1/2- gas exchange + transport/hemoglobin
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
definition of gas exchange
movement of gas between environment + blood, involving:
transport between atmosphere + alveolus (breathing)
diffusion across alveolar/capillary membranes → blood
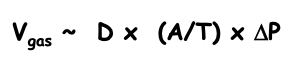
how does Fick’s Law relate to diffusion of gases across air/blood barrier
rate of gas transfer is:
directly proportional to the surface area (A), pressure gradient (ΔP), diffusion coefficient (D)
inversely proportional to membrane thickness (T)
what’s Henry’s Law
a gas will dissolve in a liquid in proportion to the gas’s partial pressure over the liquid
how is Henry’s Law related to breathing
describes solubility of O2 + CO2 in plasma, CO2 is 20x more soluble than O2 + more rapidly even though its MW is higher
what is gas exchange in the alveoli driven by
partial pressure gradients: O2 is driven into deoxygenated blood, CO2 driven out
how do you calculate alveolar PO2
alveolar gas equation: PAO2 = PIO2 - (PaCO2/0.8)
PIO2 = partial pressure of O2 in inspired air (160 mmHg)
PaCO2 = arterial PCO2
0.8 = respiratory exchange ratio
what’s A-aDO2
difference between alveolar gas + mixed arterial blood even after complete equilibration, due to small amount of blood bypassing alveoli + not becoming oxygenated → combining w/ oxygenated blood, diluting the O2
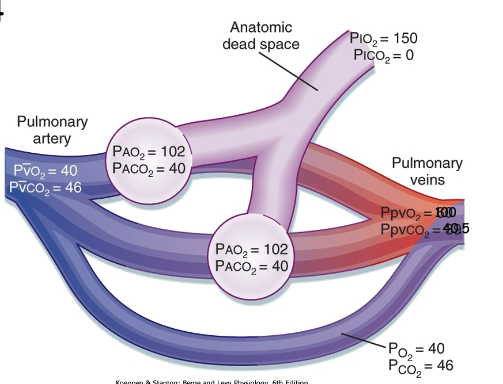
what’s normal A-aDO2
~4 mmHg, under 30 years old
how does A-aDO2 change w/ age
increases w/ age + lung compliance
abnormally high A-aDO2 indicates what
pathological problem in which gas exchange is compromised
since O2 is very poorly soluble in blood, how does it stay in the blood
via hemoglobin
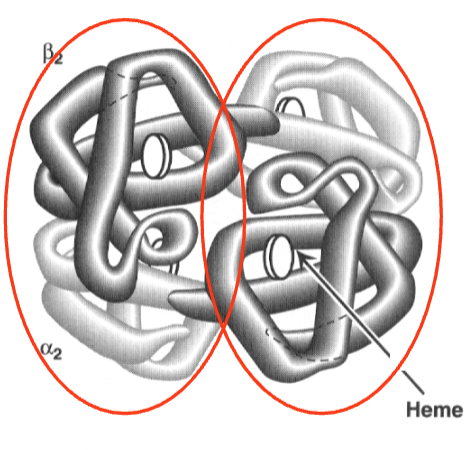
describe the structure of hemoglobin + how it carries O2
has 4 polypeptide chains, each chain has 1 heme group carrying 1 O2 molecule → 1 Hb carries 4 O2
T/F: once O2 binds to Hb, O2 no longer acts as a gas + does not contribute to the pressure
true, Hb lowers PO2 allowing more O2 to go into the blood following the partial pressure gradient
T/F: once O2 binds to Hb, Hb has a higher affinity to O2
true
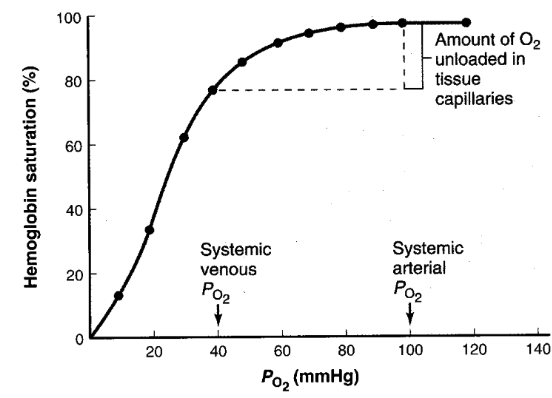
when oxygen is carried away into the tissues, how many of the O2 are taken from the Hb
only 1 out of 4, therefore Hb returns to the lungs already 75% saturated + picks up 1 O2 in the alveoli
the 3 remaining O2 on Hb after becoming “deoxygenated” represent what
reserve capacity
T/F: dissolved oxygen represents only ~1.5% of the total content in arterial blood, the other 98.5% being bound to Hb
true
what’s the purpose of the small amount of dissolved oxygen in arterial blood
maintains the PO2 necessary to keep the Hb saturated + only free O2 can diffuse across cell membranes
what 4 factors affect Hb binding to O2
temperature
pH
PCO2
2,3-diphosphoglycerate
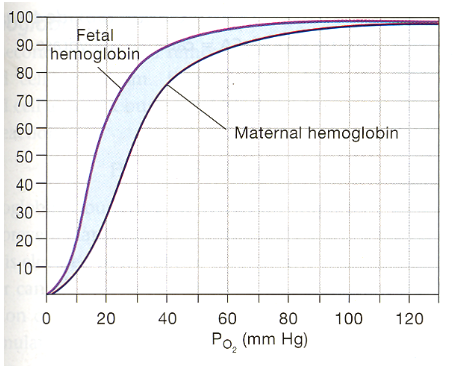
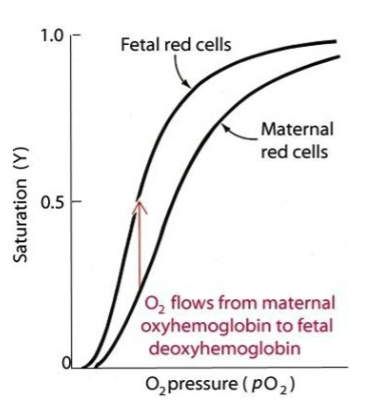
which has a higher affinity for O2: fetal Hb or adult Hb
fetal Hb
what’s methemoglobin
normal Hb’s Fe2+ is oxidized → Fe3+ by drugs/chemicals → methemoglobin, which cannot bind O2
how can methemoglobin return to being Hb
RBCs have an enzyme Met-Hb reductase that reduces Met-Hb → Hb
3 forms of CO2 transport
dissolving in blood (~6%)
conversion into bicarbonate via carbonic anhydrase in RBCs (~70%)
conversion into carbamino compounds by reacting w/ free amines on proteins (~24%)
what role does Hb have in CO2 transport
acts a buffer: Hb binds w/ the H+ produced from bicarbonate + carbamino compound rxns
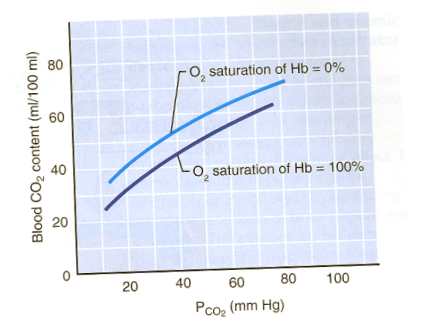
T/F: Hb saturated w/ O2 doesn’t bind as well to CO2 , compared to Hb not saturated w/ O2
true, increasing PO2 facilitates release of CO2 from Hb, while decreasing PO2 allows Hb to take up more CO2 + H+ (Haldane effect)
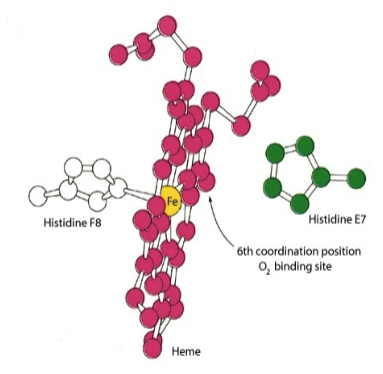
what’s myoglobin
protein in muscle that contains:
heme: a prosthetic group
proximal histidine: chelates iron directly
distal histidine: enables oxygen binding
meat turning brown is because of what
Fe2+ in myoglobin → Fe3+
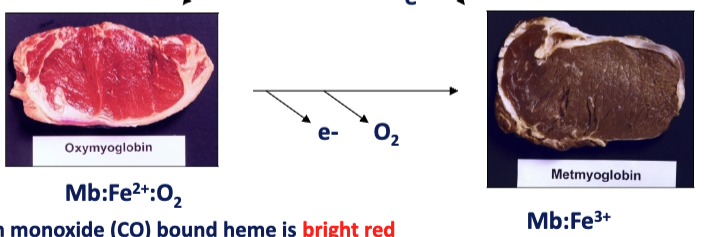
what keeps heme in its Fe2+ state
O2 + CO
3 important functions of myoglobin
increases solubility of O2
facilitates O2 diffusion
stores O2
distinguish the subunits within Hb
Hb has 2 alpha + 2 beta subunits, alpha subunits in contact w/ beta subunits
T/F: once Hb/Mb binds to O2, structure of Hb/Mb changes slightly
true
T/F: if Hb behaved like Mb, very little O2 would be released in the capillaries
true
Hb exists in which 2 forms
T-state: taut, not bonded to O2
R-state: relaxed, bonded to O2
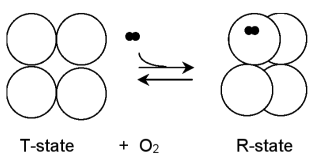
which Hb form is more stable
T-form, than R-form w/o O2
R-form has increasing affinity for O2 when
as it gains more O2 molecules
describe what happens to the structure of Hb when it binds to O2
Fe2+ ion moves → subtle conformational change in 1 subunit, which is in close contact w/ another subunit → causing other subunits to move
T/F: in addition to picking up O2, Hb also unloads CO2 from the blood → alveolus
true
what’s the Bohr effect
H+ is a negative allosteric effector: H+ causes Hb to drop O2 aka lower pH causes Hb to drop O2, lowering its affinity to bind O2
CO2 is a negative allosteric effector: CO2 binds to Hb, lowering its affinity to bind O2

describe the subunits of fetal Hb (HbF)
2 alpha subunits + 2 gamma subunits
what’s the main difference between HbA + HbF
HbF has the ability to bind to BPG, an allosteric effector of Hb → allowing HbF to have a higher O2 binding affinity
what happens if BPG binds to HbA
lowers its O2 binding affinity → allows you to adapt to high altitudes by delivering O2 despite lower O2 in the lungs
3 types of hemoglobinopathies
sickle cell
methemoglobin
thalassemias
sickle cell disease affects which subunit of Hb
glutamate mutates to valine on the exterior of beta subunit → making Hb insoluble (HbS)
T/F: Hb is normal in sickle-cell pts as long as it’s oxygenated
true
once deoxygenated, what happens to Hb in sickle cell pts
formation of deoxy-HbS-polymer → distorting the RBC shape
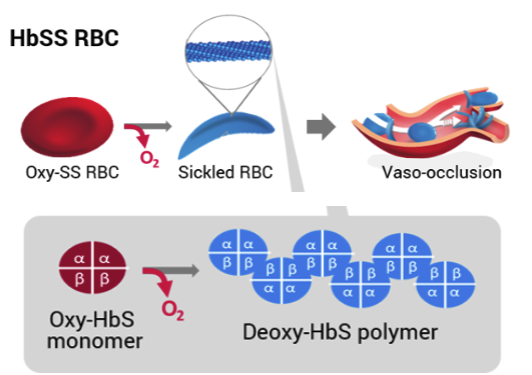
4 treatments of sickle cell
antibiotics
hydroxyurea: stimulates HbF production
bone marrow transplant
gene therapy
what are thalassemias
no mutation in Hb, but imbalance between the alpha + beta subunits
2 types of thalassemia
alpha: lack of alpha chain, too much beta
beta: lack of beta chain, too much alpha
alpha thalassemia predominates where vs. beta thalassemia
alpha: Asian + African populations
beta: Mediterranean populations
how is thalassemia treated
blood transfusion