Necrosis
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
What is necrosis?
Necrosis is the local death of tissues within a living individual, resulting from irreversible cell damage.
What factors determine the significance of necrosis?
Where? The location of the necrotic tissue.
How much? The extent of the tissue affected.
How fast? The speed at which necrosis develops.
What happens locally during necrosis?
Irritation causing inflammation
Accumulation of white blood cells (WBCs):
Initially, neutrophils
Later, macrophages
What are the systemic reactions to necrosis?
Release of enzymes from dead cells
Clinical pathology: Measuring enzymes in the blood can indicate organ damage.
Increased serum enzyme levels:
Liver cell destruction → Release of alanine transaminase (ALT)
Muscle damage → Release of creatine kinase (CK)
Acute phase response (general systemic response to tissue injury).
What happens to the cytoplasm in necrosis?
Eosinophilia: The cytoplasm becomes more pink (eosinophilic) due to the detachment of ribosomes. This results in a loss of ribosomal RNA.
Swollen and granular: The cytoplasm appears swollen and may have a granular texture.
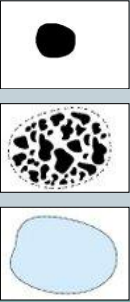
What happens to the nucleus in necrosis?
A. Pyknosis: The nucleus becomes small and dark, indicating chromatin condensation.
B. Karyorrhexis: The nucleus fragments into smaller pieces.
C. Karyolysis: The nucleus fades or dissolves as chromatin is broken down.
Why bother classifying necrosis?
Suggest possible causes of tissue damage
Narrow down differential diagnoses
What should be noted about necrosis as a process?
Necrosis is a dynamic process
Peracute lesions may show no change—the cell dies before any morphological changes are visible (e.g., acute toxicity).
What are the main types of necrosis?
Coagulative
Caseous
Liquefactive
Fat
What tissue is exposed to liquefactive necrosis?
Liquefactive necrosis typically affects tissues with a high fat content, like the brain and central nervous system, due to the action of enzymes that liquefy the tissue.
What is coagulative necrosis?
Cell/tissue architecture remains intact
Delayed/inactivated enzymes
Commonly caused by anoxia (ischemia), such as in renal infarcts or myocardial infarcts, and certain chemicals.
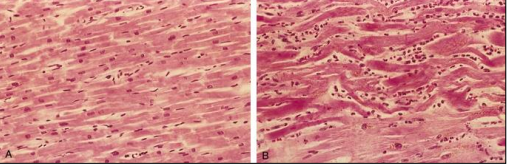
Which is normal cardiac tissue?
A. Left- Normal cardiac tissue with reduced nuclei and striations
B. Right- Necrotic cardiac myocytes

Whats the name of this condition?
Renal infarct
Red
Early stage with haemorrhage
Patients can experience abdominal or flank pain, nausea, vomiting, fever or hypertension

What condition is this?
Renal infarct
White
Loss haemoglobin and start fibrosis which leads to shrinkage.
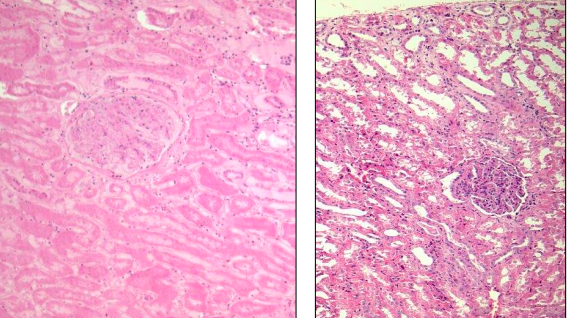
Which is considered a normal glomerulus?
Left
What are the characteristics of caseous necrosis?
Loss of cellular and architectural detail.
Cheesy appearance.
Caused by certain bacteria, such as Mycobacteria and Corynebacterium pseudotuberculosis.
What happens in liquefactive necrosis?
Formation of a liquid mass of necrotic tissue.
Associated with pyogenic bacteria that form pus.
In the central nervous system (CNS), it is referred to as malacia (softening).
What are the key features of fat necrosis?
Saponification, a process where fatty tissue is broken down and turns into soap-like substances.
Caused by:
Fescue toxicity in cattle
Pancreatitis in dogs
Vitamin E deficiency in cats
Strangulated lipomas in horses
What are the potential outcomes of necrosis?
Liquefaction: formation of pus or abscesses.
Sequestration: encapsulation of necrotic tissue.
Regeneration: replacement of damaged tissue with the same type of cells.
Repair: scarring.
What happens during liquefaction of necrotic tissue?
Small areas of tissue turn into fluid with enzymes and neutrophils.
Large amounts of fluid and enzymes are released.
Particles are removed by the bloodstream or lymphatics.
What is suppuration and what causes it?
Suppuration involves the formation of pus, which is made up of necrotic debris, neutrophils, and tissue fluid.
Caused by pyogenic bacteria.
An abscess occurs when pus is confined within a tissue.
What is sequestration in necrosis?
Sequestration is the encapsulation of necrotic tissue that has not liquefied.
Seen in coagulative or caseous necrosis.
The necrotic tissue, called a sequestrum, is surrounded by a fibrous capsule.
Example: Bone necrosis.
What occurs during the repair process in necrosis?
Repair (organisation) involves the presence of:
White blood cells
Capillaries
Fibroblasts
It leads to scarring.
What is regeneration in necrosis?
Regeneration occurs when dead cells are replaced by new cells of the same type.
Requires:
Cells in the affected tissue that can multiply (e.g., labile, stable, or permanent cells).
Some cells surviving the initial damage.
Intact extracellular microarchitecture.
Best example: Liver regeneration.
What defines gangrene?
Gangrene is necrosis combined with putrefaction.
Putrefaction is the breakdown of tissue by bacteria, with dead tissue becoming accessible to bacteria and the normal defense mechanisms inactive.
What are the types of gangrene?
Moist gangrene: Affects tissues with large amounts of blood and fluid.
Dry gangrene: Typically affects tissues without much fluid.
Gas gangrene: Caused by gas-forming bacteria (e.g., Clostridium), which are anaerobic and produce exotoxins.
What does gangrene look like?
Dark/greenish color due to:
Poorly oxygenated blood
Breakdown of red blood cells (RBCs) and pigments.
Formation of iron sulfide from hydrogen sulfide and RBC iron.
Foul odor from the breakdown of tissue.
Cold, unresponsive tissue that doesn’t bleed.
Often is a line of demarcation between necrotic and healthy tissue.
What are the sequelae of gangrene?
Tissues may fall off, commonly in the tips or extremities.
If untreated or severe, gangrene can lead to death.
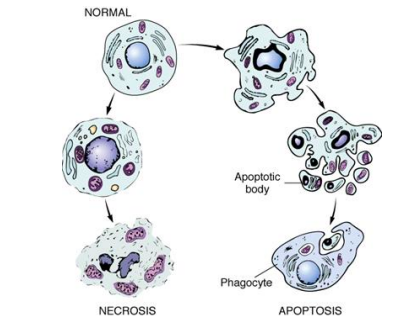
What is apoptosis?
Apoptosis is programmed cell death or "cell suicide".
It plays a crucial role in:
Tissue remodeling (e.g., embryonic development, metamorphosis, and regression).
Some anti-cancer drugs target this process.
Apoptosis does not involve inflammation.
How is apoptosis executed?
Apoptosis is primarily executed by caspases.
Caspases are activated through extrinsic and intrinsic pathways.
What initiates apoptosis?
TNF (Tumor Necrosis Factor)
Fas ligand
Deprivation of growth factors
DNA damage
Immune stimulation
What occurs in the extrinsic pathway of apoptosis?
Death receptor TNFR1 and Fas are crosslinked.
Death domain activation triggers caspase activation.
Caspase 8 is activated.
What occurs in the intrinsic (mitochondrial) pathway of apoptosis?
Increased mitochondrial permeability releases pro-apoptotic molecules.
Decreased growth factors lead to the loss of anti-apoptotic proteins (e.g., Bcl2, Bcl-x).
Pro-apoptotic proteins like Bak, Bax, and Bim replace them.
Release of cytochrome c from the mitochondria activates the caspase cascade.
Caspase 9 is the first to be activated.
What happens during the execution phase of apoptosis?
Caspases 8, 9, 6, and 3 disrupt the cytoskeleton and break down the nucleus.
Histology shows shrunken cells, fragmented cytoplasm, and apoptotic bodies, which are phagocytosed by other cells.
No inflammation occurs during apoptosis.
What is a caspase?
Caspases are a family of enzymes that play essential roles in apoptosis and cell death.
They are responsible for breaking down cellular structures and executing programmed cell death
What is apoptosis and why is it important?
Apoptosis is programmed cell death that eliminates damaged, unnecessary, or potentially harmful cells without causing inflammation.
It is essential for tissue remodeling, including during embryonic development, metamorphosis, and regression of tissues.
Apoptosis also plays a role in controlling cancer and other diseases by eliminating damaged cells.
What are the two main pathways of apoptosis?
The two main pathways of apoptosis are:
Intrinsic Pathway (Mitochondrial Pathway): Triggered by internal stress such as DNA damage or lack of growth factors.
Extrinsic Pathway (Death Receptor Pathway): Triggered by external signals, such as death ligands binding to death receptors on the cell surface.
What are the key steps in the intrinsic (mitochondrial) pathway of apoptosis?
Cellular Stress Detection: Internal stress like DNA damage or oxidative stress activates pro-apoptotic proteins (e.g., Bax and Bak) from the Bcl-2 family.
Mitochondrial Outer Membrane Permeabilization: Bax and Bak form pores in the mitochondrial membrane, releasing cytochrome c.
Cytochrome c Release: Cytochrome c binds with Apaf-1 to form the apoptosome, which activates caspase-9.
Activation of Caspases: Caspase-9 activates caspase-3 and caspase-7, executing apoptosis by cleaving key cellular proteins.
DNA Fragmentation: Caspases cleave proteins involved in DNA repair, leading to DNA fragmentation.
Cellular Breakdown: The cell shrinks, and fragments into apoptotic bodies, which are engulfed by phagocytes.
What are the key regulators of the intrinsic pathway?
Bcl-2 Family Proteins: The balance between pro-apoptotic (e.g., Bax, Bak) and anti-apoptotic proteins (e.g., Bcl-2, Bcl-xL) determines whether apoptosis will occur.
Cytochrome c and Apaf-1 are crucial for activating the caspase cascade.
What are the key steps in the extrinsic (death receptor) pathway of apoptosis?
Death Receptor Activation: Death ligands (e.g., FasL, TNF) bind to death receptors (e.g., Fas, TNFR1) on the cell surface.
Formation of DISC: This triggers the formation of the Death-Inducing Signaling Complex (DISC), recruiting caspase-8.
Activation of Caspase-8: Caspase-8 activates downstream effector caspases (e.g., caspase-3, caspase-7).
Caspase Cascade: Caspases cleave cellular proteins, leading to apoptosis.
Crosstalk with Intrinsic Pathway: Caspase-8 can activate Bid, linking the extrinsic pathway to the intrinsic pathway and amplifying apoptosis.
Cellular Breakdown: Similar to the intrinsic pathway, the cell undergoes shrinkage, DNA fragmentation, and formation of apoptotic bodies, which are phagocytosed.
What are the key regulators of the extrinsic pathway?
Death Receptors: Fas, TNFR1, and TRAIL receptors are key players.
Caspases: Caspase-8 (initiator), caspase-3, and caspase-7 (effector) execute the cell death program.
What are the differences and similarities between the intrinsic and extrinsic pathways?
Triggering:
Intrinsic Pathway is triggered by internal cellular stress (e.g., DNA damage, oxidative stress).
Extrinsic Pathway is triggered by external signals, such as binding of death ligands to death receptors.
Molecular Components:
Intrinsic involves the mitochondria and Bcl-2 family proteins.
Extrinsic involves death receptors and caspases.
Crosstalk:
The extrinsic pathway can activate the intrinsic pathway by cleaving Bid, leading to mitochondrial permeabilization and enhancing apoptosis.
What is the overall outcome of apoptosis through both pathways?
Both the intrinsic and extrinsic pathways lead to programmed cell death (apoptosis) through the activation of caspases, resulting in cell shrinkage, DNA fragmentation, and the formation of apoptotic bodies.
These bodies are then engulfed by phagocytes, preventing inflammation and tissue damage.
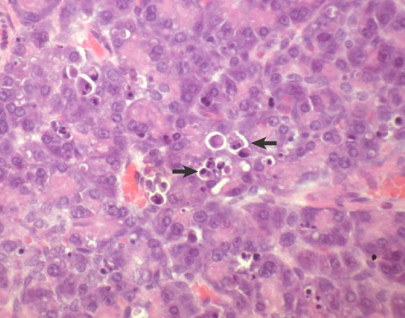
What is occuring at the marked location?
Apoptosis