ANSC*2340: Final Exam
1/231
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
232 Terms
endocrine system
Works together with the nervous system.
Helps to maintain homeostasis in the body.
Responsible for producing messengers (hormones) that will coordinate the body’s response to different situations and stimuli.
Reacts slowly to changes, but sustains the responses for long periods.
Cells → hormones (messengers) → blood stream → target tissues (most body cells and tissues).
endocrine glands (“ductless” glands)
Glands located throughout the body that secrete small amounts of hormones directly into the bloodstream.
e.g. thalamus, hypothalamus, pituitary gland, adrenal gland, pancreas, ovaries, testes
exocrine glands
Glands that secrete their products onto epithelial surfaces through ducts.
e.g. pancreas (digestive enzymes), sweat glands, salivary glands, mammary glands, sebaceous glands
hormones
Chemical messengers produced by endocrine glands. Travel in the bloodstream to all parts of the body and bind to their particular receptors in or on the target cells.
Divided into three groups: peptide, streroid, monoamine.
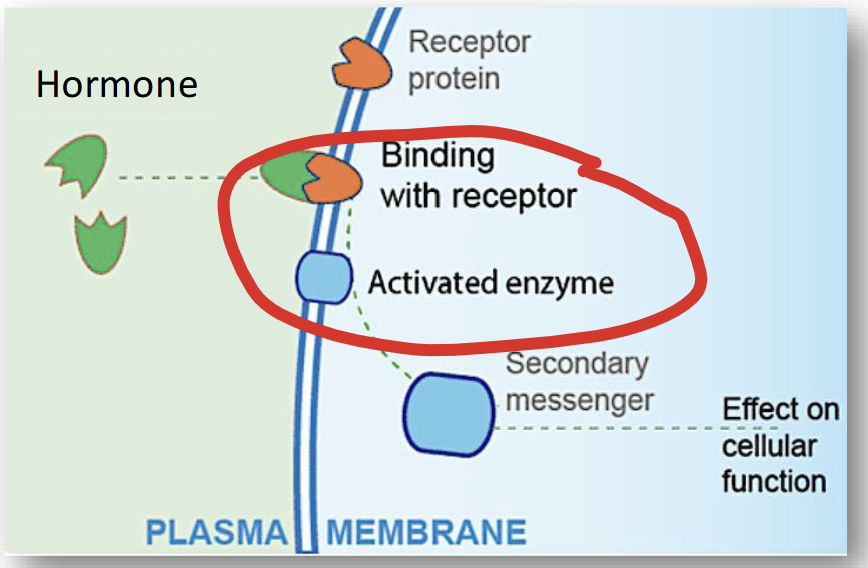
hormones with membrane receptors
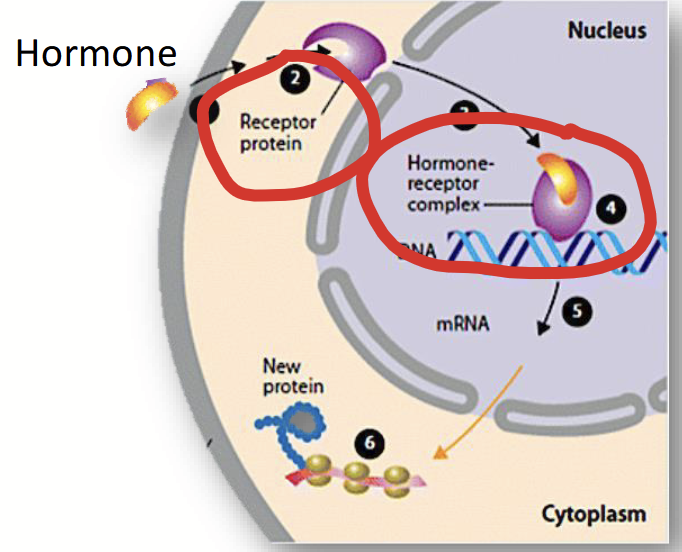
hormones with internal receptors
peptide hormones
Contain 200 or more amino acids.
Hydrophilic (soluble in water).
Easily travel in blood plasma.
Require receptors!
The most common type of hormone.
steroid hormones
Lipids synthesized from cholesterol.
Hydrophobic (insoluble in water).
Must bind to a transporter protein to travel in blood plasma.
Their receptors are found inside the cell (in the cytoplasm or in the nucleus).
monoamine hormones
Derives from amino acids and retain an amino group.
Contain both hydrophilic and hydrophobic types of hormones.
hormone secretion
Controlled by a feedback system:
Levels of hormones “feed back” the gland that produced it.
Feedback can increase or decrease the production levels of the hormone.
negative feedback
Rising levels of the hormone decrease the activity of the gland.
e.g. T3/T4
positive feedback
Falling levels of the hormone increase the activity of the gland.
major endocrine glands
Consist of the hypothalamus and the pituitary gland.
hypothalamus
A part of the diencephalon of the brain. It controls hormone release from the pituitary gland by producing, releasing, or inhibiting hormones under the control of nervous impulses.
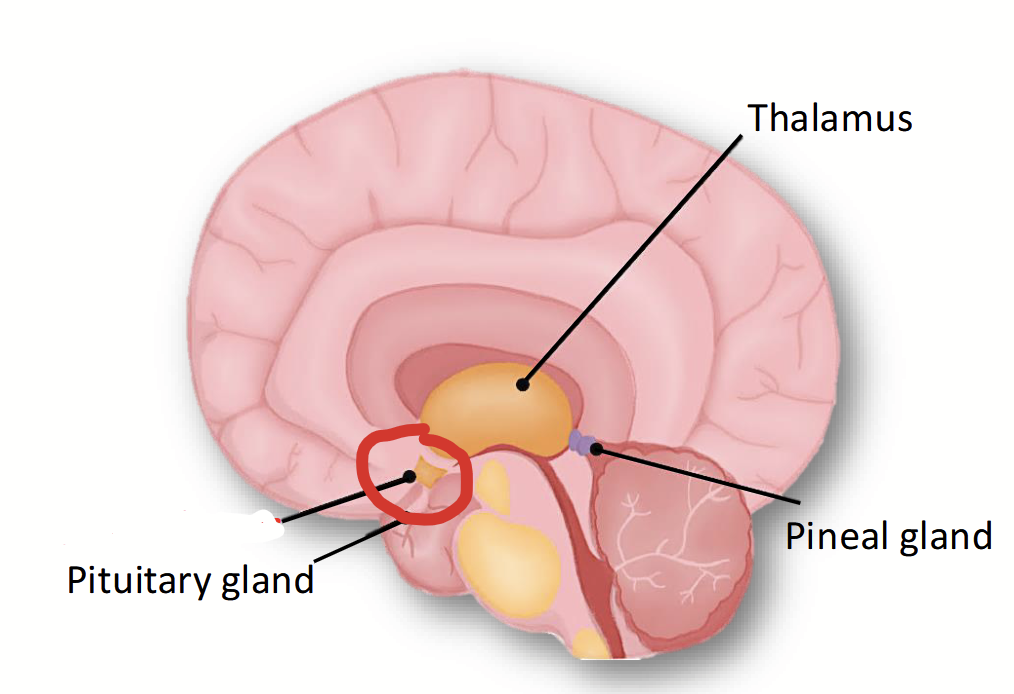
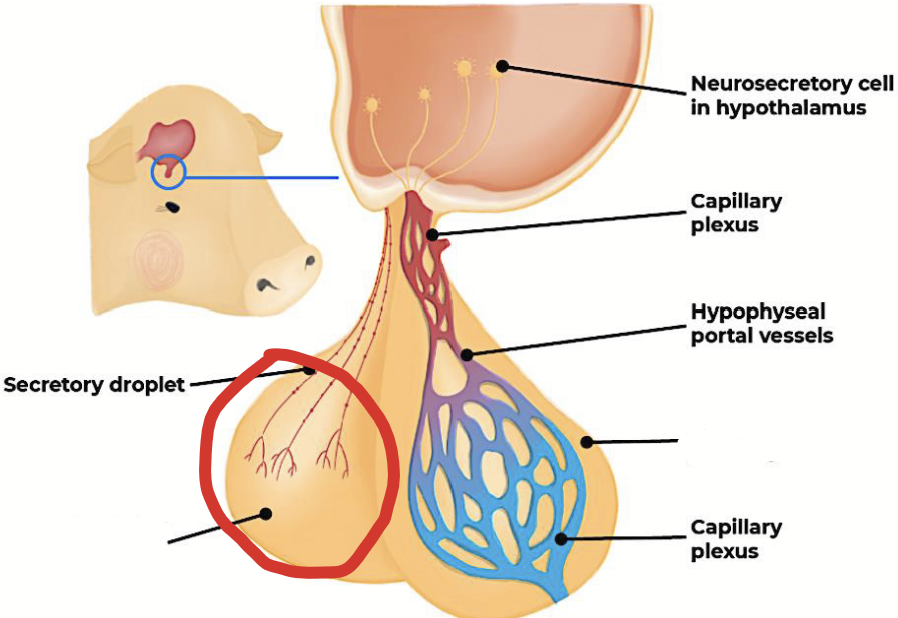
pituitary gland
Located ventral to the hypothalamus and is attached to it by a slander stalk. Also called the hypophysis.
Blood vessels and nerve fibres in the stalk enable the hypothalamus to control the activity of this gland and therefore most of the rest of the body. Its hormones direct the activity of other endocrine glands in the body.
Divided into two parts, with different structures, origins, and functions: anterior and posterior.
anterior pituitary
Part of the pituitary gland that produces most hormones. Connected with blood vessels (portal blood vessels). When stimulated by the hypothalamus or via direct feedback by target tissues, produces hormones.
Hormones from the hypothalamus are secreted into portal blood vessels, which carry them to this part of the pituitary gland.
Develops from glandular tissue in the embryo.
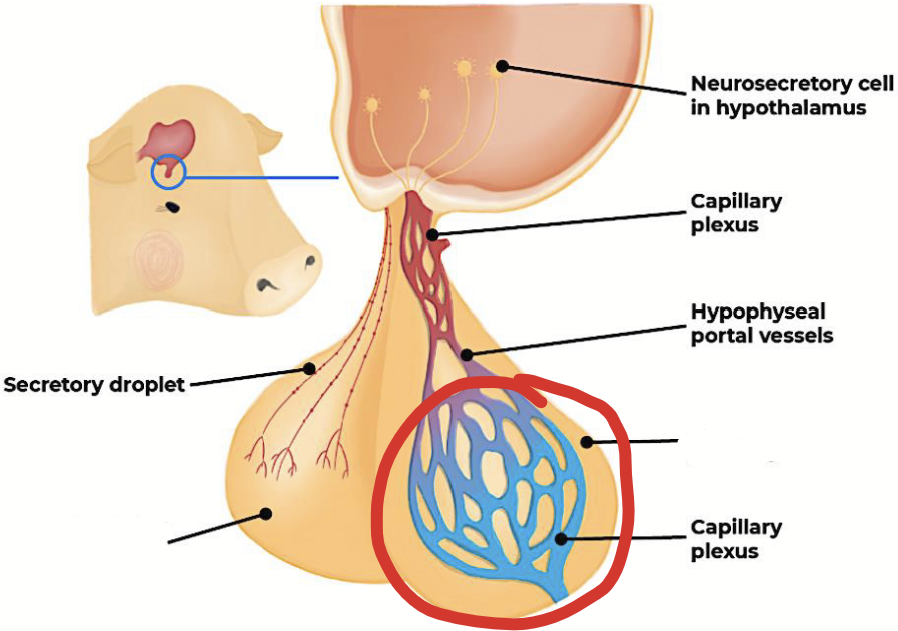
posterior pituitary
Part of the pituitary gland that is connected to the hypothalamus via nerve fibres. It does not produce hormones. Rather, it stores (main function) and releases two hormones produced in the hypothalamus.
Neurosecretory cells in the hypothalamus produce hormones that are transported down nerve fibres to this part of the pituitary. Their release is controlled by nerve impulses from the hypothalamus.
Nerve impulses from the hypothalamus tell the nerve endings here when to release stored hormones into the bloodstream.
Develops from the nervous system in the embryo.
anterior pituitary hormones
Growth hormone (GH)
Prolactin
Thyroid-stimulating hormone (TSH)
Adrenocortictropic hormone
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LSH)
Melanocyte-stimulating hormone
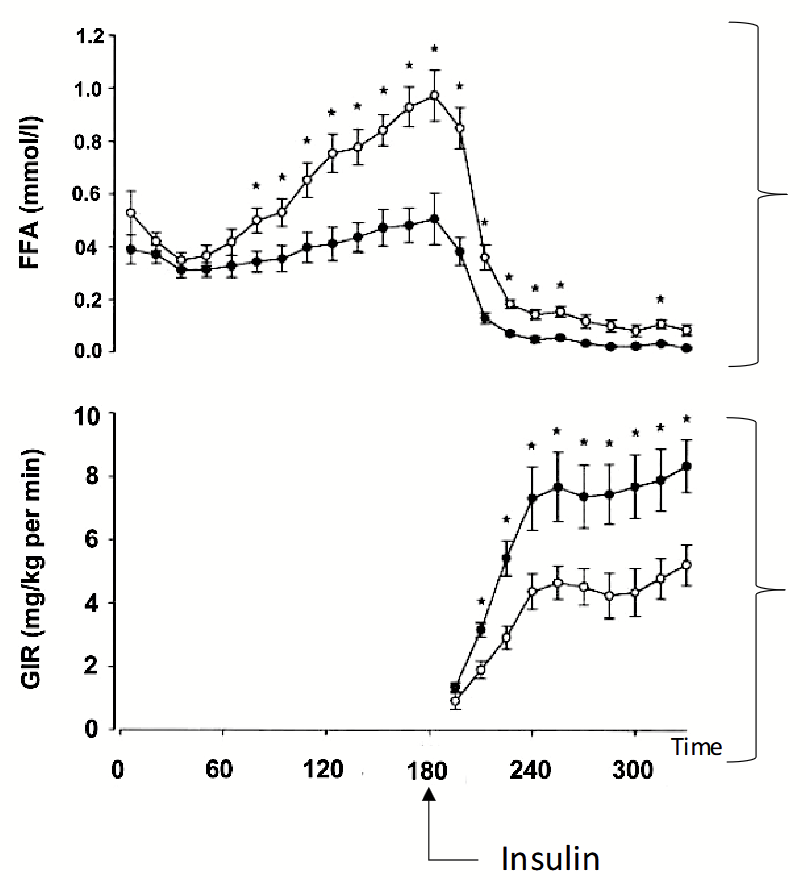
growth hormone (GH)
Hormone produced by the anterior pituitary that acts in all body cells to help regulate the metabolism of proteins, carbohydrates, and lipids.
Effects on metabolism: encourages anabolism of proteins → enhances tissue growth; catabolism of lipids and carbs.
Causes mobilization of fat tissue and breakdown of lipids for energy production (catabolism).
Discourages cells from using carbohydrates as energy sources, causing increased levels of blood glucose (opposite effect of insulin).
growth hormone effects on metabolism
Greater levels of free fatty acids when hormone was infused → breakdown of lipids into FFA.
Lower levels of glucose when hormone was infused during hyperinsulinemic clamp → lower levels because we are using glucose.
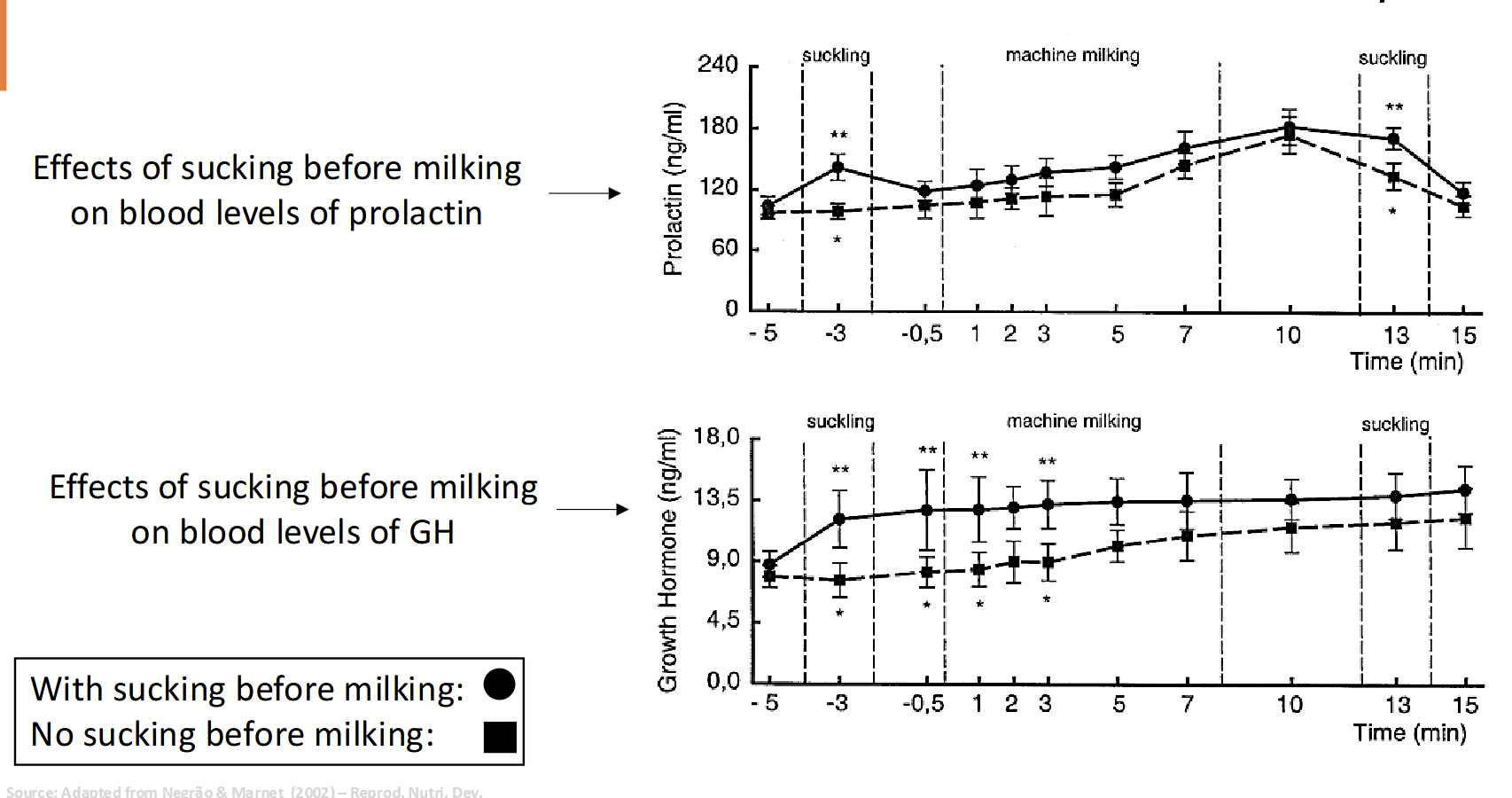
prolactin
Hormone produced by the anterior pituitary. Helps trigger and maintain lactation (secretion of milk by mammary glands). Its production and release is stimulated by nursing or milking of the teat (once ceased, milk production will also cease). Also supports breast tissue growth.
Has a positive feedback cycle.
lactation
Positive feedback via prolactin. Milk is released when offspring suckles on the teat → more suckling, more prolactin is released.
Suckling → milk release → offspring growth → teeth growth → pain while suckling → mother stops suckling → no nursing → less prolactin → lactation ceases.
Cows: don’t want to dry up, stimulate suckling via machines.
prolactin and growth hormone levels due to external stimulus
Greater levels of prolactin when suckling before milking: suckling leads to brain readying itself for body’s milking → brain stimulates hormone.
Also stimulates the release of oxytocin, which plays a role in GH levels.
Greater levels of growth hormone when suckling before milking: stimulates sensory nerves → stimulates brain activity in hypothalamus → hypothamalus stimulates anterior pituitary → stimulates hormones → body readies itself for milking.
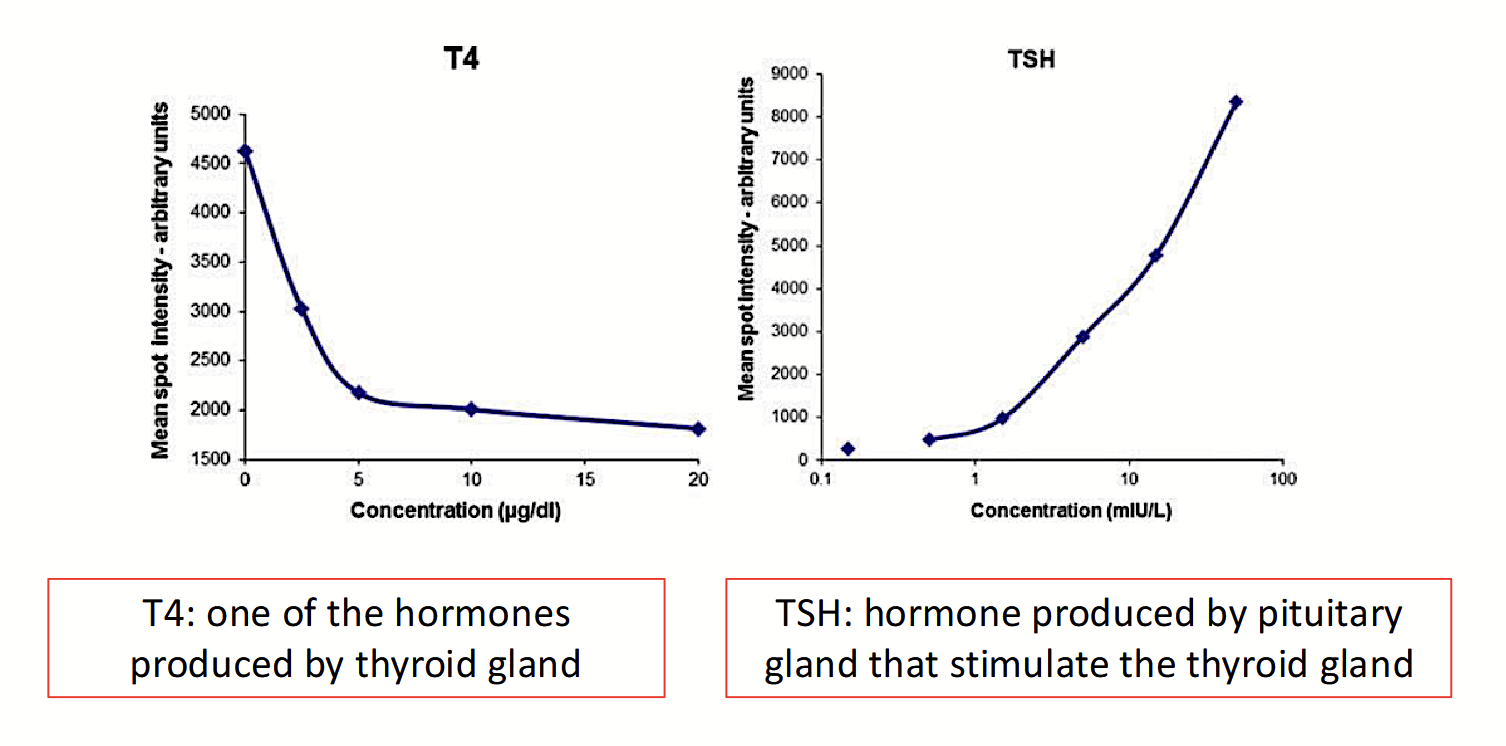
thyroid-stimulating hormone (TSH)
Hormone produced by the anterior pituitary. Stimulates the growth and development of the thyroid gland, causing it to produce its hormones (T3 and T4).
Production is regulated by thyroid hormone levels → negative feedback mechanism.
TSH feedback cycle
Negative feedback cycle:
Low levels of thyroid hormones (T3/T4 below bodily needs) → feedback stimulates anterior pituitary gland to produce more TSH → TSH activates thyroid gland → produces more T3 and T4.
Adequate/high levels of thyroid hormones (T3/T4 levels reach bodily demand) → feedback stimulates anterior pituitary gland to produce less TSH → TSH activates thyroid gland → thyroid gland produces less T3 and T4.
follicle-stimulating hormone (FSH)
Hormone produced by the anterior pituitary. Stimulates the growth and development of follicles in the ovaries and thus oogenesis (female gamete production).
Hypothalamus releases GNRH → stimulates anterior pituitary → produces hormone.
Stimluates the secretion of estrogens (female sex hormone → positive feedback) and stimulates spermatogenesis in males (negative feedback).
In males, stimulates the Sertoli cells to produce sperm → more sperm → signals less production.
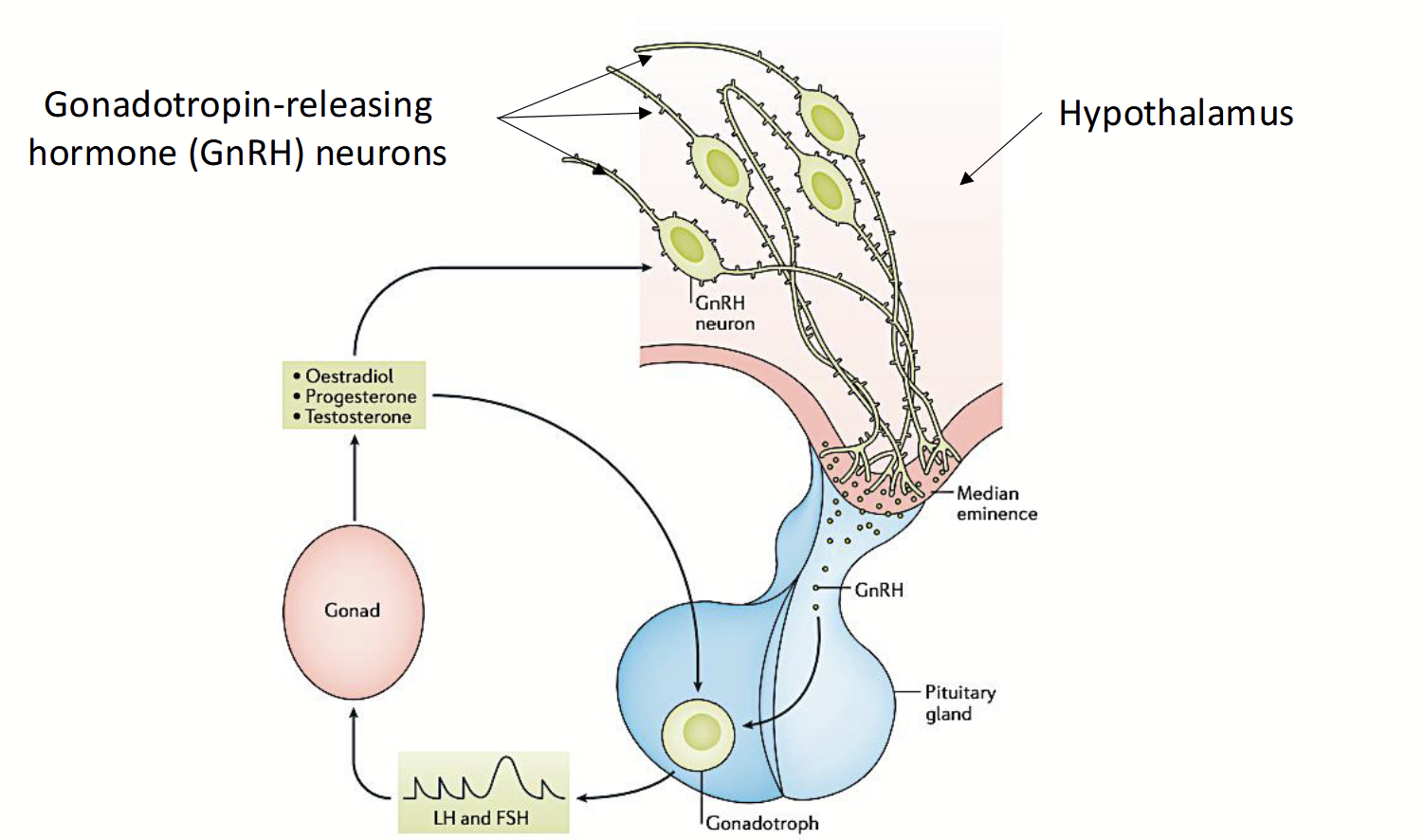
gonadotropin-releasing hormone (GnRH)
Released from the hypothalamus to stimulate the anterior pituitary to produce and released FSH.
luteinizing hormone (LH)
Hormone produced by the anterior pituitary. Completes the process of follicle development in the ovary that was started by FSH, triggering the ovulation of an egg.
Mid-cycle: positive feedback → ovulation.
As the follicle grows and produces more estrogens, they feed back to the anterior pituitary, causing lowered FSH production and higher production of this hormone.
Once ovulation has occurred, high hormone levels stimulate the cells left behind in the empty follicle to multiply and develop into another endocrine structure: the corpus luteum.
In males, stimulates interstitial cells in the testes to produce testosterone.
gonadotropins
FSH and LH, since they stimulate the growth and development of the gonads (ovaries and testes).
hypothalamic-pituitary-gonadal axis
Hormonal system that regulates FSH and LH production.
GnRH neurons → GnRH starts production in the hypothalamus → stimulates anterior pituitary → pituitary releases FSH and LH in response to GnRH.
Negative feedback cycle for males.
Positive feedback cycle for females.
melanocyte-stimulating hormone (MSH)
Hormone produced by the anterior pituitary. Associated with colour changes in pigment cells of reptiles, fish, and amphibians.
posterior pituitary: hormones released
Antidiuretic hormone
Oxytocin
antidiuretic hormone (ADH)
Hormone produced by the hypothalamus; stored (at nerve endings) and periodically released by the posterior pituitary.
Helps the body conserve water in times of short supply by acting on the kidneys. Causes the kidneys to reabsorb more water from the urine they are producing back into the bloodstream.
Hypothalamus detects osmolarity in the blood and signals the posterior pituitary to release the hormone.
Caffeine and alcohol inhibit this hormone!
Prevents diuresis!
oxytocin
Hormone produced by the hypothalamus; stored (at nerve endings) and periodically released by the posterior pituitary.
Uterus: induces contraction via myometrium (layer with lots of muscles).
Breeding: helps movement of spermatozoa up to oviducts (via uterine contractions).
Parturition: aids the delivery and the expulsion of the placenta (via contractions).
Mammary glands: milk let-down (of milk previously produced) to the lower parts of the gland. Hormone circulates down to the mammary gland and causes the cells around the alveoli and small ducts to contract. Release of hormone is stimulated by nursing of teats.
oxytocin action on myometrium
Endogenous and exogenous oxytocin promotes myometrium contraction by activation of its receptors and its action on the voltage-regulate Ca2+ channels that facilitate Ca influx to the cell. Ca ions bind to G-protein receptors (activate phospholipase pathway).
Oxytocin acts on the smooth muscle cells of the myometrium.
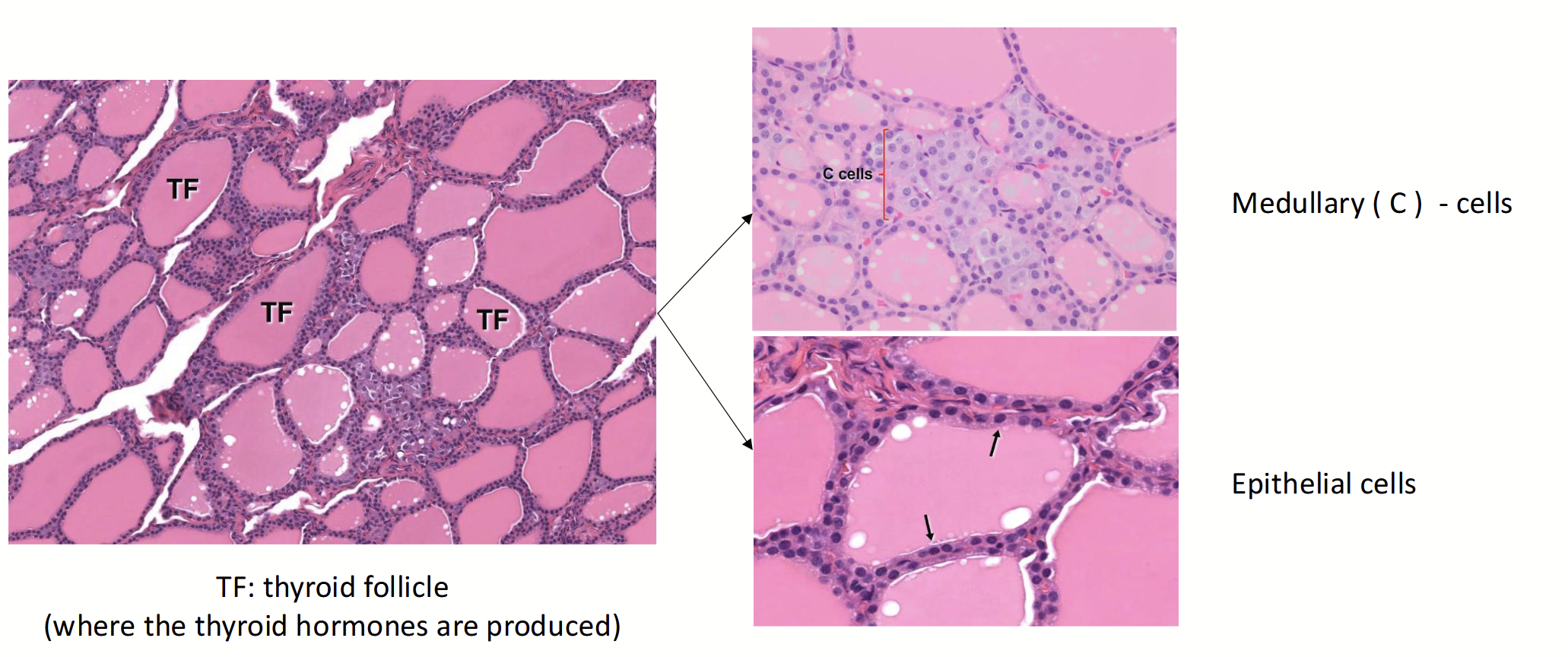
thyroid gland
Major endocrine gland that consists of two lobes located on each side of larynx.
Contains two distinct populations of hormone-secreting epithelial cells:
Thyroid follicular epithelium
Medullary (C) cells
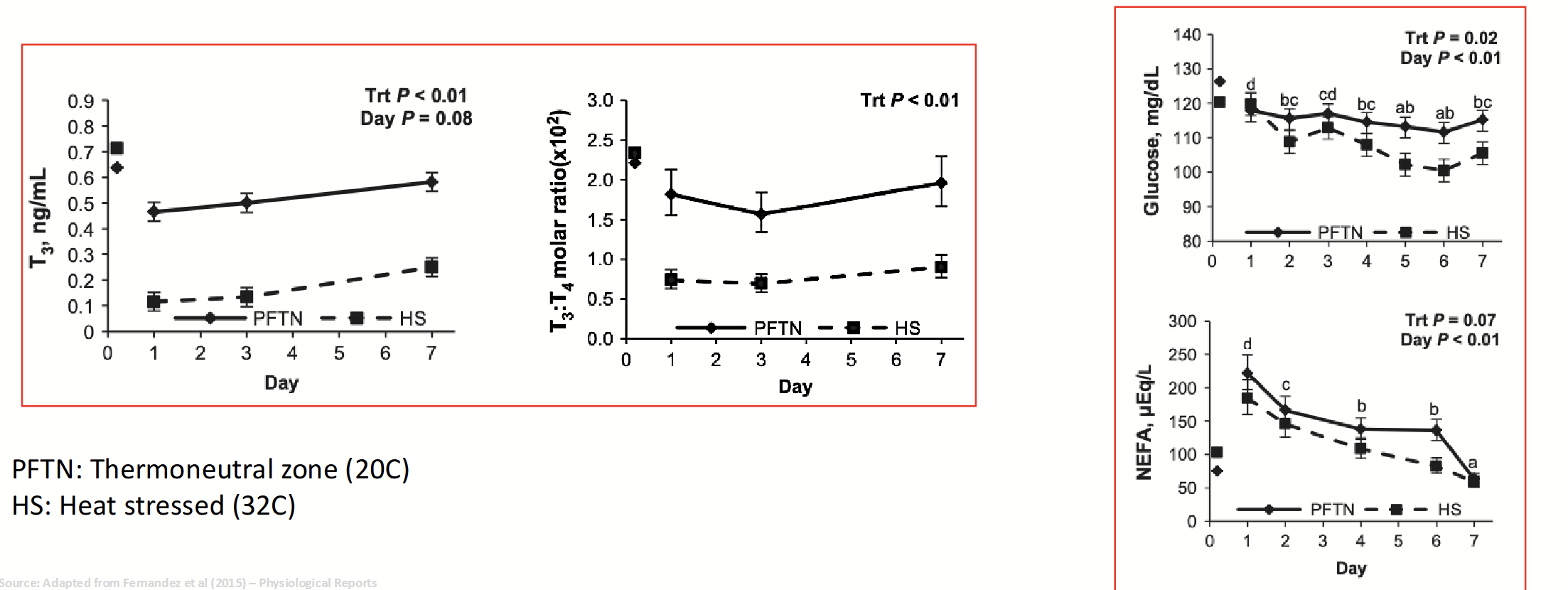
T3
The most biologically active form of thyroid hormone.
T4
Form of thyroid hormone that is converted to T3 in peripheral tissues, mainly in the liver, kidney, and muscle (as needed).
T3 and T4
Thyroid hormones. High levels lead to heat production + fat and glucose metabolism.
Calorigenic effect:
Regulates metabolic rate of the cells.
Helps to generate heat and maintain body temperature.
Protein, carbohydrate, and lipid metabolism:
May induce protein anabolism or catabolism.
Depends on the energy availability in the diet.
hyperthyroidism
High levels of T3 and T4. Causes cachexia (feeling too hot).
hypothyroidism
Low levels of T3 and T4. Leads to low levels of glucose metabolism and obesity.
thyroid gland: body temperature and metabolism
High T3 and T4:
More glucose available (thyroid makes too much hormone, leading to more breakdown, causing glucose buildup in liver).
High body temperature.
Low T3 and T4:
Less glucose available.
Lower feed efficiency, lower growth rates.
Lower body temperature.
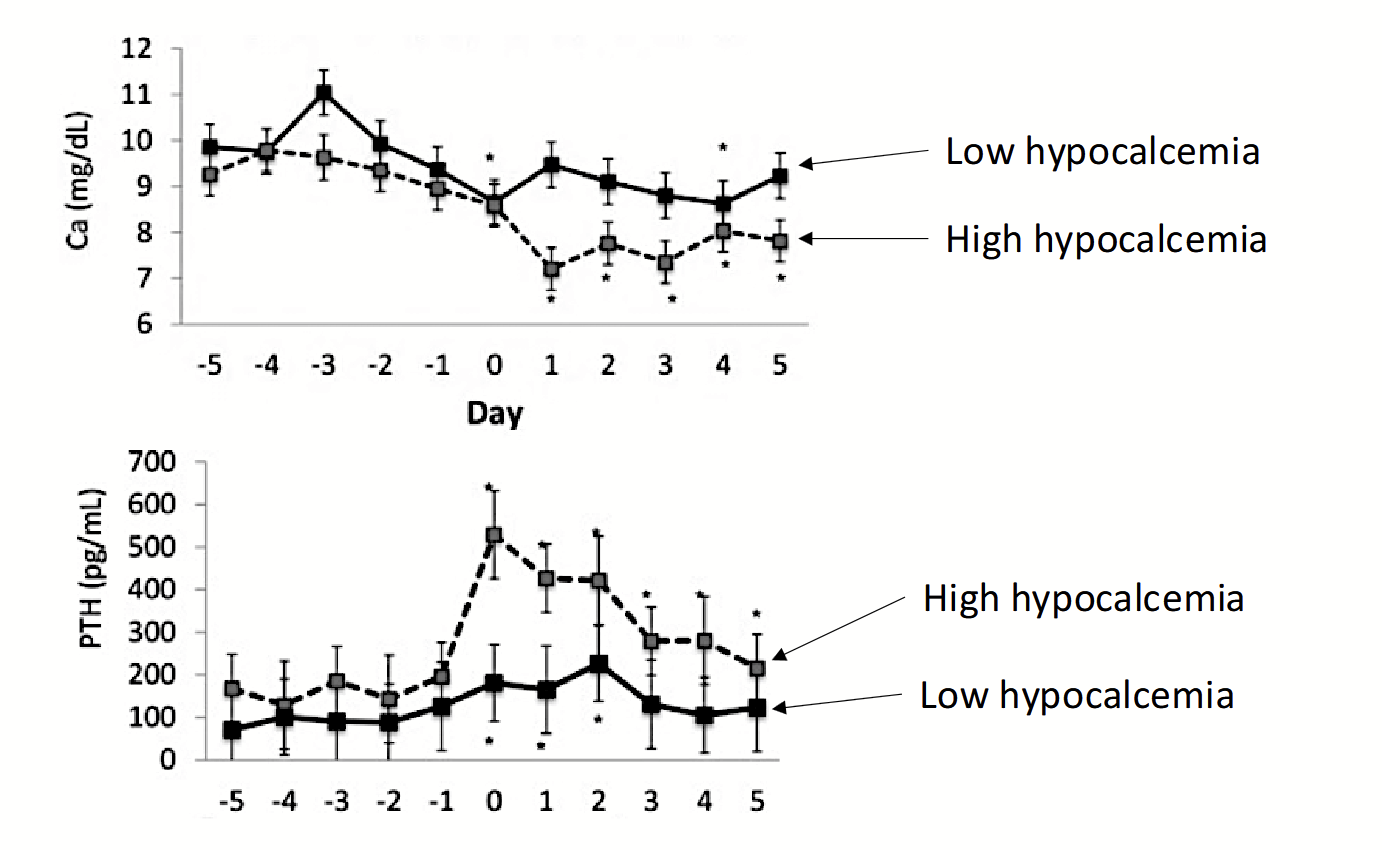
calcitonin
Hormone produced by C cells located between the thyroid follicles. Is one of two hormones involved in maintaining homeostasis of blood calcium levels.
Inhibits the resorption of bone Ca (inhibits release of bone Ca into blood) and increases urinary Ca loss → aims to lower blood concentrations of Ca.
Increase Ca2+ deposition in bone by osteoblasts.
Decrease Ca2+ uptake from intestines.
Decrease Ca2+ reabsorption from urine.
parathyroid gland
Several small, pale nodules in, on, or near the thyroid glands. Produces parathyroid hormone (parathormone).
parathyroid hormone
Hormone produced by the parathyroid gland. Helps to maintain blood calcium homeostasis. Is the antagonist (has the opposite effect) of calcitonin.
Increases renal Ca absorption and production of 1,25(OH)2D3 (active form of Vitamin D) → stimulates Ca absorption by intestinal epithelial cells.
Increase Ca2+ breakdown of bone by osteoclasts.
Increase Ca2+ uptake in intestines.
Increase Ca2+ reabsorption from urine.
parturient paresis (milk fiver)
A common disease following calving in dairy cattle. Caused by the high demand for Ca when the lactating period begins. Results from an inability of homeostatic mechanisms to regulate calcemia.
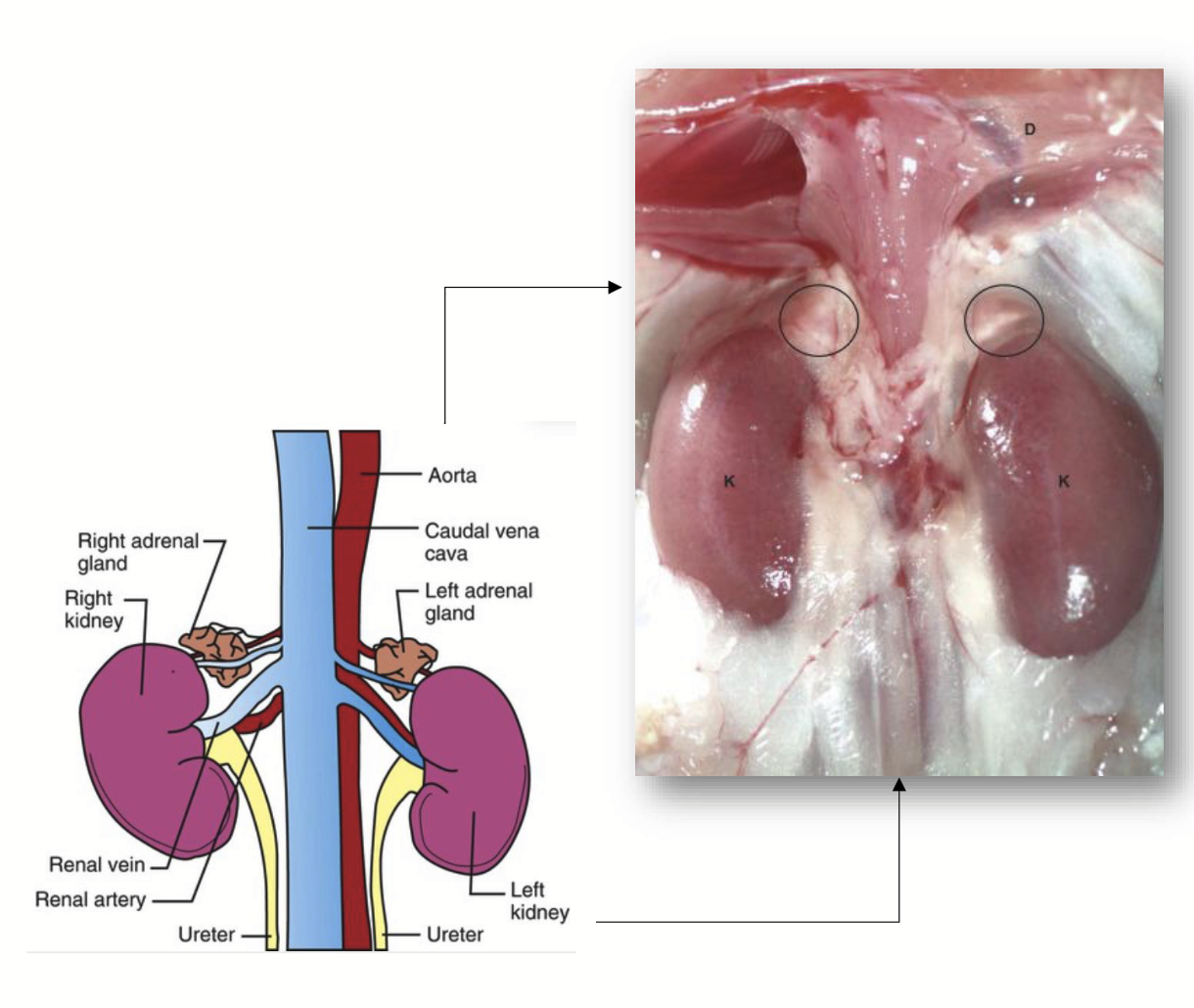
adrenal glands
Major endocrine glands found cranial and proximal to the kidneys.
Appear to be single structures, but they are actually two glands → has outer adrenal cortex and inner adrenal medulla, which have different structures and functions.
Stimulated and controlled by ACTH, a hormone produced by the anterior pituitary.
Produces three main groups of hormones:
Glucocorticoid hormones
Mineralocorticoid hormones
Sex hormones (small amounts)
glucocorticoid hormones
Lipophilic hormones produced in the adrenal cortex. Nave a negative feedback cycle.
Cortisol
Cortisone
Corticosterone
Prevent fainting, have a general hyperglycemic effects → activates mechanisms to increase blood glucose levels, important in flight or flight reactions.
Cause lipolysis and proteolysis → gluconeogenesis (increasing blood glucose).
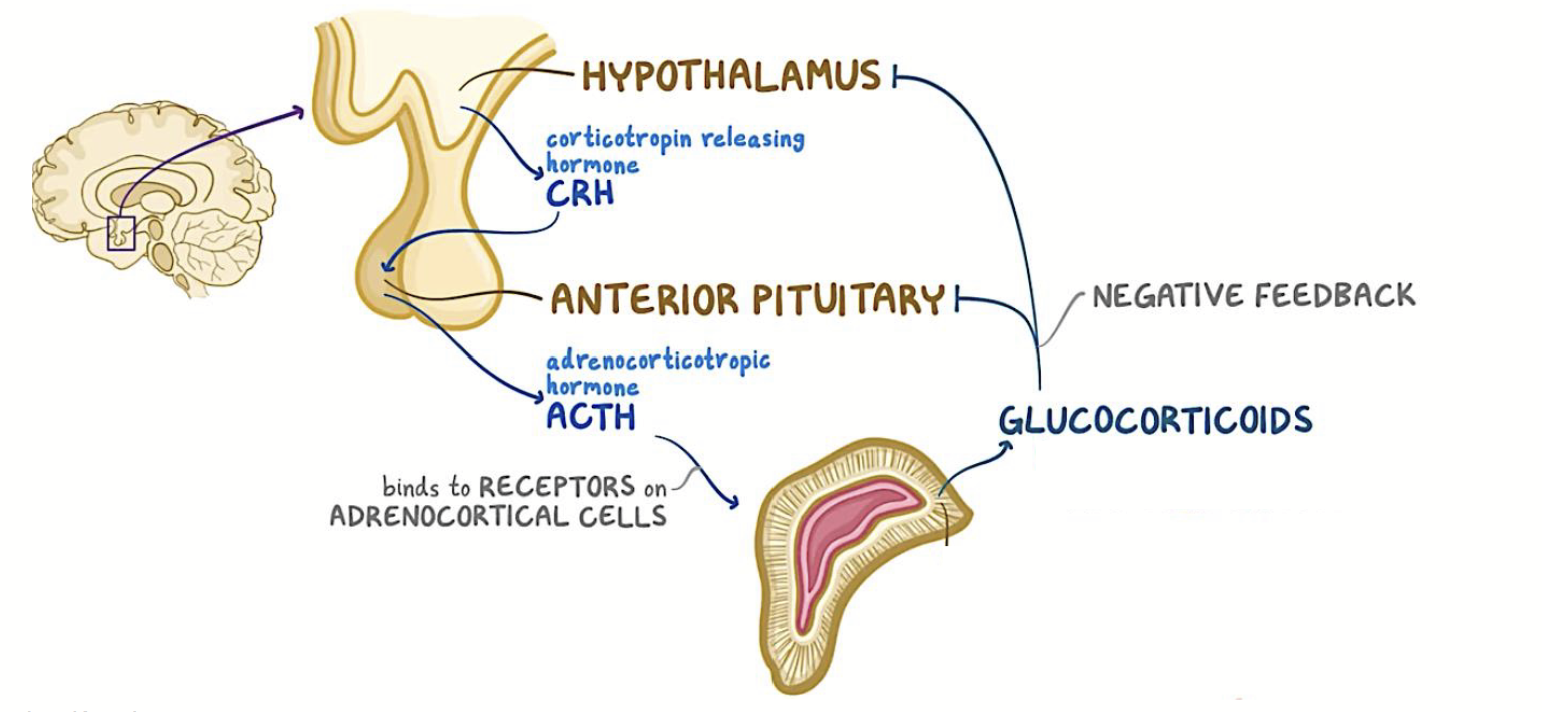
adrenocorticotropic hormone (ACTH)
Hormone produced by the anterior pituitary. Regulates the adrenal cortex via binding to receptors on adrenocortical cells.
adrenal medulla
Domain of the adrenal glands. Their secreting cells are modified neurons, which secrete hormones into the bloodstream.
Produces two very similar hormones, whose secretion is controlled by the sympathetic portion of the autonomic nervous system:
Epinephrine
Norepinephrine
adrenal medullary hormones
Epinephrine and norepinephrine → circulate around the body, helping to produce the whole-body fight-or-flight effect.
High levels of epinephrine lead to glycogen breakdown and reduced pH in meat → pale colour and water loss (PSE).
Long-term stress causes reduced glycogen and low lactic acid in muscle, resulting in high pH → dry and dark (DFD).
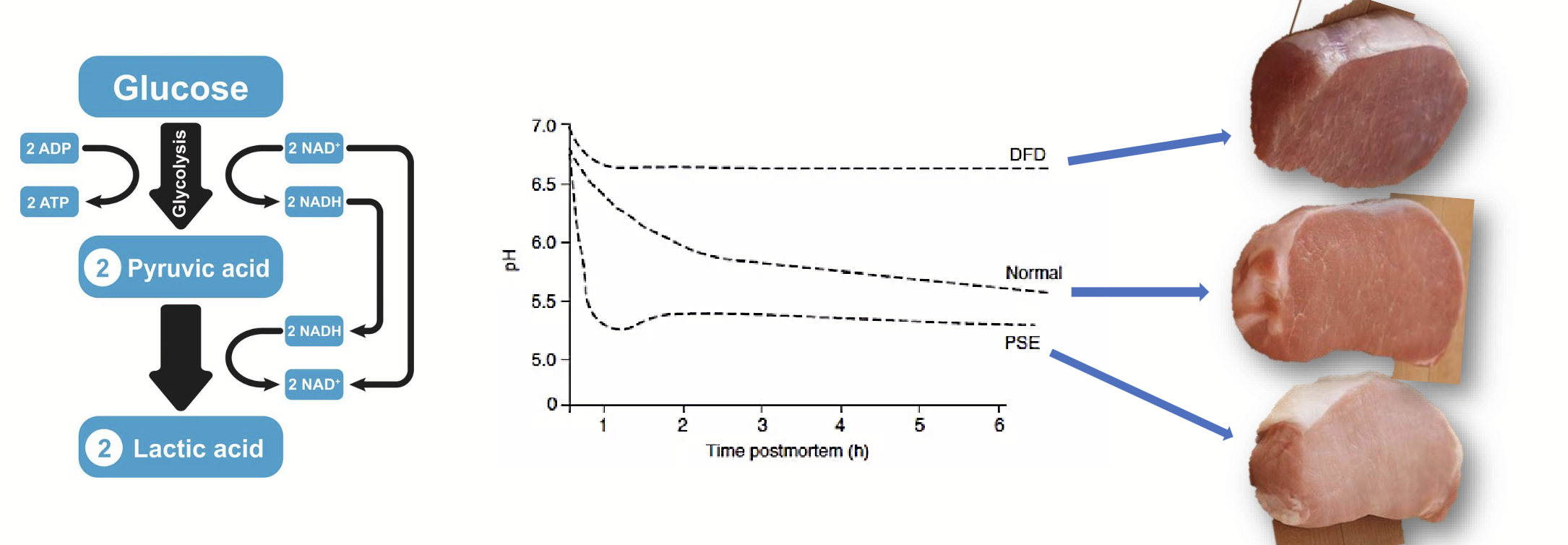
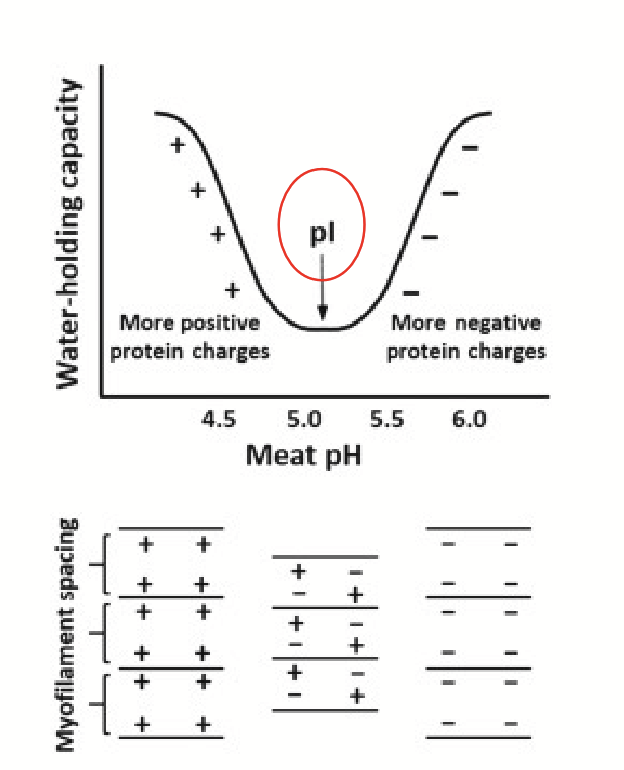
adrenal hormones and meat quality
pH in postmortem muscle declines due to the accumulation of lactic acid → reduction in the availability of reactive groups on the muscle proteins for binding water.
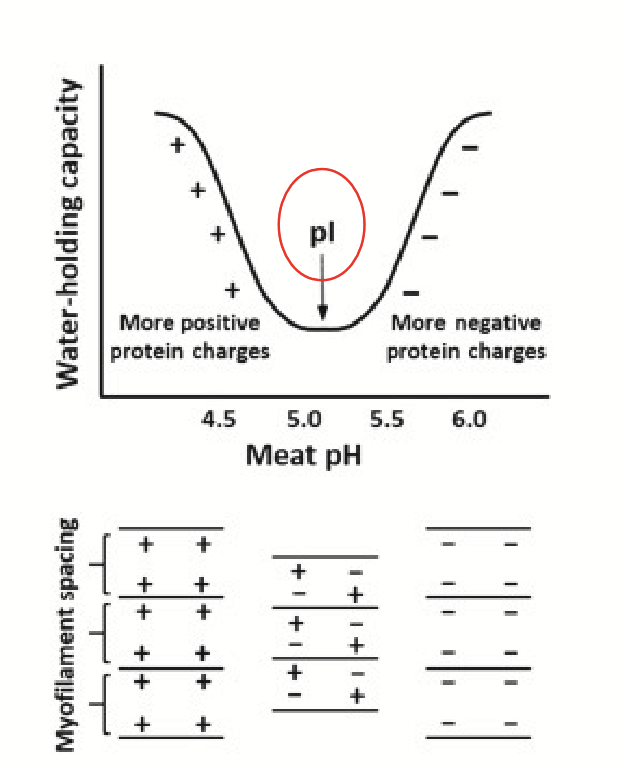
isoelectric point (pI) of a muscle protein
The pH at which the number of negative and positive charges on the protein are essentially equal and the overall net charge of the protein is zero.
At this pH, the positive and negative charged groups within a protein attract each other and the ability of the protein to attract and hold water is minimal.
mineralocorticoid hormones
Hormones produced in the adrenal cortex.
Target organ: kidney.
Main hormone: aldosterone.
aldosterone
The main mineralocorticoid hormone. Produced in the adrenal cortex and targets the kidney. Regulates the levels of important mineral salts in the body.
Acts mostly in the distal convoluted tubule and collecting ducts (starts with reabsorption of water).
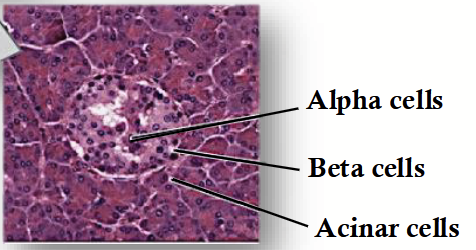
pancreas
Major endocrine gland that has both exocrine and endocrine functions. Its endocrine component makes up only a small percentage (1-2%) of the total volume of the organ.
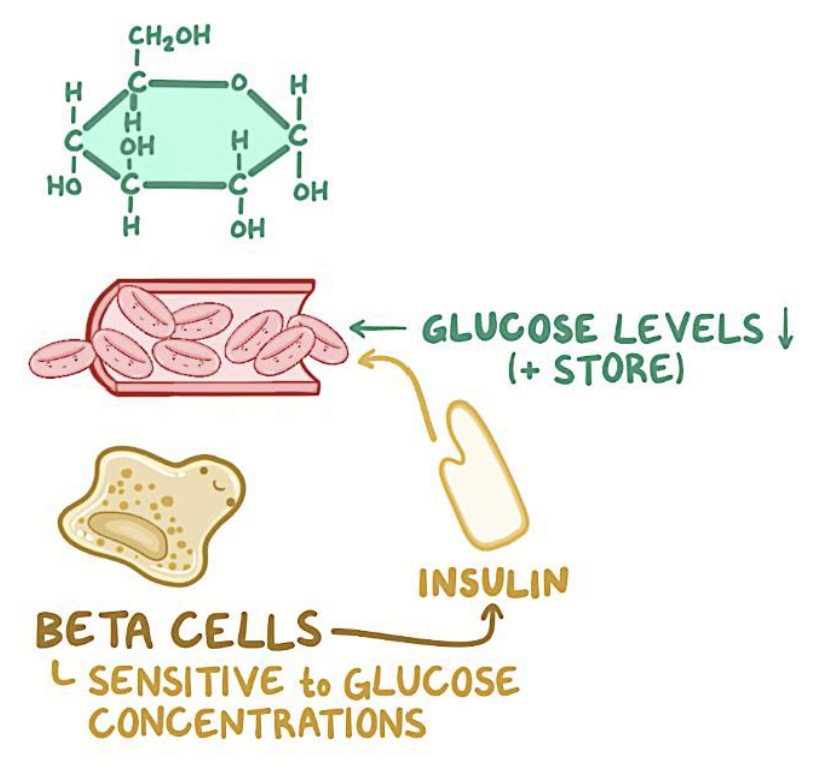
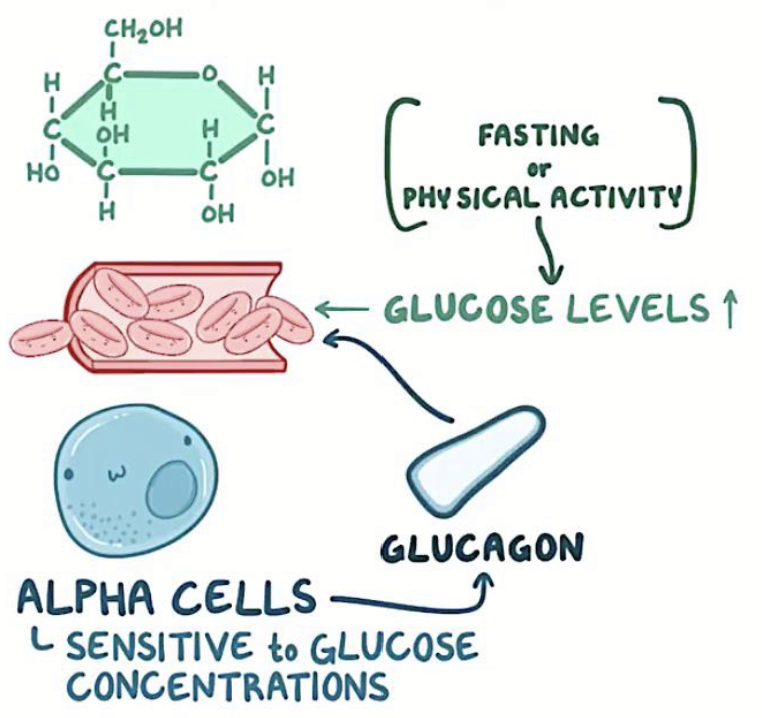
Contains islets containing…
Beta cells: produce insulin.
Alpha cells: produce glucagon.
Delta cells: produce somatostatin.
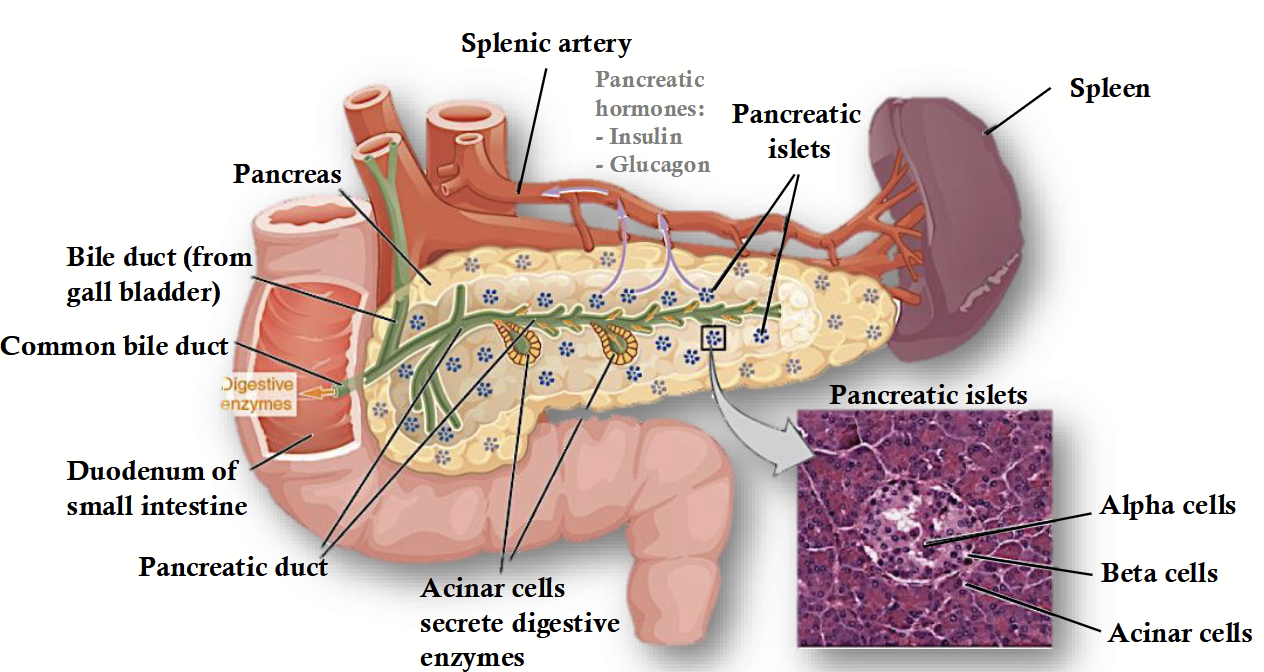
pancreatic islets
Contains:
Beta cells: produce insulin.
Alpha cells: produce glucagon.
Delta cells: produce somatostatin.
insulin
Trigger: increased glucose levels in bloodstream.
May be increased directly by dietary factors.
May be increased indirectly by action of other nutrients such as fatty acids and proteins.
GOAL: reduce blood glucose levels via cellular absorption.
glucagon
Trigger: decreased glucose levels in the bloodstream.
Want to increase blood glucose levels during fasting or after intense activity.
Also may be due to intense stress.
GOAL: increase blood glucose levels.
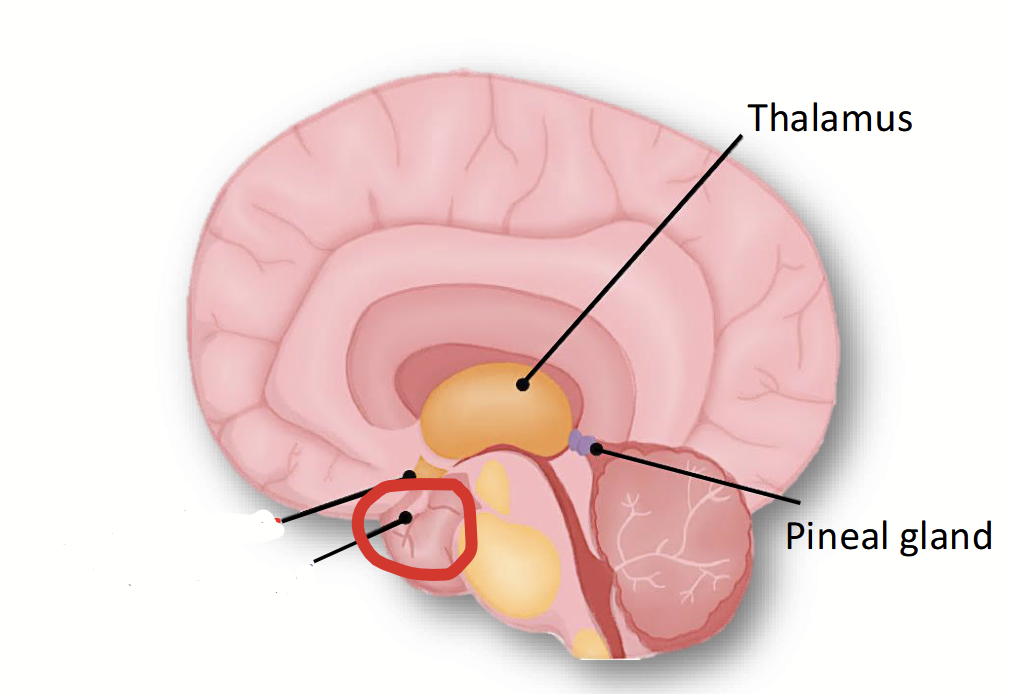
pineal body
Part of the brain located at the caudal end of the deep cleft that separates the two cerebral hemispheres. Functions are not well understood yet but known to produce melatonin, which affects wake-sleep cycles. May also play a role in the timing of seasonal estrus cycles in some species.
ovaries
Produce estrogens and progestins (and relaxin).
testes
Produce androgens (main one = testosterone).
thymus
Organ with partial endocrine function. Helps kickstart the immune system early in an animal’s life → promotes T cell development via thymosin and thymopoietin for cell-mediated immunity.
heart
Organ with partial encodrine function. Cardiomyocytes secrete brain natriuretic peptide (BNP), which is measured to determine heart failure.
stomach
Organ with partial endocrine function. Secretes gastrin to increase gastric fluids.
placenta
Organ that produces relaxin to relax uterine muscles and soften the cervix in preparation for birth.
skin
Organ with partial endocrine function - some species make Vitamin D3 here (properties of a hormone).
duodenum
Organ with partial endocrine functions: secretin (peptide hormone that regulates water homeostasis throughout the body and regulates secretions in the stomach, pancreas, and liver).
epinephrine
IN LIVER CELL:
Binds to β-receptor, glycogen deposits in cells break down and glucose is released from the cell.
IN SKELETAL MUSCLE BLOOD VESSEL:
Binds to β-receptor, causing the vessel to dilate.
IN INTESTINAL BLOOD VESSEL:
Binds to α-receptor, causing the vessel to constrict.
SYMPATHETIC NERVOUS SYSTEM EFFECTS:
Increased heart rate and output.
Increase blood pressure.
Dilated air passageway in lungs.
Decreased GIT function.
thyrotropin releasing hormone (TRH)
Hormone released from the hypothalamus to stimulate TSH secretion from the anterior pituitary.
Negative feedback loop → short and long.
colloids
Microscopic follicles found on the thyroid glands. Where T3 and T4 are stored (released when needed).
estrogens
Type of hormone produced by the ovaries. Cause physical and behavioural changes (preparation for breeding and pregnancy).
progestins
Type of hormone made by the corpus luteum. Functions in the maintenance of pregnancy.
Used to help avoid spontaneous abortions and suppress estrus in mares.
relaxin
Hormone made by the corpus luteum, uterus, or placenta (depending on the species). Relaxes the ligaments of the birth canal. Made late in pregnancy.
testosterone
Male sex hormone produced by testes. Contributes to secondary male sex characteristics, development of accessory sex glands, and growth of penis.
acinar cells (acini)
Cells in the pancreas with exocrine functions - synthesize, store, and secretesdigestive enzymes.
somatostatin
Hormone produced by the delta cells in pancreatic islets, the hypothalamus, and the intestine.
Inhibits secretion of insulin and glucagon.
Inhibits secretion of GH and TSH.
Inhibits cell division (used in cancer therapy).
Decreases GIT activity (inhibits acid and gastrin release from parietal cells in gastric pits).
adipose tissue
A specialized type of connective tissue that is composed of fat cells.
Located:
Beneath the skin (subcutaneous fat)
Between the muscles (intermuscular fat)
Behind the eyeballs
On the surface of the heart + around kidneys
Surrounding joints
In bone marrow
Among the omentum of the abdomen (e.g. internal, visceral, or body cavity fat)
Within the muscle (intramuscular fat)
subcutaneous fat
Adipose tissue located beneath the skin.
intermuscular fat
Adipose tissue located between the muscles.
intramuscular fat
Adipose tissue located within the muscle.
fat deposition
Fat stores present in an animal that are essential for life.
Internal fat depots protect vital organs.
Fat cells can expand or shrink depending on the amount of lipids being stored in them.
Fat gets deposited when energy inputs exceed energy requirements.
Body deposits this extra energy as fat.
adipose tissue function
General classification: modified connective tissue
Energy store: 2.25 times the energy in fat vs the amount of energy found in CHO or protein.
Fat added to diet can provide concentrated amount of energy to meet demands for high production.
Can mobilize fat stores to meet NRG requirements.
Pregnant + lactating animals will mobilize stores for additional NRG requirements.
Thermal insulator: prevents heat loss.
Mechanical shock absorber
Improves appearance of a finished carcass: use of the term “finishing” in red meat production.
Improves palatability or eating quality for meats: higher amounts of intramuscular fat (marbling) = more flavourful, more juicy.
adipose tissue: carcass quality
Setting up subcutaneous fat (hypodermis) → gives finished carcass appearance.
Effect on carcass grading:
Beef cattle: carcasses require 2 mm fat cover and certain amounts of marbling for carcasses to grade as high-quality beef.
Beef and pork: too much fat on carcass results in lower returns for producers; packing plants want lean carcasses and do not want to have to trim excessive fat.
marbling fat (intramuscular fat)
Doesn’t necessarily have an impact on tenderness.
Juiciness and flavour intensity are highly influenced by this:
The more marbling present, the higher the juiciness and flavour intensity!
Off flavours and odours can be due to oxidation of fats.
measuring fat deposition
Probe: measure fat depth in carcass and determine amount of lean yield.
Ultrasound and imaging software
origin of adipose tissue
Fetal synthes (early on in embryonic life)
Role of mesenchyme: originates from mesoderm.
Adipose cell precursors congregate in globules and accumulate small droplets of lipid.
Droplets will congregate and form large mass of lipid in the center of the cell.
Precursors are called preadipocytes or adipoblasts.
Stimulated to differentiate by various hormones.
mesoderm
One of the three primary germ lines that will produce all the tissues in the body. Responsible for synthesizing connective tissues.
mesenchyme
Originates from mesoderm.
Responsible for the synthesis of blood, skeletal tissues, lymphatic cells, and connective tissues (including adipose).
preadipocytes/adipoblasts
Adipose cell precursors. These cells resemble fibroblasts (in theory, the same cells that produce collagen and elastin can produce adipose tissue).
Located wherever fat may develop in the body. Stimulated to differentiate by various hormones: insulin, thyroid hormones, insulin growth factor-1 (IGF-1).
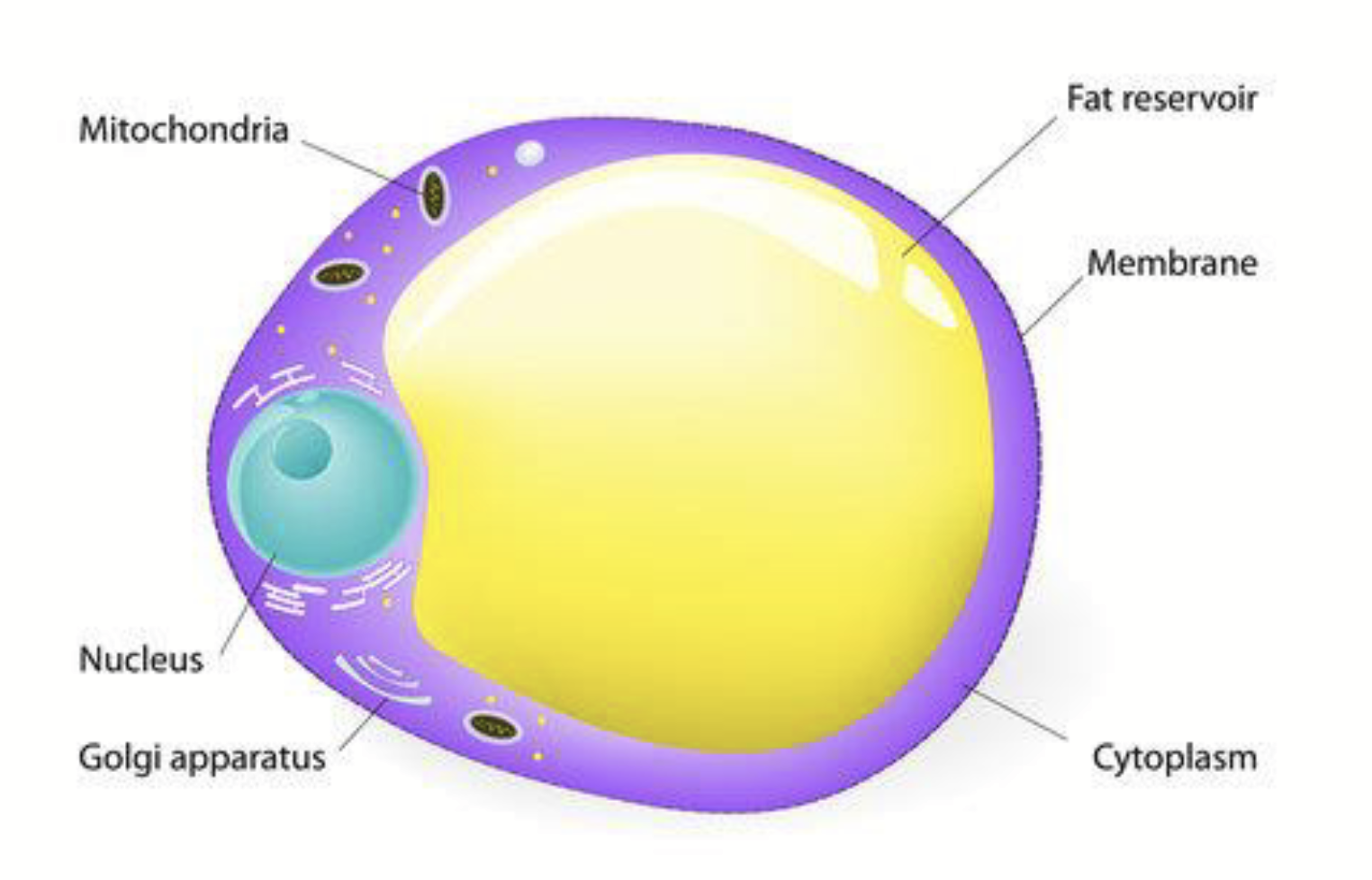
adipocyte
Cell filled with lipid.
Has nucleus, mitochondrion, and organelles; cytoplasm is pushed to one side of the cell.
Only small amounts of cytoplasm - results in low water content.
20g fat comes with 1g water (< 5%).
Meat protein (muscle) contains ~80% water.
Mature cells: > 95% lipid or triglyceride.
Once the cell starts to store triglyceride, it can no longer divide.
adipose tissue depots
Sites in the body where there is an accumulation of adipocytes.
Range in size:
Small groups of cells between muscle fasiculi are called intermuscular or seam fat (not very valuable to meat industry).
Large numbers of cells subcutaneously or viscerally (body cavity fat, e.g. kidney fat).
Intramuscular fat deposited in loose networks of perimysial connective tissue close to blood vessels.
Well supplied by blood capillaries (highly vascularized):
Because of the need to deposit fat in the first place - when fat is mobilized, need to provide energy for animals via blood capillaries.
Continuously grow:
Depending on energy intakes versus energy requirements.
Hypertrophy of the adipocytes occurs when there is an increase in adipocyte cell size due to high energy consumption.
Can be mobilized depending on nutritional status of the animal:
Fat cells can be used by the animal for supplying NRG to meet their demands.
Net fat accretion dependent on NRG inputs v.s. NRG requirements.
Fat deposition and mobilization require rich supply of blood vessels and enzyme systems.
accretion
The process of growth or enlargement by a gradual buildup.
hypertrophy of adipocytes
Occurs when NRG consumed exceeds NRG needs, resulting in an increase in adipocyte cell size.
internal, body cavity, and visceral fat
Adipose tissue depots that protect and insulate organs (e.g. omentum, mesenteries).
omentum
Thin sheet of adipose tissue located (contained) in a large fold of connective tissue.
Located over stomach and intestines.
Also called caul fat.
mesenteries
Thin connective tissue membranes supporting intestines. Also called lace fat.
phases of fat deposition
Phase 1: internal fat = first fat depots to be deposited in the body:
Visceral and kidney fat
Caul fat (omentum) and mesenteries
Phase 2
Subcutaneous
Intermuscular
Phase 3
Intramuscular
why does fat deposition occur in phases?
The body prioritizes internal fat storage/deposition because it protects vital organs and serves as a quick energy reserve for essential bodily functions.
fat deposition: phase 1
Internal fat is the first fat depots to be deposited in the body.
Visceral fat → metabolically active, provides quick source of energy in times of need.
Kidney fat
Caul fat (omentum) and mesenteries