Biology 30 - Unit 3 Booklet 1: Reproduction (Questions)
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
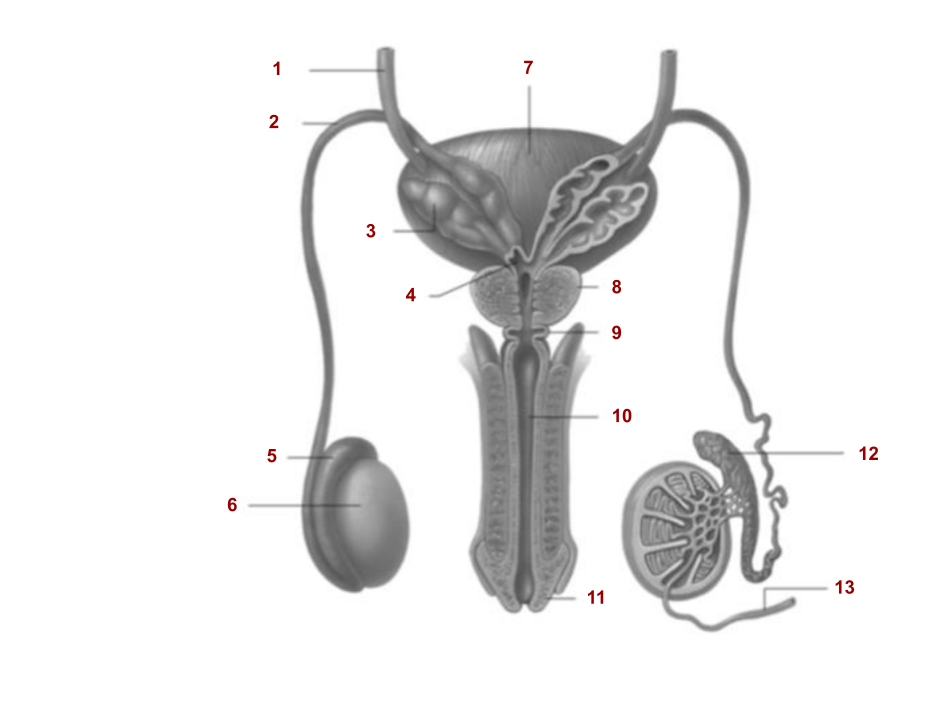
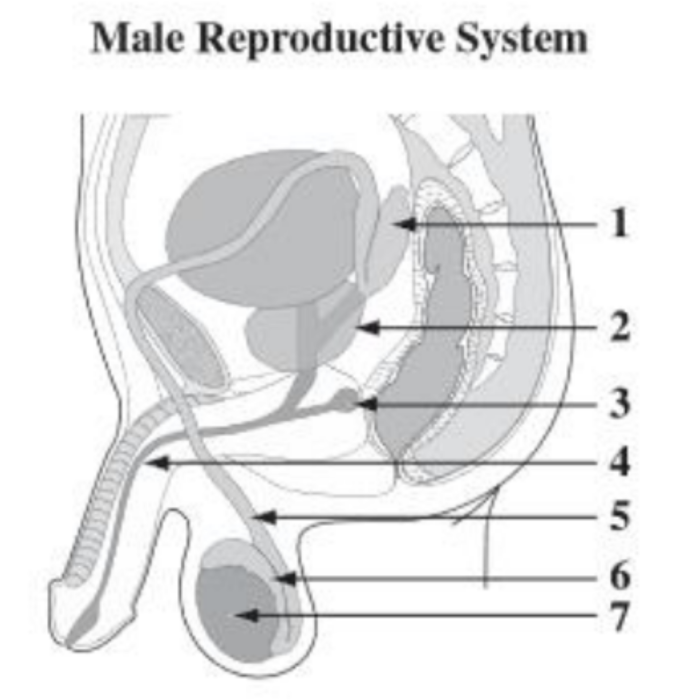
1
Ureter
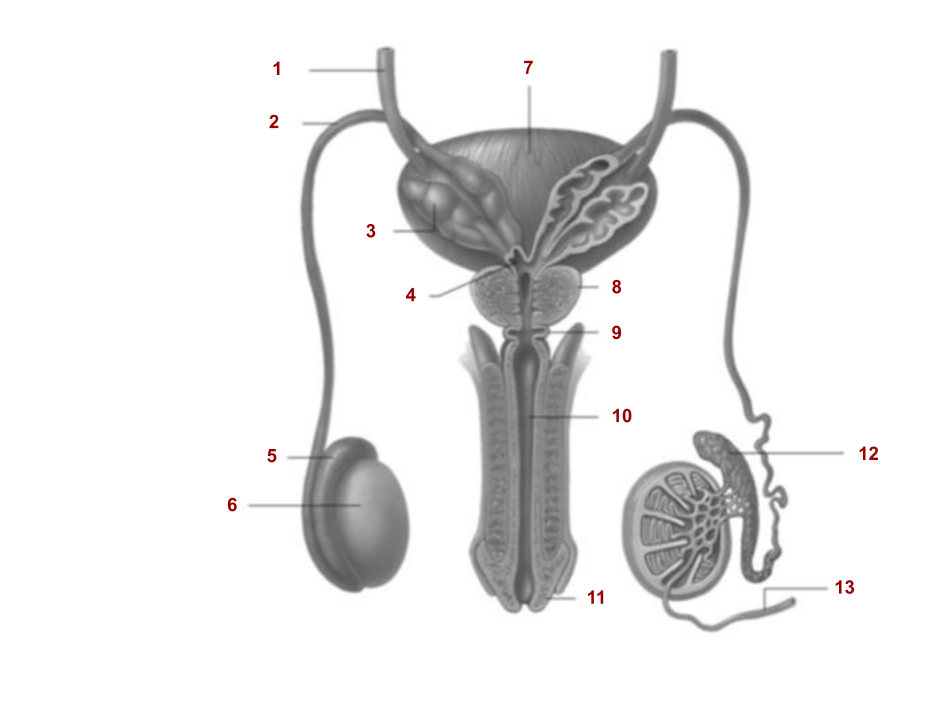
2
Vas Deferens
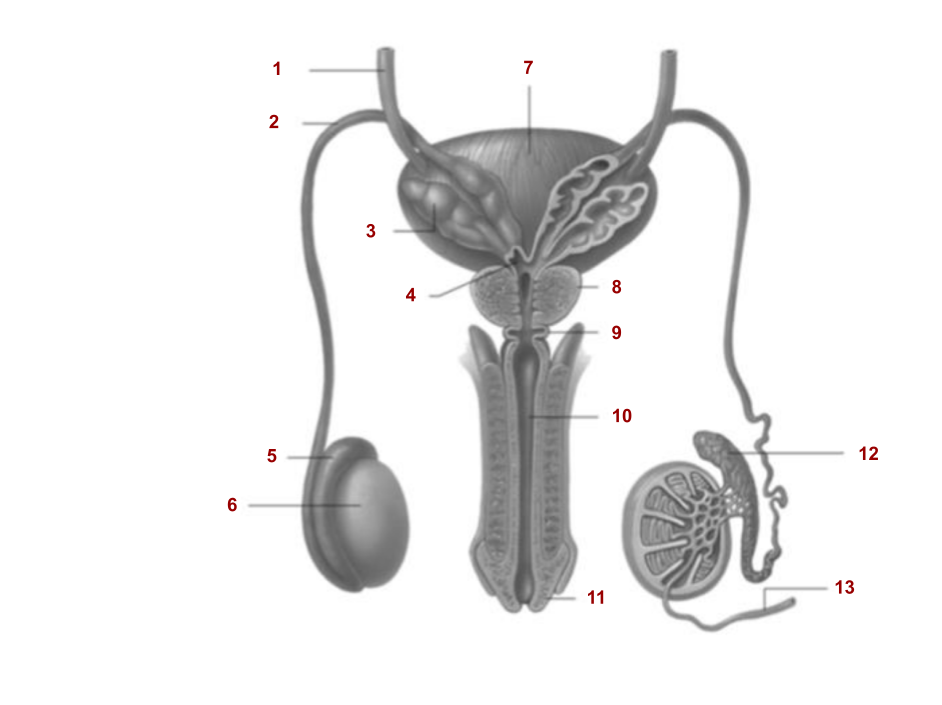
3
Seminal Vesicle
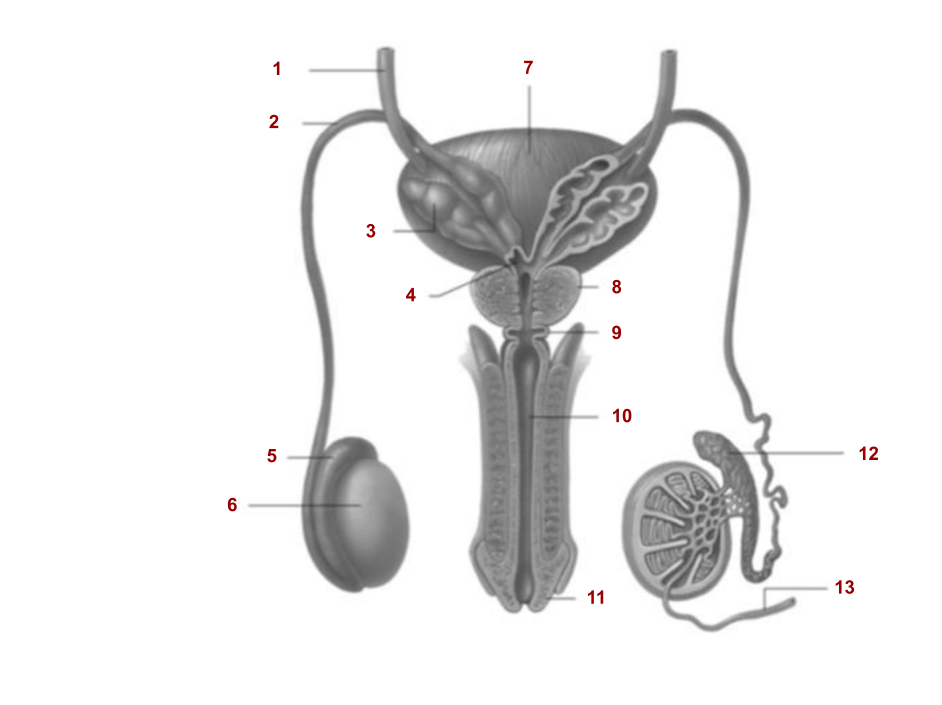
4
Ejaculatory Duct
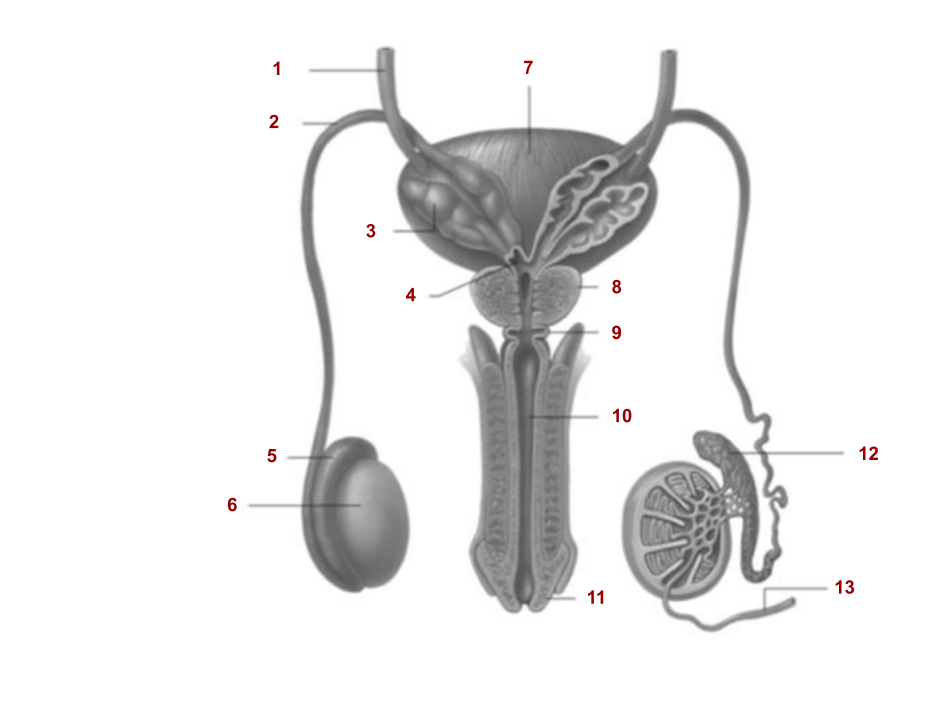
5
Epididymis
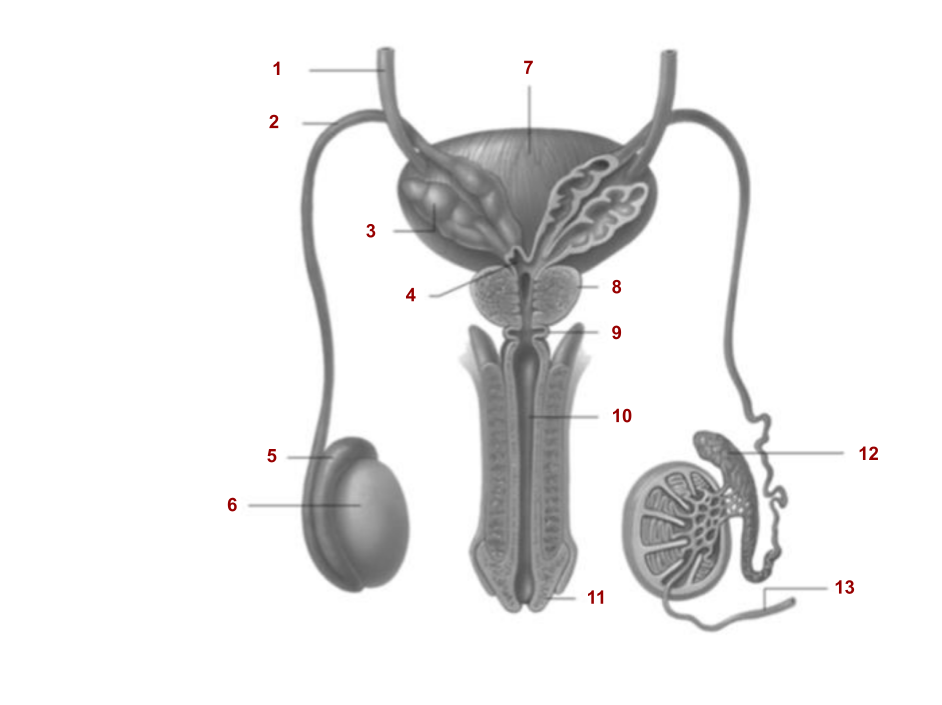
6
Testes
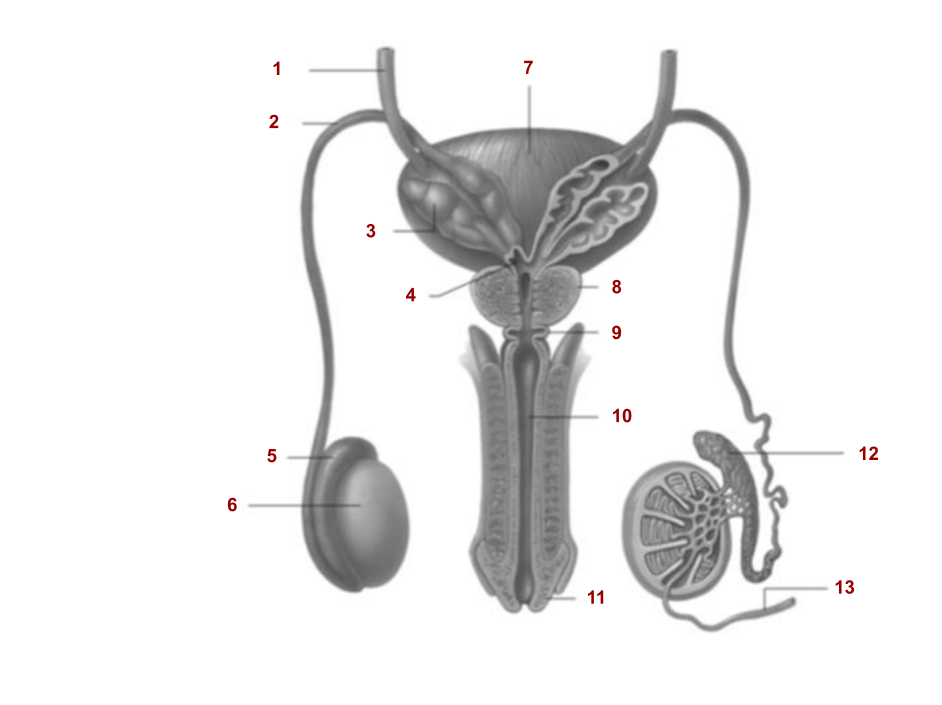
7
Urinary bladder
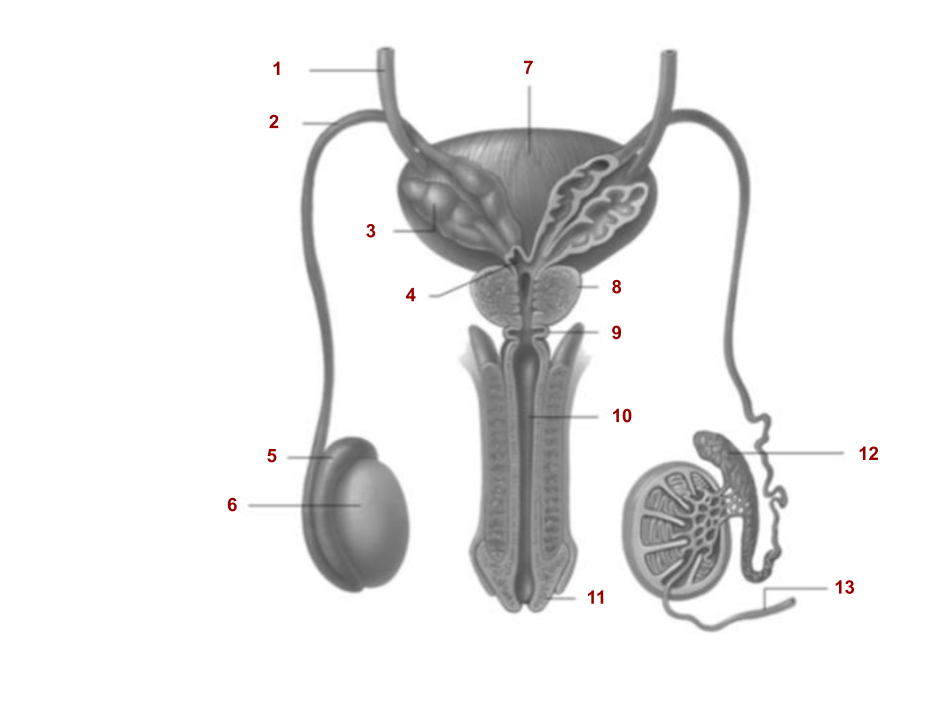
8
Prostate gland
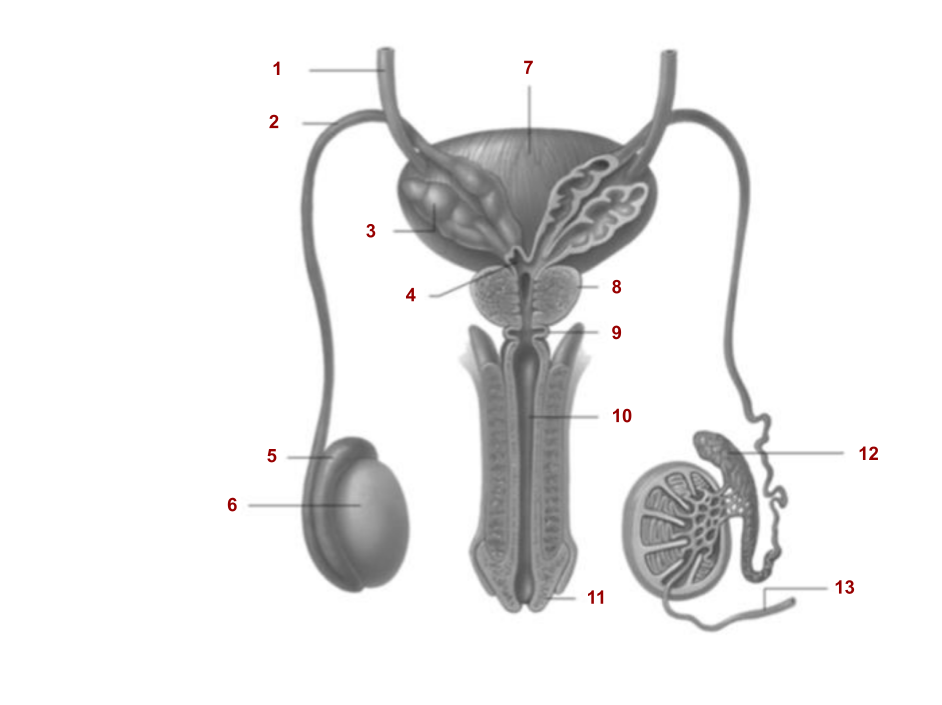
9
Cowper’s gland
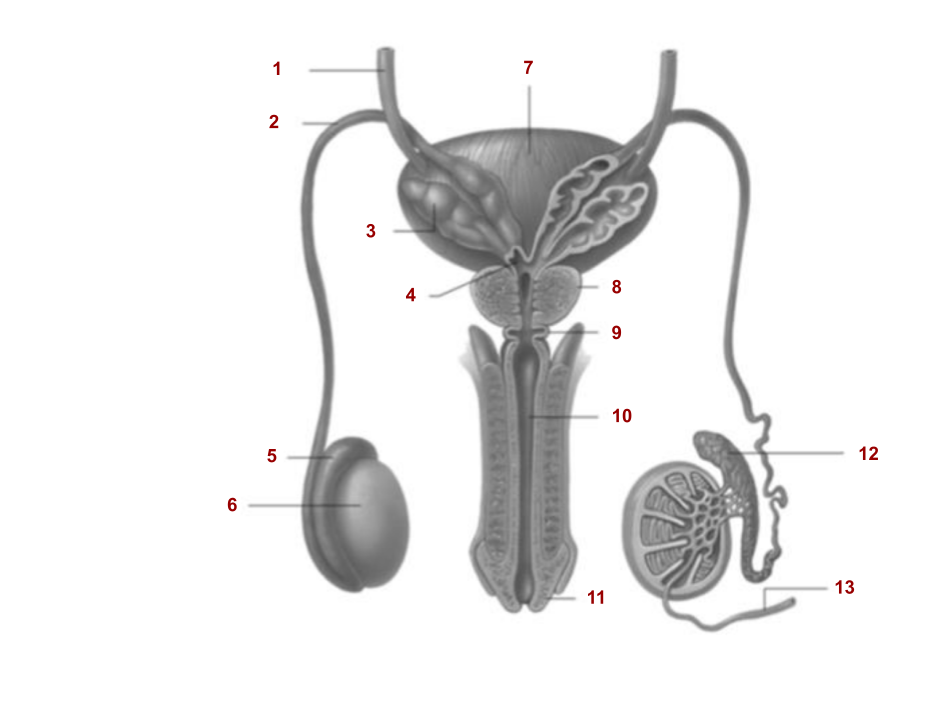
10
Urethra
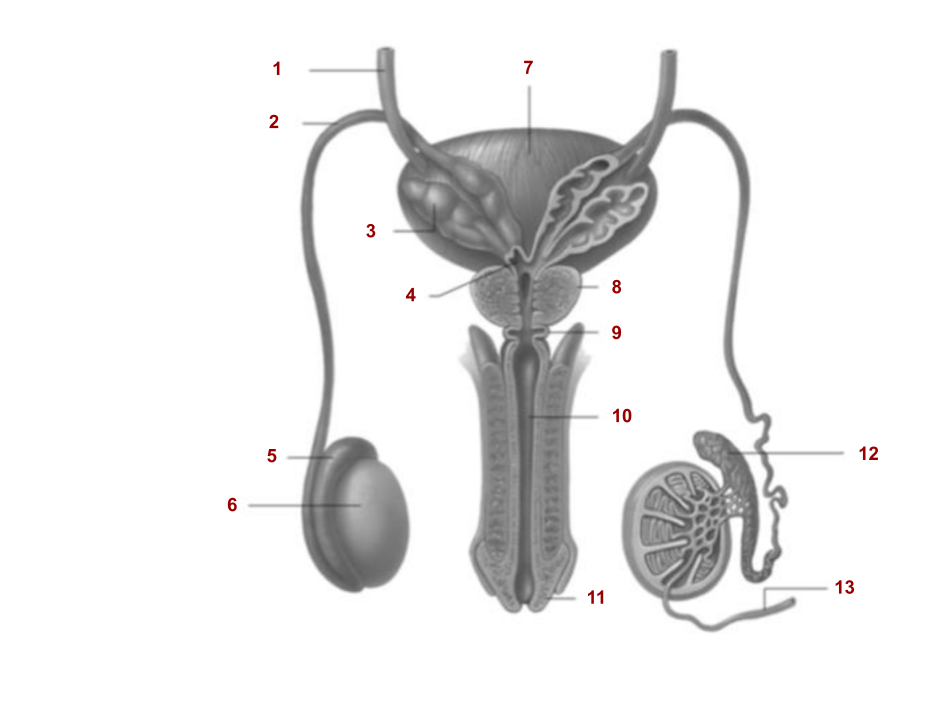
11
Glans penis
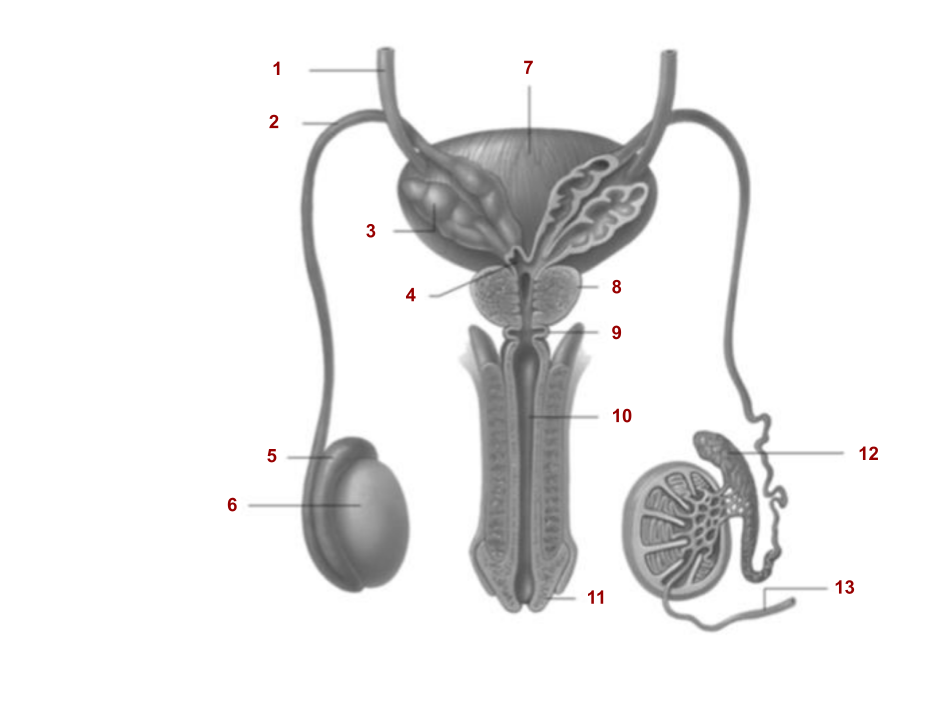
12
Epididymis
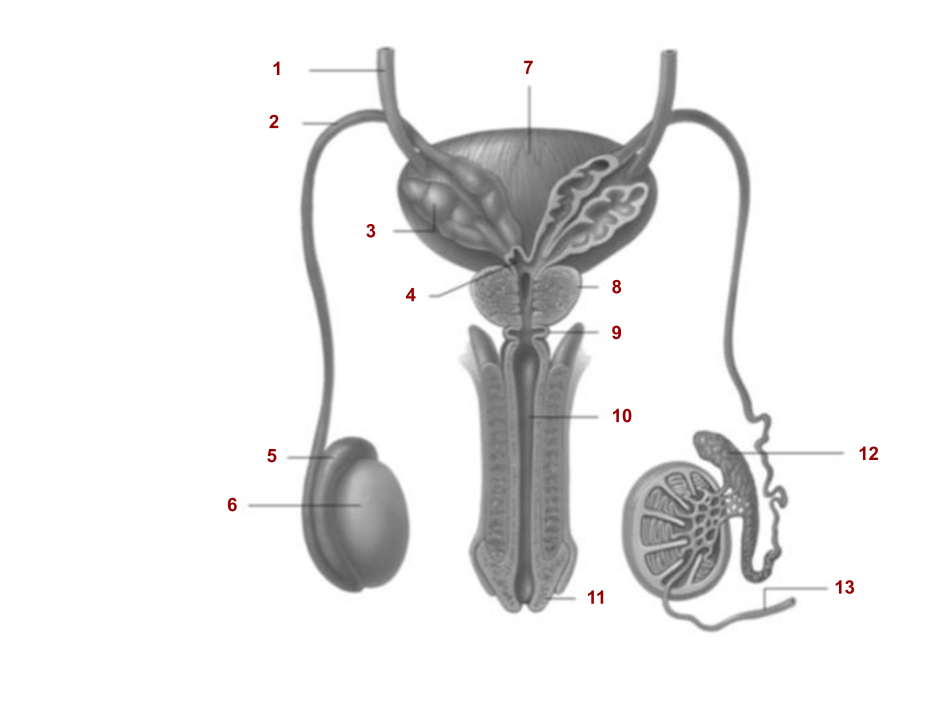
13
Seminiferous tubules
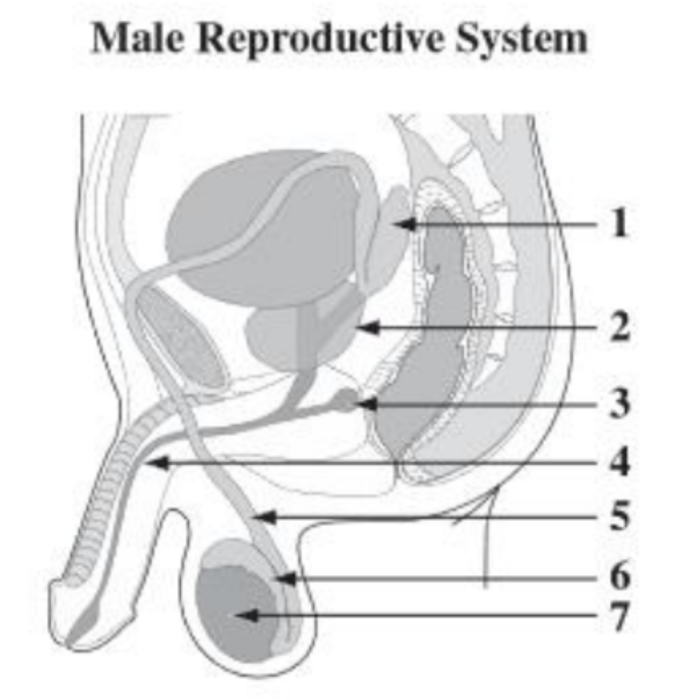
1
Seminal vesicle
2
Prostate gland
3
Cowper’s gland
4
Urethra
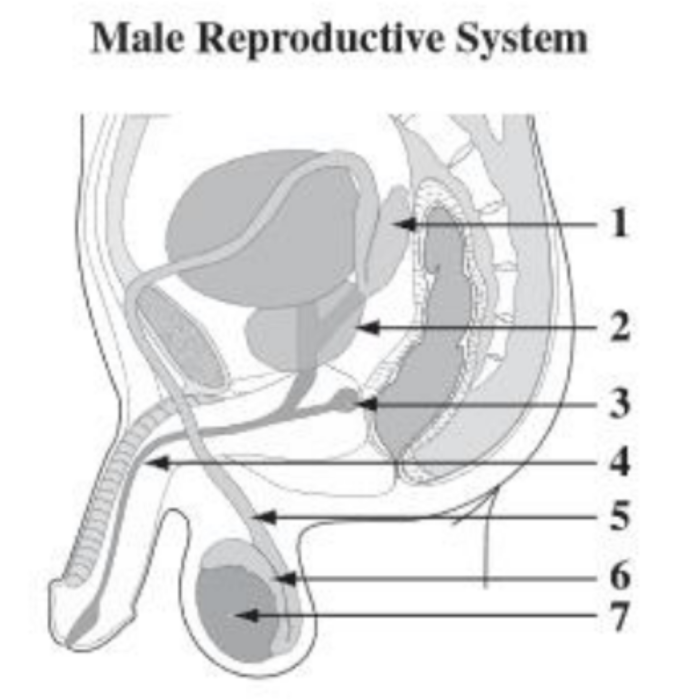
5
Vas deferens
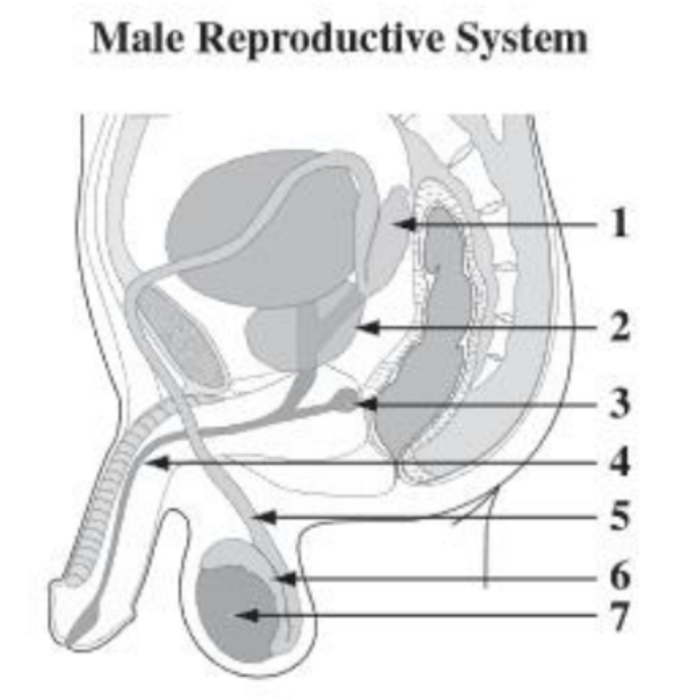
6
Epididymis
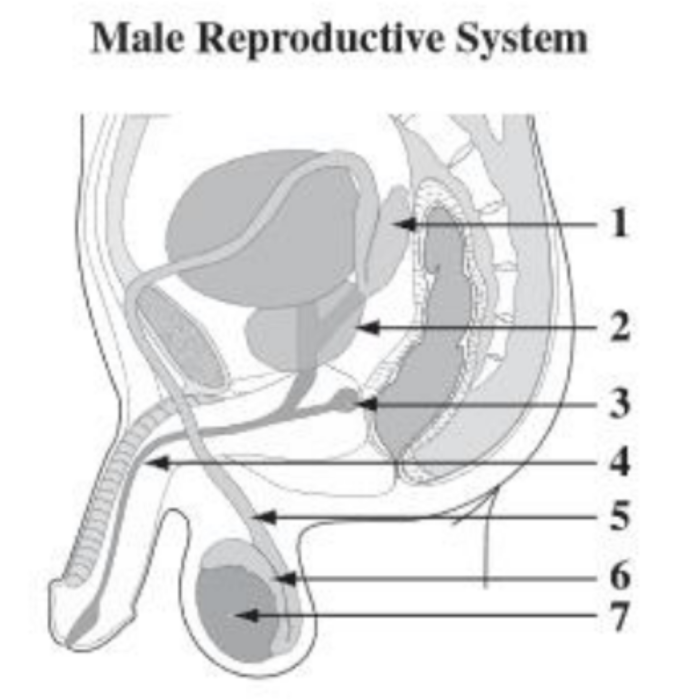
7
Testes
What temperature does the testes need to be and why?
3 degrees celsius below normal body temperature because any temperatures higher will kill sperm
How mature is a sperm cell when it leaves the testes?
Not fully mature, not motile yet
Describe the process of spermatogenesis.
Diploid spermatogonia found on the walls of the seminiferous tubules, which may divide by mitosis to produce more spermatogonia, transform into diploid primary spermatocytes. Spermatocytes go through meiosis to produce four haploid spermatids that then differentiate into sperm by losing most of their cytoplasm and gaining motility
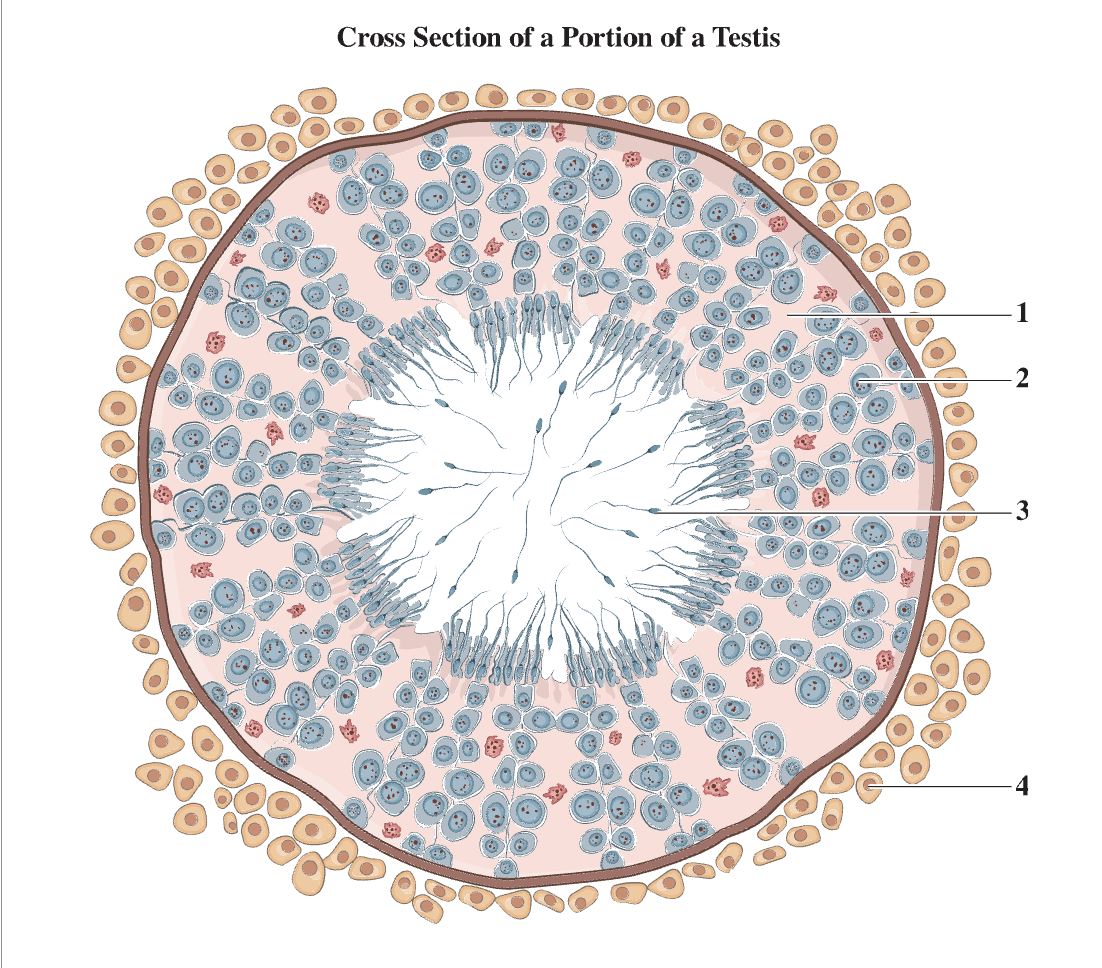
1
Spermatogonium
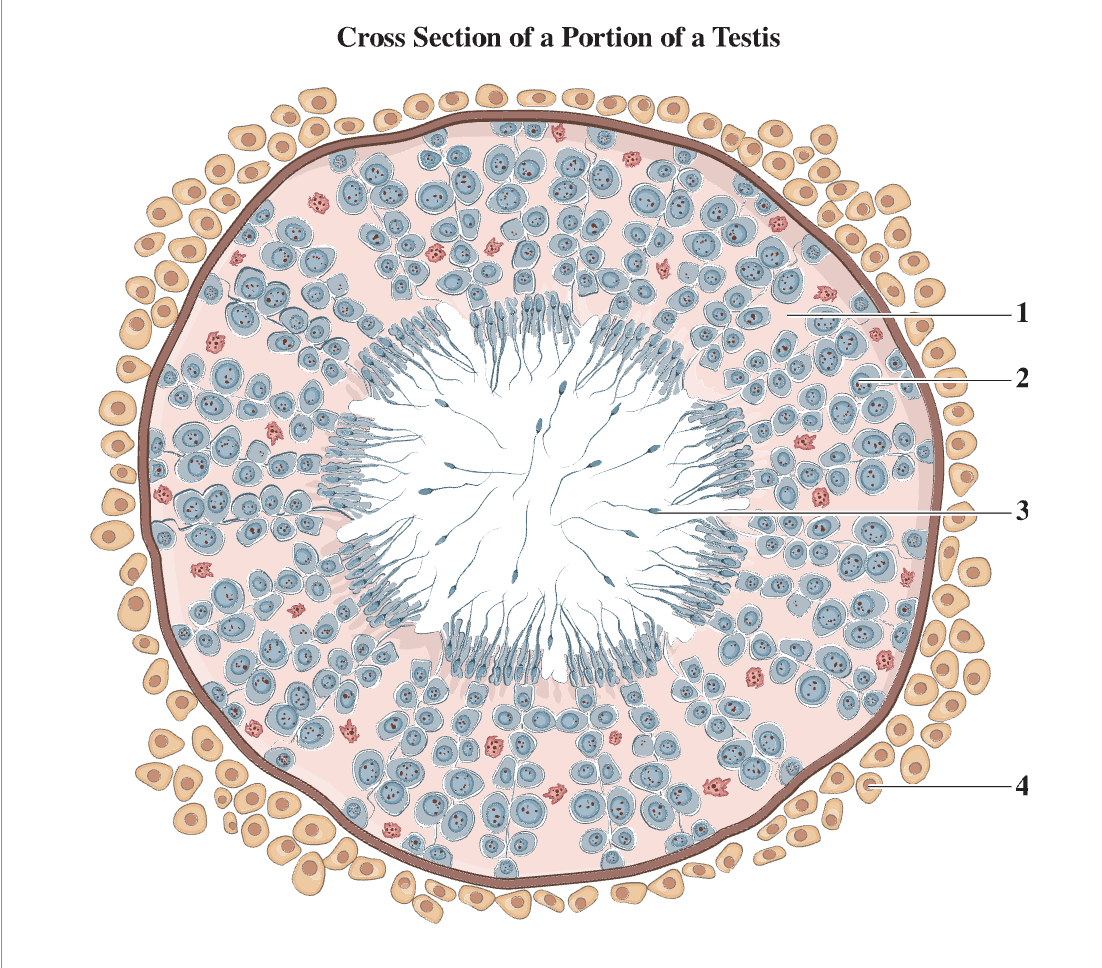
2
Spermatocyte
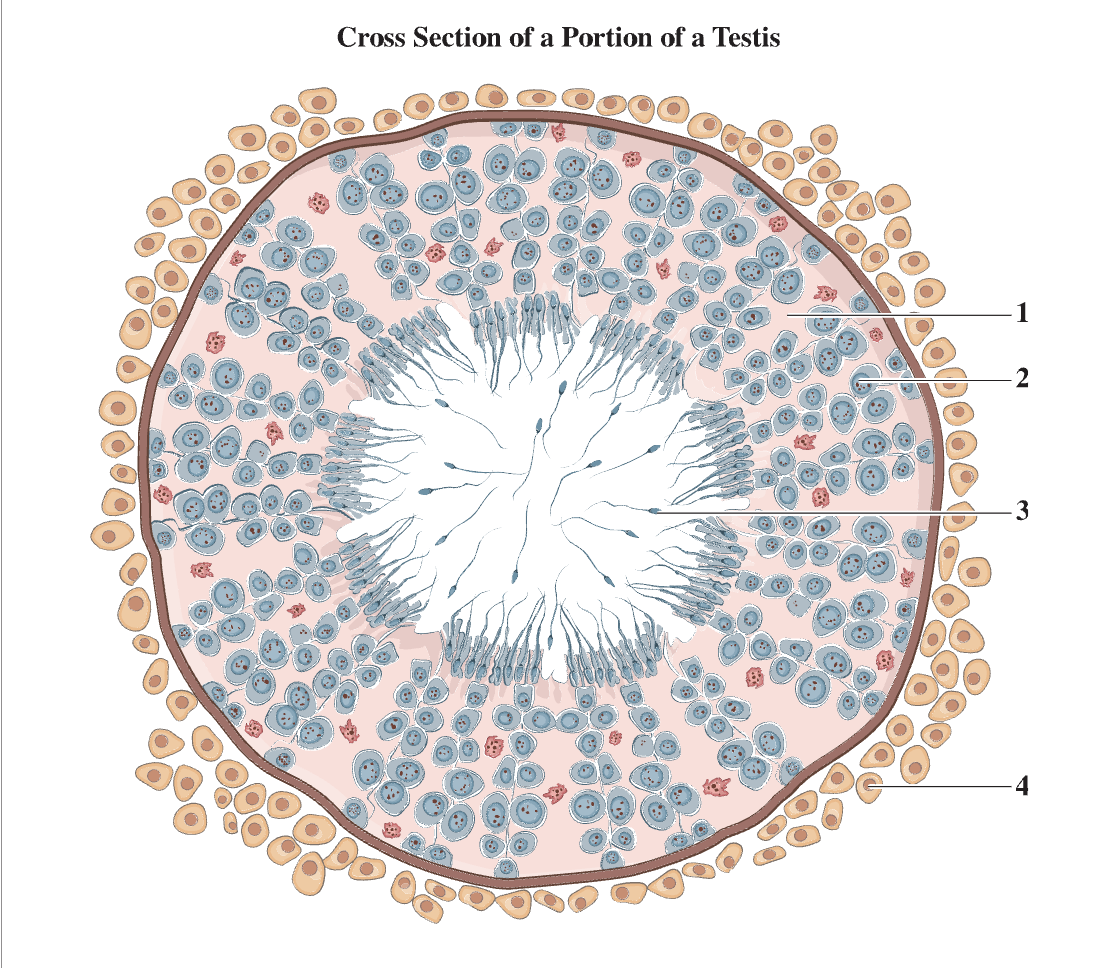
3
Sperm cell
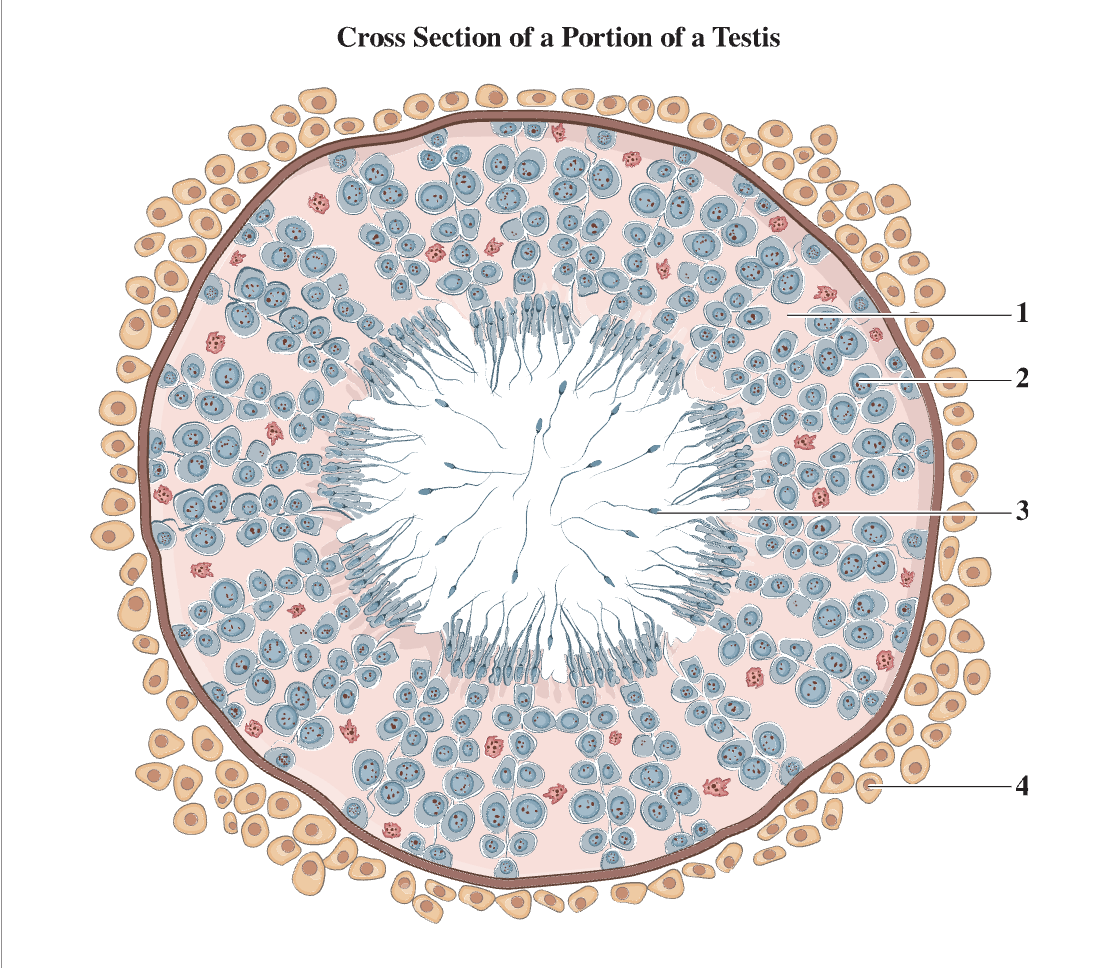
4
Interstitial cell
How mature is a sperm cell when it leaves the epididymis?
Fully mature, motile
What occurs from the blockage of the vas deferens?
Prevention of sperm movement from testes to external environment
What is the route taken by sperm from conception to ejaculation?
Sperm in the testes/seminiferous tubules go to the epididymus to be fully matured. They then are expelled to the vas deferens, which carries sperm from the testes to the inside of the body. They arrive at the ejaculatory duct, where sperm mixes with ejaculatory fluid from the cowper’s gland, seminal vesicle, and prostate gland. They then arrive at the urethra, and the ejaculatory fluid containing sperm leaves the penis
What is the fluid excreted from the seminal vesicle (elements and their uses)?
Contains fructose for sperm energy and prostaglandins that stimulate uterine peristalsis in females to help move semen up the uterus
What is the fluid excreted from the prostate gland (properties of elements)?
Liquifies the semes to prevent the sperm from clumping together and is alkaline to neutralize acid from residual urine in the urethra and the natural acidity of the vagina
What is the fluid excreted from the Cowper’s gland (properties, elements contained)?
Lubricates penis and vagina and protects sperm from the acidic vagina, may contain some sperm
How does an erection happen (nervous systems involved, biological processes)?
During sexual arousal, the parasympathetic nervous system causes erectile tissue (spongiosum) to fill with blood from the arteries. The pressure seals off the veins and the urethra, preventing blood from draining out and pee from entering
How does ejaculation happen (nervous systems involved, biological processes)?
The sympathetic nervous system will initiate seminal fluid to enter the urethra pushed out by smooth muscle contractions
Describe the negative feedback of spermatogenesis.
When sperm is needed, the hypothalamus releases GnRH, causing the anterior pituitary to release FSH to the sertoli cells in the seminiferous tubules. As a result, spermatogenesis is stimulated. The production of sperm releases inhibin, turning off the hypothalamus to prevent excess sperm production
Describe the negative feedback of testosterone production.
When testosterone is needed, the hypothalamus releases GnRH, causing the anterior pituitary to release LH to the interstitial cells. As a result, testosterone production is stimulated. The production of testosterone turns off the hypothalamus to prevent excess testosterone production
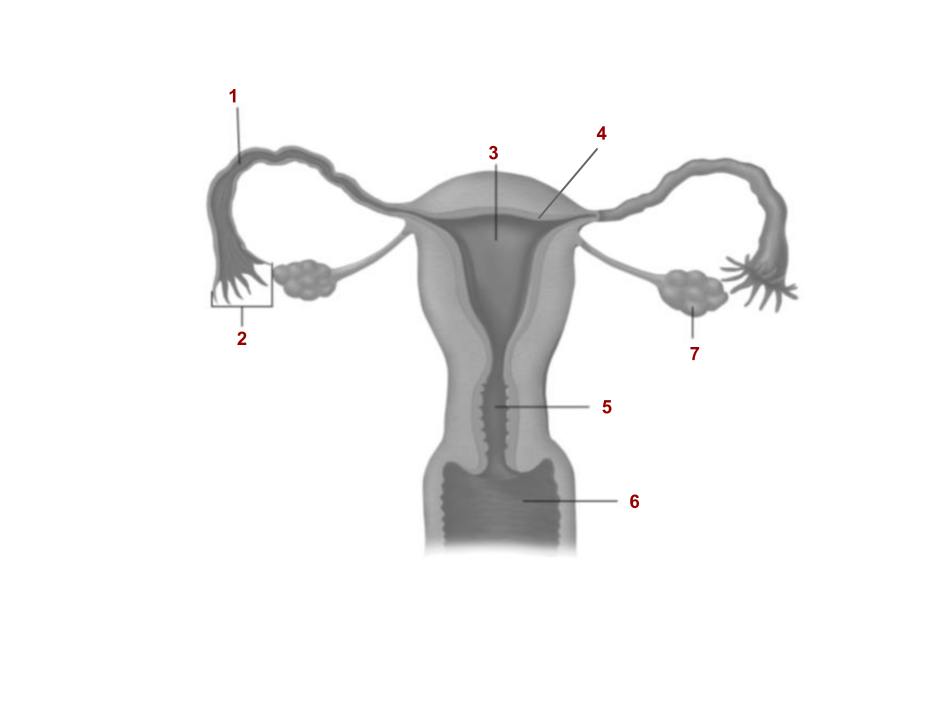
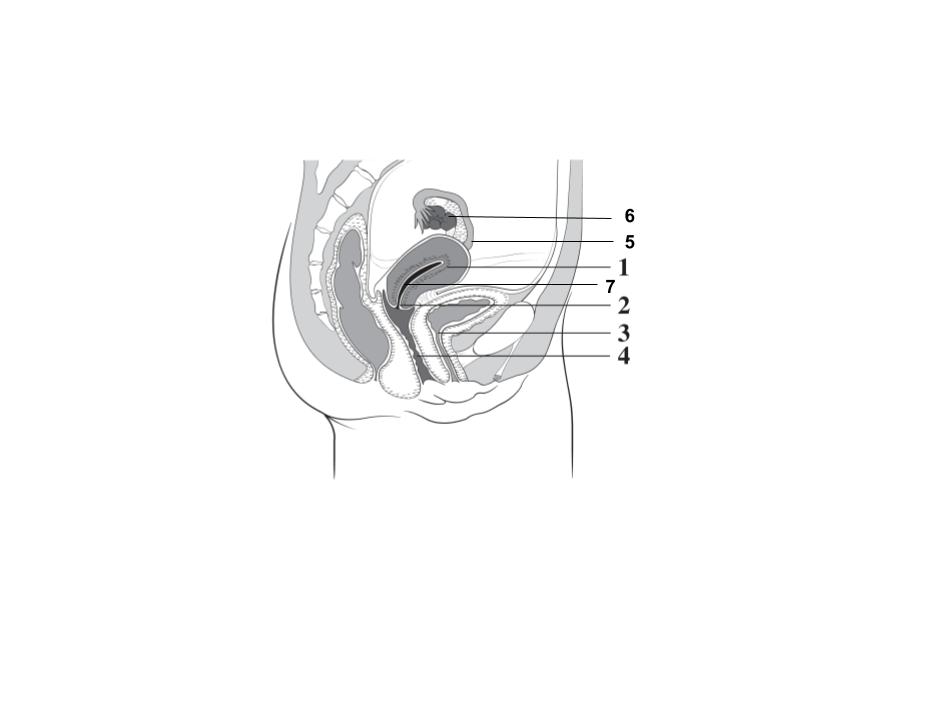
1
Fallopian tube
2
Fimbria
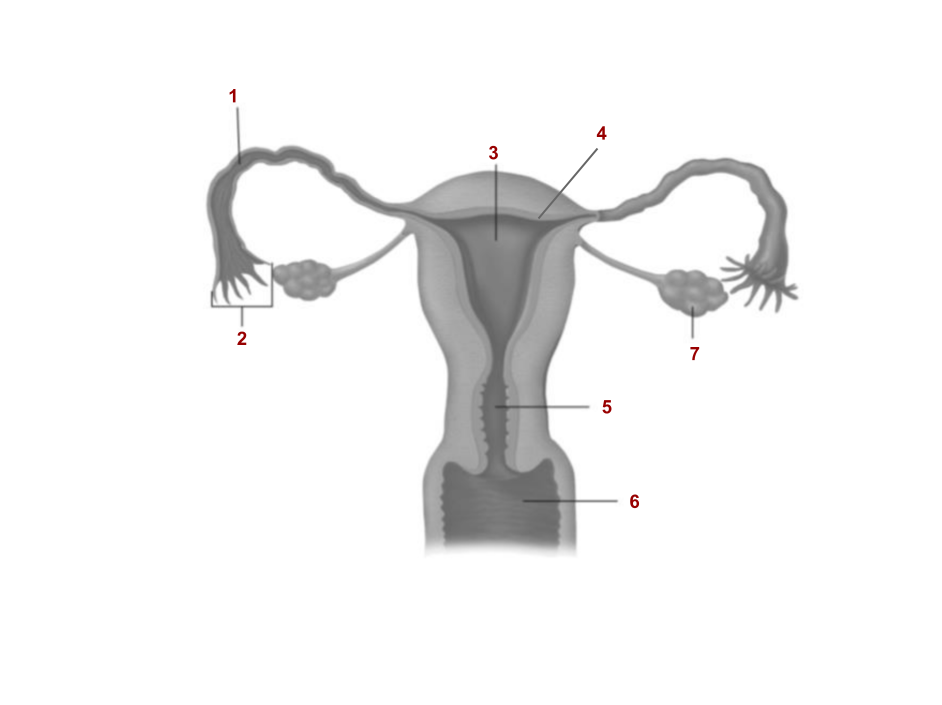
3
Uterus
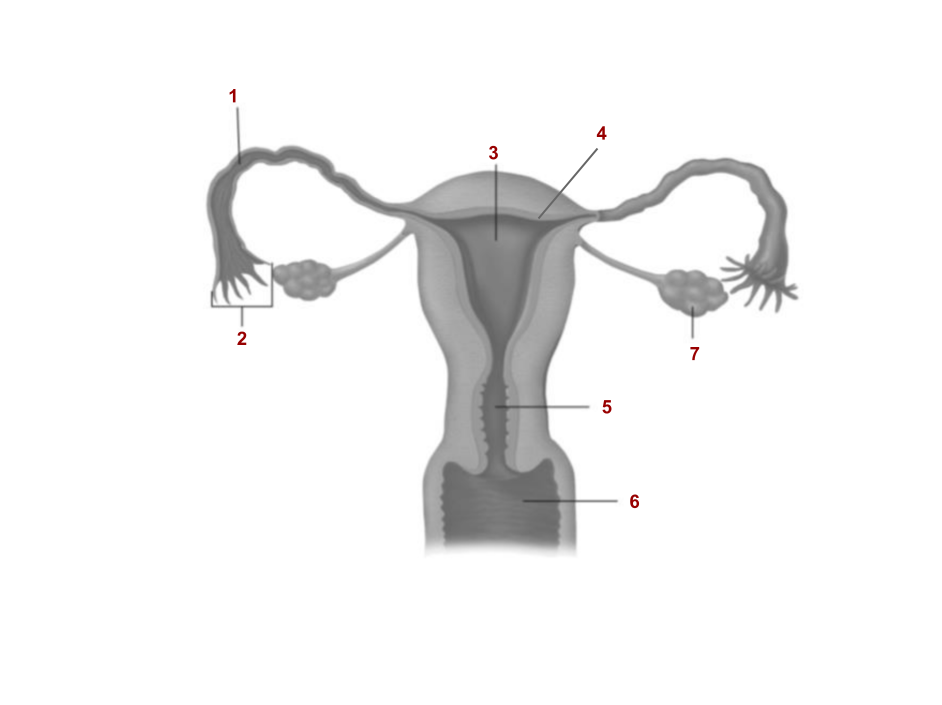
4
Endometrium
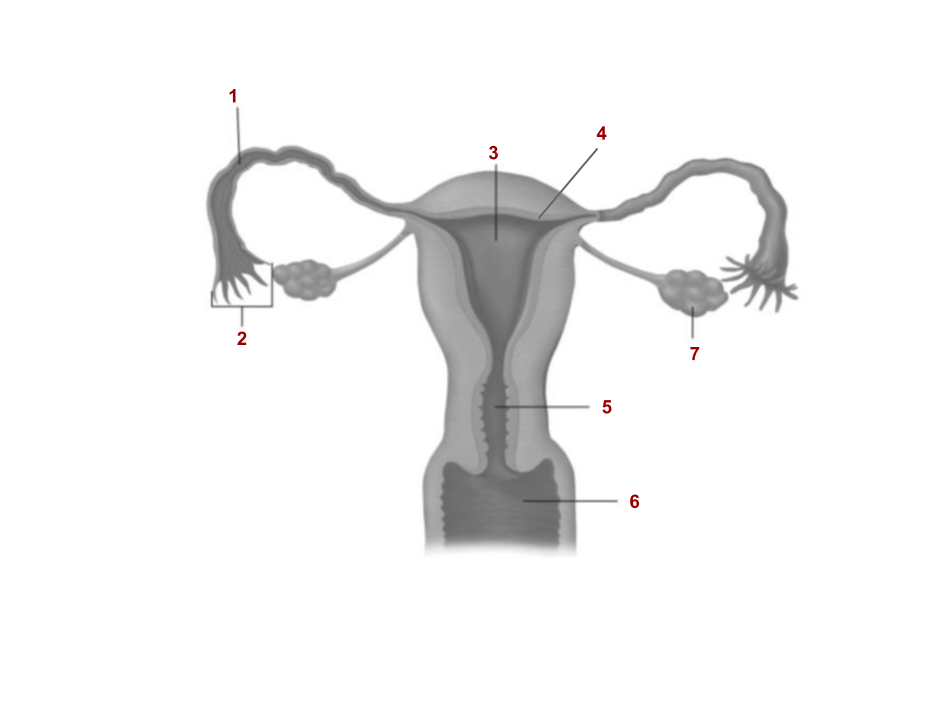
5
Cervix
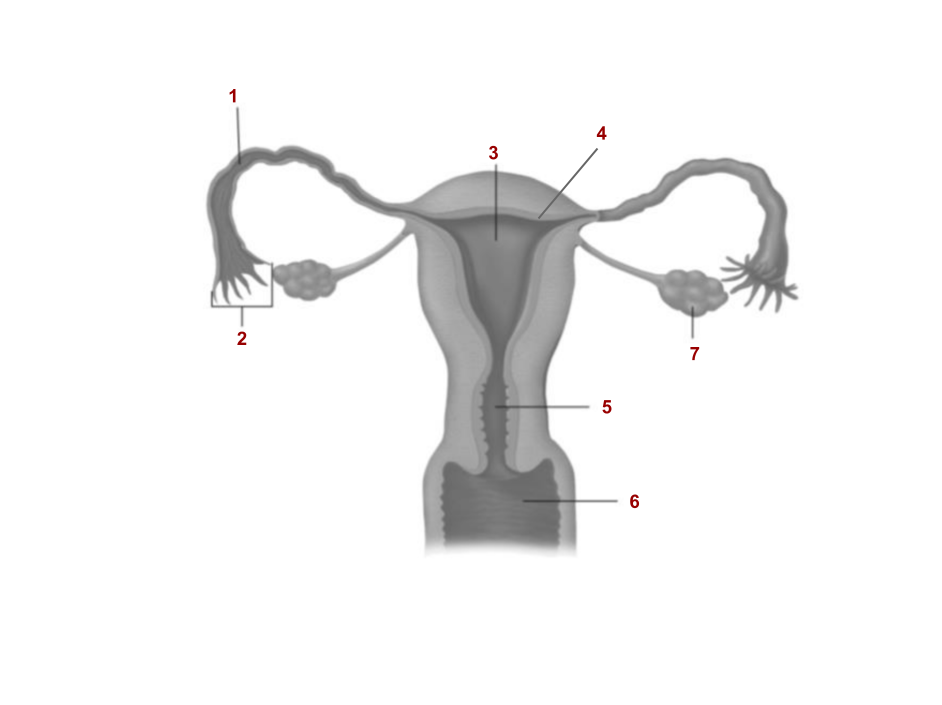
6
Vagina
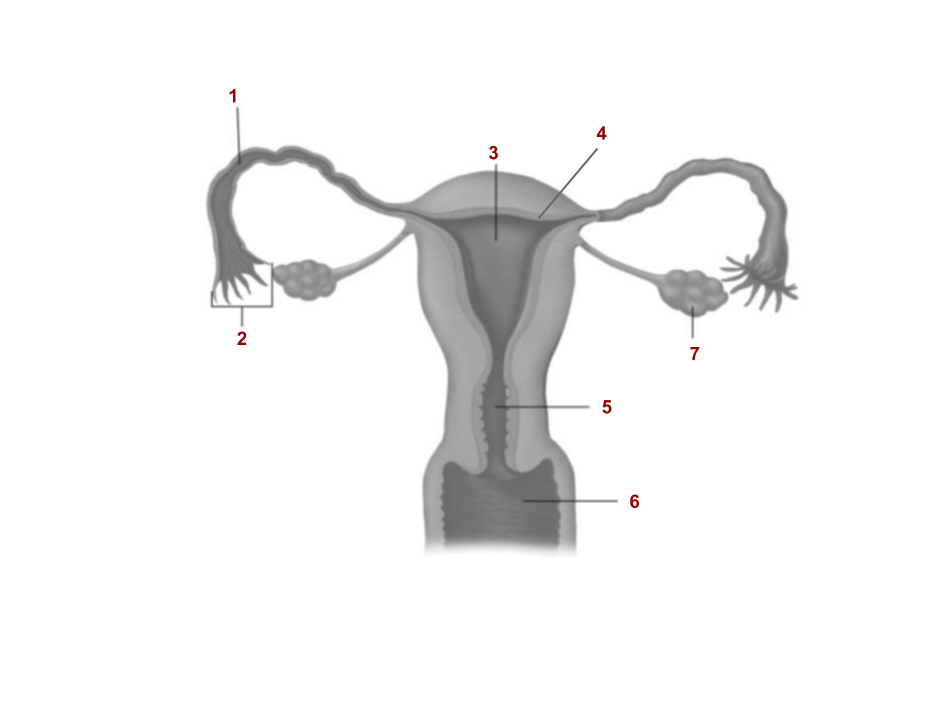
7
Ovary
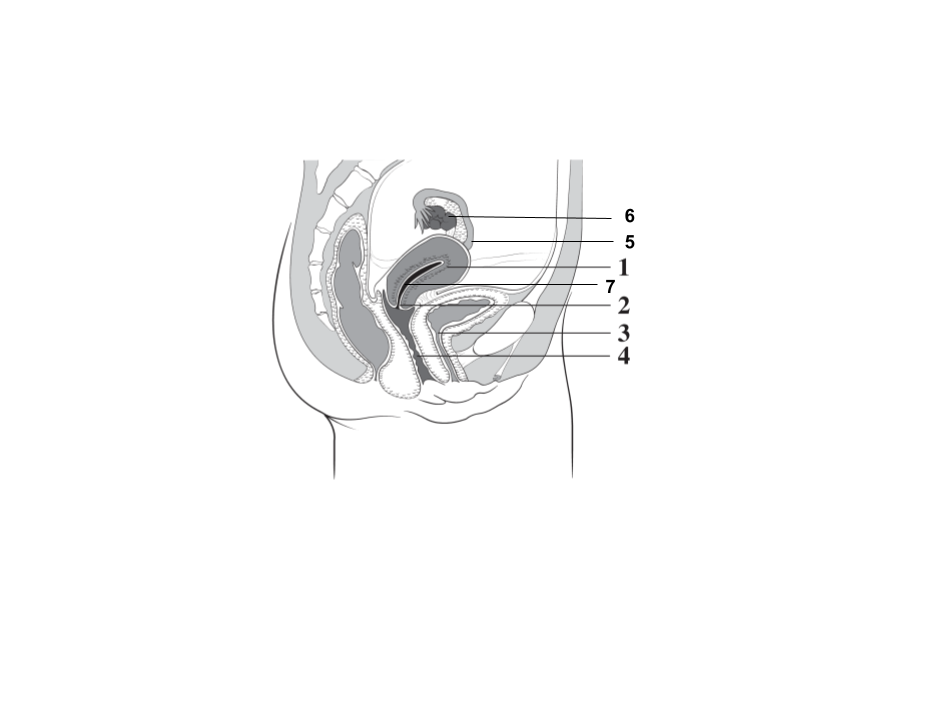
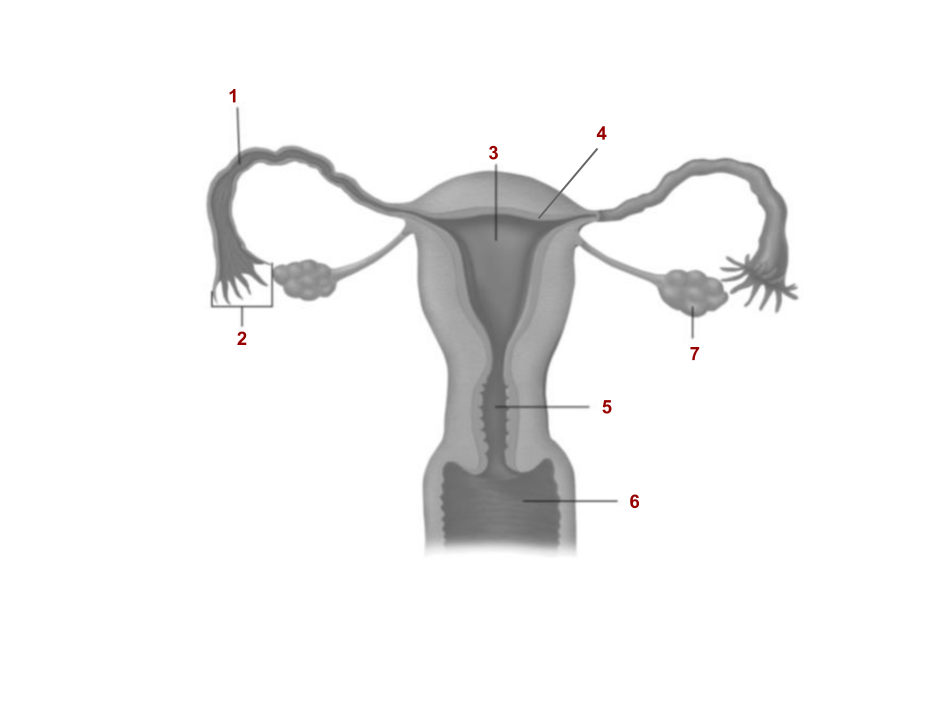
1
Endometrium
2
Cervix
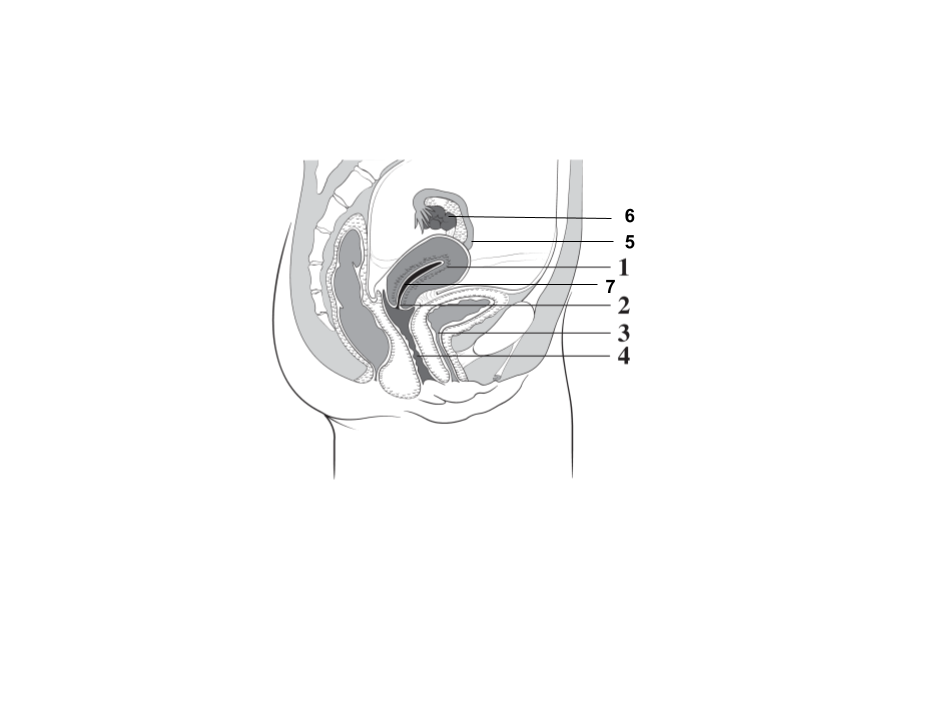
4
Vagina
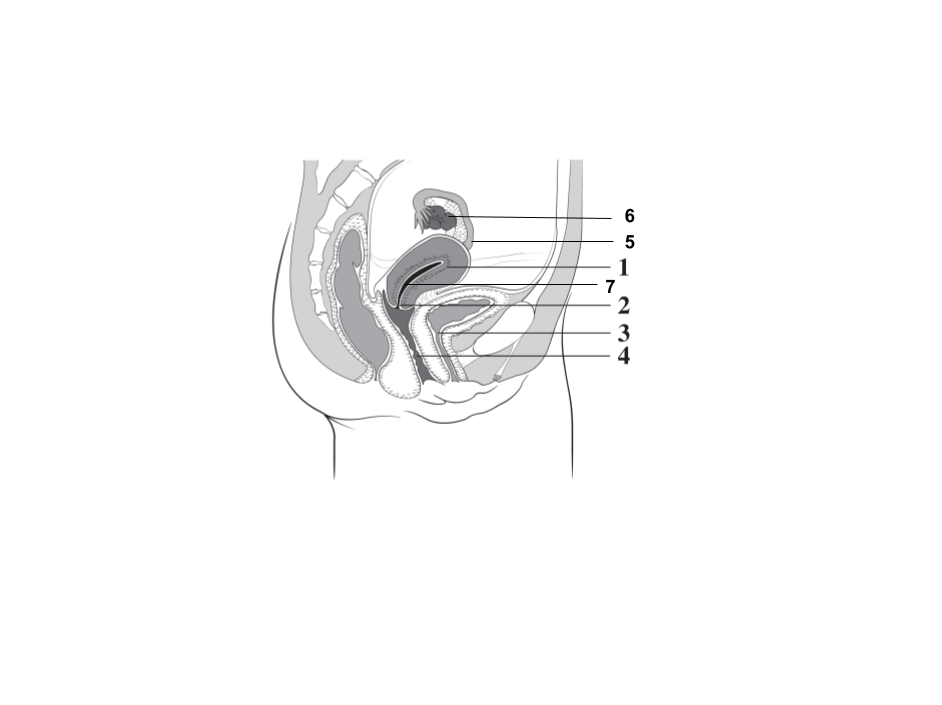
5
Fallopian tube
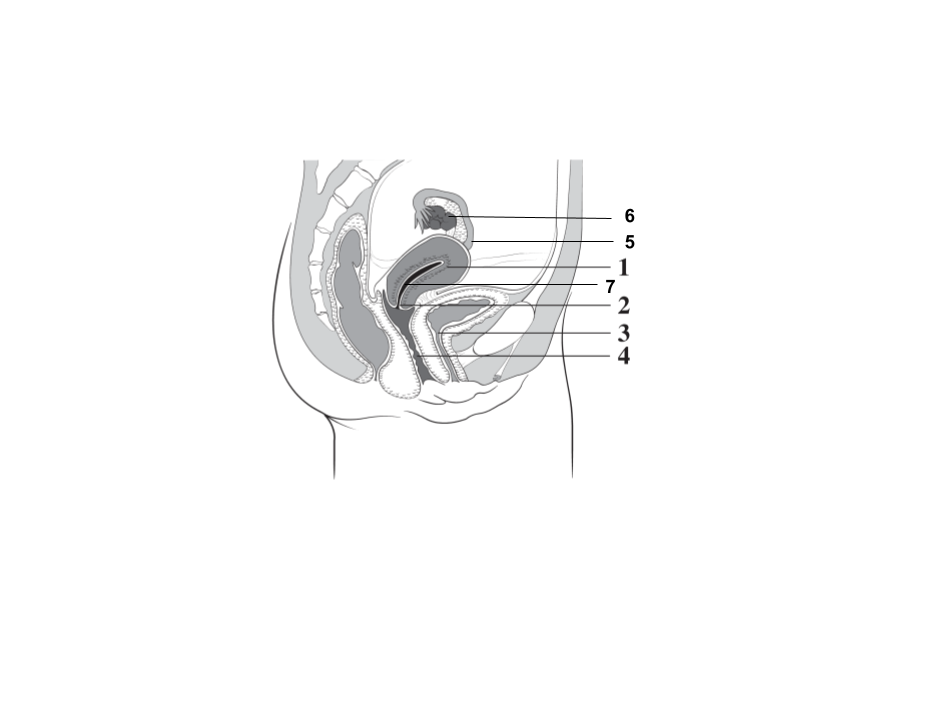
6
Ovary
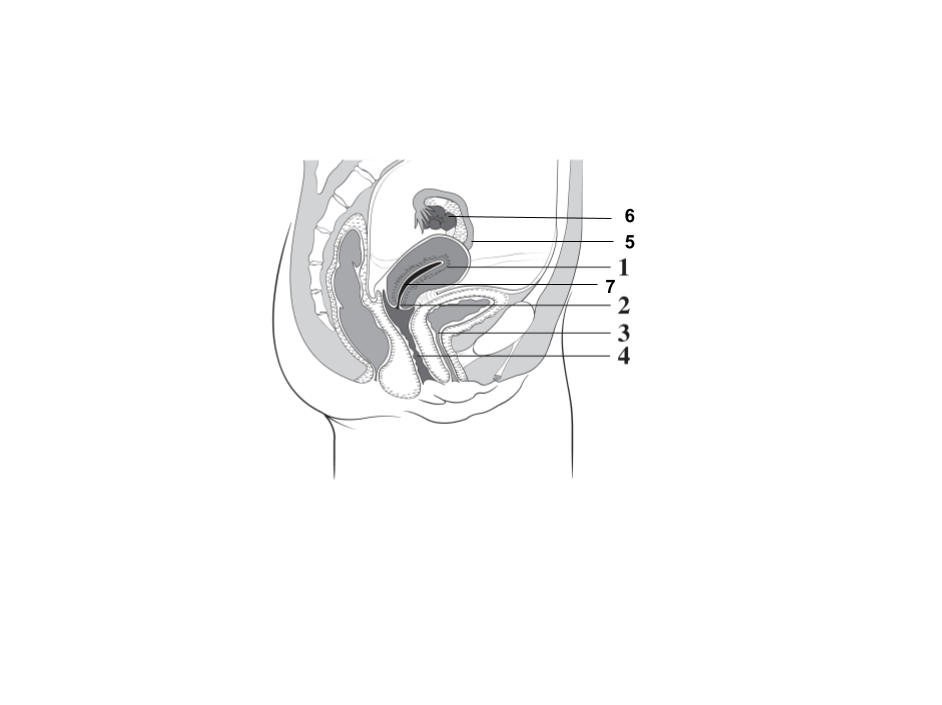
7
Uterus
What external genitalia is found in the female reproductive system?
Two sets of labia (labia major and labia minora) that surround the clitoris and vaginal opening
Describe the process of oogenesis.
Diploid oogonia found in the ovaries, which may divide by mitosis to produce more oogonia, transform into diploid primary oocytes. Primary oocytes grow larger and go through meiosis I to produce to produce a haploid secondary oocyte and a first polar body, remaining as such until the secondary oocyte is fertilized. After fertilization, meiosis II is completed and the secondary oocyte becomes a fertilized ovum and a second polar body
How are oogenesis and spermatogenesis similar?
Both sex cells begin as diploid stem cells and go through meiosis to become specialized haploid reproductive cells, both occur in the reproductive system
How are oogenesis and spermatogenesis different?
Spermatogenesis produces 4 sperm while oogenesis produces 1 ovum, equal division of cytoplasm in spermatogenesis but unequal distribution in oogenesis as most goes to ovum, and little goes to polar bodies
Why are fimbria and cilia needed?
The fallopian tubes don’t actually touch the ovaries, and so the egg is released into the abdominal cavity and needs to be assisted by fimbria and cilia to be sucked into the oviduct
What are the two layers of the endometrium and how are they different?
Basal layer is stable and does not change in thickness while the functional layer changes thickness with menstruation
What are the four phases of the female menstrual cycle?
Flow/menstrual phase, follicular phase, ovulation phase, luteal phase
Describe the flow phase of the female menstrual cycle (biological activity, days elapsed).
The shedding of the endometrium causes blood to flow out of the uterus. This marks day 1 of the cycle and can last 4-5 days.
Which hormones are present during the flow phase and why?
Low levels of all hormones due to estrogen and progesterone production in the luteal phase inhibiting GnRH production, thereby decreasing LH and FSH levels. Low hormone levels cause the flow phase to begin
Describe the follicular phase of the female menstrual cycle (biological activity, days elapsed).
This is a period of repair and thickening of the endometrium to prepare for possible fertilization in the upcoming ovulation phase. Follicle development is stimulated in the ovary, and the endometrium thickens. Occurs during day 6-13.
Which hormones are present during the follicular phase and why?
FSH levels increase in order to stimulate follicle development. The developing follicle produces rising estrogen levels
Describe the ovulation phase of the female menstrual cycle (biological activity, days elapsed).
The follicle reaches its maximum size and bursts, causing the secondary oocyte to be released. Occurs on day 14.
Which hormones are present during the ovulation phase and why?
FSH is at its highest because the development of the follicle has been stimulated to its max. LH is also at its highest because high levels of LH cause ovulation to occur. Estrogen is at its highest because the follicle has grown to its largest and has released the maximum amount of estrogen.
Describe the luteal phase of the female menstrual cycle (biological activity, days elapsed).
Stage of final preparation of the endometrium to receive a fertilized ovum. Corpus lutem develops and produces hormones essential for pregnancy. Occurs from day 14 to day 28.
Which hormones are present during the luteal phase and why?
LH (lower levels than ovulation but high enough to develop corpus lutem) stimulates the development of the corpus luteum. Corpus luteum creates progesterone, causing progesterone levels to spike. Estrogen is also created in low levels by the corpus luteum. Estrogen and progesterone inhibit GnRH production, thereby decreasing LH and FSH levels and initiating the flow phase
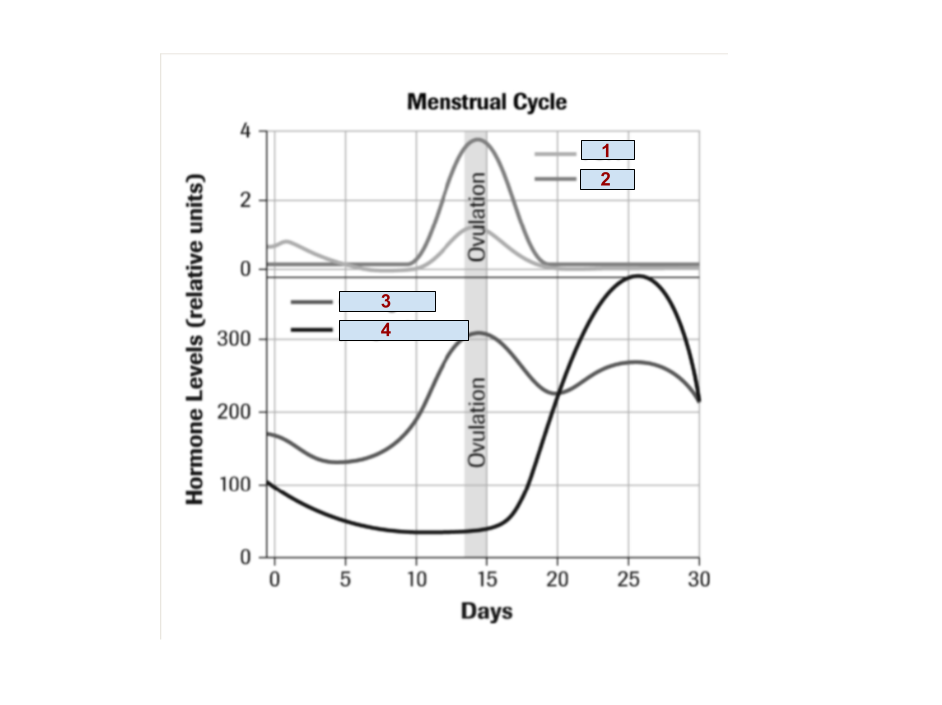
1
FSH
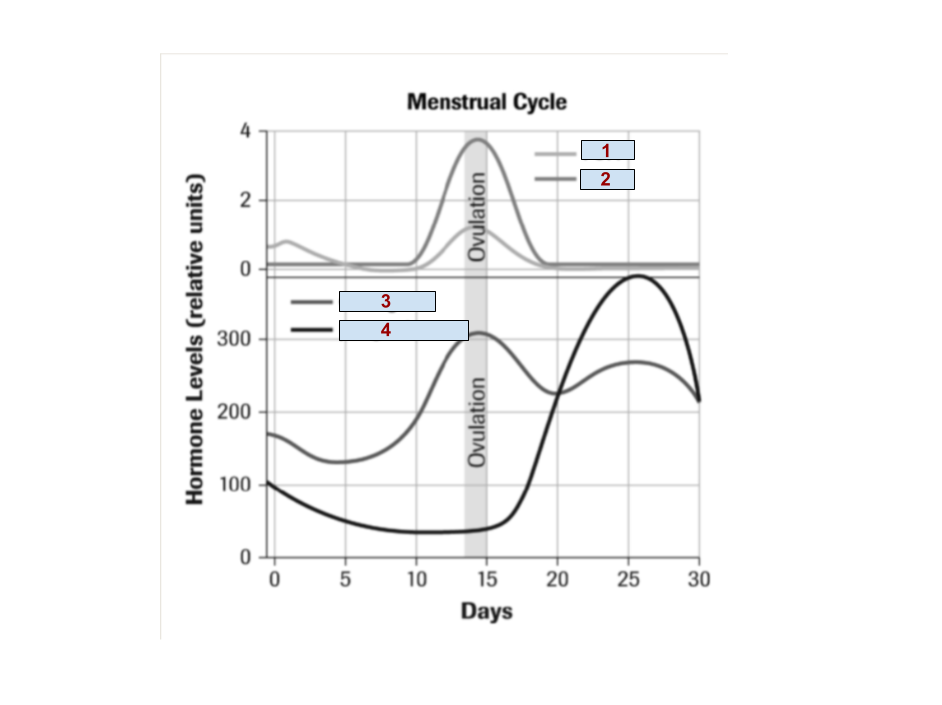
2
LH
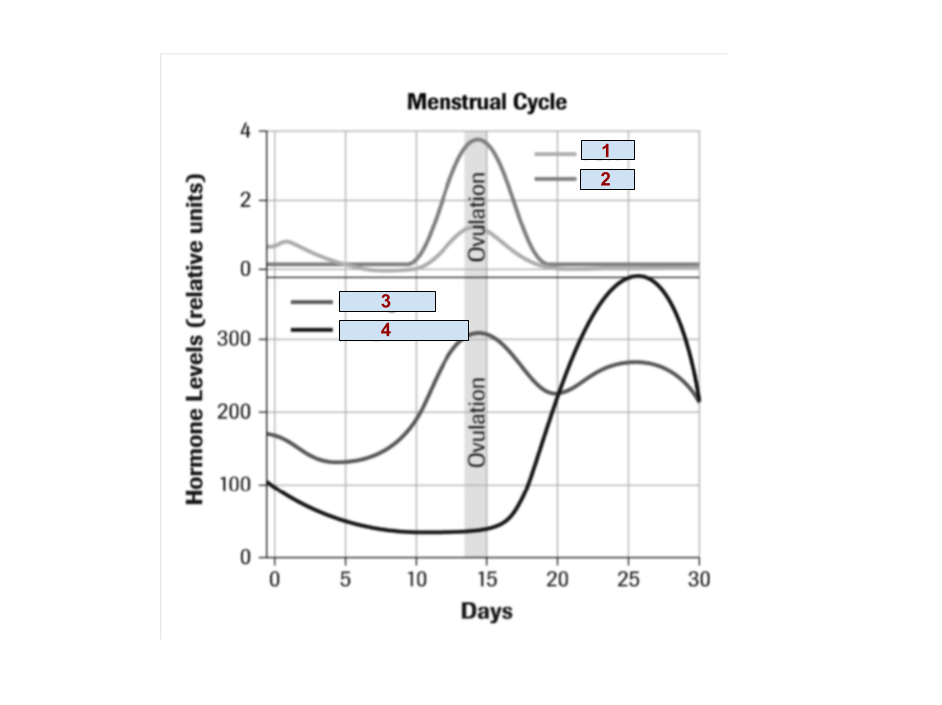
3
Estrogen
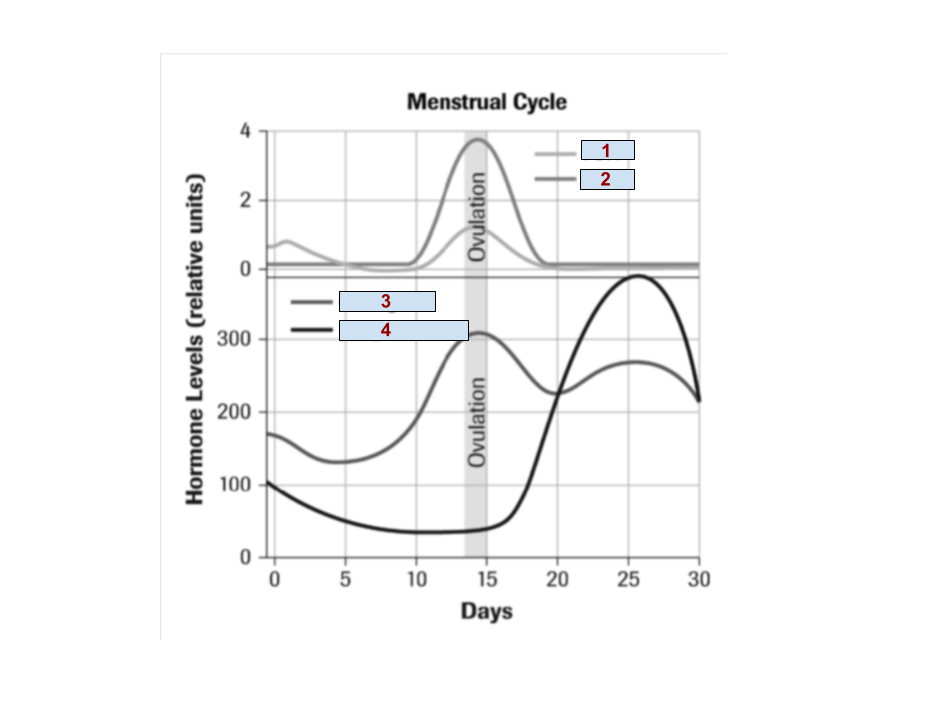
4
Progesterone
Describe the negative feedback of endometrium development.
During the follicular phase, the hypothalamus releases GnRH, causing the anterior pituitary to release FSH to the follicle in the ovary. As the follicle develops, estrogen is produced, which develops the endometrium and also develops secondary sex characteristics. The production of estrogen shuts off GnRH production, which shuts off FSH production to prevent excess estrogen production
Describe the negative feedback endometrium maintenance.
During the luteal phase, the hypothalamus releases GnRH, causing the anterior pituitary to release LH to the corpus luteum in the ovary. As the corpus luteum develops, progesterone is produced, which maintains the endometrium. The production of progesterone shuts off GnRH production, which shuts off LH production to prevent excess progesterone production