Bio 226 Respiratory Lec
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
160 Terms
Respiratory system
supplies body with O2 for cellular respiration and dispose of CO2 (waste product of cellular respiration)
What system is closely coupled with the respiratory system?
circulatory system
What 4 processes are involved in respiration?
pulmonary ventilation (breathing), external respiration, internal respiration, and transportation of gases
What 2 processes does the respiratory system oversee?
pulmonary ventilation (breathing) and external respiration
What 2 processes does the circulatory system oversee?
transportation of gases and internal respiration
Pulmonary ventilation
breathing; movement of air into and out of lungs
External respiration
exchange of O2 and CO2 between lungs and blood; moves air out of the lungs
Transportation of gases
exchange of O2 and CO2 gases in blood
Internal respiration
exchange of O2 and CO2 between systemic blood vessels and tissues; moves air into the lungs
What is oxygen used for?
O2 is used for metabolism which produces energy
What is the concentration gradient of air flow?
From higher concentration of air to lower concentration of air
Nose (external nose and nasal cavity) function
Produces mucus to filter, warm, and moistens air
Paranasal sinuses function
Warms, moistens, and filters incoming air
Pharynx function
Passageway for air and food and facilitates exposure of immune system
Larynx function
Air passageway; prevents food from entering respiratory tract
Trachea function
Voice production and air passageway
Bronchial tree function
Cleans, warms,and moistens incoming air
Alveoli function
Site of gas exchange
Lung function
Houses respiratory passages
Pleurae function
Produces lubricating fluid
Sphincter function of larynx
Vocal folds may act as a sphincter to prevent air passage (ex. Valsalva’s maneuver)
Valsalva’s maneuver
Glottis closes to prevent exhalation, muscles will contract, abdominal pressure rises…to help empty rectum or stabilize trunk during heavy lifting.
Trachea
Windpipe; extends from larynx into mediastinum, where it divides into two main bronchi
How many layers is the trachea made up of?
3; mucosa, submucosa, and adventitia (includes hyaline cartilage, trachea lips, and carina)
Mucosa
Ciliated pseudostratified epithelium with goblet cells
Submucosa
Connective tissue with zero mucous glands supported by 16-20 C-shaped cartilage rings
C-shaped cartilage rings
Prevents collapse of trachea
Adventitia
Outermost layer made of connective tissue
Trachealis
Smooth muscle fibers; contracts during coughing to expel mucus
Carina
Last tracheal cartilage that branches into two main bronchitis; mucosa is highly sensitive
Violent coughing will be triggered if any foreign object makes contact with this structure
Bronchial tree
Air passages undergoing 23orders of branching
What structures give rise to respiratory zone structures?
Conducting zone structures
Conducting zone structures
Trachea > R/L Primary (main) bronchi > R/L Secondary (lobar) bronchi > R/L Tertiary (segmental) bronchi > bronchioles (less than 1 mm diameter) > terminal bronchioles (less than 0.5 mm diameter)
What change occurs during the transfer of air from bronchi to bronchioles?
Support structures change:
Cartilage rings become irregular plates
In bronchioles, elastic fibers replace cartilage
Respiratory zone structures
Respiratory bronchioles > alveolar ducts > alveolar sacs (saccules) > alveoli (last stop before gas exchange)
Respiratory membrane
Blood air barrier consisting of alveolar and capillary walls that fuse basement membranes (thin~0.5 ųm); allows for gas exchange by simple diffusion
What do alveolar walls consist of?
Type I alveolar cells (simple squamous epithelium-gas exchange) and Type II alveolar cells (cuboidal epithelium)
Type II alveolar cells function
Secrete surfactant and anti microbial proteins (pneumocyte)
What structures are alveoli surrounded by?
Fine elastic fibers and pulmonary capillaries to keep structures intact
Alveolar pores
Connects adjacent alveoli to equalize air pressure throughout lungs (provides alternout routes in case of blockage)
Alveolar macrophages (dust cells)
Keeps alveolar surfaces sterile in case of pathogens being swallowed/breathed in
2 million dead pathogens/hour are carried by cilia to throat and swallowed
Pleurae
Thin, double-layered serosal membrane; divides thoracic cavity into two pleural cavity into two pleural compartments and mediastinum
Parietal pleura
Membrane on thoracic wall, superior face of diaphragm, around heart, and between lungs (closest to other structures)
Visceral pleura
Membrane on internal lung surface (closest membrane to lung/organ)
Pleural fluid
(Fill slit-like pleural cavity between two pleurae) lubrication and surface tension that assists in expansion and recoil of lungs
Inspiration
Gases flow into lungs
Expiration
Gases exit lungs
Atmospheric pressure (Patm)
Enough air pressure present to push air into lungs; 0 mm Hg (760 mm Hg)
Trans pulmonary pressure
4 mm Hg (difference b/t 0 & -4); pressure transferring from blood to lungs
Intrapleural pressure (Pip)
-4 mm Hg (756 mm Hg); pressure b/t visceral & parietal pleura (pulls lungs open to expand to breathe easier)
Intrapulmonary pressure (Ppul)
Pressure within lungs; 0 mm Hg (760 mm Hg)
Pulmonary Ventilation
Consists of inspiration and expiration
Boyle’s law
Relationship between pressure + volume of a gas; if amount of gas is the same and container size is reduced, pressure will increase
Pressure inside of lungs is low, air can flow in (inhale) when lungs are filled w/ air (^ vol), air pressure outside lungs lowers (exhale)
Inspiration in pulmonary ventilation
active process involving inspiratory muscles
Action of the diaphragm
contracts downward and flattens out which increases thoracic volume (inhalation)
Action of intercostal muscles
rib cage is lifted up and out which increases thoracic volume (inhalation)
When can forced/deep inspiration occur?
during vigorous exercise or in people with COPD (chronic obstructive pulmonary disease)
Activated accessory muscles are also known as
scalenes, sternocleidomastoid, and pectoralis minor (erector spinae muscles of back also help to straighten thoracic curvature)
What is the function of activated accessory muscles?
further increase thoracic cage size, creating a larger pressure gradient so more air is drawn in
Passive process
also known as quiet expiration
Forced expiration
active process that uses oblique + transverse abdominal muscles
Three factors that influence the ease of air passage + amount of energy required for breathing:
airway resistance, alveolar surface tension, lung compliance
Airway resistance
major nonelastic source of resistance to gas flow; occurs in airways which in turn drives gas movement
Alveolar surface tension
the attraction of liquid molecules to one another at a gas-liquid interface which tends to cause alveoli to shrink (collapse)
Surfactant
body’s detergent-like lipid and protein complex that helps reduce surface tension of alveolar fluid (prevents collapse + produces type II cells)
Lung compliance
measure of change in lung volume given change in transpulmonary pressure (stretch of lung)
Why is lung compliance normally high?
the ability of lung tissue stretch
surfactant
easier to expand lungs
-diminished by aging
Respiratory volume
assesses respiratory status
Respiratory capacities
the combination of respiratory volumes to give insight on a person’s ability to transfer O2 into tissues
Anatomical dead space
consists of air that remains in passageways
Alveolar dead space
space occupied by non functional alveoli (due to collapse)
Total dead space
sum of anatomical and alveolar dead space
Spirometry can distinguish between:
obstructive pulmonary disease and restrictive disease
Obstructive pulmonary disease (COPD)
increased airway resistance (bronchitis)
Restrictive disease
reduced TLC due to disease or exposure to environmental agents (firbrosis)
Pulmonary functions tests
measure rate of gas movement
Forced vital capacity (FVC)
amount of has forcibly expelled after deep breath
Forced expiratory volume (FEV)
amount of gas expelled during time interval of FVC
FEV1
is the amount of air expelled in the 1st second
External respiration
diffusion of gases between blood and lungs
outside of body>lungs>blood
Internal respiration
diffusion of gases between blood and tissues
inside of body>blood>tissues
External and Internal respiration are subject to what processes?
basic properties of gases and composition of alveolar gas
Pulmonary gas exchange
involves exchange of O2 and CO2 across respiratory membranes
Exchange of O2 and CO2 is influenced by:
Ppg and has solubilities
thickness and surface area of membrane
ventilation-perfusion coupling
Ventilation-perfusion coupling
matching of alveolar ventilation with pulmonary blood perfusion
What form of respiration involved capillary gas exchange in body tissues?
internal respiration
Tissue PO2
lower partial pressure than in arterial blood, so O2 moves from blood to tissues
Tissue PCO2
higher partial pressure than in arterial blood, so CO2 moves from tissues into blood
Venous blood return pressure
PO2 = 40 mm Hg
PCO2 = 45 mm Hg
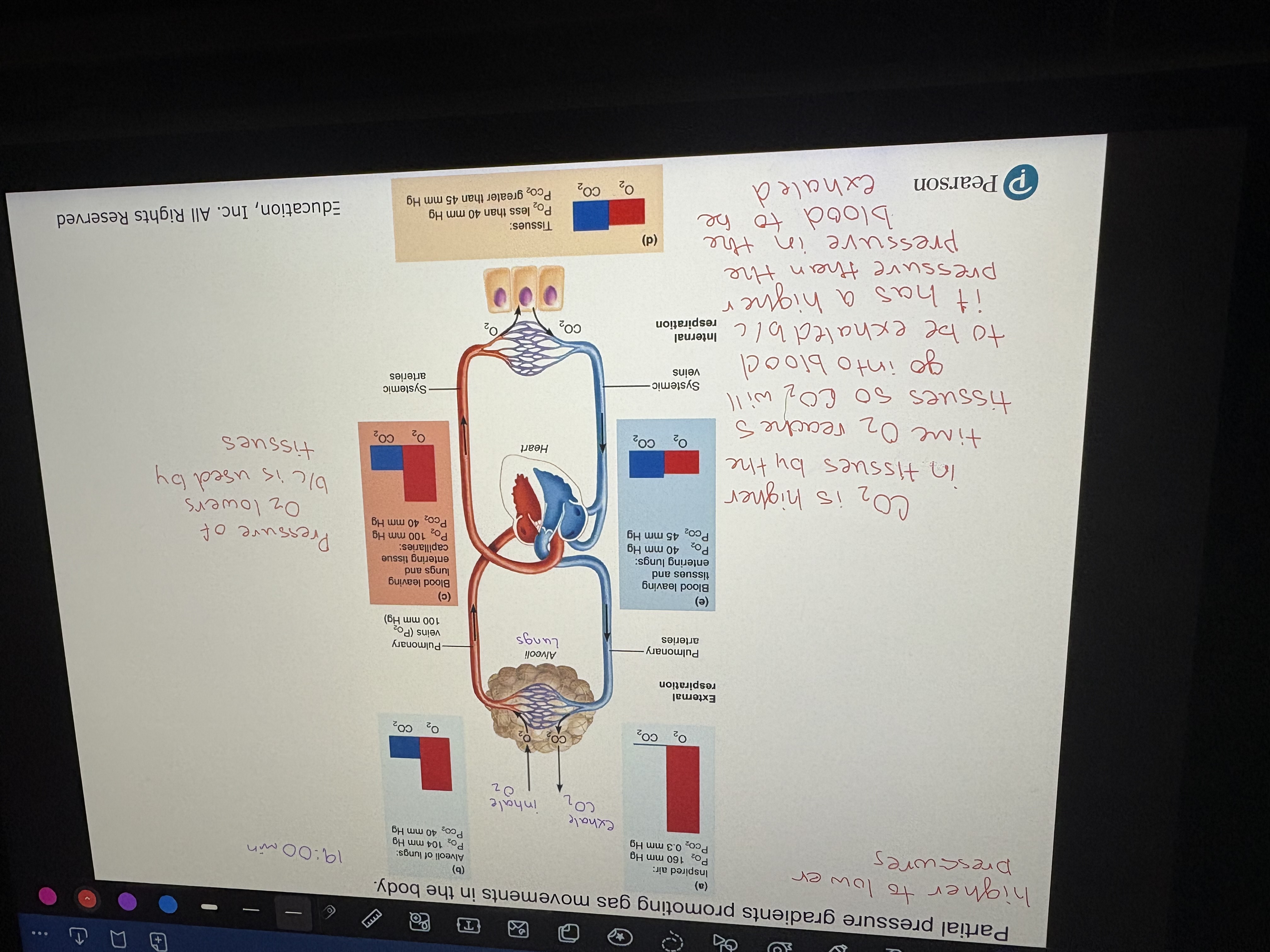
Partial pressure gradients promoting gas movements in the body
Factors that influence hemoglobin saturation:
PO2 + PCO2; partial pressure of O2/CO2 (^ pressure = ^ saturation)
Temperature (heat)
Blood pH
Concentration of BPG (bisphosphoglycerate)
Where is BPG produced?
during glycolysis by RBCs; when BPG levels ^ then O2 levels decrease
What happens when cells metabolize glucose?
the use of O2 increases in PCO2 and H+ in capillary blood
declines blood pH (acidosis)
increases PCO2 causing hemoglobin+O2 bond to weaken (Bohr effect)
O2 unloading occurs
What decreases hemoglobin affinity for O2?
heat production during movement
Hemoglobin-oxygen dissociation curve
percentage of Hb saturation with O2 at any partial pressure of oxygen
What influences the dissociation curve?
pH, CO2, Exercise, Temperature (effect how well O2 comes off Hb)
PO2 (lungs)
100 mm Hg (about 100% saturation)
PO2 (tissues at rest)
40 mm Hg (about 75% saturation)
PO2 (tissues during exercise)
15 mm Hg (about 25% saturation)
How is CO2 transported in the blood?
by being dissolved in plasma, bound to Hb, or as HCO3 ions (buffers to control pH-70%)