (usually with erythromycin estolate)
GI disturbances
drug interactions:
theophylline, carbamazepine, cyclosporine, phenytoin, lovastatin, and simvastatin are metabolized by CYP3A4 enzymes → drugs will not metabolize → increased blood levels (erythromycin & clarithromycin (but NOT azithromycin) are CYP3A4 liver enzyme INHIBITORS)
concurrent use of bactericidal + bacteriostatic antibiotics (space them apart!)
ex:
Erythromycin (E-mycin): resistance is generally not a problem in short-term therapy
Second gen of erythromycins: Azilides (broader spectrum with fewer adverse effects/less G disturbance)
Azithromycin (Zithromax), Clarithromycin (Biaxin)
Lincomycins: Clindamycin
mechanism of action: inhibits protein synthesis; DOSE DEPENDENT
bacteriostatic: 150mg
bactericidal: 300mg
spectrum of activity: effective against most gram (+) organisms; gram (-) anaerobes are resistant to it
indications:
acute bacterial exacerbation of chronic bronchitis, acute bacterial sinusitis, community-acquired pneumonia
dental infections, periodontitis (off-label)
penetrates well into GCF
adverse effects:
PSEUDOMEMBRANOUS COLITIS (clindamycin is notorious for this) → do NOT give to pts with GI issues, Crohn’s disease, ulcerative colitis, pseudomembranous enterocolitis
visual disturbances
liver dysfunction
pregnancy category: B
Tetracyclines
mechanism of action:
spectrum of activity:
indications:
periodontal disease (adjunctive therapy, rapidly progressing)
concentrates higher in GCF than in blood
adverse effects:
contraindications:
pregnancy or lactation (Pregnancy category: D): affects skeletal growth of fetus and child; permanent tooth discoloration during tooth development in last half of pregnancy
children ≤ 8 yrs
risk of superinfections due to candida (take with a probiotic)
photosensitivity
drug interactions:
do NOT take with dairy products, iron, Mg-containing products, antacids (doxycycline & minocycline are okay with dairy)
wait ≥ 2 hrs before/after taking with lipid-lowering drugs (i.e. colestipol/Colestid, cholestyramine/Questran)
oral contraceptives
concurrent use of bactericidal + bacteriostatic antibiotics (space them apart!)
ex: Tetracycline HCl
Semisynthetic analogues: Doxycycline hyclate & Minocycline HCl
NOT used in Dental Medicine:
Sulfonamides
Vancomycin
Aminoglycosides
Sulfonamides: synthetic analogue of para-aminobenzoic acid (PABA)
mechanism of action: inhibits synthesis of folic acid from PABA in bacteria
indications: HIV/AIDS pts for Pneumocystis carinii pneumonia (PCP)
Vancomycin
spectrum of activity: gram (+) bacteria (i.e. Clostridium difficile)
Aminoglycosides:
indications: serious systemic infections, burns
Topical Antibacterial Agents
use: LOCAL delivery of antimicrobial agents by topical application or by controlled-release devices
routes of administration:
supragingival: mouth rinse, dentifrice, oral irrigator
subgingival: oral irrigation, controlled-release devices
Arestin (Minocycline HCl → an antibiotic)
Periochip (an antimicrobial)
Oral Rinses
substantivity: ability of the drug to absorb or bind to intraoral surfaces with subsequent release of the drug in its active form
drug interactions:
alcohol-containing mouth rinses (Peridex, PerioGuard, Listerine)
metronidazole (Flagyl) → disulfiram-effect
Chlorhexidine Gluconate (CHX)
mechanism of action: antimicrobial with HIGH SUBSTANTIVITY (12 hrs); disrupts oral microbiome to reduce biofilm formation
indications:
antiseptic cream for wounds, preoperative skin cleanser, surgical scrub
gingivitis and implant mucositis
adverse effects:
faster accumulation of supragingival calc
staining of teeth (disrupts oral microbiome to reduce biofilm formation, but the acquired pellicle still forms which can stain)
use for ≤ 2 wks!!
increases acidity of oral microbiome
can increase BP (CHX affects nitrate-reducing bacteria → the oral nitrate oxide pathway plays a key role in maintaining nitric oxide (NO) homeostasis which affects blood pressure regulation)
Drug Interactions:
positive charge of CHX causes it to bind to negatively-charged molecules in toothpastes (e.g. Fl, SLS) and inactivates CHX → rinse 30 mins before/after toothbrushing
birth control
ex:
0.12% concentration of CHX with 11.6% alcohol: Peridex, PerioGuard
alcohol-free: GUM, Butler
Tuberculosis
Tuberculosis: Mycobacterium tuberculosis attacks the lungs (75%), kidneys, spine, and brain; one of the top 10 causes of death and the leading cause of death from a single infectious agent (above HIV/AIDS) with 1/3 of the world’s population being infected
Spread: coughing, sneezing, speaking (NOT shaking hands, sharing food/drink, kissing, touching objects)
Testing
PPD (Purified Protein Derivative) Two-Step Mantoux Tuberculin Skin Test: 0.1mL tuberculin PPD injected into inner surface of forearm; must be read within 48-72 hrs
no reaction = no infection
reaction (induration) = infection (latent or active)
the immune system of a person who was infected years prior may not react and give a false negative (2nd PPD will prompt a boosted reaction)
IGRAs (Interferon-Gamma Release Assays): one-visit blood test; results read within24-48 hrs; used if a false positive from a BCG vaccination is suspected
BCG (Bacille Calmette-Guerin) Vaccine: no longer routinely used; at best provides 80% protection for 15 years; can cause false-positive PPDs
LTBI (Latent TB Infection): person is infected but NOT infectious (immune system is keeping the infection latent, but TB can multiply and become active again)
NO symptoms, (+) PPD, (-) chest x-ray, (-) sputum smear
Diagnosis:
cough lasting ≥ 3 wks; hemoptysis, pain in chest, fatigue, weight loss, no appetite, fever, chills, night sweats
(+) PPD, (+) chest x-ray, (+) sputum smear
if (+) chest x-ray → take sputum smear to detect acid-fast bacilli and sputum culture for sensitivity testing
Treatment:
IMMEDIATE isolation and tx
DOT (Directly Observed Therapy): pts who are community health risks are institutionalized
≥ 2 weeks of multi-drug therapy, 3x (-) sputum smears → continue for 2 months on four-drug regimen → then 4 months on isoniazid (INH) and rifampin (RIF)
≥ 2 weeks of multi-drug therapy includes:
Isoniazid (INH) with Pyroxidine (Vit B6)
Rifampin (RIF)
Pyrazinamide (PZA)
Ethambutol (EMB)
sputum cultures help determine resistant strains of TB
TB with HIV: treated with the same drugs as those without HIV/AIDS, but hold a higher risk for resistant TB; often treated with higher doses of INH and RIF to prevent relapse with RIF-resistant organisms; tx can be longer
TB with children: higher risk of disseminated disease (spreads to different parts of the body), so prompt tx is needed; rare for young children to spread TB; lower risk of drug resistance so tx starts with INH, PZA, RIF; EMB not routinely given to children < 13yrs due to risk of decreased visual acuity and temporary loss of vision
TB Drug Therapy
Isoniazid (INH):
bactericidal ONLY AGAINST ACTIVELY-GROWING TB
hepatotoxic: abdominal pain and jaundice (increased risk with alcohol & acetaminophen)
GI problems, peripheral neuropathy, anemia
must be taken with Pyroxidine (Vit B6) to prevent peripheral neuropathy
med consult needed to determine liver enzyme levels prior to administering local anesthesia
Rifampin (RIF):
hepatotoxic (not as dramatic as INH)
GI disturbances, nephritis
orange bodily excretions and secretions
Pyrazinamide (PZA):
hepatotoxic, rash, hyperuricemia, GI disturbances
Ethambutol (EMB):
optic neuritis, rash, GI disturbances, malaise