The role of nutrition and nutritional supplements in vulnerable elderly patients
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
What is malnutrition
a state of nutrition in which a deficiency or excess of energy, protein and other nutrients causing adverse effects on tissue/body form and fucntion
Malnutriotion symptoms
Weight loss
Low BMI
Reduced food intake
Disease burden
reduced metabolic regulation
cachexia
loss of skeletal muscle mass with or without loss of fat mass
non-reversible by conventional nutritional support
Cachexia symptoms
weight loss/ low BMI
decreased muscle strength
abnormal biochem
fatigue
anorexia
Sarcopenia
reduction in skeletal muscle mass and function
part of aging process
consider muscle mass, muscle strength, physical performance
Sarcopenia symptoms
loss of mobility
reduced muscle function
reduced physical performance
Frailty
Increased vulnerability for developing increased dependency and or mortality when exposed to a stressor
PINCH ME
P ain IN fection C onstipation H ydration M edication E nvironmental
Risk factors for malnutrition
old age > 65years
care home/ nursing home
complex health needs e.g. Learning difficulties or mental health disorders
Chronic conditions e.g. diabetes, kidney disease, chronic lung disease
dementia, cancer
drugs, alcohol
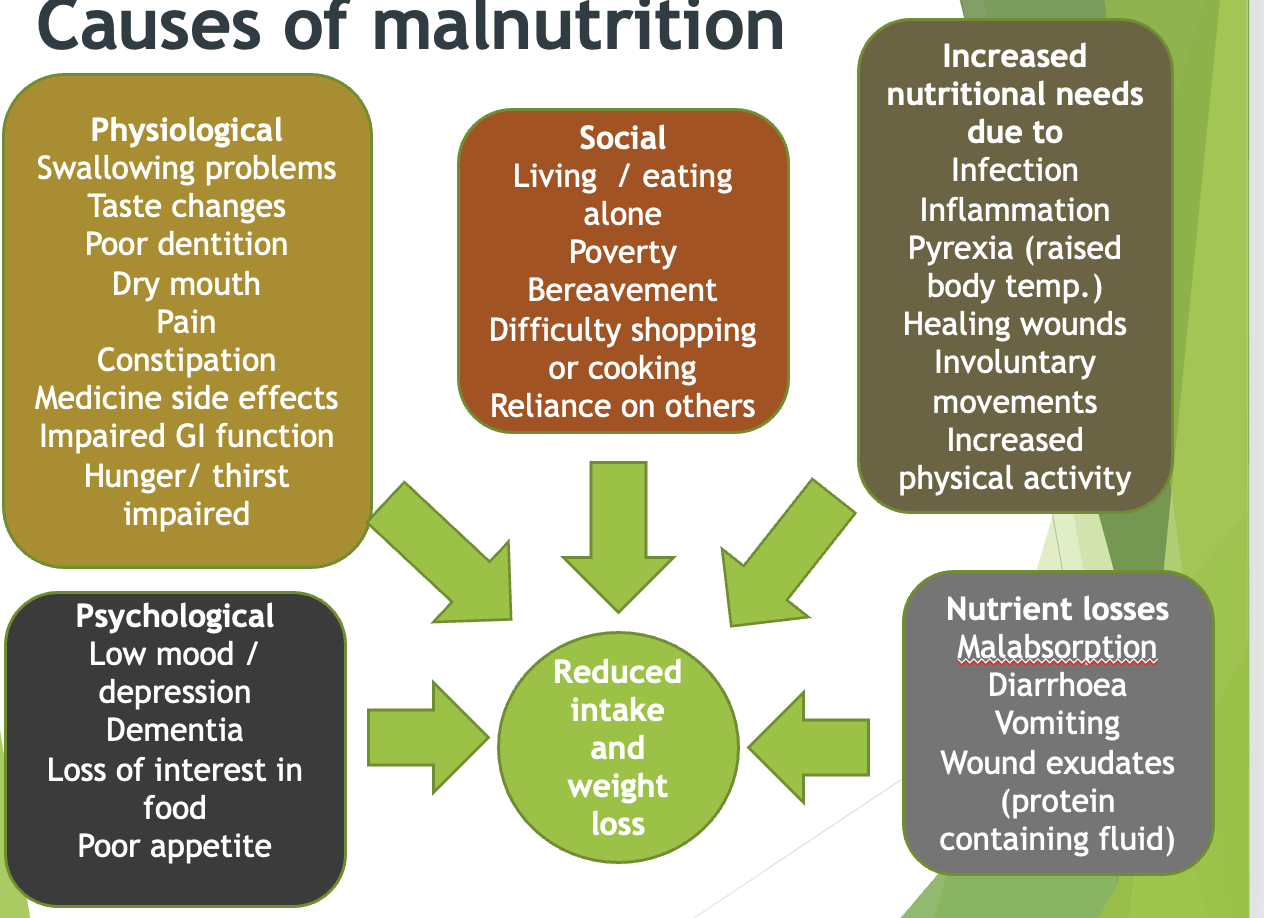
What are some causes of malnutrition
What are some physiological consequences of malnutrition
Frailty
reduced fat and muscle
poor wound healing
reduced mobility, fatigue
increased risk of infection
Weak cough
Poor absorption of nutrients
More side effects from medicines
What are some physiological consequences of malnutrition
Low mood / depression
Confusion
Appetite further reduced
What are some outcomes of malnutrition
More falls and pressure ulcers
More hospital admissions
More GP visits
Require more prescriptions
Longer length of stay
Reduced quality of life
Increased mortality
What guidelines can we use to identify malnutrtion
NICE guidelines
CQC
MUST: Calculate BMI, % weight loss, acute disease affect score, overall risk of malnutrition, management guidelines
How do we measure disease related malnutrition
BMI less than 18.5 kg/m2
Unintentional weight loss >10% in the last 3-6 months
or
BMI less than 20 and unintentional weight loss of 5% in the last 3-6 months
eating little in the past and upcoming 5 days
poor absorptive capacity
How can we treat malnutrition
manage affecting factors
set treatment aims
food based nutrient dense diet
oral nutritional supplements
review + monitor
What factors can affect food intake
difficulty swallowing
unable to use cutlery
constipation/ constipating medicines
Nausea and vomiting
do they struggle to buy/cook food
What kind of targets can be made
avoid further weight loss
achieve BMI 18.5 or 20
wound healing
regaining lost weight
What should make up a nutrient dense fortified diet
Balance of protein, energy, fibre, electrolytes, vitamins, minerals
Milkshakes
high protein/high energy snacks
fortified foods, avocado, cheese, nut, butter, seeds
simple advice e.g. add nut butter to porridge, add cheese to soup, add milk powder to puddings
What multivitamins can be advicsed
Vitamin D 10 micrograms 400 iU
reduces mortality, complications, improves weight and function
what are some clinical considerations that make nutritional supplements inapporpriate
Dysphagia: cannot have thick fluids
renal impairment: affects protein and electrolyte
pressure area; affects protein and micronutrient
fluid restriction
vegan, allergies, intolerances
What are some practical considerations that may be inappropriate
physical ability to make up milkshakes/powdered supplements
impact on compliance
What is the ACDB criteria for oral nutritional supplements
Short bowel syndrome
Dysphagia
Intractable malabsorption
Pre-operative preparation of undernourished patients
Inflammatory bowel disease
Total gastrectomy
Bowel fistulae
Disease related malnutrition (chronic/acute) – can be evidenced by MUST
MUST HAVE 2 OR MORE HIGH RISK FACTORS
ONS
prescribe 2 first line oral nutritional supplements
trial 2 weeks
consider flavours, acceptability
commonly milkshakes, juice, pudding, savoury
shots/powders/jellies/gels not balanced macro/micornutrients
How do we review and monitor patients
record weight
Is there ACBS indication
What is their MUST score
food advice?
aims of treatment
supplements?
cost effectiveness
prescribed dose
trialled supplement