Deck 5: Choroid & Lens + Outflow pathway
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
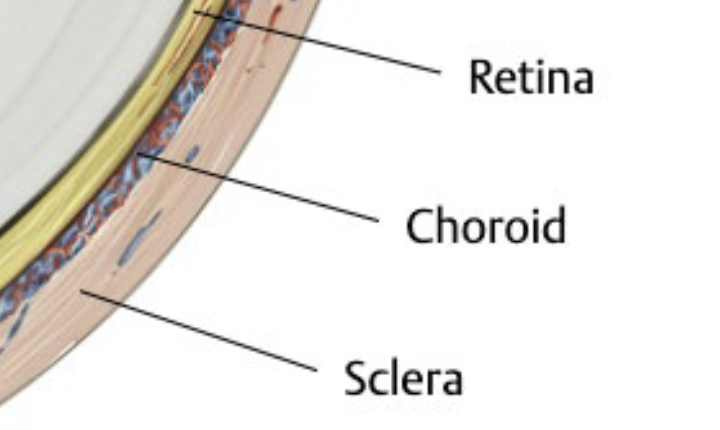
Define Choroid.
layer of dense vasculature thats continuous with the ciliary body vasculature till the optic nerve
Spongy, layered system of progressively smaller blood vessels residing within a pigmented, fibrocellular matrix
b/w the sclera & retina
Thickest in the macular & thinnest in its peripher
overall thickness declines with
normal aging
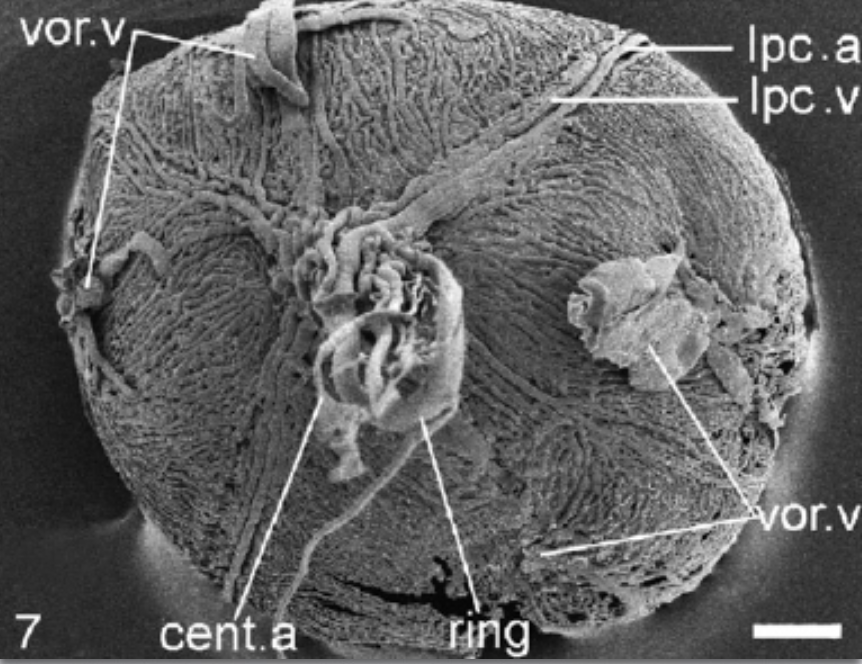
Describe the blood supply to and from the choroid.
From choroid:
supplies nutrients and O2 to the outer retina (photoreceptors & RPE)
high flow rate (similar to kidney’s flow rate)
To choroid:
ophthalmic artery supplies blood via branches of posterior and anterior ciliary arteries
majority from LPCA
segmented blood supply (each segment has its own supply)
borders between segments (watershed zones) are at higher risk of poor circulation
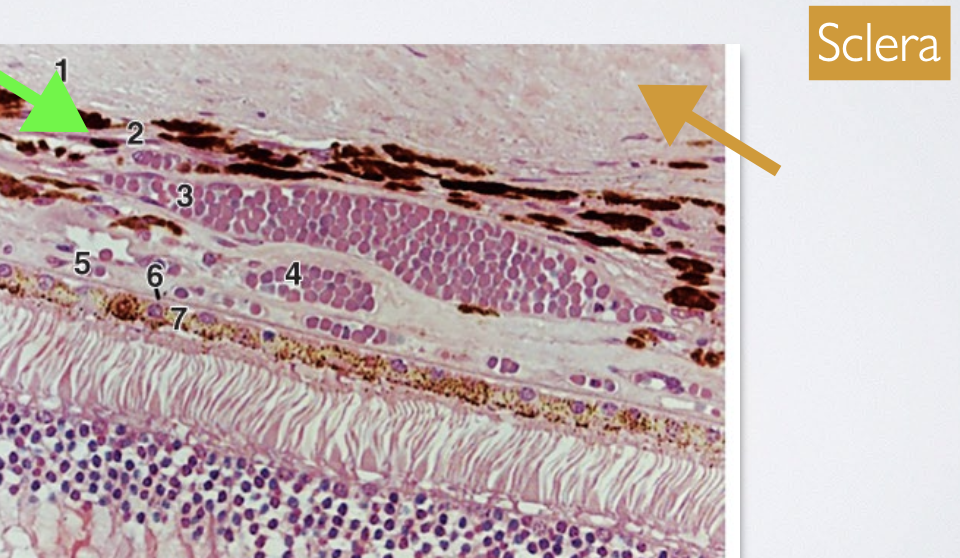
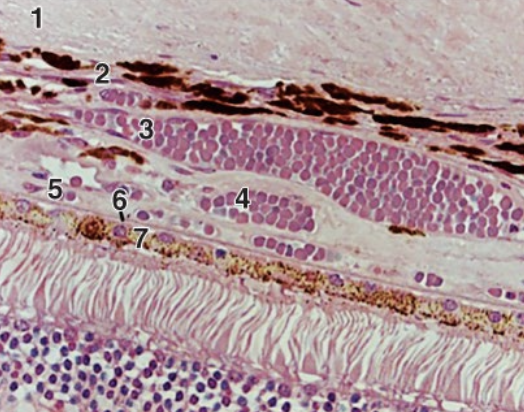
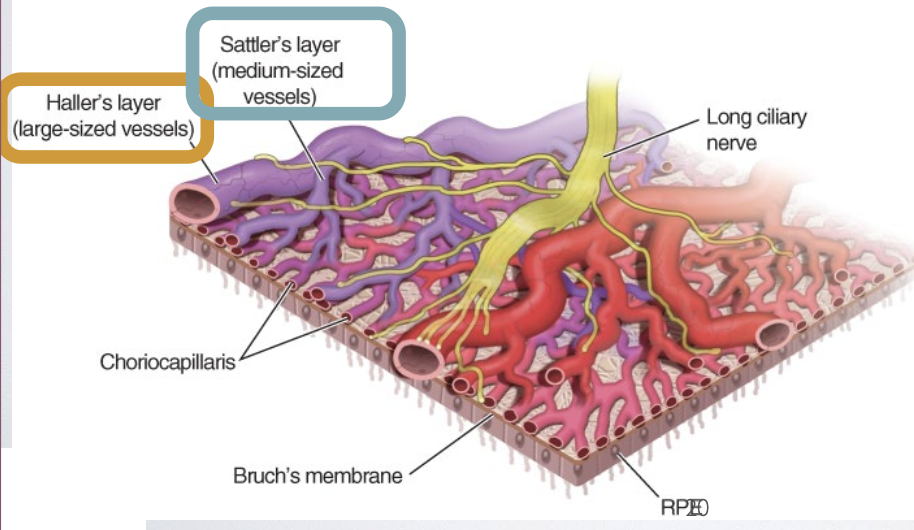
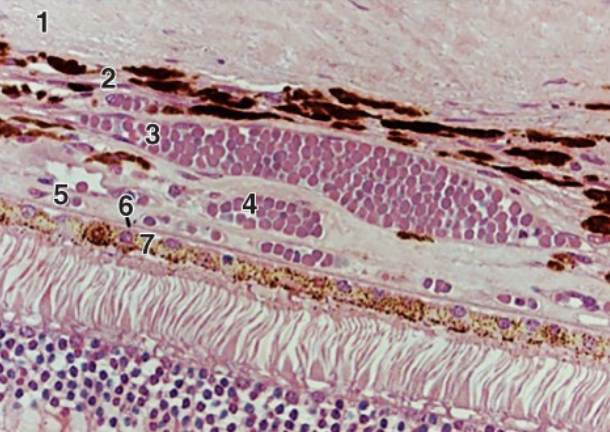
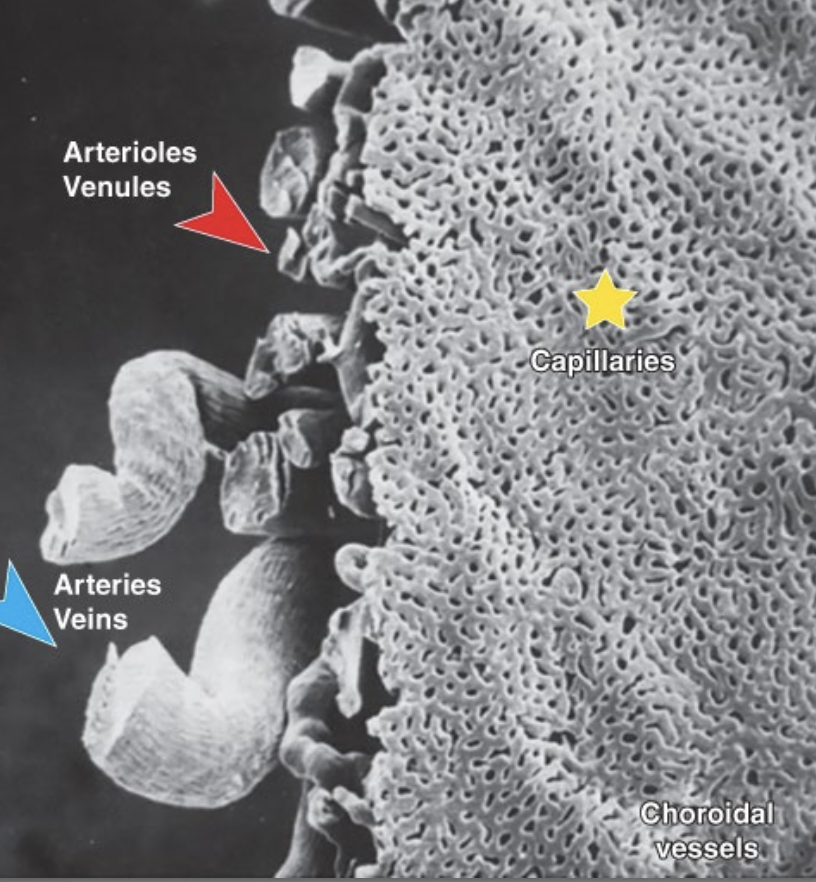
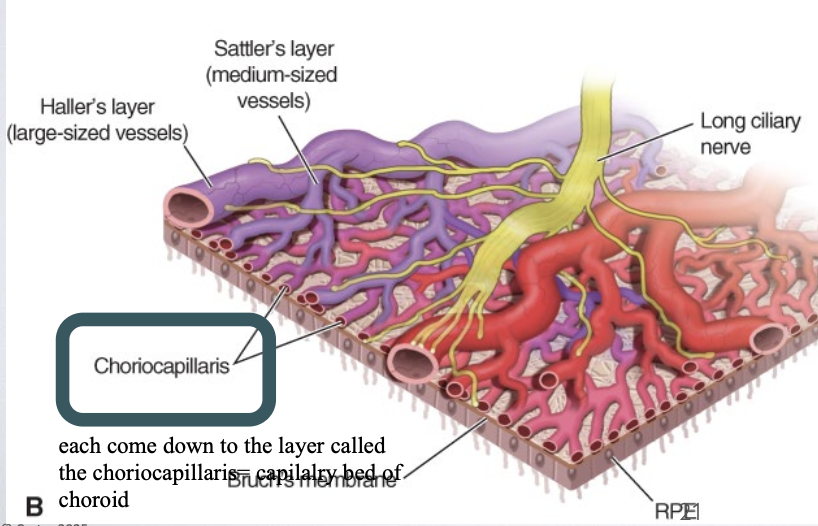
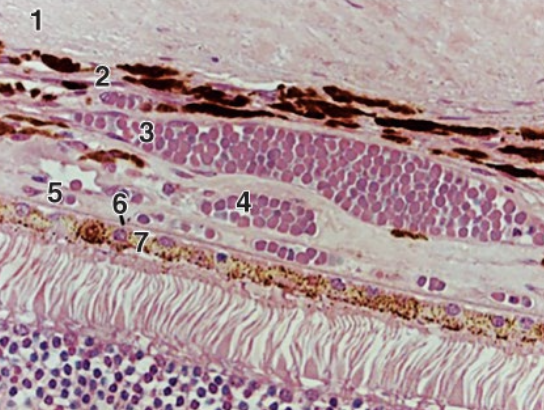
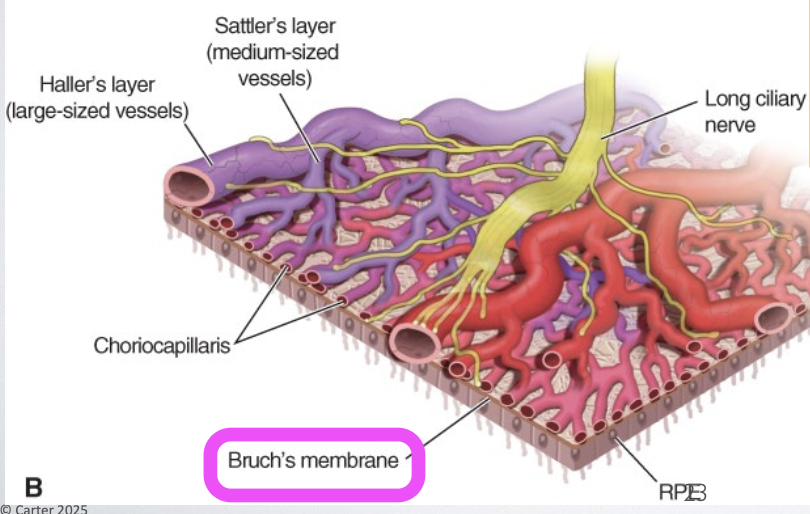
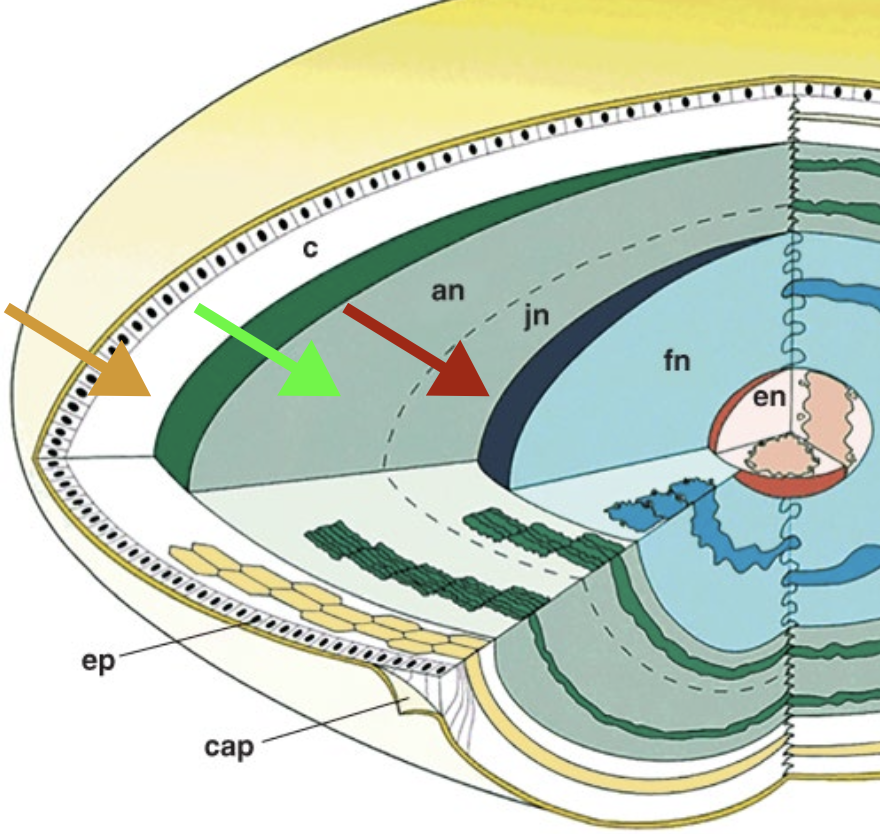
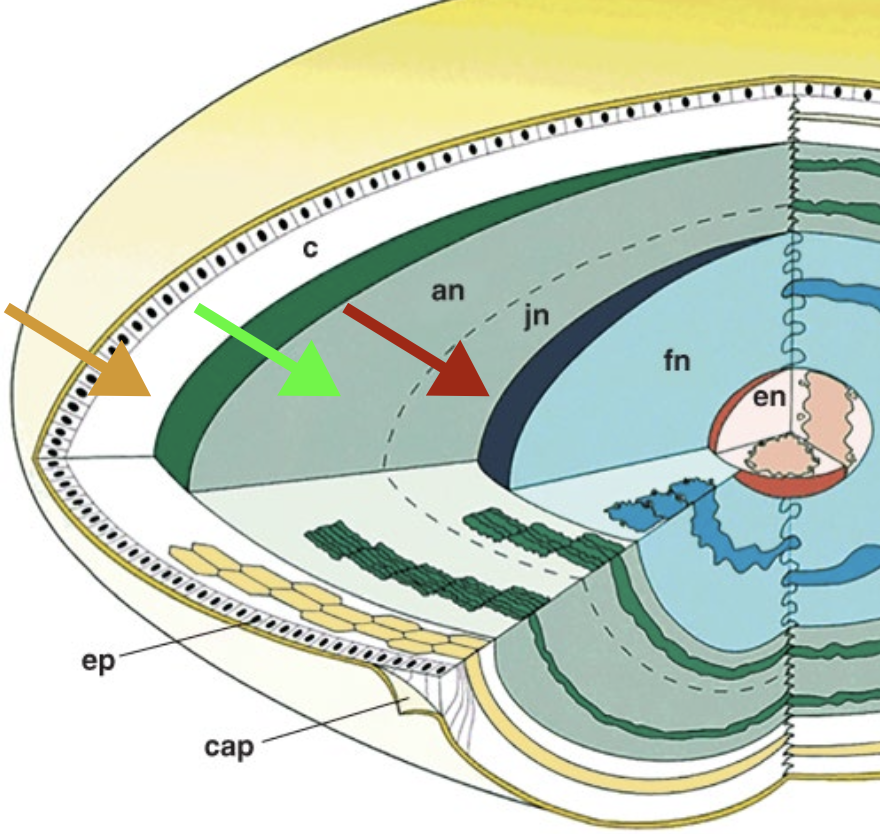
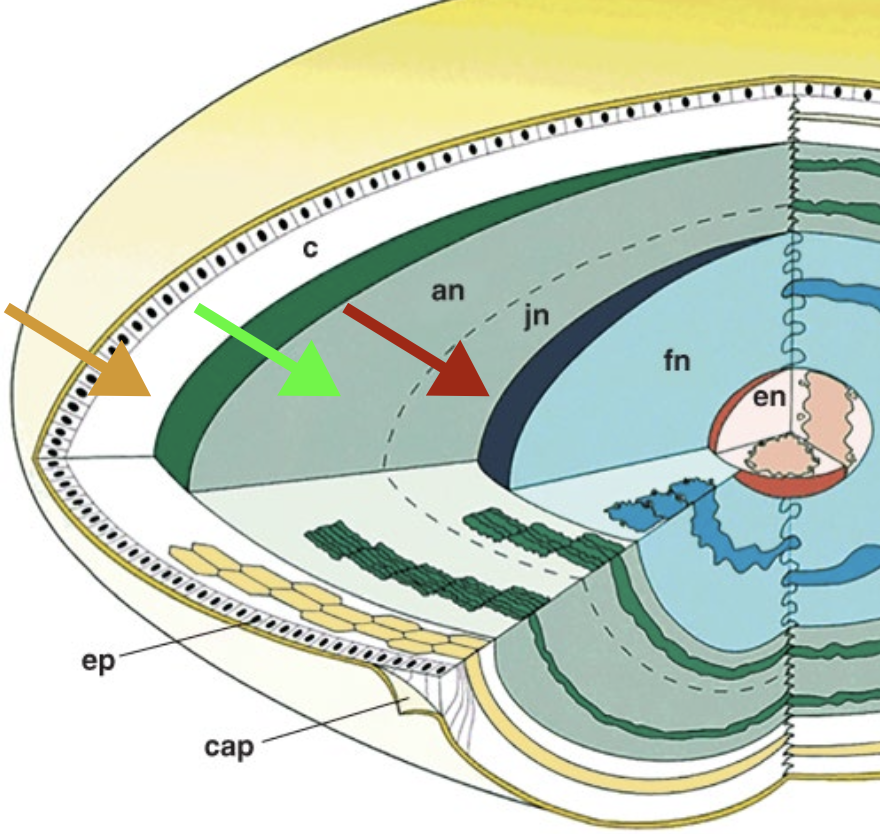
List the layer of the Choroid from (external to internal)
→ divided based on vessel size in each layer
Suprachoroid (suprachoroidal space)
Haller’s layer of large vessels
Sattler’s layer of medium vessels pigmented CT stromal matrix
Choriocapillaris
Bruch’s membrane
Where do the various layers of vessels of the choroid reside within?
pigmented CT stromal matrix
Choroid Layers
What is the Suprachoroid layer?
→ “potential space (2)” b/w the sclera (lies internal to the lamina fusca of the sclera) and choroid, where “could” travel through
it’s a thin pigmented CT layer
Choroid Layers
What is the Haller’s layer?
has large blood vessels + closest to the sclera (3)
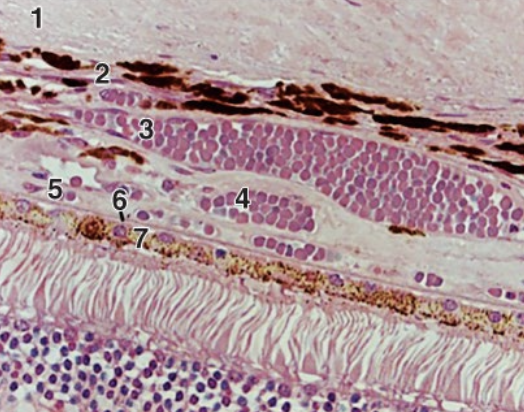
Choroid Layers
What is the Sattler’s layer?
has medium blood vessels + lies under the Haller’s layer, closer to the choriocapillaris (4)
Choroid Layers
What is the Choriocapillaris layer?
→ functional capillary bed of the choroid that supplies nutrients & O2 to the avascular outer retina (photoreceptors and RPE) (5)
has the largest capillaries in the body
these capillaries are fenestrated ONLY along the surface facing the retina (Bruch’s membrane), not on the side facing deeper choroidal layers
fenestrations allow for the rapid passage of nutrients and O2
Choroid Layers
What is the Bruch’s membrane?
→ a thin compound BM complex enveloping layers of collagen & elastin b/w the BM of the choriocapillaris and that of the RPE (6)
Choroid Layers
List the 5 laters of the Bruch’s membrane.
BM of choriocapillary endothelium
Outer collagenous layer
1 Discontinuous elastic layer
Inner collagenous layer
BM of RPE
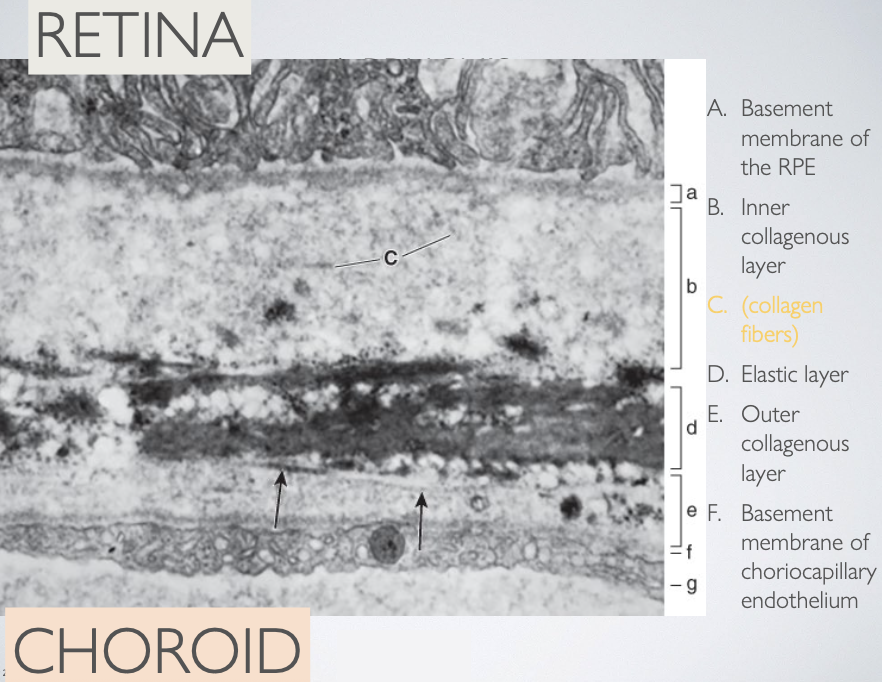
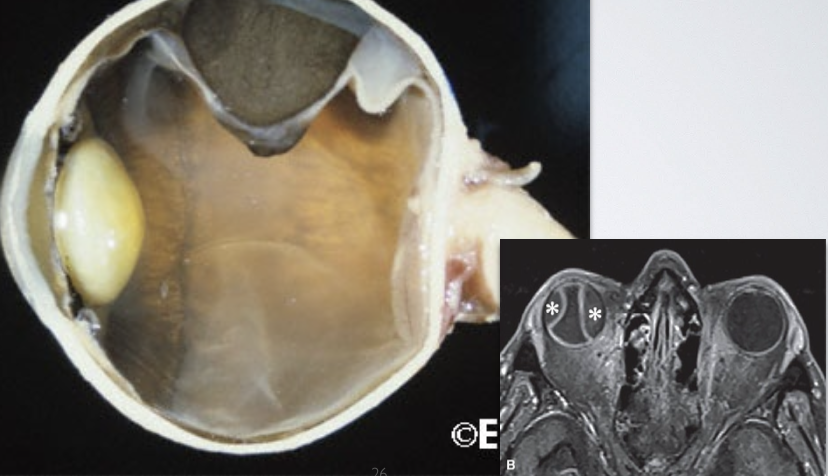
What role does Bruch’s membrane play when a tumour expands in the choroid?
due to its elastic layer, the Bruch’s membrane is very effective at preventing expanding masses (tumours) from breaking through the retina
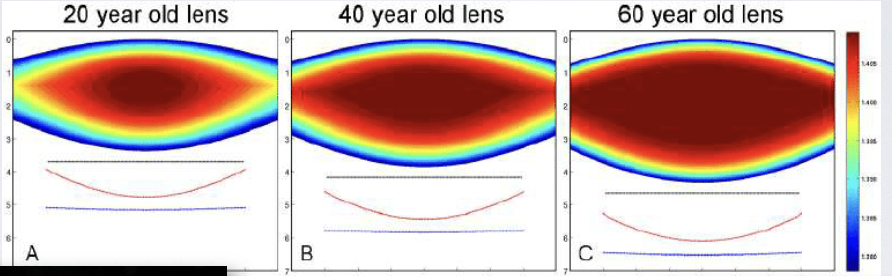
How does the lens size and function change with age? How does this compare to the cornea?
Cornea nearly reaches its adult diameter at birth
Lens diameter continues to increase throughout life → presbyopia → ability to accommodate decreases
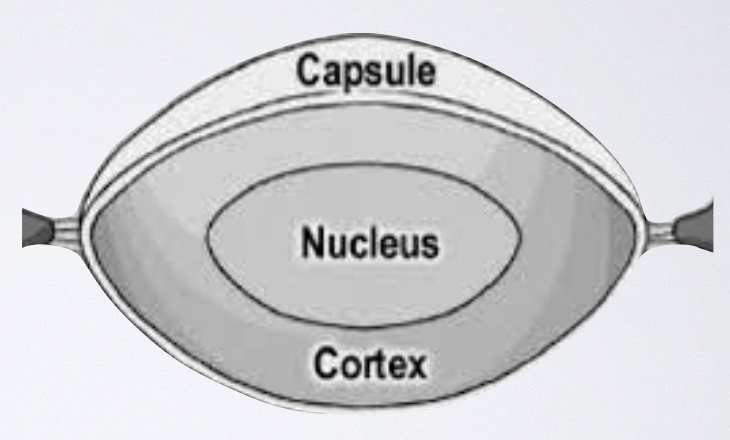
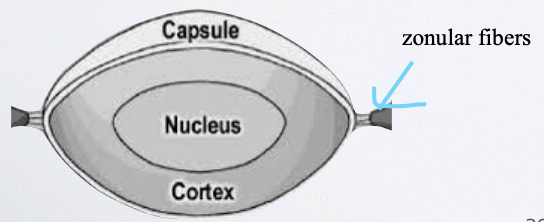
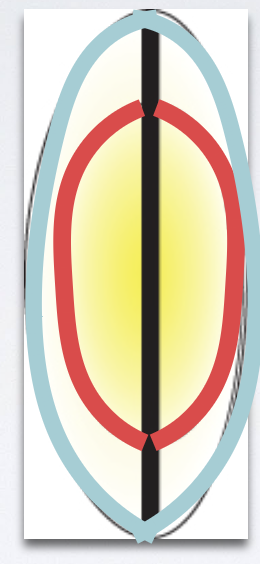
List the 4 major parts of the Lens.
Capsule (elastic ziplock bag)
Nucleus
Cortex
Epithelium
Parts of Lens
What is the len’s capsule?
shows elasticity but doesn’t have elastin
Zonular fibers attach to the capsule
What is the “beaten metal” (peau d’orange) appearance of the lens, and when is it seen?
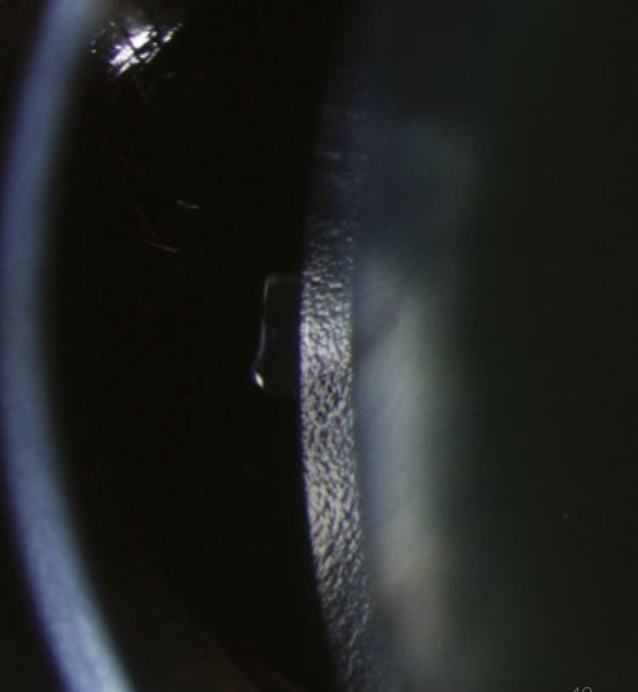
→ viewed with a slit-lamp using oblique illumination, the anterior capsule of the lens shows a “beaten metal” or “orange peel” (peau d’orange) appearance
occurs because the lens surface is not perfectly smooth, giving it a fine, textured reflection that resembles hammered metal
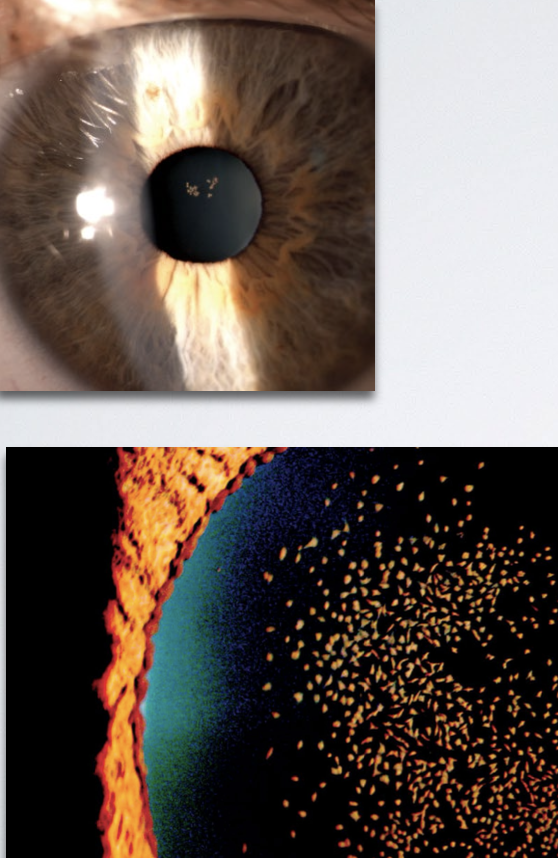
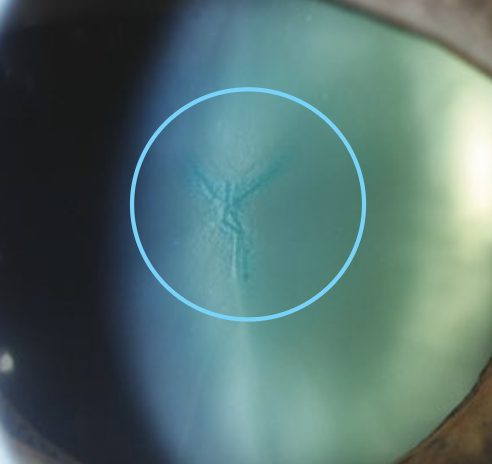
What are epicapsular stars?
Normal but uncommon variant
Starfish-shaped melanocytes can be seen on the anterior lens capsule
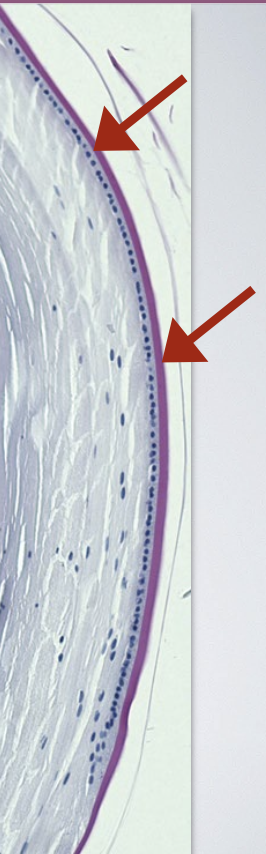
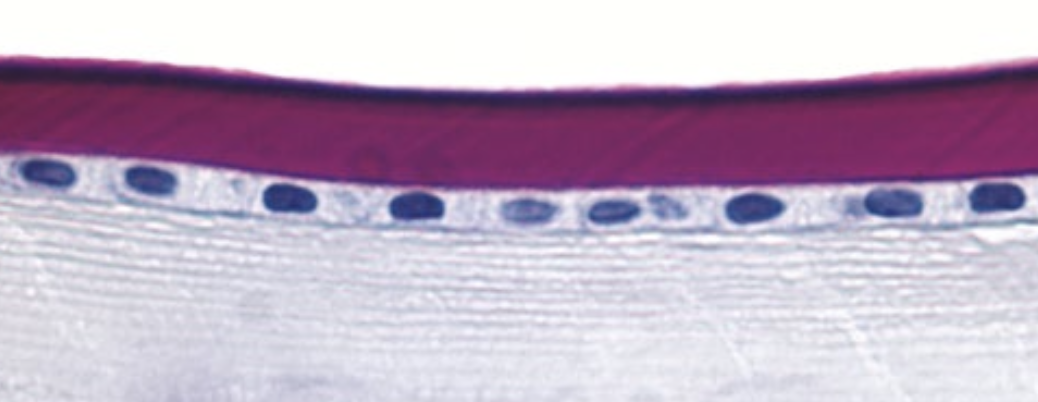
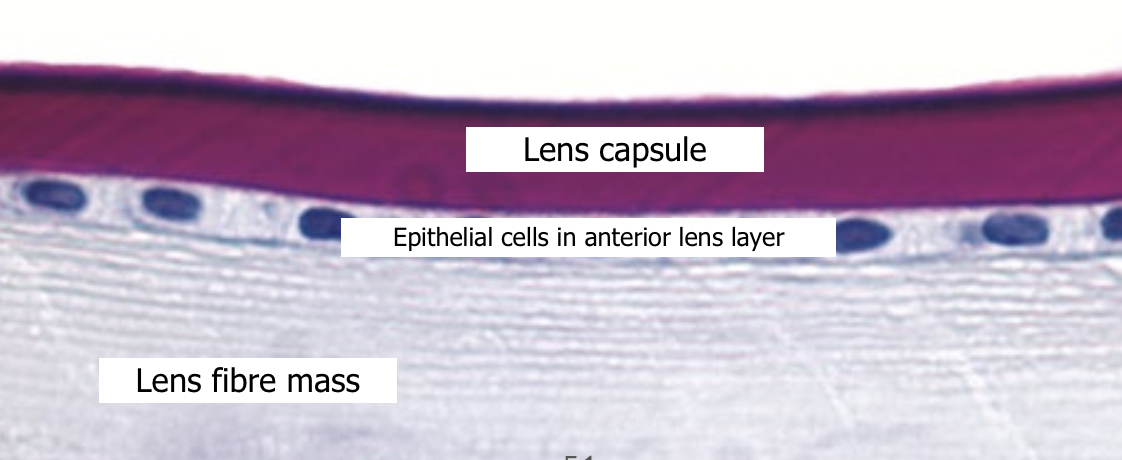
What are the key histological features of the lens capsule?
Lens capsule - true PAS-(+) BM
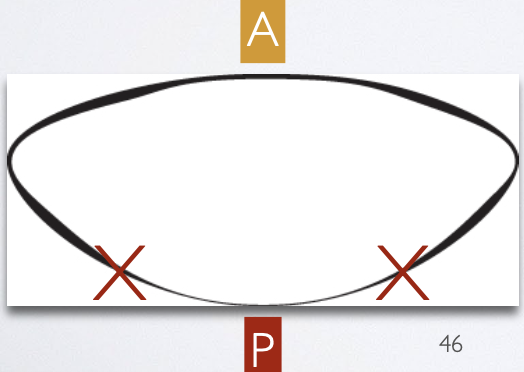
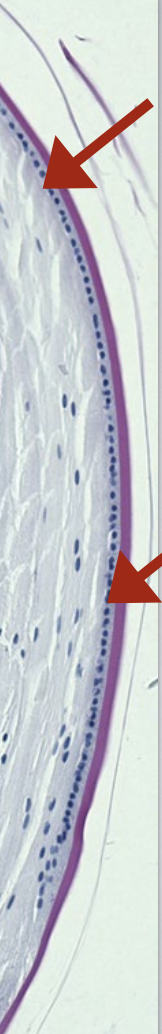
varies in thickness (thickest anteriorly & thinnest at the posterior pole)
has a very slow turnover (months to years)
made up of 2 lamina (layers) that can separate under certain disease conditions

Why is the slow renewal rate of the lens capsule clinically helpful?
allows the lens capsule to remain intact during cataract surgery, which helps prevent scarring and supports proper healing and lens replacement
Where is the lens epithelium located?
found just under the lens capsule, on the anterior ½ of the lens
no epithelium on the posterior surface of the lens
Anteriorly: capsule → epithelium → lens fibers
Posteriorly: capsule → lens fibers directly (no epithelium)
What are the key features and functions of the lens epithelium?
made of cuboidal epithelial cells
Apex - faces inward toward the lens fiber mass
Basal - rests on the lens capsule (its BM)
Cells at the anterior epithelium divide, and their daughter cells migrate to the equator, where they differentiate into new lens fibers
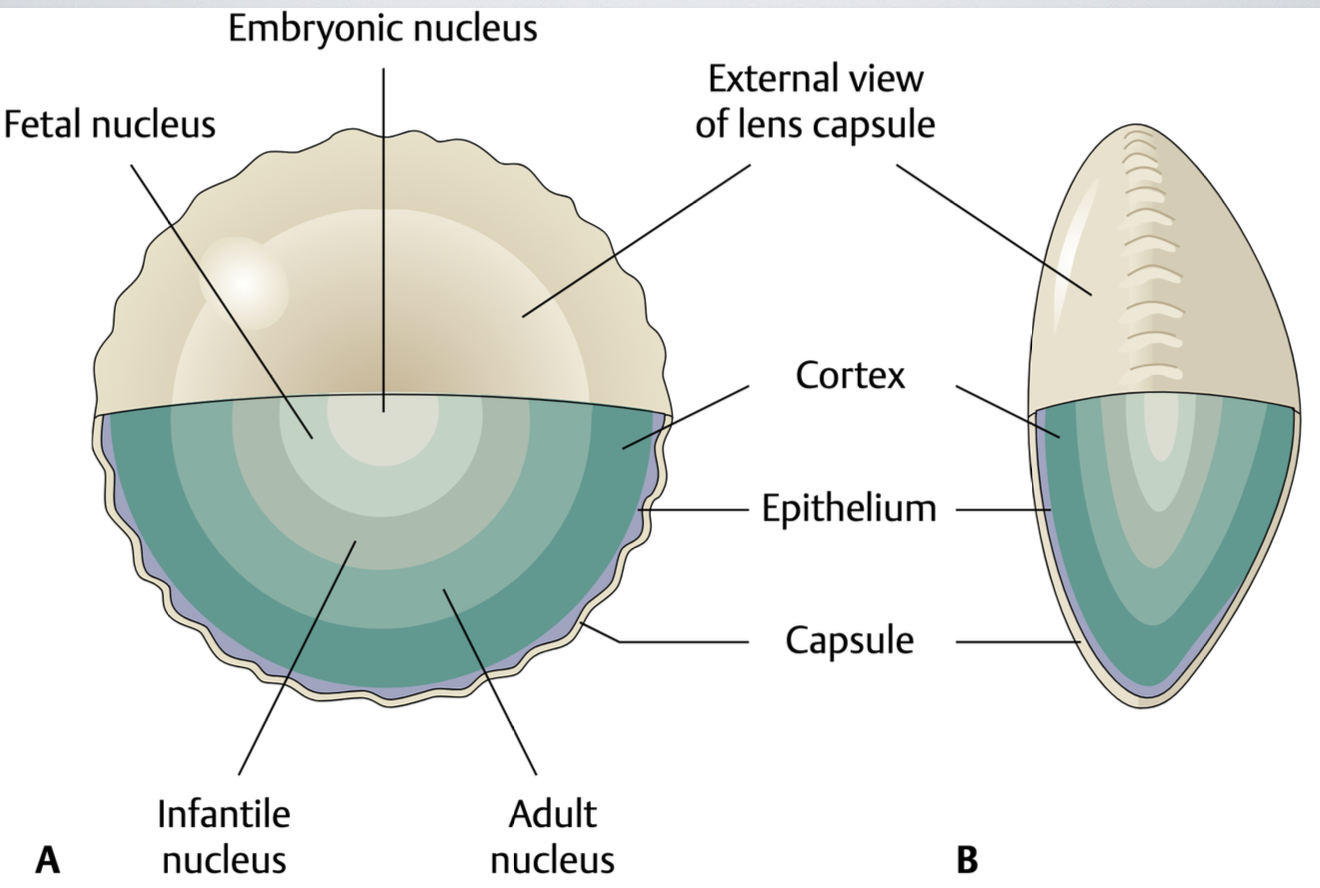
What are the 2 main parts of the lens mass? Mention the colouration difference between the two.
Lens nucleus (central region)
Lens cortex (outer region)
→ nucleus appears slightly yellow compared to the cortex, but both remain transparent
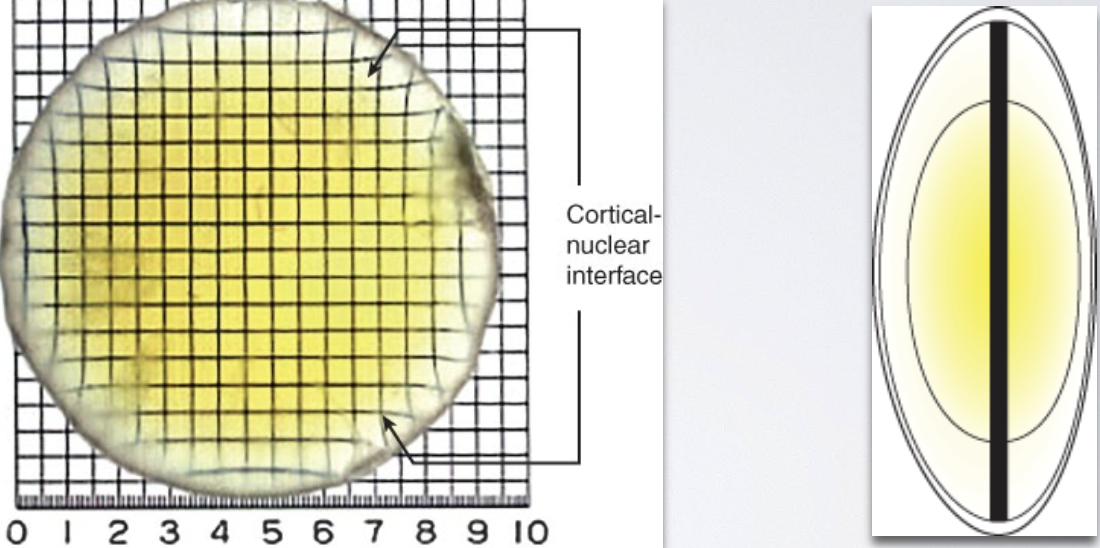
What are the optical properties of the lens nucleus vs the lens cortex?
Nucleus = acts like convergent (+) lens b/c it’s thicker in the center
Cortex = acts as a divergent (-) lens b/c it’s thicker in the edges
Describe the histology of the fibre mass (main bulk/body) of the lens.
made of thin, band-shaped, hexagonal lens fibers
Each lens fiber comes from 1 epithelial cell
New layers of fibers are continuously added to the outside of the existing fiber mass, but always under the anterior epithelium
What are the defined subsets of the lens nucleus, and how are they ordered from oldest to youngest?
Embryonic nucleus (oldest)
Fetal nucleus
Juvenile nucleus
Adult nucleus (youngest)
Subsets of Nucleus
Describe the Embryonic Nucleus.
“Represents the “first cells” of the lens”
formed from 1er lens fibers
Comes from epithelial cells that originally lined the posterior ½ of the lens during in-utero development
Once these cells differentiate into fibers, the posterior epithelial layer is completely used up → this is why no cuboidal epithelial cells are found on the posterior half of the mature lens
Subsets of Nucleus
Describe the Fetal Nucleus.
→ Fibers formed from anterior epithelial cells after embryonic nucleus but before birth
formed the same way as the embryonic nucleus
fetal nucleus continues to build upon the embryonic core
Describe the fibre attachment of the Fetus nucleus.
→ Fibers attach at the anterior & posterior poles
As more fibers form, attachment shifts from a single point to lines → forming Y-shaped sutures
Anterior Y suture: upright (↑)
Posterior Y suture: inverted (↓)
Y-Sutures are created when ends of lens fibers interdigitate (fit together)/interlock from opposite sides of the lens → ensure lens can be continuously reshaped during accommodation
Visibly seen in young adult lenses → become more complex with age as more fibers are added
Subsets of Nucleus
Describe the Juvenile Nucleus.
Formed b/w birth & puberty
“area” where cells begin to lose their nuclei as they mature into lens fibers
Subsets of Nucleus
Describe the Adult Nucleus.
Formed after puberty
“area” where lens cells have completely lost their nuclei
What is the Cortex of the lens?
Outermost lens layer
has the most recently formed fibers that still have nuclei
New fibers are constantly being added to the cortex & adult nucleus throughout life
List the 2 major roles of the zonules.
Hold the lens firmly in place
2. Work with the ciliary muscles to help the lens accommodate
**since it has 2 diff roles, they have little condensations
condensations - localized thickenings of zonular fibers
List the 3 major groups of the Zonules.
Anterior Packet
Posterior Packet
Vitreous (hyaloid) zonules
this is outside the “condensation”
What is the aqueous humour?
→ Clear nutritive fluid that supplies nutrients + removes wastes from the avascular cornea, lens, & TM
Secreted into the posterior chamber of the eye at ~2.5 μL/min in adults aged 20 to 83 years
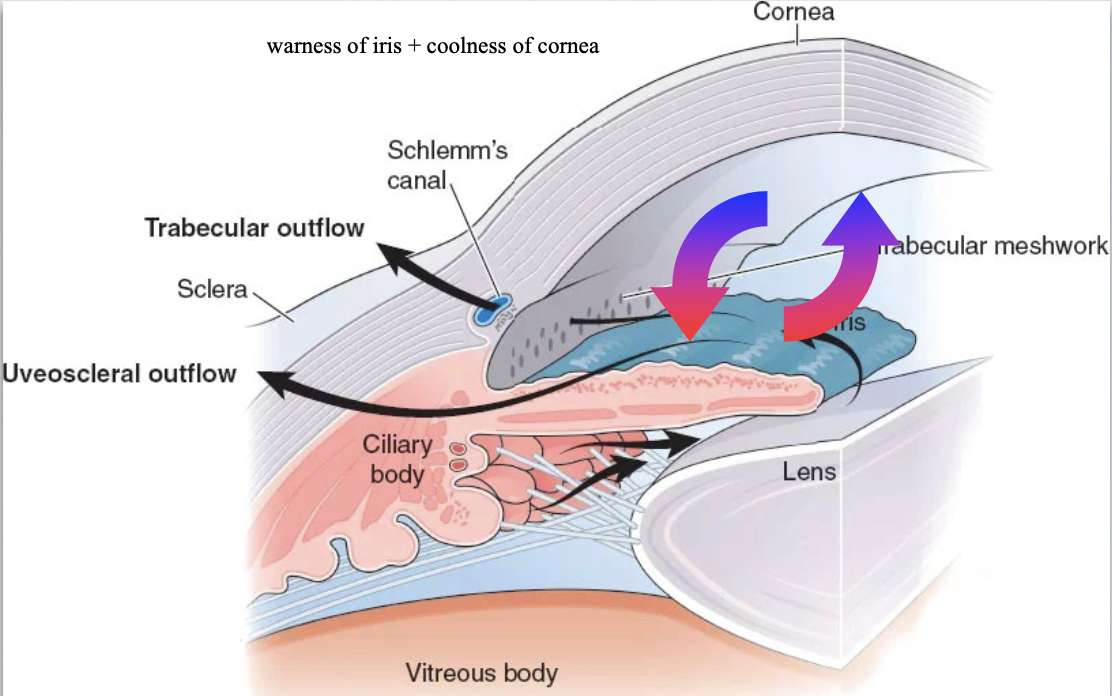
Describe the flow pathway of Aq humor in the anterior chamber.
Production - by the ciliary body in the posterior chamber
Movement to Anterior Chamber:
flows through the pupil into the anterior chamber
can’t diffuse through the iris b/c the posterior layer is non-permeable
Circulation (Convection Current):
In the anterior chamber, the aq humor circulates due to a temperature difference:
Warm iris - b/c it’s closer to body temp (vascular)
Cool cornea - b/c it's exposed to air
Temp difference creates a convection current
Rises along the warm surface of the iris
Falls along the cooler inner surface of the cornea
During circulation, it exchanges nutrients and waste products with surrounding tissues
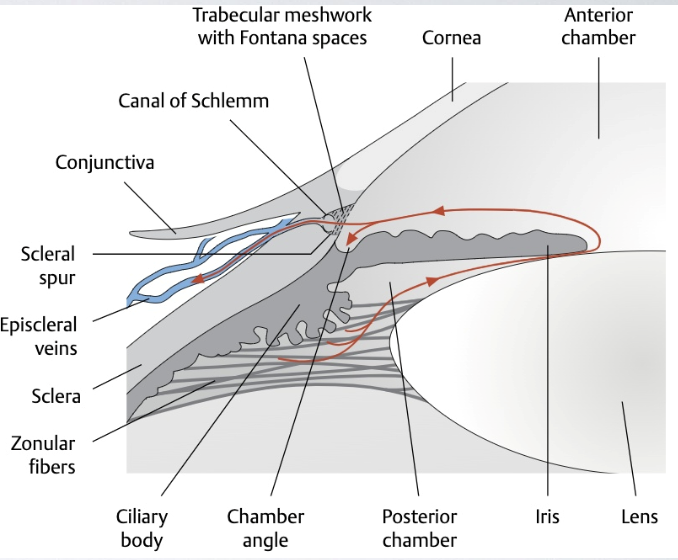
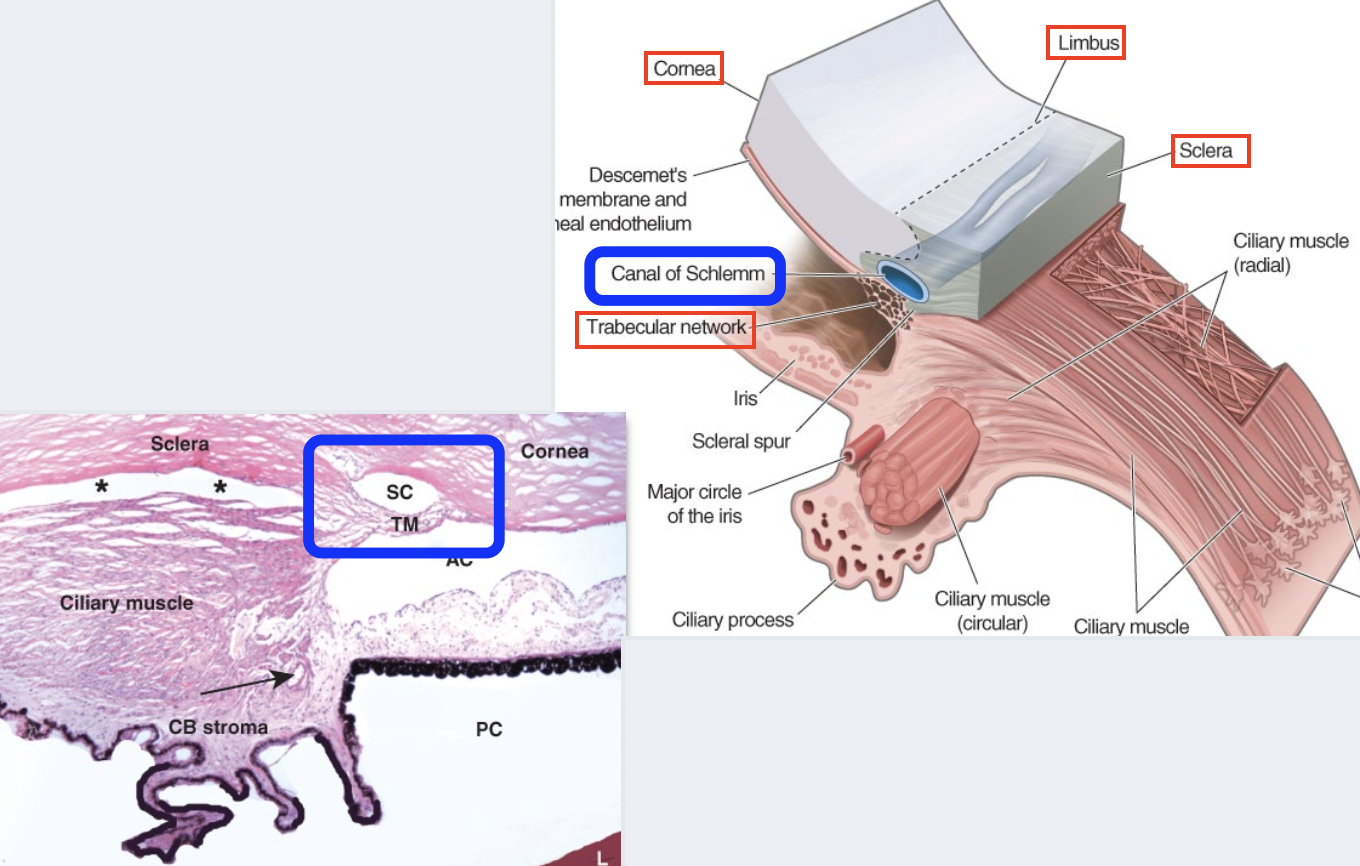
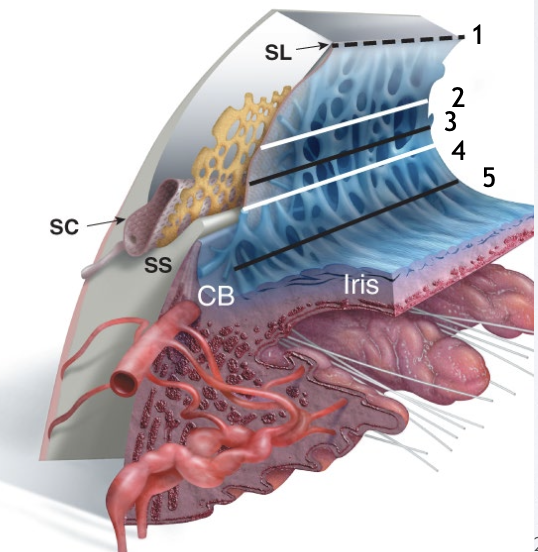
Aqueous humor leaves the eye through 2 main pathways. Describe them.
1. Trabecular (Conventional) Outflow
major pathway (aka “Schlemm’s canal pathway”)
Aq drains through the TM→ Schlemm’s canal → episcleral venous system
Pressure-dependent system
2. Uveoscleral (Unconventional) Outflow
minor pathway
Aq passes into the → CT of the ciliary body band near the root of the iris → percolates through the connective fascicles of the ciliary muscle → supraciliary space
exits through the sclera
OR passes through emissarial channels
Less pressure-dependent (b/c it uses spaces)
What determines whether aq humor will enter the trabecular outflow pathway or the uveoscleral pathway?
Position of the scleral spur
If aq enters the angle above the scleral spur → Trabecular outflow pathway
If aq enters the angle below the scleral spur → Uveoscleral pathway
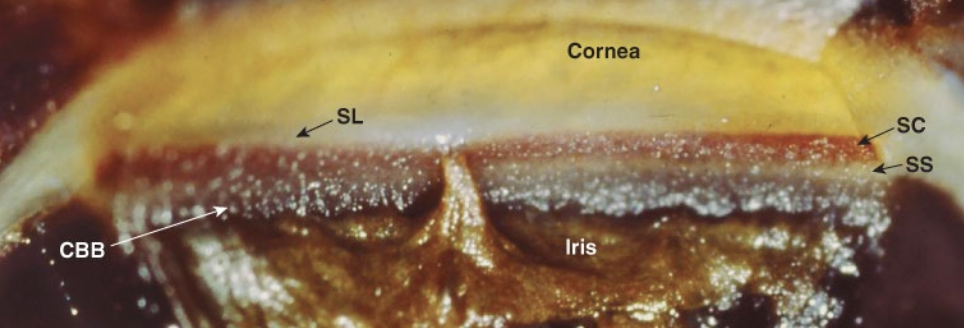
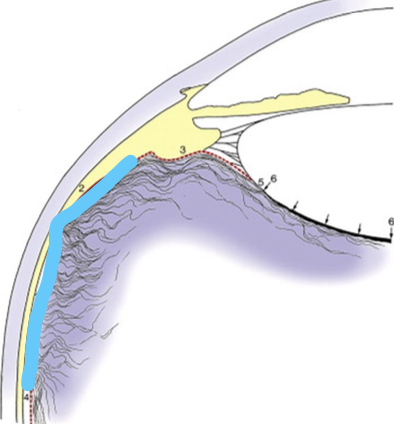
What is the “angle of the eye”?
“Iridocorneal angle”
location where the iris, ciliary body, cornea & sclera meet
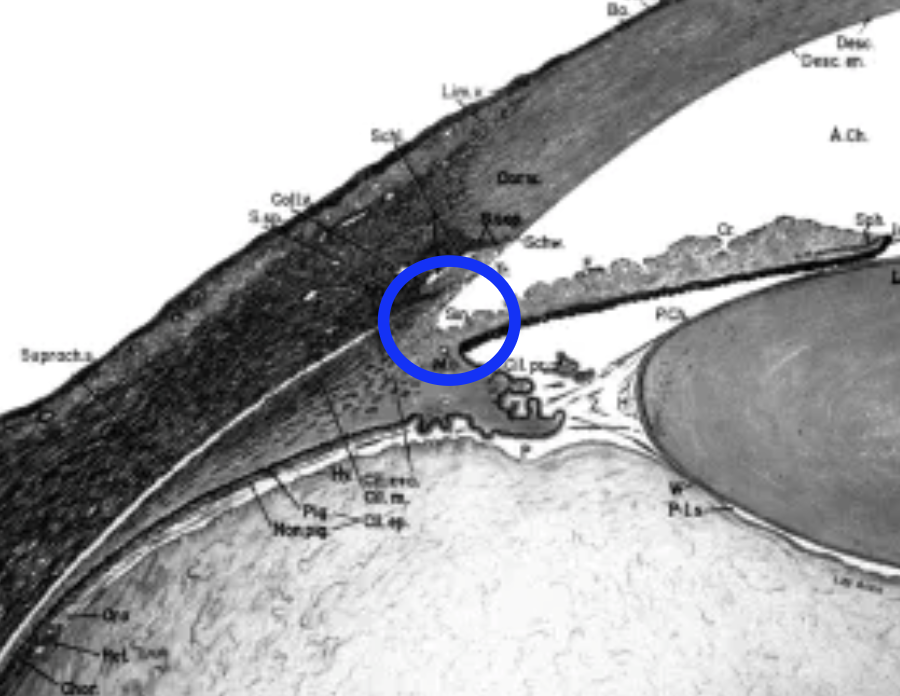
What’s found in the “angle of the eye”?
Root of the iris
Ciliary body and band
Scleral spur
Schlemm’s Canal
Schwalbe’s line
TM
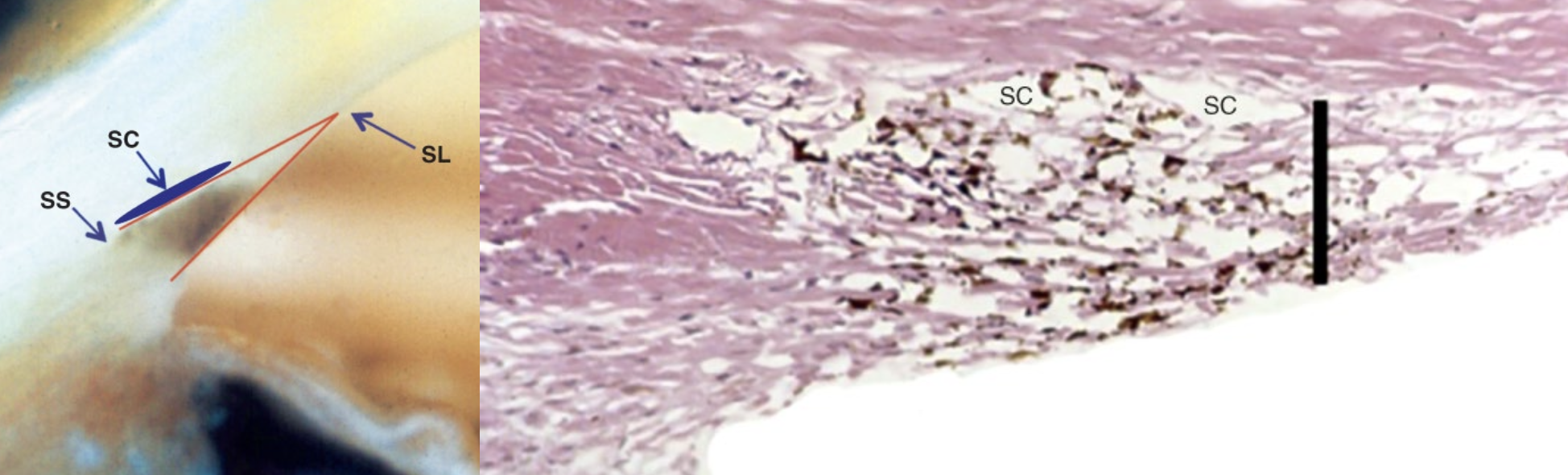
Where do the TM & Schlemm canal reside?
within the internal scleral sulcus
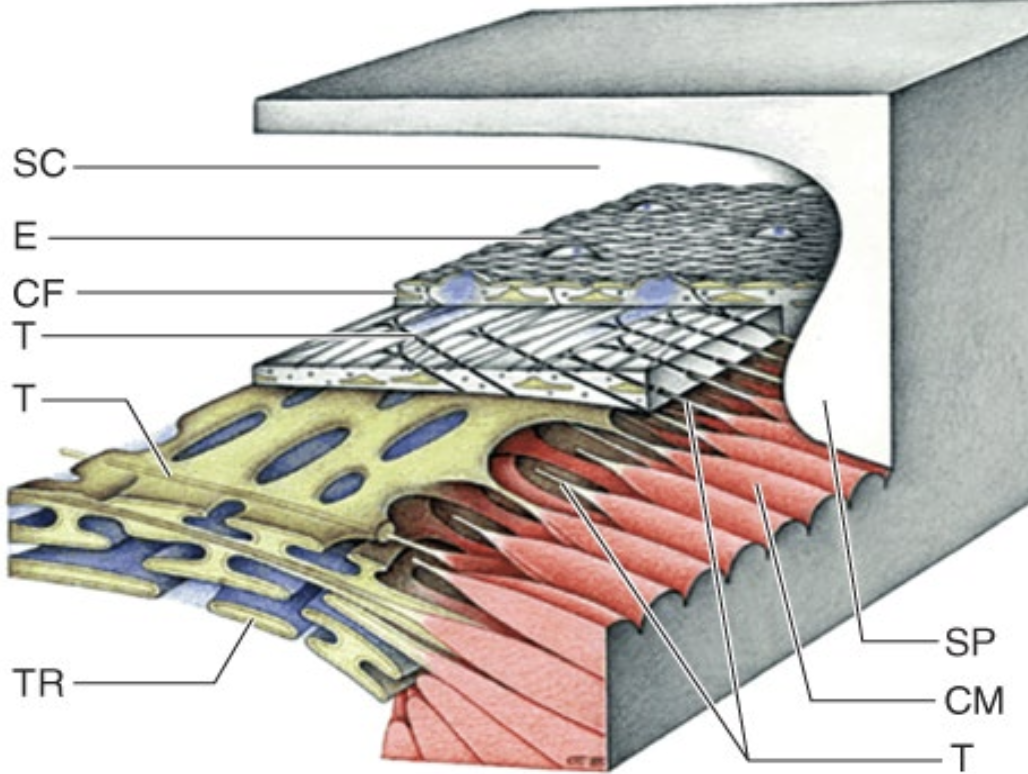
What is the Trabecular Meshwork?
→ triangular wedge of avascular tissue that encircles the anterior chamber angle around the entire eye
Apex - attaches to the most posterior lamellae of the corneal stroma + Schwalbe’s line
Schwalbe’s Line: peripheral edge of Descemet’s membrane
Base - attaches to the sclera + stromas of the ciliary body & iris root
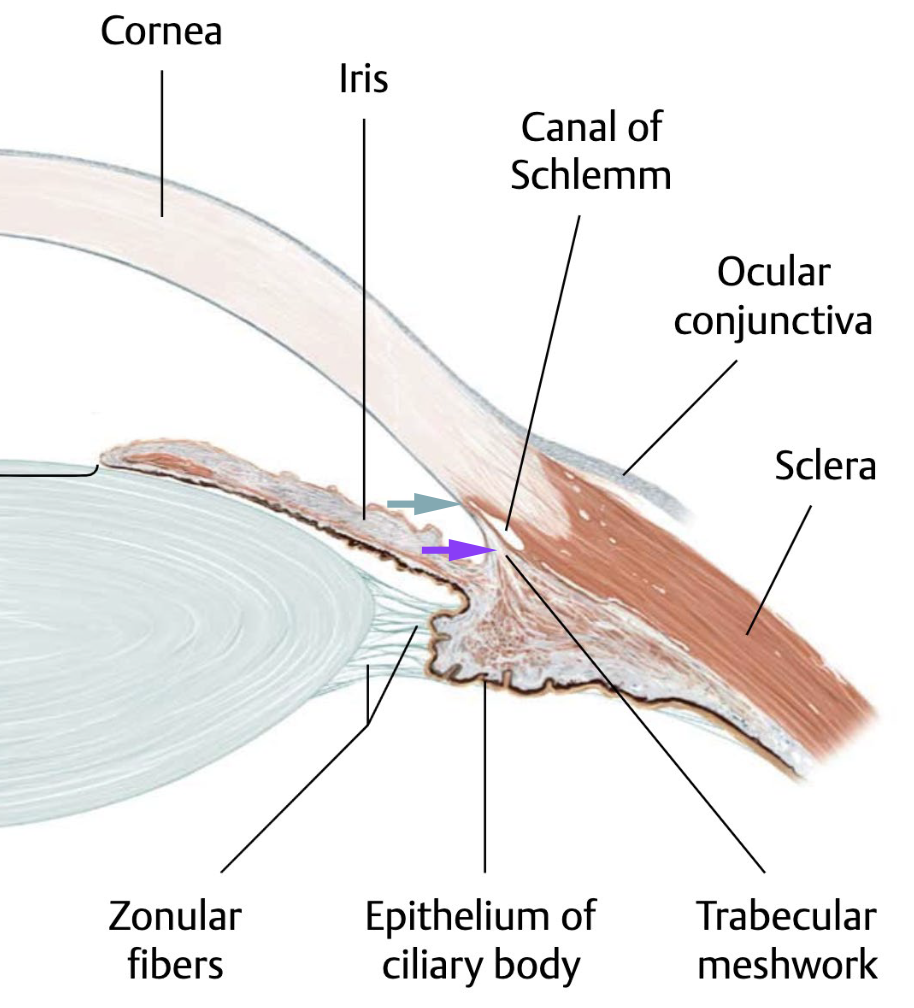
What is the Scleral spur?
a “lip” of sclera that projects into the base of the TM

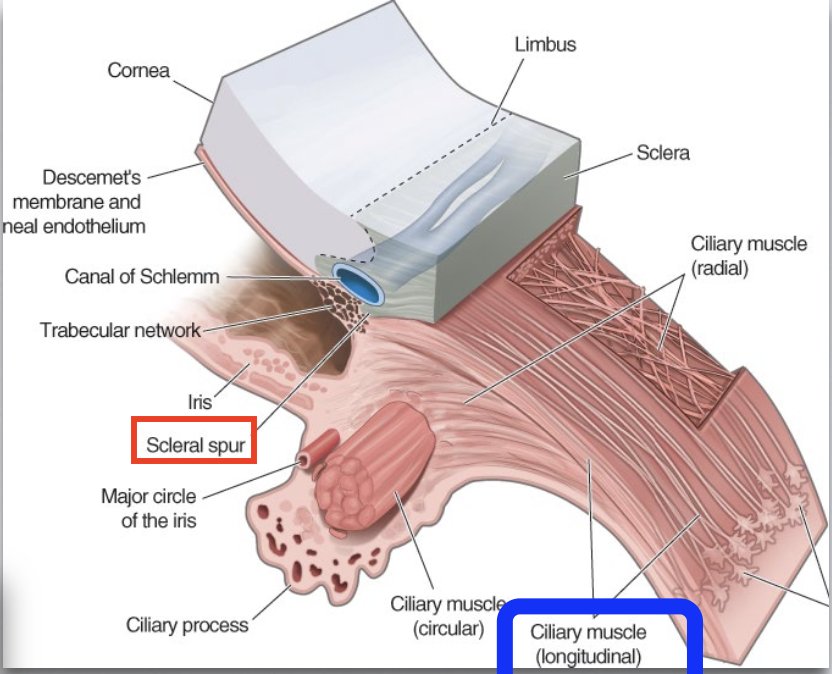
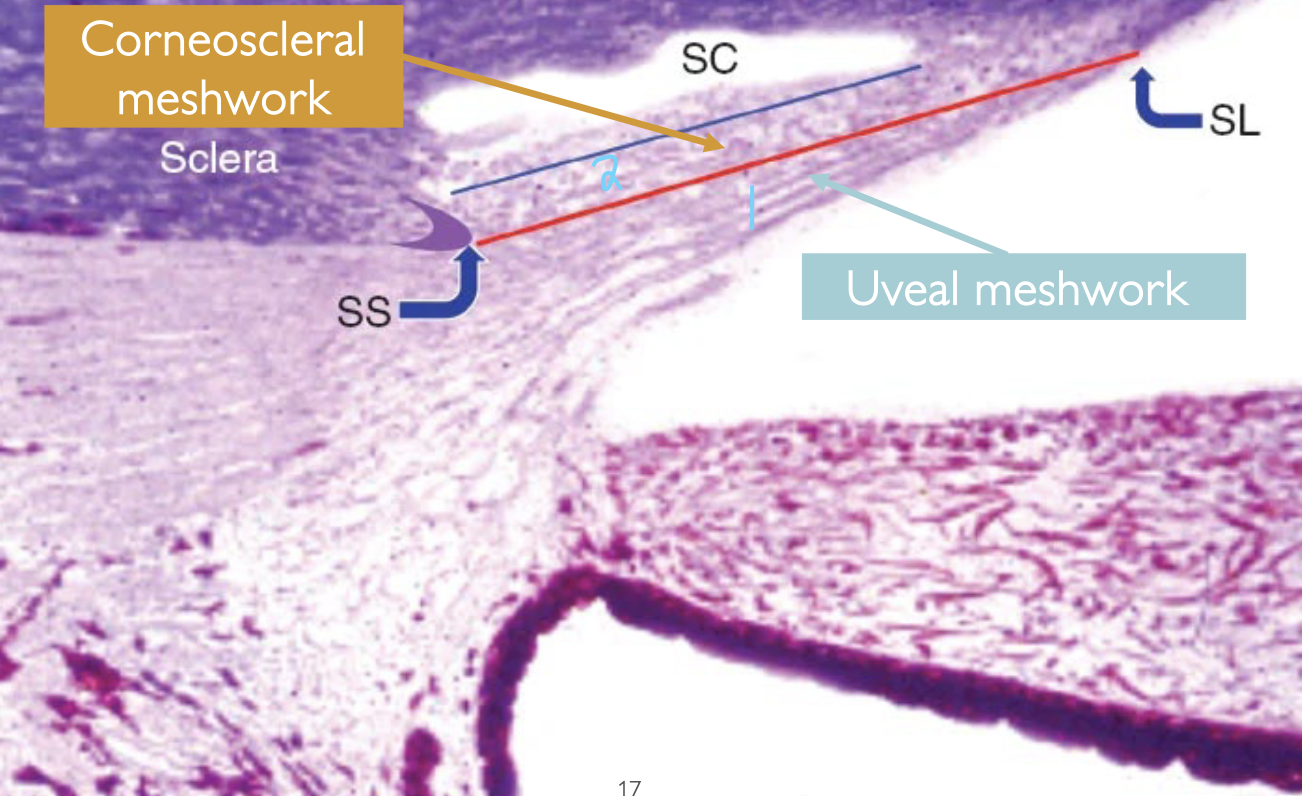
An imaginary line drawn from the scleral spur → Schwalbe’s line which separates the TM into 2 of its major parts (2 triangles). Describe these major parts.
1) Uveal meshwork
TM is closer to the anterior chamber
extends from Schwalbe’s line to the stroma of the ciliary body & iris (i.e., anterior uvea)
has large gaps b/w its trabeculae → allow aq humor to easily pass through this region first
2) Corneoscleral meshwork
TM closer to Schlemm’s canal
extends from Schwalbe’s line + most posterior lamellae of the corneal stroma to the scleral spur
has smaller gaps → provides more resistance to aq outflow as fluid moves toward Schlemm’s canal
In the TM, what happens to filtration as the spaces get progressively narrower (from Uveal and Corneoscleral meshwork)?
Filtration is NOT affected
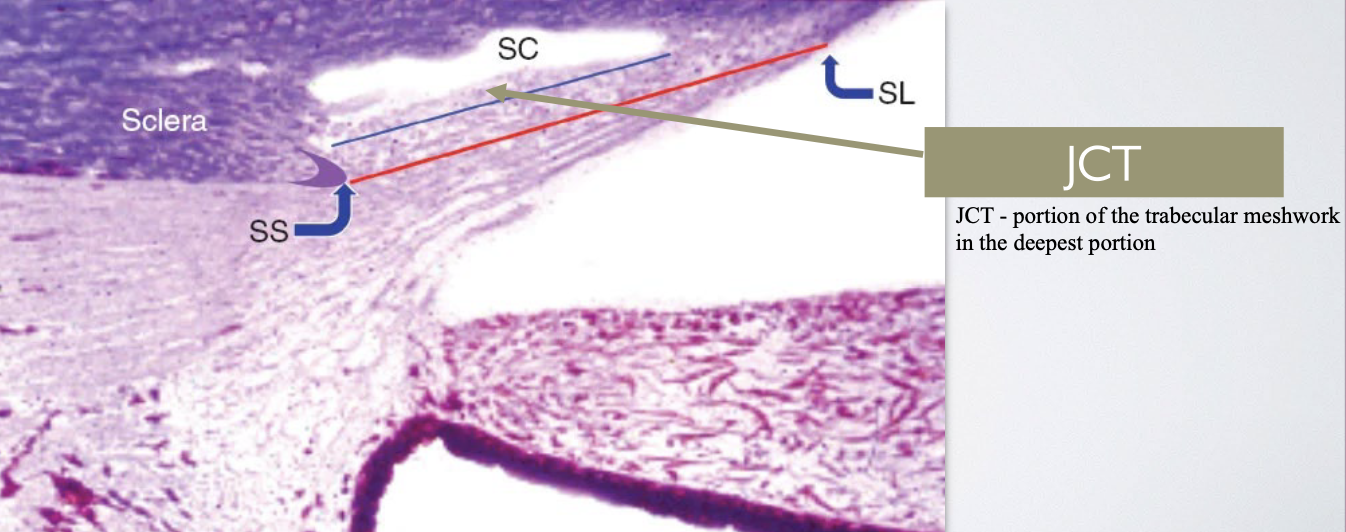
What is the Juxtacanalicular Connective Tissue (JCT) and where is it located?
→ aka Cribriform meshwork (has lots of holes)
narrow strip of loose, cellular CT that represents the deepest TM portion
Location: b/w the deepest trabeculae of the corneoscleral meshwork & Schlemm’s canal
What is the Schlemm’s Canal?
→ endothelial cell–lined channel that runs around the eye, parallel to the limbus
Location: junction of the cornea & sclera, near the TM
Function: receives aq humor from the trabecular outflow pathway, where it then drains into episcleral veins to maintain IOP
Recall Slide: List the main locations of the Aq Humor Outflow Pathways in order.
Ciliary body (production)
Schlemm’s canal (Conventional / Trabecular outflow)
Uveoscleral outflow (Unconventional pathway)
What is the role of some tendons longitudinal bundle of the ciliary body?
Attaches to the scleral spur ( “lip” of sclera)
Contracts & pulls the scleral spur down and back
This opens up the TM, enlarging its pores
Allows more aq humor to exit
↓ IOP
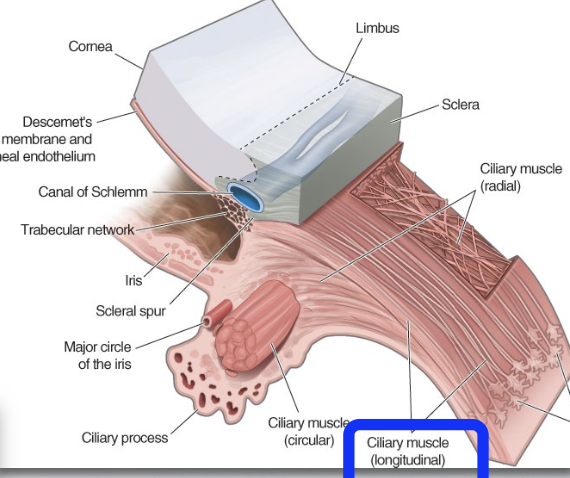
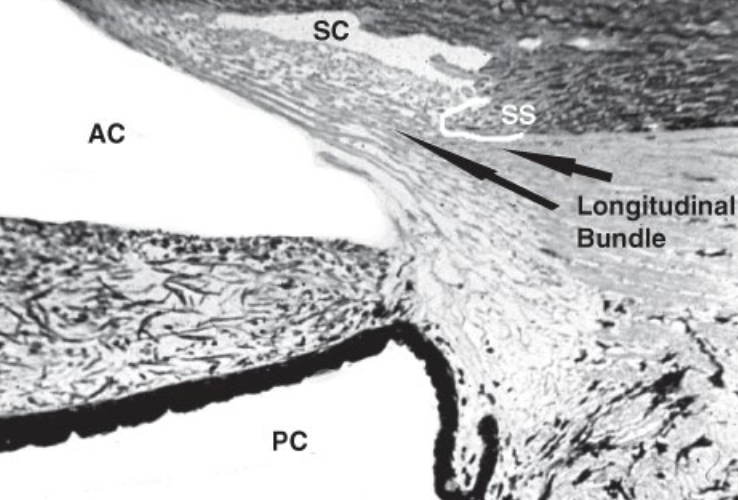
What is the role of the additional tendons (elastic connecting fibrils) from the longitudinal bundle of the ciliary body?
→ extend into the TM forming the cribriform plexus
hold the Schlemm’s canal open to prevent it from collapsing, when IOP rises
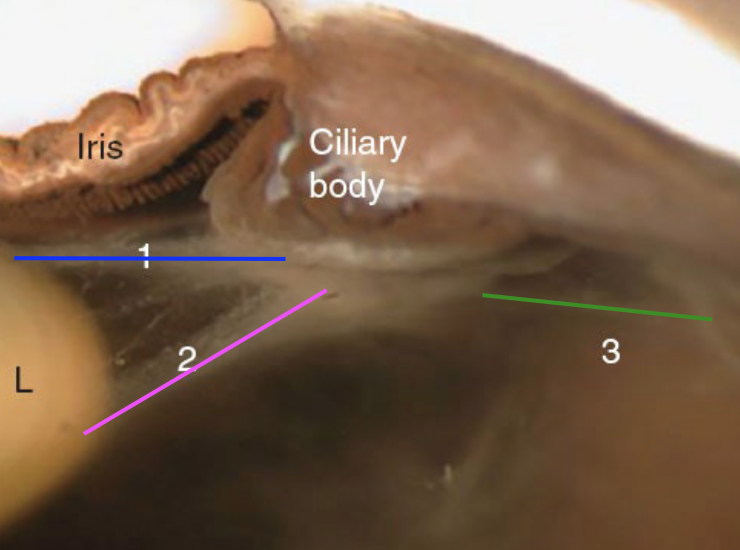
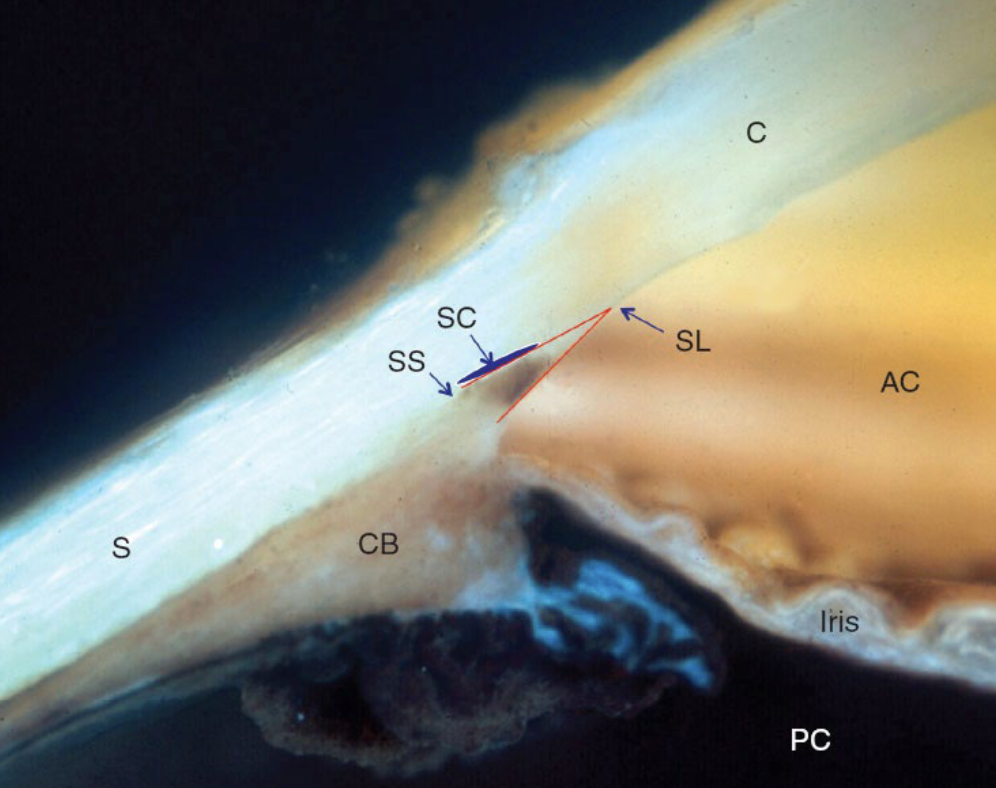
Gonioscopy
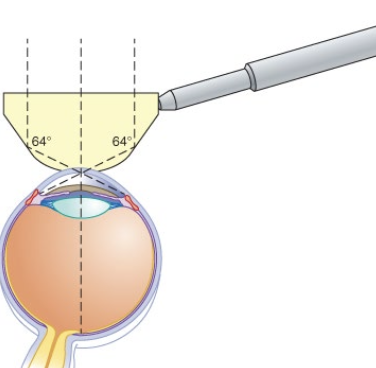
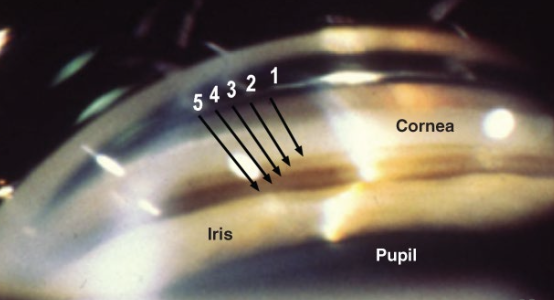
What is gonioscopy and why is it used?
→ allows clinicians to see around the cornea to view the angle tissues of the eye with goniolens or gonioprism
b/c angle structures can’t be seen directly with a slit-lamp b/c they’re covered by the perilimbal sclera
Gonioscopy
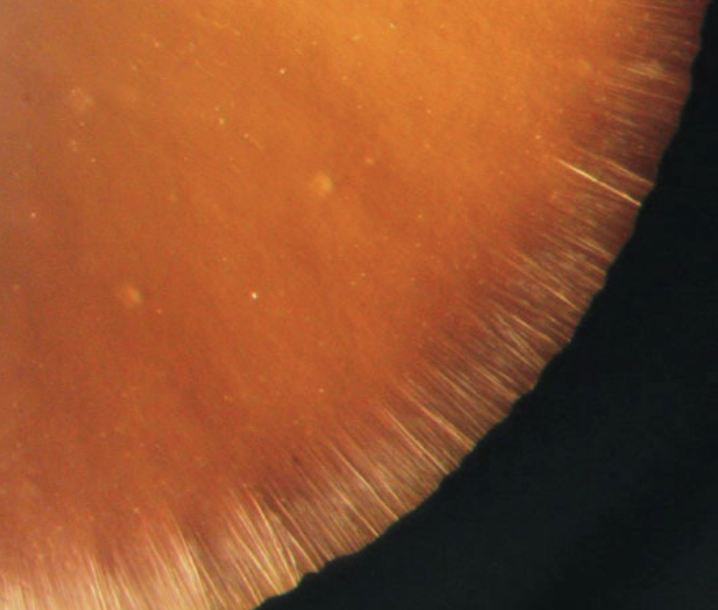
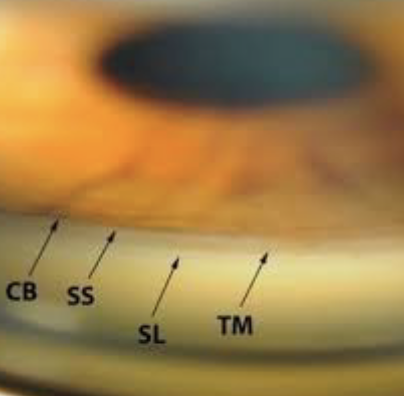
Where is pigmentation found in older normal eyes, and how does it appear during gonioscopy?
found in the posterior portion of the TM that drains directly into Schlemm’s canal
appears as an “extra” pigmented band in older eyes
Gonioscopy
In a gonioscopic (macrophotograph) view of the angle of the eye, what five lines or structures can be seen?
Schwalbe’s line
Anterior (non-flow) meshwork - “beginning of triangle,” less flow
Posterior (flow) meshwork - “base of triangle,” more flow (wider area)
Scleral spur
Ciliary body band
Vitreous Body
Describe the characteristics of the Vitreous body.
occupies ~75–80% of the eye’s volume
gel-like structure made of:
≈98% water
Collagen fibers
Hyaluronic acid
Highly viscous and elastic → maintains eye shape
Vitreous Body
What are the main roles of the Vitreous body?
Supports the shape of the eyeball
Acts like a “shock absorber” to protect the retina
A pathway for light to reach the retina without distortion
Vitreous Body
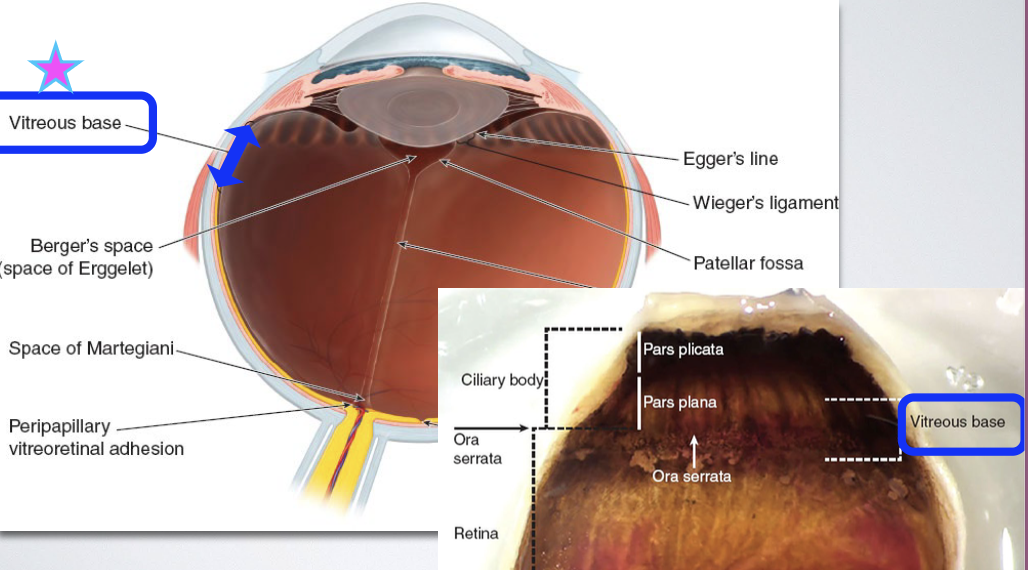
What are the anterior, peripheral, and posterior boundaries of the vitreous body?
Anterior boundary:
back surface of the lens
Retrozenular portion of the posterior chamber
Peripheral & posterior boundaries:
Pars plana of the ciliary body
Optic disc
Retina
→ All surfaces in contact with the vitreous are BM
Vitreous Body
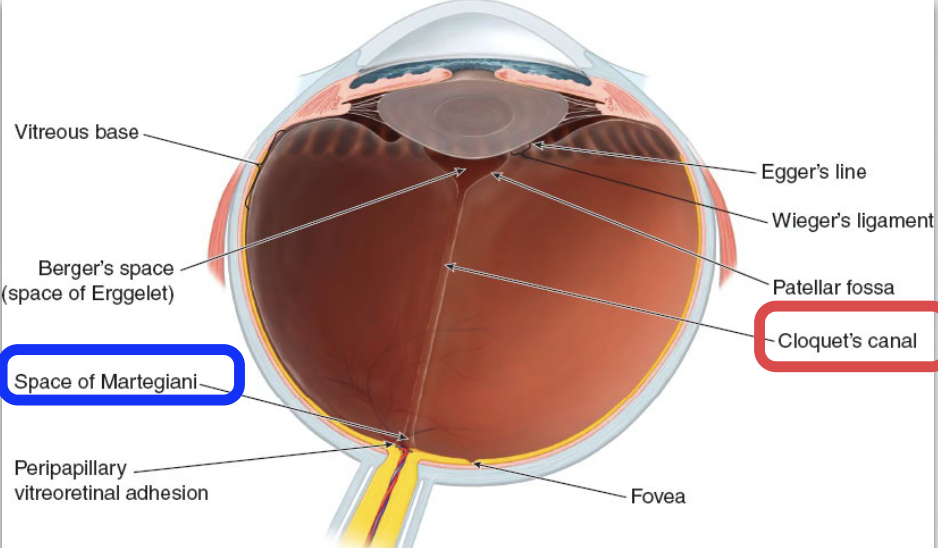
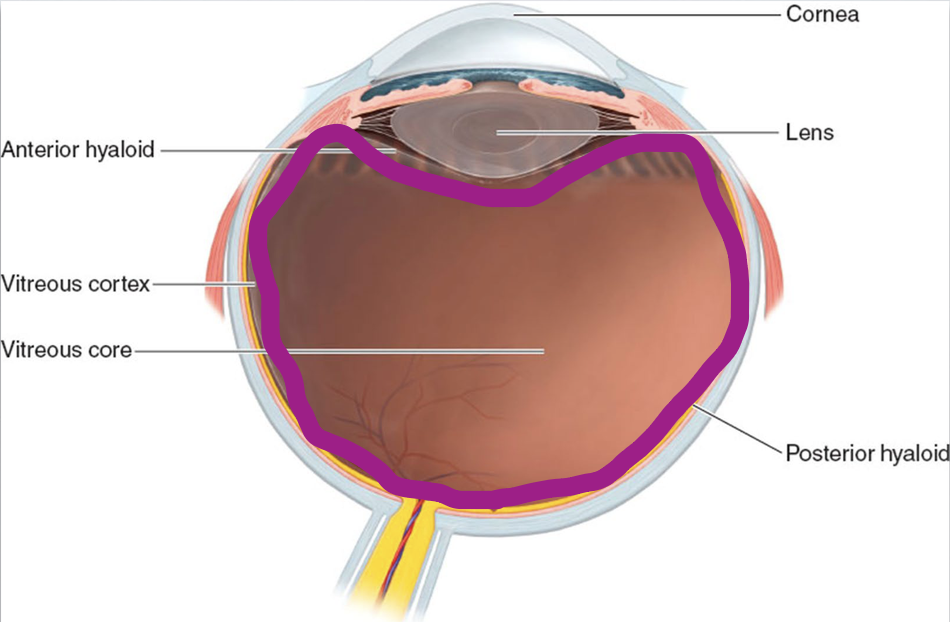
What are the zones of the vitreous body and how are they organized?
→ organized based on density
Outer zone: Vitreous cortex (hyaloid surface/membrane) - important
Intermediate zone: lies just inside the cortex, surrounding the central canal
Center zone: occupied by Cloquet’s canal (the central, less dense core)
Vitreous Face
The surface of the vitreous body (hyaloid surface/membrane) is divided into anterior and posterior “faces”.
What do these faces face?
What do they contain?
Anterior face - Faces the lens and ciliary body
Posterior face- Lies against the retina
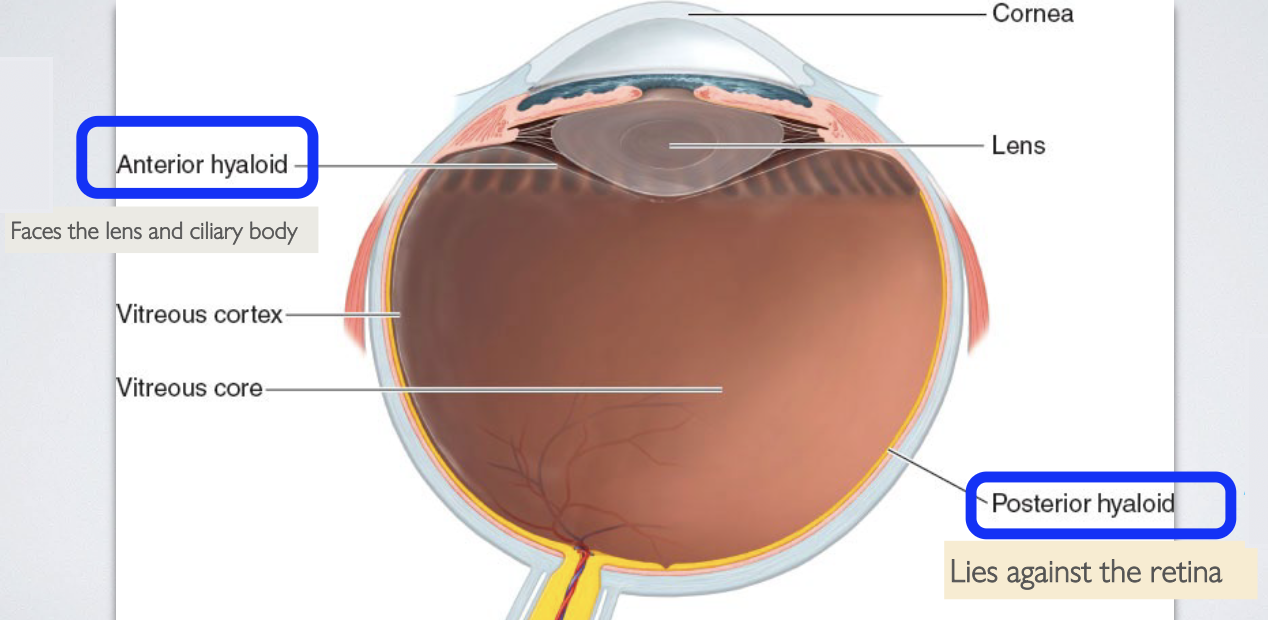
Note: These “faces” are not separate membranes; they’re descriptive terms for the orientation of the vitreous body.
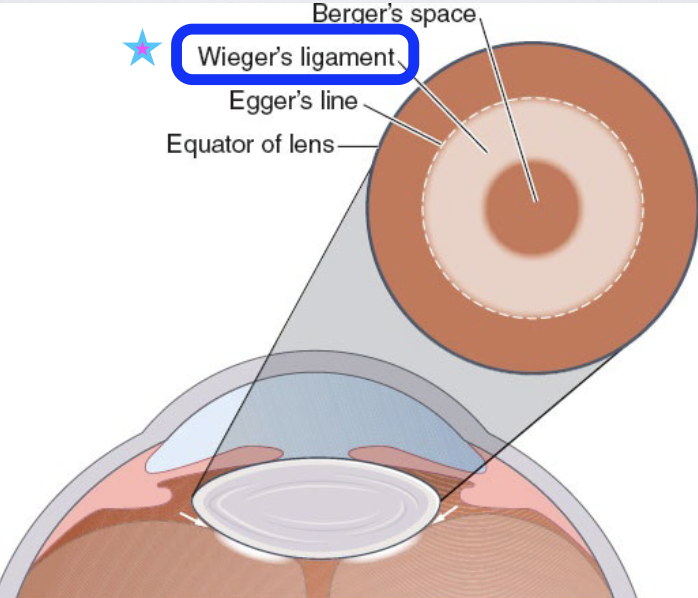
What structures does the Anterior face of the vitreous contain?
patellar fossa — an indentation in which the lens sits
What is the retrolental space (of Berger) and why is it clinically important?
→ “potential space” b/w the posterior lens capsule & patellar fossa
provides space for cataract surgery
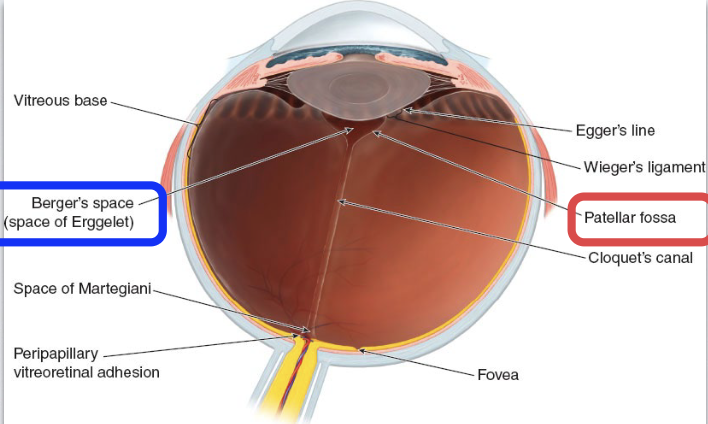
Vitreous Face
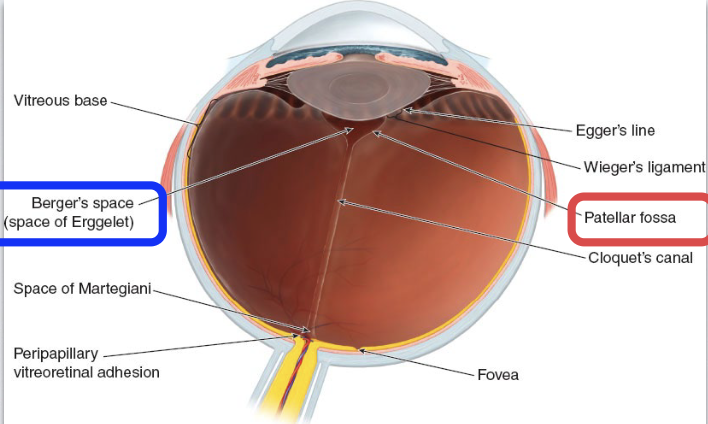
Where are the strongest attachments of the vitreous face, and what is their order of strength?
Strongest attachment:
Vitreous base at the ora serrata (most important)
Other attachments, in ↓ strength:
Posterior lens
Optic disc
Macula
Retinal vessels
Vitreous Face
What is the vitreous base and where is it located?
→ region where the anterior and posterior vitreous faces meet
overlies the ora serrata
Recall: it’s the strongest attachment
Vitreous Face
What is the main attachment of the anterior vitreous face, and how does it change with age?
Hyaloideocapsular ligament (of Weiger)
connects the anterior vitreous face to the posterior lens capsule
this “bond” ↓ with age → potential vitreous-related issues in older individuals
associated with Berger’s space and Egger’s line
What is Cloquet’s canal, and where does it begin and end?
→ central channel within the vitreous body
aka "hyaloid channel or retrolental tract
Starts at: Berger’s space near the lens
Ends at: Area of Martegiani - a funnel-shaped space at the optic nerve head that continues with the canal