Unit 4 - Introduction to Limb Loss
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
Etiologies of Amputation
Etiology of Amputations
Peripheral Vascular Disease (PVD) (82%)
Diabetes
Trauma (16%)
Military, work-related, farming
Cancer (1%)
Osteosarcoma
Congenital (1%)
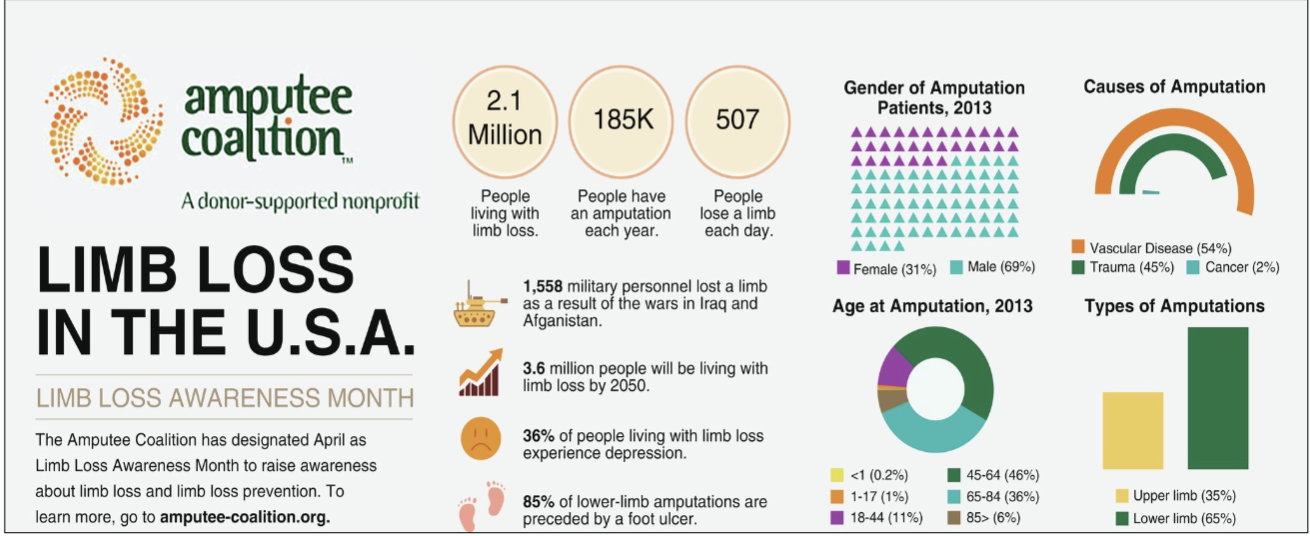
Limb Loss Statistics
U.S.A.= 2.1 million people with amputations
Expected to double by 2050
185,000 amputation surgeries/year (300-500/day)
The number of amputations caused by diabetes increased by 24% from 1988 to 2009
85% of amputations result from a foot ulcer
55% of individuals with a unilateral dysvascular amputation
Amputation of the second leg within 2‐3 years
African‐Americans up to 4x more likely to have an amputation
Lifetime healthcare cost = approx. $509K, $361K without limb loss
Peripheral Vascular Disease (PVD)
Leading cause of amputations:
Diabetes
Arteriosclerosis
Thromboembolism
Chronic Venous Insufficiency
Complicated by neuropathy
Amputation of the contralateral limb in 50% of patients in 2 to 5 years
Diabetes
PVD more common in persons with diabetes than without
Hypertension most predisposing factor for LE amputations in persons with diabetes.
Complications
vision issues —> neuropathy —> infections
Age & Amputation
Peak age range: 41-70 years old
75% of all amputations > 65 years old
Thus, most of your patients with amputations will be older adults!
The Diabetic Foot
Assessment
In addition, to tests and measures, check footwear
Care
Education on footwear
Keep the feet moist
Skin care
Skin inspection
Trauma
Second most common cause of amputation (16%)
Military, work or vehicle related accidents, farming
Most common in young adult men
Cancer
Account for about 1% of amputations
Osteosarcoma
Primarily affects children and adolescents
Congenital Limb Difference
Represents just under 1% of amputations
Slightly higher incidence of UE vs. LE
Amniotic Band Syndrome
Factors Affecting Rehabilitation
Health status
Age
Cognitive status
Comorbidities
Level of amputation
Amputations of the Toes
Localized level of gangrene
Neuropathic ulcer on plantar surface
Infection or osteomyelitis of the phalanges
Neoplasms
Ray Resection
Vascular disease, Neuropathic ulcer, Osteomyelitis
Surgery of choice for 4th and 5th ray removal
Not surgery of choice if 1st and 2nd ray removed
Orthotic or prosthetic shoe filler
Transmetatarsal
Ray resection of all five metatarsals proximal to metatarsal heads
Risk factors for poor healing
Equinovarus
Need toe filler in shoe
Lisfranc
Disarticulation of tarsal/metatarsal joint
Attempt to maintain transverse arch of midfoot
Chopart
Disarticulation of midtarsal joint
Between talus and navicular bones and calcaneus and cuboids
Leaves calcaneus and talus intact
Equinovarus deformity
Requires custom footwear or orthosis
Symes
Disarticulation of the talocrural joint
Calcaneus and talus removed
Bilateral malleoli are beveled
Repositions fat pad/soft tissue under distal tibia/fibula
Transtibial
Muscles crossing knee joint are preserved
Fibula is cut approximately ½ to ¾” above tibia
Anterior aspect of tibia is beveled
Long posterior flap vs. equal length flap
ERTL Procedure
Strut from the tibia to fibula
Bone bridge will enhance weight bearing and increase total surface area for load transfer
Increased reoperation rates
Requires longer operative and tourniquet times than standard BKA
New method = titanium strut
Knee Disarticulation
Excellent and large weight bearing end
Long lever arm controlled by strong muscles
Increased stability of the patient’s prosthesis
No bone cut and very few muscles
Patella may or may not be spared
Difficulty establishing equal prosthetic knee center
More distal knee center
Rotationplasty
Usually from malignant neoplasm
Ipsilateral ankle reattached at 180-degree angle
Creates a knee joint
Preserves growth plate to allow similar knee center at maturity
Transfemoral
Preservation of length of femur
Myodesis vs. Myoplasty
Beveled end of femur
Nerves cut for good coverage by muscle
Traditional transfemoral surgery
Osseo-integrated transfemoral
Hip Disarticulation and Hemipelvectomy
Amputation undertaken to preserve life
Significant body mass removed/blood loss
Increased risk of blood clot of the intact limb
Limited activity begins once patient medically stable
Common Techniques at all Levels
Myodesis and Myoplasty
suturing muscle to bone or muscle to muscle
Common Techniques at all Levels
Fibular versus tibial length
tibia always longer by ~2cm or 0.5in
Common Techniques at all Levels
Beveling ends of bone for decreased heterotrophic ossification
Flaps (according to vascular pathology generally)
Common Techniques at all Levels
Nerve resection
without trauma to the nerve - usually with a scalpel not scissors
Osseointegrated Transfemoral Amputations
Trauma
Osteosarcoma
Initially from Sweden (1990’s)
Implant directly into bone via coupling
Has a stoma
Osseointegration
Interface between tibia or femur prosthetic components
No need for socket as the interface
Allows for proprioceptive input, less heat retention, less skin breakdown from contact
Infection risk
Neuromas
A high rate of amputees acquire
Some Treatment Options are TMR and RPNI. These surgeries involve proper nerve handling at the time of procedure
Neuroma Removal and Z-plasty
*a painful growth of a bundle of nerves usually arising from agitation
Ill-fitting socket
Irritation from surrounding tissues/structures.
Surgical techniques:
Z-plasty
Balloon implantation for scar mobility
RPNI: Regenerative Peripheral Nerve Interphase
Implants nerve segments into a denervated muscle graft.
Generally, for lower extremity as the LE prostheses do not have the same ability to be controlled yet as UE prosthetic devices
TMR: Targeted Muscle Reinnervation
Pioneered in 2002 (Kuiken and Dumanian) at Northwestern
Originally for UE amputations to control prosthetics using normal muscle actions by routing to nearby motor nerves
Re-route nerves to specific muscles to control the prosthesis for the shoulder joint, or for transhumeral amputations.
Secondarily reduces phantom limb pain by creating neuromuscular junctions
Pre-operative Considerations
Explore patient and family’s expectations
Explain sequence of events (do NOT include time expectations)
Reinforce realistic expectations
Answer questions within PT scope
Anticipate psychological status
Clergy or rehab psychologist
Pain control
Pre-operative Considerations
Prehab
Cardiovascular
Intermittent claudication
Treadmill training
Pre-prosthetic training
Pre-prosthetic education
Set up for evaluation within 1-2 days post-op
AMPREDICT
VA decision tool, estimates mortality or re-amputation
Not for anyone with previous amputation
Peri-Operative Considerations
Prosthetic education and realistic expectations
Peer visitor (Amputee Coalition)
Home evaluation
Work and social environments
Multi-disciplinary network
Outcomes measures (applicable only)
Acute Care: Pain Management
Alleviate acute discomfort
Biophysical agents
Medications as prescribed
Learn precipitating and relieving factors for pain
Generate motivation
Team approach
Acute Care Goals
Wound and residual limb healing
Residual limb shaping
Potential protective dressing
Contracture prevention
Education
Peer visitor when possible
All the above without complications!
Acute Care Examination
Determine surgical techniques and visualize incision(s)
Myodesis, mypoplasty, direction of vascular/muscle flaps
Motor learning, including previous use of AD or DME
Bed mobility and CAN attempt transfer
Facilitates a rehab discharge
Positioning of limb
Neutral? Contracture pattern developing?
Limb measurements/observations
Edema control method
Contracture Prevention for Amputations
Positions of comfort
Imbalance of muscle strength/intact
Contracture pattern in transtibial
Knee flexion, can be hip flexion
Rarely (hip abduction and external rotation)
Contracture pattern in transfemoral
Hip flexion, hip abduction, and hip external rotation
Skin Protection and Hygiene
Goal: to protect against the adverse effects of infection, and external mechanical forces including pressure, friction, and shear
Patient-Centered Management after an Amputation
Individuals with a new amputation
Patient-centered care and multidisciplinary teams
Edema control
Pain control
Wound healing
Protect incision
Facilitate preparation for prosthetics
Interventions: Edema Control
Limb volume, shaping, and postoperative edema
Soft dressings
Pressure garments: Shrinkers
Removable Semi-rigid Dressings
Polyethylene
Zinc Oxide
Interventions: Elastic Wraps
Wrapping a limb
Distal pressure > proximal pressure
Pressure applied on oblique turns
No wrinkles
Do not leave any areas open
Overlap ace bandage by ½ to 1”
Interventions: Elastic Wraps
Prevent contractures
Transfemoral (hip flex, hip abd, ER)
Adductor roll
Transtibial (knee flex, hip abd, ER)
Wrapping Advantages/Disadvantages
Does not aid in the shaping of the residuum
Requires ~5+ years to completely shrink and mature the residual limb
To be effective, keep wrapped except for bathing
Re-applied and cleaned a minimum of every 24 hours
Requires frequent reapplication
Provides very minimal amount of compression (mmHg) and is inconsistent
Soft Dressing Advantages
Low cost
Easy wound inspection for healing and infection control
some can be easier to don/doff
tubular elastic can provide consistent compression
elastic wraps can be modified for variable compression
Soft Dressing Disadvantages
Can have poor control of edema if donned or sized incorrectly
All have the need for frequent re-application
Some are difficult for the patient to apply independently and correctly
Inadequate trauma protection
High potential to create a tourniquet
Spandagrip Advantages/Disadvantages
Circular elastic bandage in the shape of a tube
Can be cut to the desired length
Multiple sizes
Less mmHg than shrinker socks
More consistent mmHg than elastic wraps
Shrinker Socks
Sometimes easier than an ace wrap
More expensive initial cost
NO USE until the staples or sutures are out
Provides about 30-40mmHg
New shrinkers as volume reduces
Shrinkers Advantages
Easier to use for transfemoral
Slipping is minimized because the hip spica (for transfemoral) aids suspension
Better compliance than with elastic bandages
Shrinkers Disadvantages
Increased expense
Multiple shrinkers as the residual limb loses edema/volume
Does not prevent an adductor roll
Tends to be uncomfortable over sensitive areas or bony prominences
Requires hand strength and dexterity to apply
Dressing Advantages/Disadvantages
Combination Dressings
If necessary, ace wraps may be applied over shrinker socks but often cannot be tolerated for long periods of time.
Some prosthetists suggest wearing a silicone sleeve over their shrinker sock to increase mmHg compression for fitting.
NOTE: Please be aware of skin breakdown, skin sensitivities and tolerance to fluid re-absorption
Interventions: Edema Control
IPOP: Immediate Post Operative Prosthesis
Casted by surgeon and prosthetist in the OR
Sometimes removable
Interventions: Edema Control
EPOP: Early Post Operative Prosthesis
Always removable
Off the shelf, not custom made
IPOP/EPOP Advantages
Improved shaping, healing time
Protection from trauma
Maintenance of strength and function
Prevention of contractures
Early return to balance and ambulation tasks
Improved social and emotional well-being
Shorter hospital stays and overall recovery time
Earlier identification of the functional level that determines components
Reduction in severity of phantom pains
IPOP/EPOP Disadvantages
Potential for risk for falls or injury
Limited WB can inhibit healing
Ambulation is sometimes encouraged too soon
Difficult to attain proper fitting and pressure relief
Difficult to inspect the limb if it is not removable
Difficult to match the sound side
NOT indicated for incontinence
Semi-rigid advantages
Compared with rigid dressings and IPOP are less expensive
Improved edema control
Improved trauma protection
Remains relatively secure during functional mobility
Minimal movement inside the dressing
Semi-rigid disadvantages
Need for trained personnel to apply dressing initially and for training
Lack of easy inspection to monitor healing (not removable if Unna Paste)
Can be unsuitable for incontinent patients
Limb Measurement
Measure girth routinely to control and monitor edema
Measure redundant tissue (“dog ears,” adductor roll)
Residual limb shape (bulbous, cylindrical, conical)
Assessment of type and severity of edema
Assess for other skin problems
Myodesis and myoplasty operative techniques can determine limb shape, muscle mass retained and therefore determines muscle strength
Initially measure residual limb length in terms of a long, medium or short residuum
Interventions for Persons with Recent Amputations
Skin Care and Scar Management
Range of Motion and Flexibility
Muscle Performance
Endurance
Postural Control
Wheelchairs, Seating, and Adaptive Equipment\
Bed Mobility and Transfers
Ambulation and Locomotion
Care of the Remaining Limb
Examination of a Patient
Complete patient-client history
Systems Review
Tests and measures
Patient-Client History Review
Demographic and Sociocultural Information
Developmental Status
Living Environment
Health, Emotional, and Cognitive Status
Medical, Surgical, and Family history
Current Condition
Systems Review
Cardiopulmonary and cardiovascular
Musculoskeletal
Neuromuscular
Integumentary
Communication
Tests & Measures
Acute postoperative pain
Phantom sensation and phantom pain
Residual limb length and volume
Integumentary integrity and wound healing
Circulation
ROM and muscle strength
Joint integrity and mobility
Muscle performance and motor control
Upper extremity function
Aerobic capacity and endurance
Attention and cognition
Sensory Integrity
Mobility, locomotion, and balance
Posture, ergonomics, and body mechanics
Self-care and environmental barriers
Postoperative complications
Common Outcome Measures Used in Assessment
Performance Based
Amputee Mobility Predictor
No Prosthesis (AMP-noPro)
Timed Up and Go (TUG)
Two Minute Walk Test (2MWT)
Self-report measures
Houghton Scale
Prosthetic Evaluation Questionnaire (PEQ)
Prosthetic Limb Users Survey of Mobility (PLUS-M)
Evaluation, Diagnosis, & Prognosis
PT diagnosis
Plan of care: Prognosis
Plan of care: Determining appropriate goals
Triple Threat
Loss of function, loss of sensation, and loss of body image
Many amputees adapt well
Resilience
Ingenuity and dedication of caregivers
The observed psychological response to amputation is determined by many variables
Psycho-social variables
Biological variables
Social drivers of health
Psychosocial Support
Single/widowed individuals
Increased psychological distress
Increased difficulty in adapting to amputation
Supportive partner is ideal
Assumes a flexible approach
Takes over functions as needed
Allows autonomy and independence while supportive
At all times maintains the self-esteem of the individual
Parents remain a major source of support for children and young adults
Peer acceptance beyond the family is critical for adaptation
Psychosocial Variables: Older Adults
response to limb loss depends on:
Generational/familial responses to trauma
Social support and network
Job or volunteer status
Medical comorbidities
at greater risk for:
Depression
Polypharmacy
Frailty
Age Considerations
Infant/Toddler
Child will adapt and meet motor milestones and usually quickly learn to use prosthetics
Usually fit with a prosthesis as soon as they are developmentally ready
Be aware that parents may be in shock, denial, or experience feelings of guilt
Age Considerations
Pre-teen/teenagers
develop a “unique” identity
Traumatic to lose a limb when one’s identity isn’t yet established
Be sensitive to the need for increased modesty in teenagers and young adults
Sensitive to peer acceptance and rejection (“no one is going to look at/befriend me”)
They want to be involved with other young amputees
Sexuality can be an “unspoken concern
Age Considerations
Middle Age & Older Adults
Impact on occupation/financial status is major concern
Desire to maintain independence is a critical issue in this population
May have a sense of failure if loss of limb was due to unhealed wound
Economic Impacts
Individuals with occupations that require high degree of motor skill most vulnerable
Unemployment
Underemployment
Inability to become employed
If re-employment is likely - Office of Vocational Rehabilitation (VR)
Voc (pronounced Voke) Rehab
State funded program
Individuals with disabilities find and maintain employment
Influence of Psychosocial Aspects in Physical Therapy
Change in self-concept relative to body image
Effect of pain or altered sensation
incisional, body and/or phantom
Age considerations
Financial impacts
Depression in the Amputee Population
Strong link between psychosocial adjustment and rehab outcomes:
High-levels of anxiety and depression in amputee population
28.7% with severe depressive symptoms (Darnall et al 2005)
Individuals with higher levels of education have less depression
Only 44% received mental health service
Dreams/nightmares are common in first month post-operatively
If persistent = poor adjustment
Personality Styles
Narcissism with investment in physical appearance
Tend to react negatively to loss of limb
Co-dependent individuals may cherish sick role
May find welcome relief from pressure and responsibility
History of depression are susceptible to dysphoria
Notions of basic defectiveness
Can result self-punishing behaviors
Self-Perception: Body
Learning three (3) body images
Intact, amputee, amputee with a prosthesis
Self perception about body image is influenced by:
Age
Cultural beliefs
Social stigma, religious or spiritual beliefs, locus of control
Personality type and coping style
How a person responds to this change after an amputation may affect:
Recovery process
Personal relationships
Living environment
Vocational goals
Leisure activities
Coping Styles Influence Adaptation
Livneh et al suggest 4 basic styles:
Active problem-solving:
Seek support
Reframe the problem
Make plans to adapt
Emotion-focused:
Wishful thinker
Self-blame
Socially withdraws
Problem disengagement:
Problem avoidance
Drugs/alcohol abuse
Hyper-religion
Cognitive disengagement
Total denial
Sexuality
An area of some questions and concerns especially in the young adult
Rejection by a partner
Physical impact due to loss of body part
Prosthesis is of no use in this area
Self-consciousness
Loss of sensation depending on cause of amputation
Do not overlook discussion in this area – self-help groups may provide best source of information
Pain Considerations
Phantom pain or other Nerve pain
Pain from their prosthesis
70% at some point complain of back pain. Many times this is due to altered gait patterns
Leg length discrepancies (appropriate or inappropriate)
Incorrect fit causing amputees to accommodate to a prosthesis
Sound limb pain often due to overuse for daily activities or transfers when prosthesis is removed
Prosthesis Related Pain
Socket should be designed to avoid pressure sensitive areas
Total contact socket distributes weight of the limb across large area of tissue
Indentations in tolerant regions used to relieve pressure sensitive areas
Socket will require modifications as residual limb changes:
Muscle atrophy
Edema management
Weight change
Length change
Volume change
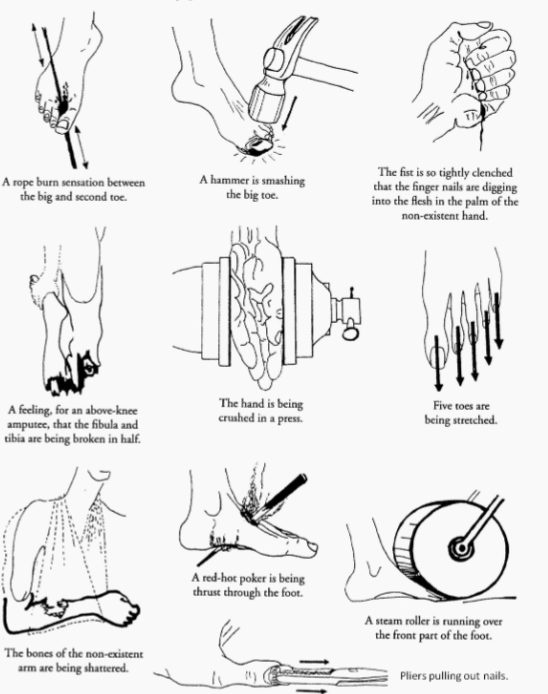
Phantom Limb Sensation
Feeling that missing limb is still present
Variety of sensations: itch, tactile touch, pressure, temperature, position, and/or movement
Non-painful
Estimated that 80-90% of patients will have some phantom sensation
May persist many years after amputation
Few studies completed to explore impact on function
May benefit or hinder patient depending on a multitude of factors
Phantom Limb Pain
Painful sensations arising from the missing portion of the limb
Estimated that 45% - 85% experience phantom limb pain
High variation in different populations being studied and no distinct instrument to assess
Usually described as sharp, shooting, tingling, stabbing
Onset is typically in first few days after amputation
Episodic or intermittent – not typically constant
Usually described as moderate in intensity – a 5 – 6 on a 10-point VAS, but great variation in studies
More information is known about LE than UE phantom limb pain
War Amps of Canada: Phantom Pain
Interventions for Phantom Pain
Pharmaceuticals: anti-depressants, anticonvulsants, opioids includes cannabinoids
Mirror box therapy
Mental imagery
Virtual reality
Nerve Stimulator: may require surgery
Acupuncture
Targeted Muscle Reinnervation (TMR): surgical
Regenerative Peripheral Nerve Interfacing (RPNI): surgical
Neuromas may Cause Phantom Limb Pain
Axons from excised nerves attempt to regenerate and grow
Epineural sheath damaged cannot direct regrowth
Nerves start to grow but get bundled, form scar tissue
Creates pain with pressure, stretching, touch
Surgical Approaches for Phantom Limb Pain
Targeted Muscle Reinnervation (TMR)
involves surgically connecting a severed nerve to a nearby muscle. Provides new target for nerve regeneration
Surgical Approaches for Phantom Limb Pain
Regenerative Peripheral Nerve Interface (RPNI)
a surgical technique used to prevent and treat pain associated with nerve injuries, particularly in amputations