Musculoskeletal Disorders in Pediatrics Overview
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
What are the main components of the musculoskeletal system?
Bones, muscles, joints, tendons, and ligaments.
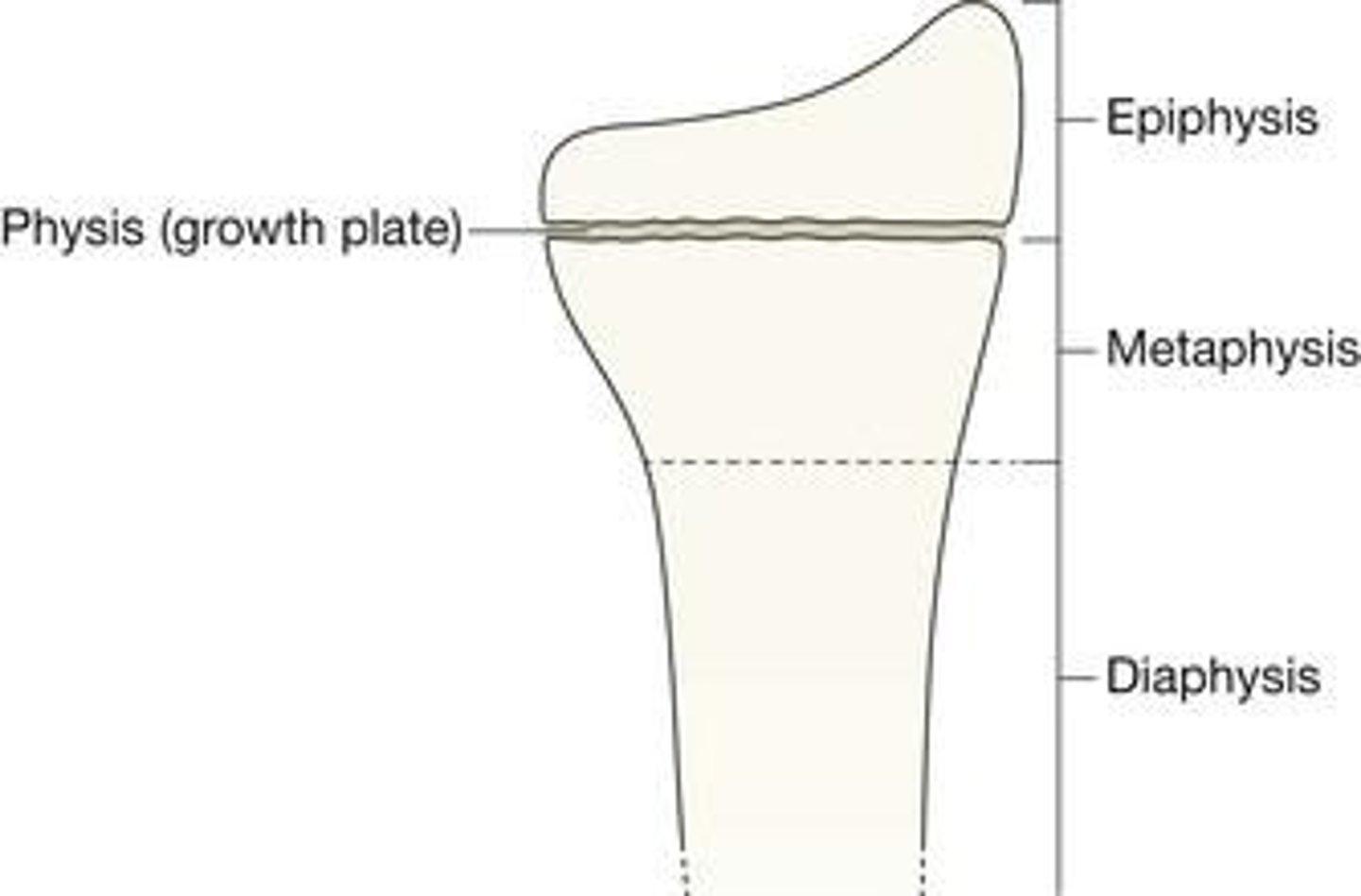
What are the key anatomical segments of growing bones?
Epiphysis (end of long bones), Physis (segment responsible for lengthening), Metaphysis (wide part where diaphysis and epiphysis meet), Diaphysis (shaft), Periosteum (sheath covering the bones).
How many bones does a newborn have, and how does this change as they grow?
At birth, newborns have 300 bones, which fuse and ossify to form 206 bones in adults.
When do the cranial sutures and fontanels close in infants?
Posterior fontanel usually closes by 2 months; anterior fontanel closes around 13 months.
What unique characteristics does a child's skeleton have compared to an adult's?
Children have an immature skeleton with increased resiliency to stress, thicker periosteum, and a greater potential for remodeling.
What is the significance of the physis in children's bones?
The physis is responsible for lengthening during growth; injury to it can have long-term effects on physical development.
How do children heal fractures compared to adults?
Children heal fractures faster than adults, requiring shorter immobilization time, but misaligned fragments can solidify sooner.
What is the difference between provisional and definitive callus in fracture healing?
Provisional callus is temporary and still developing new bone; definitive callus forms permanent osseous tissue after several weeks.
What is the recommended activity level after a cast is removed for children?
Children should avoid contact activities for 2-4 weeks and need 1-3 weeks of gradual return to full activity.
What does the acronym PRICE stand for in the context of musculoskeletal care?
Protect, Rest, Ice, Compression, and Elevation.
What are the common signs of a fracture in children?
Pain, swelling, inability to move the extremity, point tenderness, and visible deformity.
What is the most common type of fracture in children?
Fractures in the upper extremities (forearms) are the most common, occurring in 25-43% of cases.
What does FOOSH stand for in relation to fractures?
Fall onto Outstretched Hand.
What is the initial treatment for a fracture in children?
Immobilize the joint above and below the injured area, possibly reduce the fracture, and apply a splint.
What are the characteristics of a greenstick fracture?
An incomplete fracture of a long bone, typically occurring midway; if displaced, it must be reduced and placed in a long arm cast.
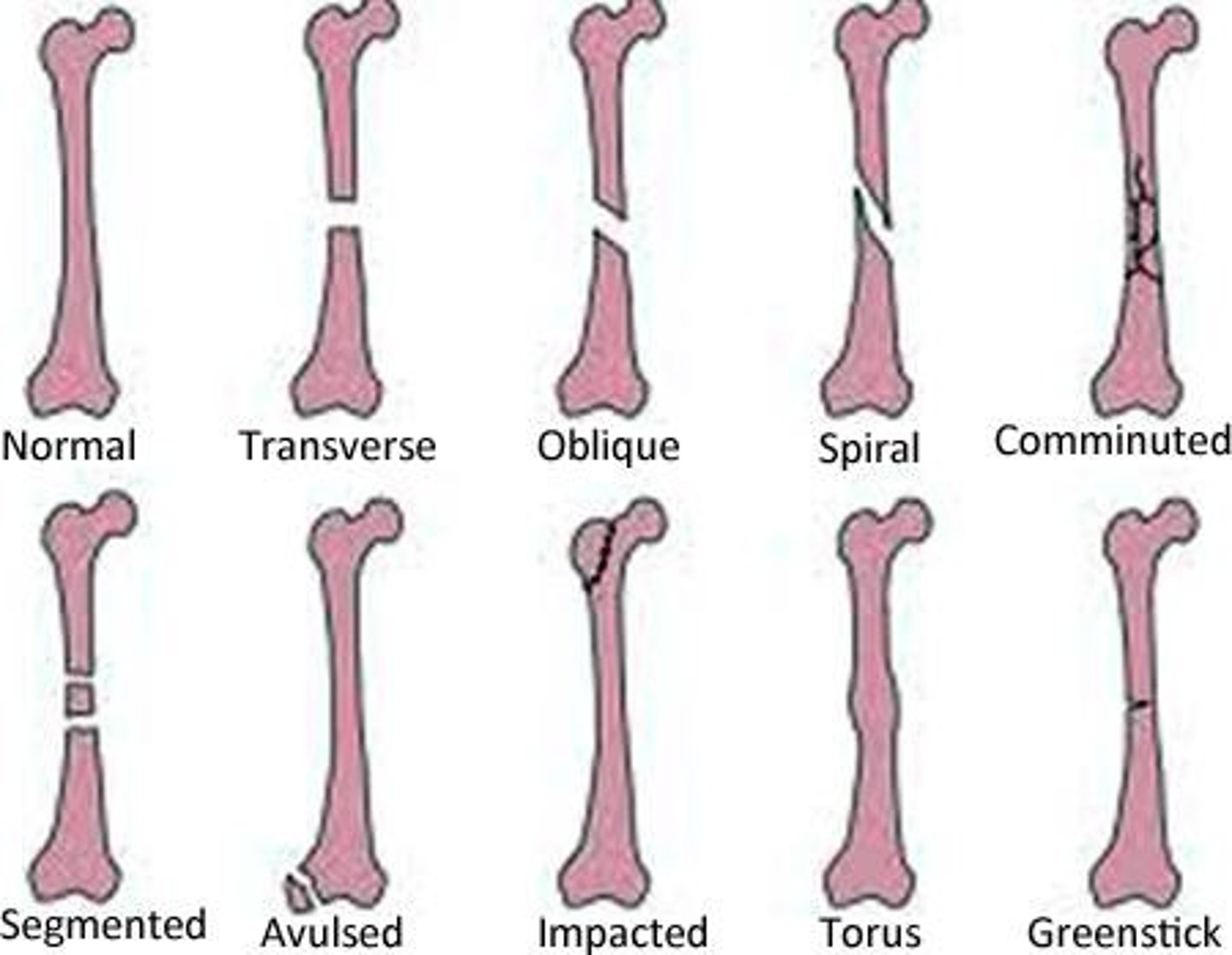
What is a torus (buckle) fracture?
A fracture where the bone bends and buckles but does not break, commonly occurring in the radius or ulna.
What is the importance of neurovascular checks in musculoskeletal injuries?
To assess movement, capillary refill, and sensation, ensuring proper blood flow and nerve function.
What role does the periosteum play in children's bone health?
It is biologically active, developing new bone and supplying blood.
How does the presence of open growth plates affect fracture healing in children?
It places children at a higher risk for complications with healing and deformity.
What are the implications of a child's increased potential to remodel bone?
Children can better repair fractured areas, especially if they have 2 years of expected growth left.
What nursing care should be provided post-operatively for musculoskeletal injuries?
Involvement of an interdisciplinary team for support, pain management, and activity-level precautions.
What are the two main types of fractures?
Simple fractures (cast) and complex fractures (involves surgery and/or orthopedic consult).
How are physeal fractures classified?
Physeal fractures are classified as Salter Harris I through IV based on the level of growth plate involvement, with higher grades indicating a greater likelihood of growth disturbances.
What is Developmental Dysplasia of the Hip (DDH)?
DDH is inadequate coverage of the ball of the socket of the hip joint or dislocation of the ball from the socket, which can lead to instability.
When is Developmental Dysplasia of the Hip (DDH) most often diagnosed?
It is most often diagnosed in the first year of life during the newborn exam but may not be identified until the child begins walking.
What factors increase the risk of Developmental Dysplasia of the Hip (DDH)?
Risk factors include breech births, swaddling with legs straight, being female, being firstborn, and having a familial history.
What are the clinical signs of Developmental Dysplasia of the Hip (DDH)?
Signs include limited hip movement (especially abduction), uneven knee heights (Galeazzi sign), uneven skin folds, and a palpable click or clunk (Ortolani and Barlow signs).
What is the recommended treatment for infants with Developmental Dysplasia of the Hip (DDH)?
The Pavlik harness is used to position the hips in alignment, worn full-time for 3 to 4 months, then at night for another 4 to 6 weeks.
What surgical intervention is needed for children aged 6 to 24 months with DDH?
Closed-reduction surgery is performed to direct the head of the femur into the acetabulum without surgical incision.
What is the purpose of a spica cast in the treatment of DDH?
A spica cast maintains alignment of the hip in the joint while the tissues repair.
What is scoliosis?
Scoliosis is a progressive condition characterized by a lateral curvature of the spine greater than 10 degrees with rotation of the vertebrae.
What are the classifications of scoliosis based on curvature location?
Scoliosis can be classified as thoracic or lumbar based on the location of the curvature.
What are the three main types of scoliosis based on cause?
Congenital, neuromuscular, and idiopathic scoliosis.
What is congenital scoliosis?
Congenital scoliosis is caused by an embryological malformation where vertebrae fail to develop or separate, leading to curvature.
What is neuromuscular scoliosis?
Neuromuscular scoliosis is curvature secondary to neurological disease of the CNS or muscles, which tends to progress rapidly.
What is idiopathic scoliosis?
Idiopathic scoliosis is diagnosed after ruling out other causes and is the most common type, accounting for 80% of cases.
What are the age categories for idiopathic scoliosis?
Infantile (under 3 years), juvenile (ages 3-10 years), and adolescent (over 10 years).
What is the most common type of scoliosis?
Adolescent idiopathic scoliosis, which manifests around puberty during growth spurts.
What are the clinical presentations of scoliosis?
Truncal asymmetry, uneven shoulders, raised hips, and a rib hump, with most patients not experiencing back pain.
How is scoliosis assessed and diagnosed?
Screening can detect curves and facilitate early intervention.
What is the purpose of screening for scoliosis in children?
To detect curves and facilitate early intervention, starting in 5th grade, and is mandatory in some states.
What is Adam's forward-bending test used for?
To examine a child's spine for misalignment and asymmetry by having them bend forward until the spine is horizontal.
What tool is used to measure the degree of truncal rotation in scoliosis assessment?
Scoliometer.
What imaging techniques confirm a diagnosis of scoliosis?
X-rays, CT scans, and/or MRI.
What is the recommended treatment for scoliosis with curves less than 25 degrees?
No treatment is required.
What is the treatment for scoliosis with curves between 30 to 45 degrees in an actively growing child?
Bracing is required, effective only if the child has not reached skeletal maturity.
How long must a child wear a brace for scoliosis treatment?
For 16 to 23 hours a day until growth stops.
What is the first-line treatment for early-onset scoliosis in children younger than 4?
Mehta casts.
What curvature degree may require surgical correction for scoliosis?
Curvature of 45-50 degrees may need spinal fusion.

What is muscular dystrophy?
A group of inherited diseases characterized by progressive muscle weakness due to muscle fiber degeneration and wasting.
What are the two most common forms of muscular dystrophy?
Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD).
What genetic defect is associated with DMD and BMD?
A defect in dystrophin, a protein that provides muscle strength and stability.
What is the incidence of DMD and BMD in males?
Approximately 15 out of 10,000 males.
At what age is DMD typically diagnosed?
Before the age of 5.
At what age is BMD typically diagnosed?
From 7 to 12 years.
What are the criteria for diagnosing Juvenile Idiopathic Arthritis (JA)?
Chronic arthritis in children under 16 with swelling or 2 or more signs for more than 6 weeks.
What are some signs of Juvenile Idiopathic Arthritis?
Limited range of motion, tenderness or pain on motion, increased heat.
What types of arthritis are included in Juvenile Idiopathic Arthritis?
Polyarticular, oligoarticular, systemic, and enthesitis-related.
What are the treatment goals for Juvenile Idiopathic Arthritis?
Preserve muscle and joint function, reduce joint destruction, control pain and inflammation, promote independence.
What is Ewing Sarcoma?
A malignant connective tissue tumor that occurs most frequently in the bone marrow of long bones.
What age group is most affected by Ewing Sarcoma?
Young adolescents and older school-aged children.
What are common symptoms of Ewing Sarcoma?
Pain at the tumor site, which may become constant and severe.
What treatments are available for Ewing Sarcoma?
Surgery, chemotherapy, and radiation.
What precautions should be taken during treatment for Ewing Sarcoma?
Caution adolescents to avoid activities that cause stress on the affected extremity.