bio topic 6
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
what is neutralisation
bind to bacterial toxins, making them neutral
what is opsonisation
makes the pathogens more recognisable to phagocytes
what is agglutination
antibodies bind to antigen causing them to clump togther and slow the movement
How do you produce an aseptic culture?
Provide organisms with appropriate nutrients
Use a sterile medium
Use an inoculating loop to transfer pathogen
Prevent contamination from air (convection current)
Pass bottle through flame, only open lids partway
Why must aseptic techniques be used?
To prevent potentially harmful microorganisms escaping from culture to air
To prevent microorganisms from the air contaminating the culture
What are the different types of culture media?
Liquid (broth)
Solid (grows cultures with discrete colonies)
Non-selective (allows broad range of microorganisms to grow)
Selective (allows only a narrow range of microorganisms to grow)
How do you isolate a singular microorganism from a culture?
streak plating
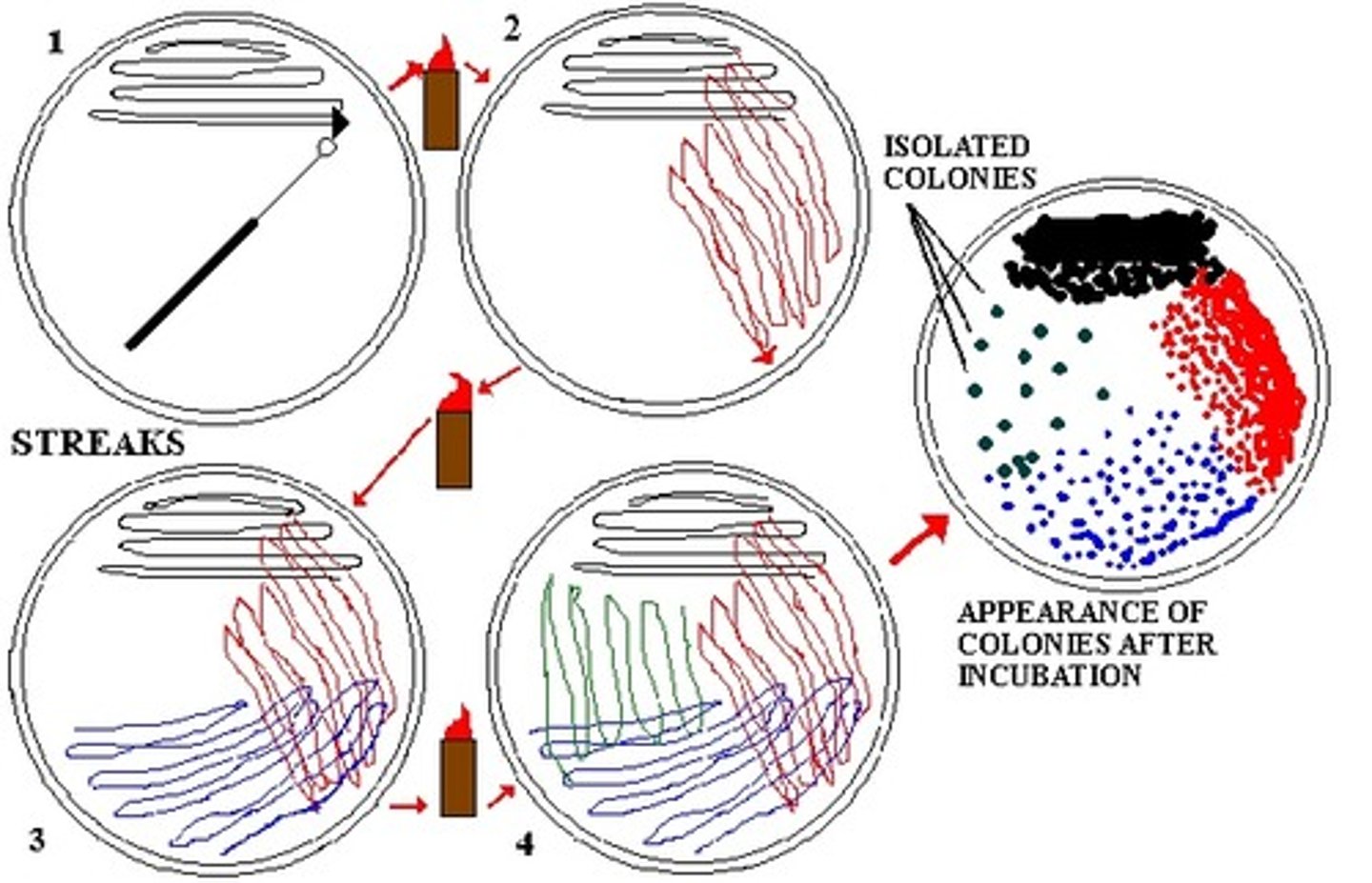
What are the steps of streak plating?
1. Flame inoculating loop
2. Dip loop in culture
3. Make three streaks on sterile plate
4. Turn the plate 90 degrees and streak again, overlapping last streaks
5. Turn and streak again
6. use isolated colonies to prepare a second plate
How do you make a serial dilution?
1. Start with 10cm^3 of undiluted culture
2. Add 1cm^3 of first tube into 9 cm^3 of sterile saline
3. Continue to add 1cm^3 from previous tubes to form serial dilutions
Why is an appropriate dilution a compromise when diluting a culture?
Must have a low enough number of microorganisms to count and a high enough number to provide a reliable sample of the culture
What are the two types of cell count?
Total count: All cells in the culture, dead or alive
Viable count: Only the living cells in the culture
What is the lag phase of bacterial growth?
First phase after inoculation when microorganisms are adjusting to their environment so the population is only increasing very slowly
What is the log phase of bacterial growth?
exponential growth
What is the stationary phase of bacterial growth?
population reaches maximum due to limiting nutrients and a build up of toxic substances
What is the death phase of bacterial growth?
A lack of nutrients and increase of toxic products cause death of microorganism
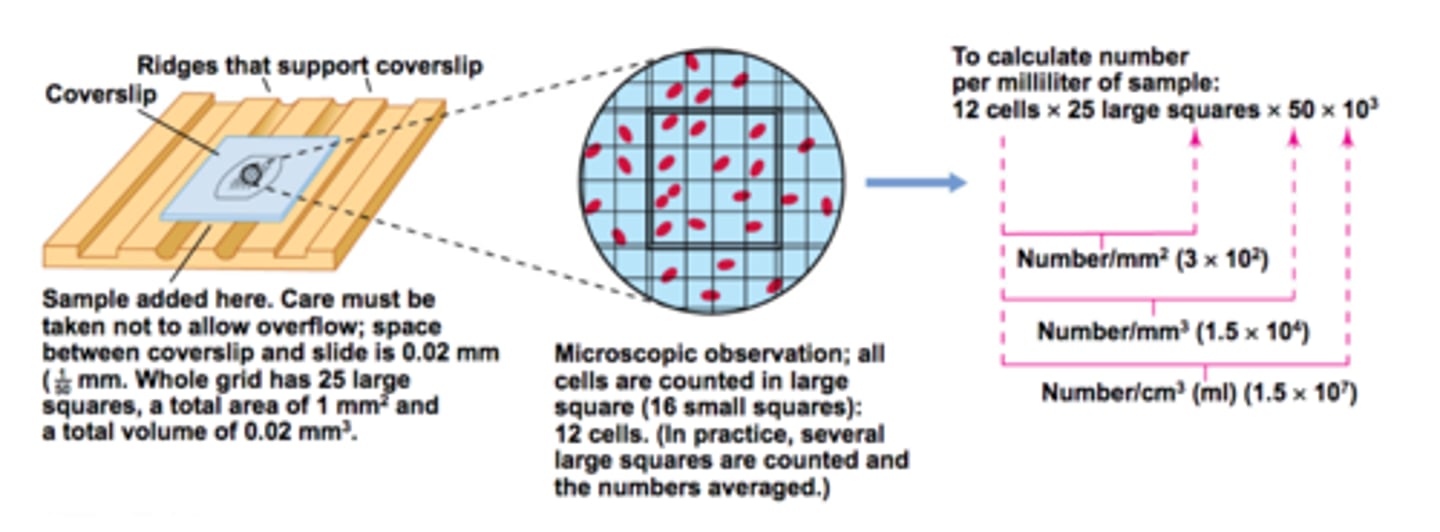
How is a direct cell count calculated?
A haemocytometer (a glass slide with a grid etched on) is placed on a slide which has been dyed with trypan blue which stains dead cells blue
Bacteria cells=number counter x10^4 per cm^3
Only counts viable cells
How is an indirect cell count used to measure dry mass of cells?
1. Filter a sample of known dilution through a pore
2. Remove water by evaporation
3. subtract final mass from initial mass (including filter paper) to calculate mass of dry microorganisms
How is an indirect cell count used to measure turbidity of a diluted culture?
The cloudiness of a sample can be calculated using a simple colorimeter to measure absorbance or transmission.
Use a haemocytometer to produce a calibration curve that relates to absorbance or transmission to the the actual number of cells.
What are the benefits and drawbacks of using serial dilutions to calculate cell count?
Benefits: cheap and simple
Drawbacks: Only counts viable cells; very slow due to incubation period and serial dilutions
What are the drawbacks of measuring turbidity?
Have to use a direct method to calculate cell count from calibration curve
Expensive
Assumes cell density is equal across culture
What is an endotoxin?
a lipopolysaccharide, associated with some Gram-negative bacteria
What is an exotoxin?
A soluble protein produced and released by bacteria as they metabolise and reproduce
Found in both Gram-negative and Gram-positive bacteria
How do pathogens harm the host?
Invade and destroy host tissues
Produce toxins
How does Mycobacterium tuberculosis attack a cell?
By host tissue invasion
Lies dormant in tubercles and not destroyed by immune system (tubercles coated in thick waxy coat)
What is host tissue invasion?
When bacteria invades and damages cells
How does Salmonella attack a cell?
By endotoxins
How does Staphylococcus attack a cell?
By exotoxins (gram positive)
Can only cause disease if they get inside tissue; if the flora changes; or if the immune system is compromised
What are bactericidal antibiotics?
Antibiotics that kill bacteria by destroying cell walls causing bacteria to burst
Especially effective against Gram-positive as cell wall is so thick
(e.g. penicillin)
What are bacteriostatic antibiotics?
Antibiotics that inhibit the growth of bacteria by stopping protein synthesis and production of nucleic acids so bacteria cannot replicate
Especially effective against Gram-negative as lipid bilayer is damaged
(e.g. tetracycline)
What is primary resistance?
When the formation of the bacteria causes it to be unaffected by an antibiotic (e.g. Gram-negative bacteria is resistant to penicillin as they only have thin cell walls)
What is secondary resistance?
When bacteria that were once susceptible to antibiotics develop resistance
What causes antibiotic resistance to develop?
Natural Selection: a mutation will create an allele of a gene which changes the effect of the antibiotic. Antibiotic resistance will be passed on to offspring increasing its frequency
Why is HIV hard to treat?
It has a constantly changing protein coat that means it is not recognised by the immune system
How is MRSA prevented?
New patients screened, isolated and treated
Antibiotics only used if needed
Antibiotic courses completed
Strict hygiene regimes
How is the spread of antibiotic resistance controlled?
Isolating infected people
Hand washing and antibacterial gel
Gloves and aprons
Restricting use of antibiotics
Completing courses of antibiotics
Developing new antibiotics
How is influenza transmitted?
via droplets generated when infected persons cough or sneeze; animal waste; infected surfaces
What is the mode of infection of influenza?
1. Ciliated epithelial cells are infected
2. Cell enters lytic pathway
3. viral particles are released
4. Virus taken into cells lining bronchi and bronchioles by endocytosis
What are the pathogenic effects of influenza?
Lysis of cells and release of toxins cause coughing, headache, vomiting and other symptoms
How is Stem Rust Fungus Transmitted?
Airborne spores of fungus
What is the the mode of infection of Stem Rust Fungus?
1. Spore germinates in water
2. Produces hyphae which enters host by stomata
3. Fungus grows into mycelium
4. Fungus surrounds all tissues in the plant
What is the pathogenic effect of Stem Rust Fungus?
Enzymes are produced to digest the plant and absorb its nutrients which causes stem to be shortened and weakened
How is malaria transmitted?
Parasite enters the body in the saliva of a female mosquito when it bites
What is the mode of infection of Malaria?
1. Parasite transmitted via mosquito
2. Parasite travels to liver
3. Parasite infects red blood cells
4. Parasite reproduces asexually inside red blood cells and causes lysis
What is the pathogenic effect of Malaria?
Lysis of red blood cells causes sweating, shaking, anaemia and liver damage
How can malaria be prevented?
Mosquito nets, insect repellent, pesticides, proper disposal of sewage, drain wetlands where mosquitoes breed, vaccination
What are the issues with malaria prevention
Not possible to drain wetlands that people use
Insecticides could have unexpected effects to food chains
Expensive to develop vaccines
What is an antigen?
A macromolecule that cause an immune response by lymphocytes.
What are physical barriers to infection?
Skin
Stomach acid (kills bacteria)
Gut and skin flora (natural bacteria flora competes with pathogens for food and space)
What is phagocytosis?
When white blood cells engulf foreign cells and digest them
What does a neutrophil do?
Ingests bacteria cells, kills it then digests it
What do macrophages do?
Ingest not only foreign cells but also body cells that are dead or dying
Display antigen of digested bacteria on surface membranes
Releases cytokines to stimulate other immune responses
What is an Antigen-presenting cell?
A cell that isolates the antigen from a pathogen and places it on its surface membrane so that it can be recognised by other cells in the immune system
What are cytokines?
Protein signalling molecules produced by certain cells such as T-helper cells which regulate the immune response by binding to cellular receptors.
What happens when a lymphocyte binds to an antigen on an antigen presenting cell?
The lymphocyte becomes sensitised and divides repeatedly to produce a clone of cells
Most become activated lymphocytes
What is clonal selection?
The repeated mitotic divisions of a sensitised lymphocyte to produce a large number of genetically identical cells
What are B effector cells?
divide to form plasma cell clones
What are plasma cells?
produce antibodies
What are B memory cells?
rovide immunological memory, allows rapid response
What are T killler cells?
produce chemicals that destroy infected body cells
What are T memory cells?
long lived cells that make up part of the immunological memory, when they meet a pathogen for the second time they divide rapidly
What are T helper cells?
activate plasma cells to produce antibodies, secrete opsonin to label pathogens
describe the cell-mediated immune response?
1. A pathogen invades a host cell, pathogen is digested and antigens joined with MHC, host cell becomes APC
2. A T killer cell binds to a surface receptor complementary to the antigen being presented and becomes activated
3. cytokines from humoral response stimulate T killer cells to divide to form T killer and memory cells
4. T killer cells destroy infected cells by binding to the APCs, releasing toxins that causes pores in the cell membrane = lysis
describe the humoral immune response?
1. A pathogen is engulfed by a macrophage, joins antigens with MHC; the cell becomes an APC
2. T helper cell CD4 receptor binds to APC which becomes activated causing it to produces cytokines
3. B cells also bind to the antigens on the APC and becomes sensitised
4. The cytokines stimulate the B cells to divide and form B memory cells and B effector cells
5. B effector cells become plasma cells which produce antibodies specific to the pathogen
What is active immunity?
Natural: natural contact with antigen through clinical infection (e.g. recovery from chickenpox)
Artificial: Immunisation with antigen (e.g. vaccination with live or killed vaccines)
What is passive immunity?
Natural: Transfer of maternal antibodies across the placenta or in breast milk
Artificial: Injection of antibodies
What is a secondary immune response?
response to pathogen carrying antigen to which there are memory cells already present in the host's body
What is herd immunity?
Enough people are vaccinated to make transmission of a disease unlikely
What are some non-specific responses to infection?
Inflammation: Histamines released by damaged white blood vessels and cause vasodilation to increase speed of delivery of antibodies
Fever: Hypothalamus increases body temperature to decrease speed of pathogen reproduction
Lysozyme action: Lysozyme (enzyme) kills bacterial cells by damaging the cell wall