Week 1 - MLS departments
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
What is an analyte?
Analyte = any substance capable of being identified or measured (ex: glucose, sodium, thyroid hormone)
What makes up the core lab?
Core lab = hematology & chemistry
Because it makes up the core of what a lab is (heavily automated, similar processes, lots of blood tubes, makes up the bulk of testing (where most testing is done))
What is considered a “stand alone” department?
Stand-alone = blood bank
What is the clinical chemistry department? Goal?
Clinical chemistry = the study of biochemical processes associated with health and disease and the techniques used to assay these processes
Involves the measurement of constituents in body fluids (blood, serum, and plasma) to help diagnosis, monitor, or determine the effect of treatment for disease
Goal = to determine abnormal values that can be attributed to where or when that disease is occurring
Scope/components: sample prep & QA/QC (because heavily automated), biochemistry, physiology, pharmacology, immunology, toxicology, urinalysis, analytical chemistry, technology, & microbiology
What is the transfusion dept.? And it’s components?
Transfusion = blood regulated like a drug
Components
Immunohematology = blood typing principles and science used by both transfusion depts. And blood banks
Transfusion services = clinical lab, typing patients, crossmatching to units, handles the issues of blood products for transfusion
Blood bank = segregated lab.
Collecting, testing, storing, and distributing donor products
Ensures safety of blood products by typing units and testing them for transmissible disease
What is the hematology dept.? What are it’s components? What does it mainly work with?
Hematology = the study of blood cells and indices in circulating blood or bone marrow in order to determine blood-related conditions or disease
Mainly focused on RBC & WBC
Hematopoietic cells = amount of circulating blood cells is regulated by the rate of production and release from the bone marrow
Work with whole blood (EDTA/purple top)
Detect anemia, polycythemia, hemoglobin issues, leukemias
Components:
Hematology
Coagulation
Urinalysis & blood fluids
What is the microbiology dept.?
Microbiology = help identify infectious disease and treat them
Disorders caused by microorganisms
Bacteriology, mycology (fungi/yeast), virology
One of most common healthcare problems encountered
Inpatient (including nosocomial infections – infections due to hospital stay)
Outpatient
Define and detect pathogens
While not overworking a sample (being able to tell what is part of the normal flora)
What does the anticoagulant tube do/is?
Anticoagulant tube = prevents clotting or coagulating of blood
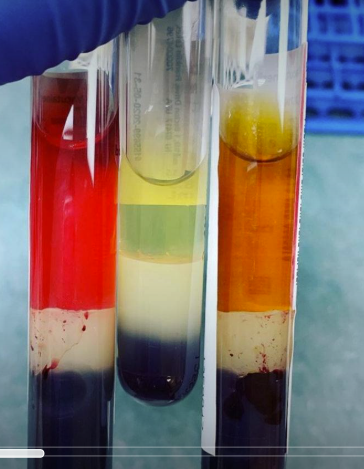
Un-clotted whole blood will produce plasma after centrifugation (EDTA/purple top)
When mixed with an anticoagulant, it’ll be plasma
What does the no additive or clot activator tube do/is?
No additive or clot activator = clotted whole blood will produce serum after centrifugation
When whole blood is allowed to clot, it’ll become a serum
What are common specimens and analytes for the clinical chemistry department?
Clinical chemistry =
Common analytes = proteins, electrolytes, blood gases, lipids, vitamins, hormones, tumor markers, & enzymes
Look at products of specific cellular gene expression/translation
Types of specimens:
Blood (whole blood, serum (more common), plasma (more common))
Body fluids (urine (more common, besides blood), CSF, any other BF)
What are common specimens and analytes for the hematology department?
Coagulation:
Specimen is critical
Blood collection tubes
Anticoagulant = will produce plasma after centrifugation
Plasma retains all clotting factors (what coag. Dept. Is looking for)
No additive or clot activator (will produce serum after centrifugation)
Serum has no clotting factors (NOT acceptable for coag. Dept.)
Sodium citrate anticoagulant (light blue)
9:1 blood-to-anticoagulant ratio
Urinalysis
Cells in urine (a few cells are normal)
RBCs, WBCs, epis
Epithelial types = squamous, transitional (from the bladder – not good in abundance), & renal tubular (from tubules – not good in abundance)
What are common specimens and analytes for the transfusion department?
Transfusion =
Whole blood => RBC and plasma tested (centrifuge needed)
What are common specimens and analytes for the microbiology department?
Specimens: all require aseptic/sterile collection technique
Swabs (genital, wound, throat, nasopharyngeal, etc.)
Urine
Stool
Tissue & bone
Body fluids & pus
Respiratory (sputum or bronchial wash/lavage. NO SALIVA)
Nails & hair
blood
What is hemolysis?
Hemolysis = damage to RBC membranes causing release of RBC contents into plasma (hemoglobin/electrolytes)
Presence of hemoglobin makes serum red/pinkish, but still clear in opacity
NOT IDEAL FOR TESTING because it affects the reliability and validity of the results (false positive/negative)
normal color = clear or yellow
What muscle markers help diagnose cardia muscle tissue in the chemistry dept.
Creatine kinase = elevated in muscular disorders, physical activity, and cardiac trauma
CK-MM = mostly in skeletal muscle
CK-MB = mostly in smooth heart muscle -> used to help diagnose heart attacks
CK-BB = in brain and prostate
Troponin = protein found in all muscle as part of actin-myosin complex
Specific subunits are present in specific muscle tissues
TnT: cardiac -> used to help diagnose heart attacks
TnL: cardiac -> used to help diagnose heart attacks
Tn0: cardia and skeletal
What is the most common test ordered in all of ML
CBC (complete blood count) = indicates the NUMBER of circulating cells and measures helpful indices
Multi-parameter electronic cell counters include an automatic diluting system
RBC (cell size and volume), Hgb (hemoglobin in one RBC), MCV, Hct (hematocrit = % of someone’s blood that is RNCs relative to their plasma), MCH, MCHC, RDW (provides estimate of difference in RBC sizes), WBC, Platelet, MPV
Ran by hematology department
Differential – peripheral blood smear (percentage result)
Indicates relative percentage of each type of WBC (lymphocytes, monocytes, neutrophils, etc.)
Drop of venous or capillary blood smeared on slide and stained to differentiate WBCs, RBCs, and platelets
WBC differential is a count of 100 WBCs examined under high power, relative percentage
Assesses morphology of RBCs and platelet hallmarks too
What are erythrocytes (RBCs)?
Erythrocytes (RBCs) = biconcave disks with no nucleus or mitochondria
Function = to transport and protect hemoglobin
Contains iron to reversibly bind oxygen
What are Leukocytes (WBCs)? (what make it)
Leukocytes (WBCs)
Neutrophil (~50-70%) = major lines of defense against infection
Mature form = segmented nucleus “seg”
Immature form = “band”
Lymphocytes (~25-45%) = responsible for much of the immune function
t-cells, b-cells, & NK cells
Monocytes (~3-7%) = largest circulating WBC (phagocytosis)
Basophil (~0-2%) = mediate inflammation (release histamine)
Eosinophil (~0-4%) = provide protection against parasites
What are platelets?
Platelets = small, disk-shaped cell fragments, with no nucleus
Formed from the cytoplasm of megakaryocytes in the bone marrow
Necessary for hemostasis (function as “plugs” to stop blood from leaking out of damaged sub-endothelium tissue of vessels)
What is the coagulation cascade?
Coagulation cascade = clotting factors bind platelets and begin cycle of platelet activation for aggregation
Then the formation and stabilization of a platelet plug (a clot)
All the factors activate to form a clot
If any number of factors are defective, clotting issues will arise
Coag. can detect a hypercoagulable state (clot very quick) or bleeding issues (slow to no clot) and test which factors may be at fault
What is measured and calculated from RBCs
RBC indices:
Measured
Measure cell size and volume
Hemoglobin is determined by spectrophotometry
Calculated:
Hematocrit = the % of someone's blood that is RBCs relative to their plasma
Average concentration of hemoglobin in one RBC
RBW (RBC distribution width) provides estimate of difference in RBC sizes
What is Thalassemia
Thalassemia = disorders of Hgb synthesis
Abnormal hemoglobin results from CBC
Mostly diagnosed by examining peripheral blood smear (differential) for RBC morphology, CBC, or electrophoresis (chemistry dept.)
What is HDN
HDN = hemolytic disease of the newborn
Postpartum evaluation (bilirubin)
What are possible origins for kidney disease?
Kidney disease origin = lowered glomerular filtration rate (GFR) or urine output (first sign). Can be from any of the following issues... (therefore lab runs many tests to see which one is the cause)
Renal issue = glomerulus, tubules
Post-renal issue = bladder, urinary tract
Pre-renal (cardiac) issue = lack of adequate blood flow into kidney
Urinalysis results are matched with serum/plasma values to provide a complete picture of disease
What dept. is most likely to utilize MT?
Microbiology department
Rapid identification
Viruses
Instances in need of rapid ID (Sepsis)
Glow-growing bacteria
Mycobacteria take 4-28 days to grow on culture media
Mycobacteria tuberculosis is highly infectious, debilitating, and highly resistant to antibiotics – shows that we need a rapid ID
Resistance genes
PCR & NGS
Benefits = more rapid than conventional culture & clearer picture of complicated infections (ability to multiplex)
Drawbacks = cannot differentiate dead cells from live & cannot differentiate normal flora from pathogen & more expensive
Technique
Multiplex PCR system = looks for numerous targets within one PCR run
What is Antimicrobial Susceptibility Testing (AST)?
Antimicrobial Susceptibility Testing (AST) = use of chemical compounds to treat infectious diseases to destroy or inhibit disease causing organisms
Often needed to predict whether a specific therapy will eradicate a pathogen
Used as a follow up to ensure infection will not return
Interpretations: for an antimicrobial
Susceptible = follow normal dosing & pathogen will be inhibited
Intermediate = higher than normal doses may be effective
Resistant = inhibition will not likely occur & not advised for use
Why is AST/Antimicrobial therapy stewardship important?
Important because of antibiotic resistance
Rampant because...
Natural selection of resistance genes
Plasmid swapping (microbes are smart, they learn from experience and each other)
Inappropriate prescription/administration
Wrong antibiotic (ineffective) or not indicated (viral infection)
Inappropriate use (not finishing the prescribed course)
Stronger resistant bacteria survive and then grow more that are resistant to the medication
ANTIMICROBIAL STEWARDSHIP CAN PREVENT MULTIRESISTANT ORGANISMS
Because infections of antibiotic-resistant organisms are becoming a more common cause of death
What type of tests/techniques are used in a clinical chemistry lab?
Clinical chemistry: methodologies
Photometry = measurement of light transmittance/absorption
Electrochemistry = measurement of electrical signals associated with a chemical system (very common)
Includes potentiometry (electrolytes, pH), amperometry (electroactive analytes – glucose/glucometer), and osmometry (moles of particles per kilogram of solvent0
Immunoassays = antibody or antigen labeled for detection
ELISA/EIA, FIA
Electrophoresis = separation of charged particles in solution when electrical field is applied (protein detections usually)
Protein, hemoglobin
Chromatography = separation of complex mixtures based on physical interaction between solutes and a “solid phase” (not as common in hospital lab)
HPLC, GC, toxic drugs, ion fragments
OTHER
Automation = Defined as the mechanization of chemical analyses
Done in order to minimize manual manipulation
Removes human performance variability
Rapid (better TATs (turnaround time))
Free-up personnel to perform other tasks
Decreases cost over time
Chemistry profiles = several chemistry analyses designed to assess a single physiological system or state
System: renal, hepatic, thyroid etc.
State: Metabolic (CMP, BMP), lipid, etc.
Most cost effective
Profiles/panels are all part of a test menu
Reason chem. Department so busy
Blood samples:
Whole blood obtained via venipuncture
The liquid portion of whole blood is captured after centrifugation & used for chemistry testing (liquid & cellular components portions)
Proper specimen collection and processing is imperative for testing
Muscle analytes = examines enzymes and proteins released from muscle upon damage of tissues from necrosis, injury or strenuous activity
Creatine kinase = elevated in muscular disorders, physical activity, and cardiac trauma (three isoforms: CK-MM, MB, & BB)
Lactate dehydrogenase
Myoglobin
Troponin (heart attack)
What type of tests/techniques are done in a transfusion lab?
Transfusion = immunohematology
Immunology = the study of immunity molecules (antigens, immunoglobulins) & systems responsible for the recognition of material deemed “foreign”
Immunohematology = combined study of immunology as it pertains to blood antigens (Ag) and antibodies (Ab)
Specifically, the principle of agglutination in immune reactions is used to visualize compatibility of blood products to patients
Major blood types & compatibility:
ABO gene on chromosome 9
Antibodies produced in plasma for “foreign” antigens
O RBCs -> Universal donor
AB RBCs -> universal recipient
Type and crossmatch = requires EDTA sample (whole blood -> RBC and plasma tested)
Anticoagulated blood sample is drawn and centrifuged to separate the RBCs from plasma (TYPE)
Forward type -> patient RBCs are typed for Ag
Reverse type -> patient plasma is typed for Ab
Blood component is then chosen based off of assumed compatibility, and is further crossmatched to the patient (CROSSMATCH)
Ex: patient plasma is combined with RBC unit
Clotting = means they are not a match
Massive transfusion = emergency protocol initiated in massive traumas when individuals need a large amount of blood products issued for life-saving measures
Maternal/fetal functions
Prenatal evaluation (Rh status (weak D/partial D Rh) & RhoGAM shot)
Postpartum evaluation = hemolytic disease of newborn (HDN)
Molecular studies in immunohematology
Mainly PCR (very sensitive, high negative predictive value
HLA typing
Tissue transplants
Stem cell transplants
Pathogen detection
Viral (donor disease)
Bacterial (collection sterility)
ABO molecular tests
Available, but not widely utilized
Serology is far cheaper and faster
What type of tests/techniques are used in a microbiology lab?
Identifying microorganisms:
Isolate and identify pathogens
Bacteria – identified via plating
Possible types of growth
Single pathogen
Multiple causative agents (multiple pathogens at once)
Account for normal flora
Narrow, change, or discontinue antimicrobial therapy (once pathogen has been identified)
Change empiric broad spectrum therapy to specific targeted treatment
Decreases risk of multi-resistant organisms
Direct smears = gram stain
Rapid stain
Purpose = assesses specimen quality (contamination), screens for microorganisms, & identifies morphology and gram reaction
Purple = +
Pink = -
Results = assist physician with initial patient management & gram + are susceptible to some antibiotics that gram - are not
Advancements =
Mass spectrometry (very fasts & inexpensive), molecular techniques, & total laboratory automation
What’s the difference between a transfusion and blood bank dept.?
Transfusion | Blood bank |
Transfusion services = clinical lab, typing patients, crossmatching to units, handles the issues of blood products for transfusion (where donor samples go to) Type and screen
Antibody screening
Issue blood products
Special testing
| Blood bank = segregated lab
|