human anatomy and physio - module 5
1/126
Earn XP
Description and Tags
musculoskeletal system
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
127 Terms
Functions of the skeletal system
Support
Protection
Assistance in movement
Mineral homeostasis
Blood cell production
Triglyceride storage
Functions of the skeletal system - support
The skeleton provides a rigid framework for other elements to connect to. It therefore gives structural support to other anatomy
Functions of the skeletal system - protection
Bone is hard, dense and strong. It commonly provides a shield for deeper, vital organs in order to protect them. Think of the skull surrounding the brain, or the rib cage surrounding the lungs and heart
Functions of the skeletal system - mineral homeostasis
Osseous tissue has a high concentration of a few important minerals, such as calcium and phosphorus. When levels of these minerals in our bodily fluids are low, they can be released from the bone to boost their concentration in our body fluids
When levels of these minerals are high in the bodily fluids, we can take these minerals from the fluids and store them in the bones
Functions of skeletal system - blood cell production
Many bones have a type of tissue inside them called the red bone marrow. It is in this tissue that new blood cells are created
Red bone marrow is red due to the high density of blood vessels in it
Functions of the skeletal system - triglyceride storage
Some bones have another type of bone marrow called yellow bone marrow
Yellow bone marrow is a very fatty tissue and largely functions to store a certain type of lipid called a triglyceride
Triglycerides are a potential energy substrate our bodies can use to create ATP
Key cells in the skeletal system
Osteoblasts are the cells that synthesise and secrete much of the extracellular matrix of bone (osteo = bone)
Chondroblasts are the cells that synthesise and secrete much of the extracellular matrix of cartilage (chondro = cartilage)
Fibroblasts are the cells that synthesise and secrete much of the extracellular matrix of dense connective tissue (which is softer than bone and cartilage)
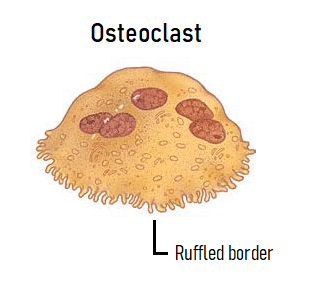
The final cell we need to know is an osteoclast. Remember that an osteoblast helps to make bone tissue. An osteoclast, on the other hand, breaks down bone tissue. A key feature of this cell is its ruffled border, which is highlighted in the picture
Classifications of bones
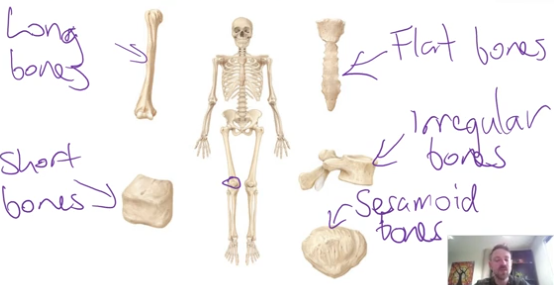
Long bones - longer than they are wide
Short bones - roughly as wide as they are long, and are somewhat cuboidal in shape
Flat bones - these bones are largely flat
Sesamoid - not a shape category, bones that grow inside tendons
Periosteum
Most bones except for long bones are made of an outer shell of compact bone and are filled on the inside with spongy bone
Outside the compact bone shell of all bones lies a connective tissue layer called the periosteum. This covers the entire bone except where there is a cartilage aspect of the bone
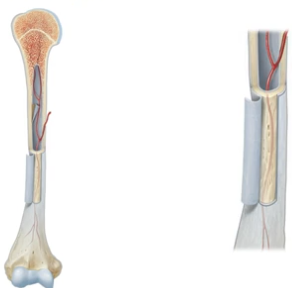
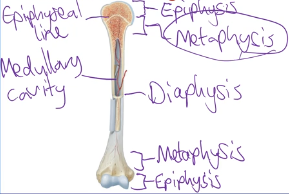
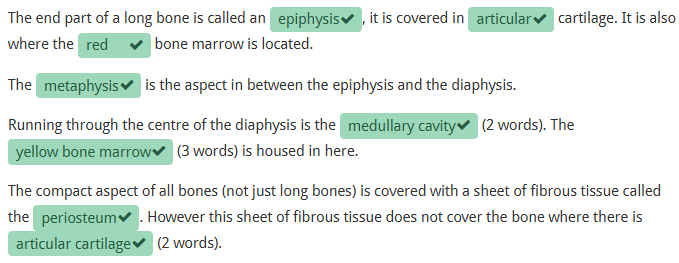
Features of a long bone
Long bones have compact bone on the outside and some spongy bone on the inside
Features of a long bone:
Epiphysis (plural = epiphyses)
Diaphysis
Metaphysis (plural = metaphyses)
Medullary cavity
Epiphyseal lines/plates
Long bone REVIEW
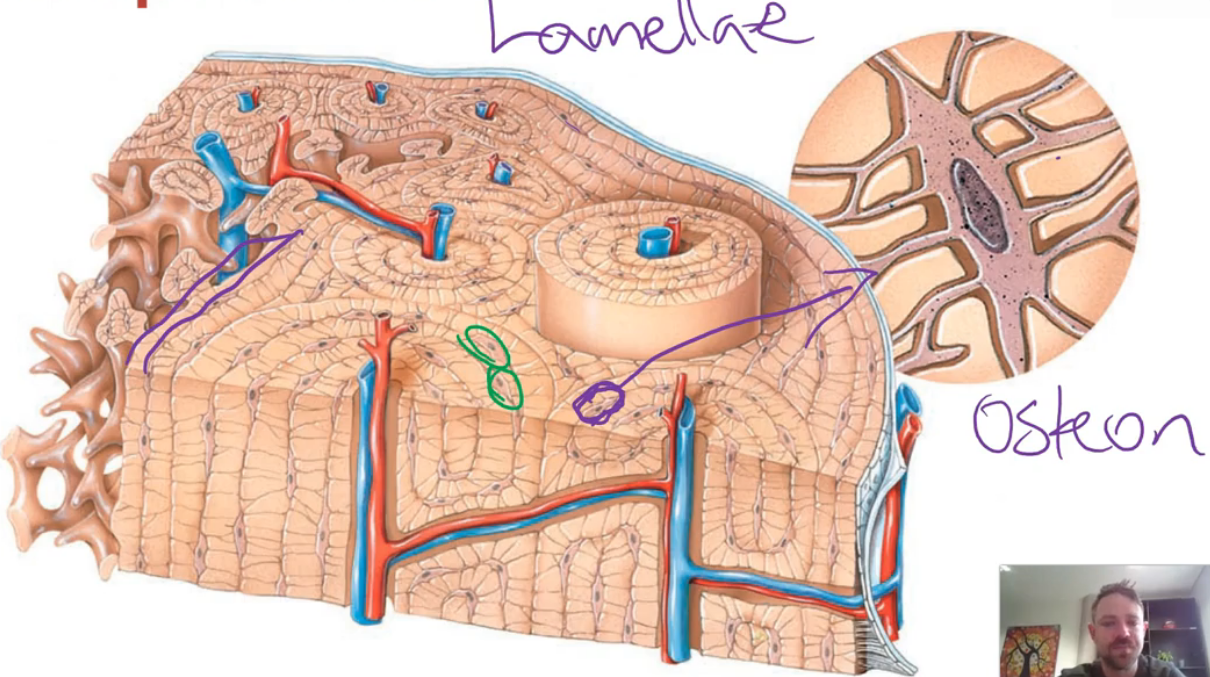
Compact bone
Also called cortical bone tissue, it is more dense than spongy bone. It has fewer spaces and is the stronger tissue of the two
It is found on the outer aspect of a bone, beneath the periosteum or articular cartilage. It consists of repeating units called osteons, which are concentric lamellae (rings of tissue) that surround a central canal, which contains vessels and nerves
At various points in between the lamellae are osteocytes. Other types of lamellae fill the spaces between and around osteons
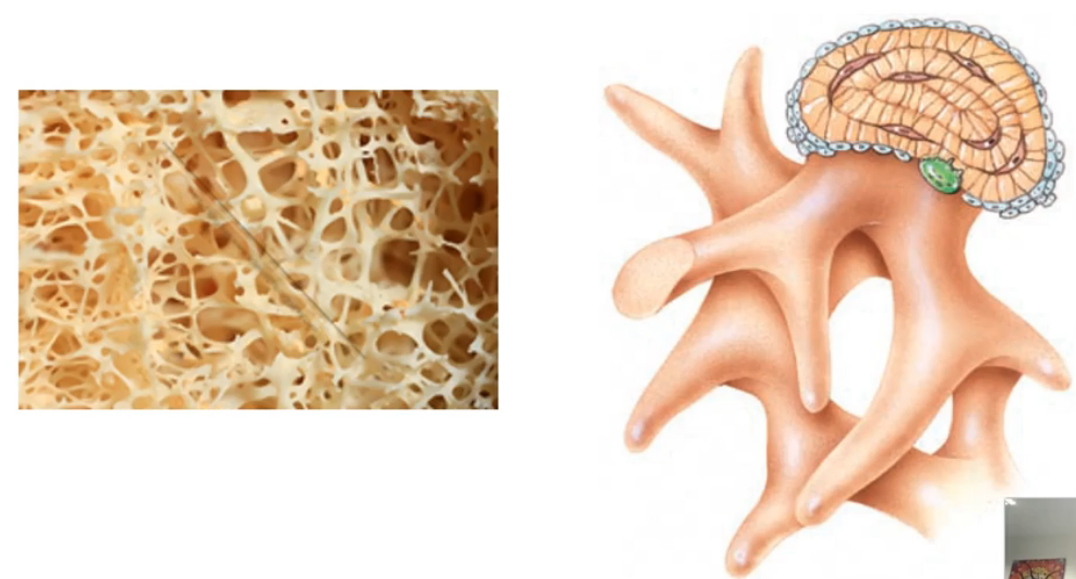
Spongy bone
Also called trabecular or cancellous bone tissue, there are many more spaces between it. This type of osseous tissue is created by a network of spicules (trabeculae) that join together
There are lots of spaces between these thin trabeculae, making this type of bone comparatively weaker. However, this structural make-up is important for a few reasons:
The increased space between the trabeculae makes this bone much lighter than compact bone. This means that the bone moves faster and more easily when a muscle pulls on it
The spaces between the trabeculae house either red or yellow bone marrow. This bone marrow contributes to two of the important functions of bone
Although spongy bone can be considered weaker than compact bone, it can increase the strength of certain parts of the bone in many different directions
Which type of bone creates the outer shell of bones
Compact bone
Which type of bone tissue is found on the inside of bones?
Spongy bone
What are the other names for spongy bone?
Trabecular bone & Cancellous bone
What is often housed between the trabeculae of spongy bone?
Red bone marrow in bones that produce blood cells, yellow bone marrow in other bones
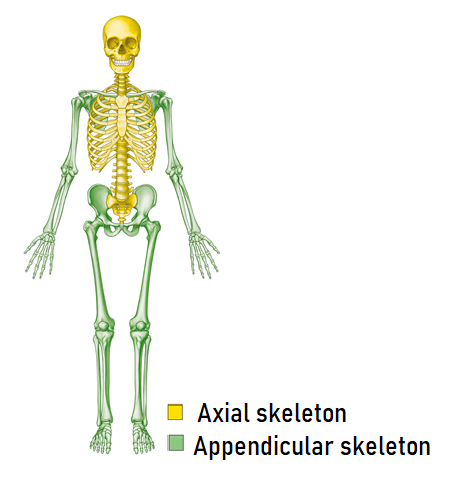
Bones of the skeleton
There are two sections of the skeletal system, called the axial and appendicular skeleton
The axial skeleton consists of the skull, spine, ribs and sternum
The appendicular skeleton consists of the bones of the upper and lower limbs, as well as the bones from the pectoral and pelvic girdles
A girdle is something that encircles something else. The pectoral girdle encircles the upper part of the rib cage, and the pelvic girdle encircles the lower spine
Bony landmarks
All bones have surface markings or particular aspects that allow specific functions. These markings/aspects of the bone are called bony landmarks
Some of these are present at birth, however many develop in response to tendons, ligaments, or other elements pulling or pushing on certain parts of the bone
Generally speaking there are 3 types of bony landmarks:
Projections
Depressions
Openings
There are many different types of projections, depressions and openings, which have specialised terms associated with them
For example, a roughly circular shaped opening is a called a foremen, however a long narrow opening is called a fissure
The names of these specific types of bony landmarks are then given further detail which relates to exactly where in the body they are found
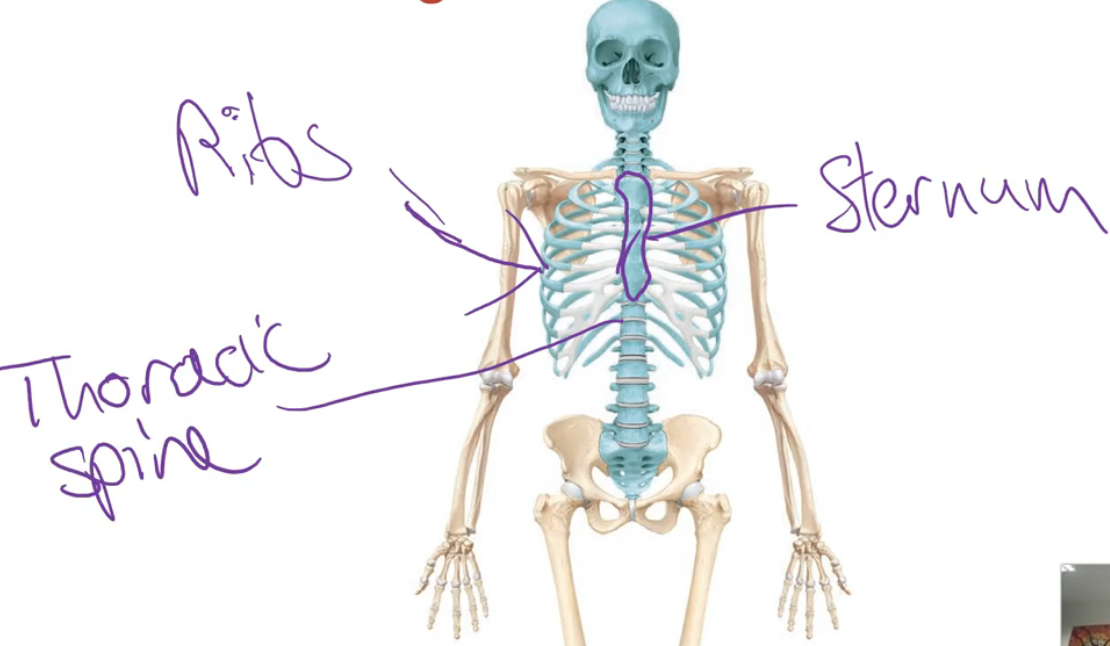
Axial skeleton overview
The axial skeleton includes:
Skull
Spine (vertebral/spinal column)
Thoracic cage
Thoracic cage components
Make up of:
Ribs: 12 pairs = 24 total
Costal cartilage: White connective tissue seen attached to ribs
Thoracic spine: The part of the spine contributing to the rib cage
Sternum: Central chest bone
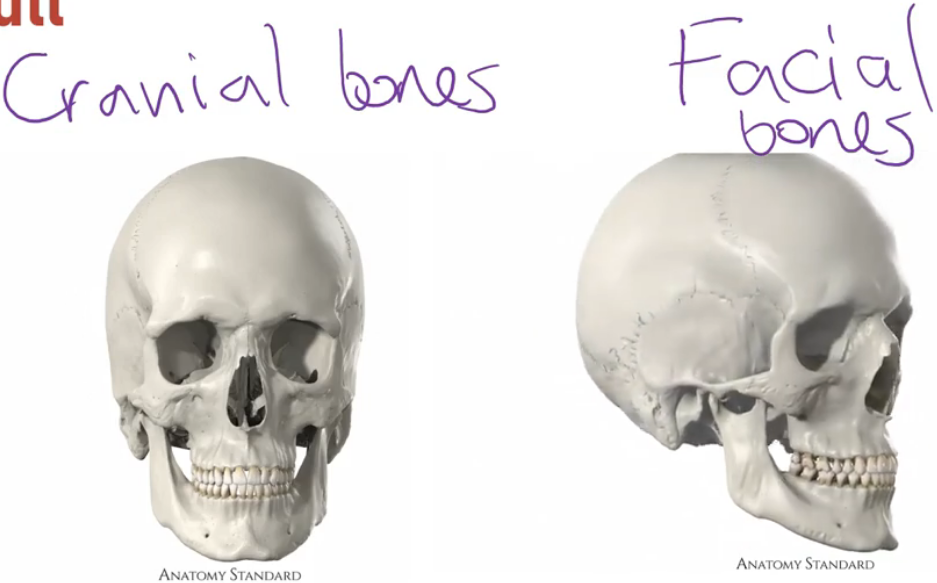
The skull
Divided into:
Cranial bones:
Make up the cavity (walls and roof) where the brain sits
Facial bones:
All other bones that do not contribute to the cranial cavity (mostly face area)
Example:
Mandible: The lower jawbone (a facial bone)
The spine (vertebral column)
Made of individual bones called vertebrae (plural), vertebra (singular)
Viewed from the front or back: appears straight
Viewed from the side (lateral): shows natural curvatures which are important for weight distribution and movement
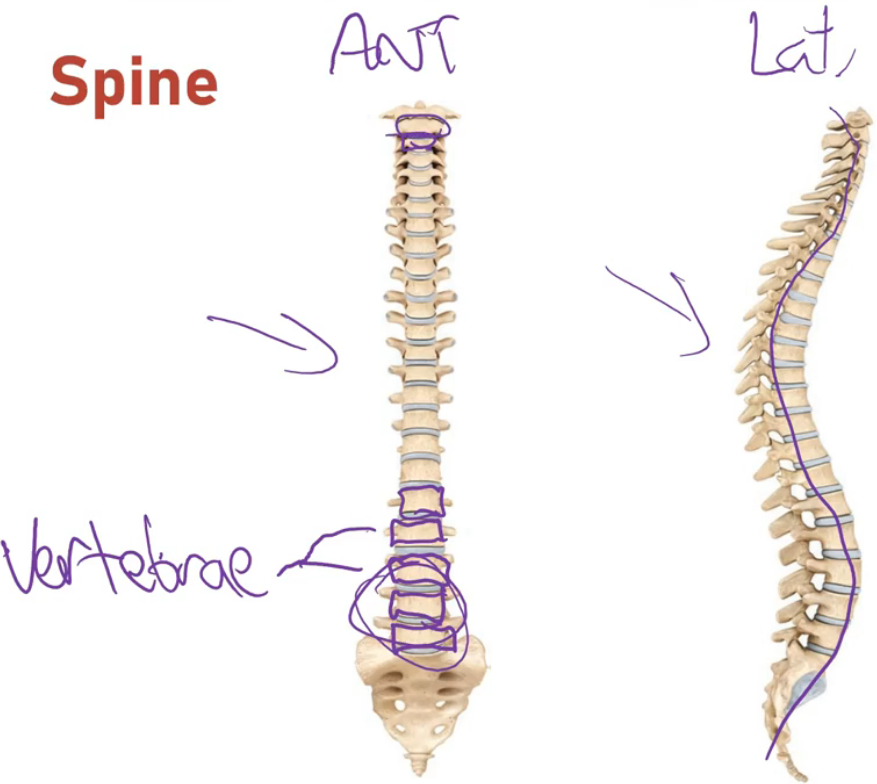
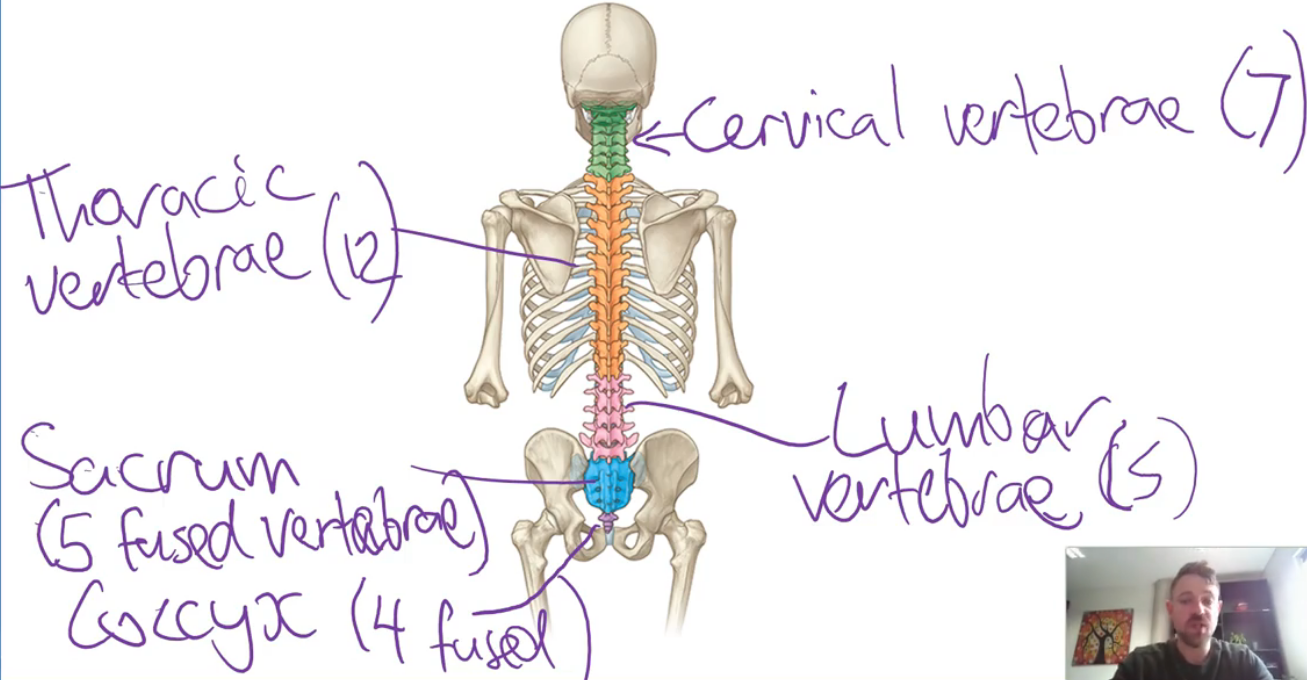
Spinal regions & vertebrae count
Cervical (neck) - 7 vertebrae
Thoracic (chest) - 12 vertebrae
Each has ribs attached
Lumbar (lower back) - 5 vertebrae (common), sometimes 4 or 6
Sacrum - 5 fused vertebrae (in adults it’s one bone; separate in children)
Coccyx (tailbone) - most commonly 4 fused vertebrae
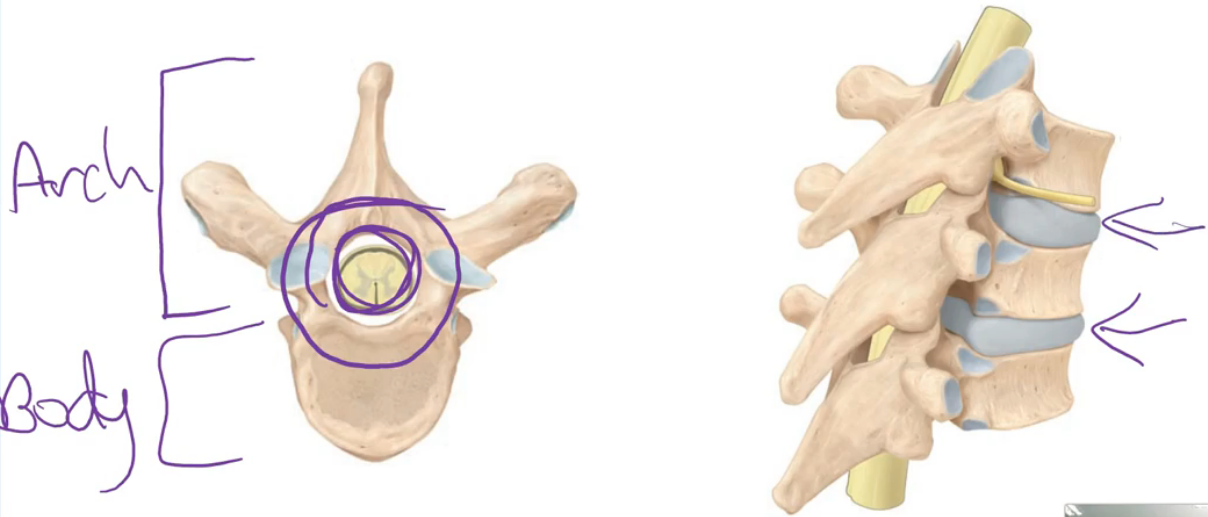
General structure of a vertebra
Two main parts:
Vertebral body (blue in diagram) - weight-bearing portion
Vertebral arch - forms the vertebral foramen (central hole) for the spinal cord
When vertebrae stack:
The vertebral foramina align, forming the vertebral canal where the spinal cord passes
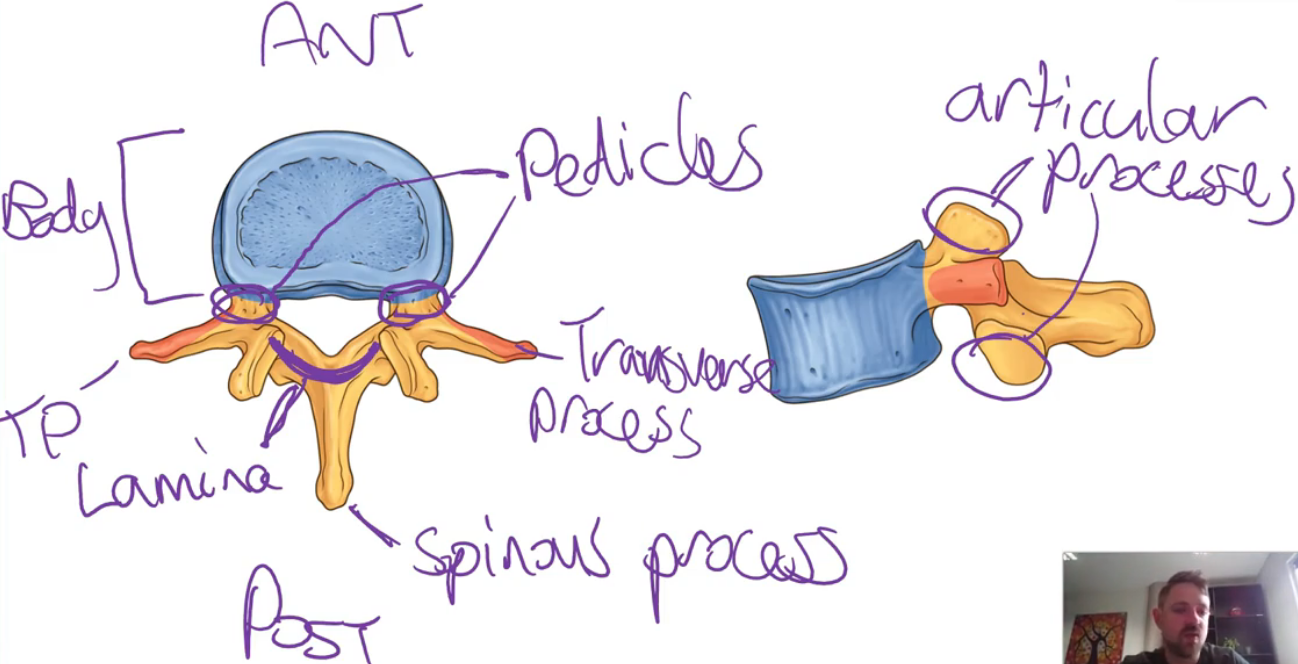
Bony landmarks of a vertebra
Vertebral body
Large, anterior portion
Vertebral arch components:
Spinous process: posterior, projects back (midline)
Transverse processes (x2): Project laterally from the arch base
Pedicles (x2): “Feet” of the arch connecting to the spinous process
Laminae (x2): Upper parts of the arch connecting to the spinous process
Articular processes (x4 total per vertebra):
Superior (2)
Inferior (2)
Allow articulation between vertebrae
Opening:
Vertebral Foramen: Central hole for the spinal cord
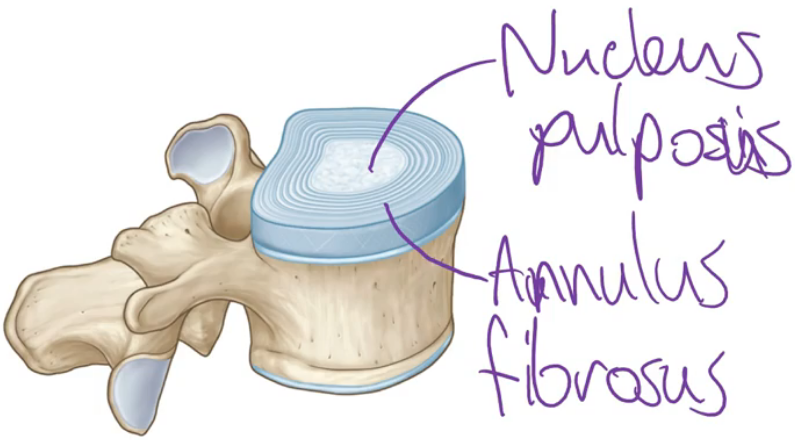
Intervertebral discs
Located between vertebral bodies (except between sacrum & coccyx)
Two parts:
Nucleus Pulposus:
Inner, gelatinous core (pulp-like)
Annulus Fibrosus:
Outer, tough cartilage in rings
Appendicular skeleton overview
The appendicular skeleton consists of four main parts:
Pectoral girdle
Upper limbs
Pelvic gridle
Lower limbs
A girdle is a structure that encircles part of the body
Pectoral girdle
Location: Encircles the upper part of the thorax (rib cage)
Bones involved (2 bones per side):
Clavicle (collarbone): A Long bone running in the transverse plane. Connects:
Medially to the sternum
Laterally to the scapula
Scapula (shoulder blade): Broad, flat bone on the posterior side of the rib cage. Articulates with the humerus
Upper limb bones
Connected to the pectoral girdle
a. Arm
Humerus: The single long bone of the upper arm
b. Forearm
Radius: Lateral bone (thumb side)
Ulna: Medial bone (pinky side)
c. Wrist
Carpal bones: 8 small bones grouped together
d. Hand
Metacarpals: 5 bones forming the structure of the hand
Phalanges: Bones of the fingers
Same name and spelling as the toe bones
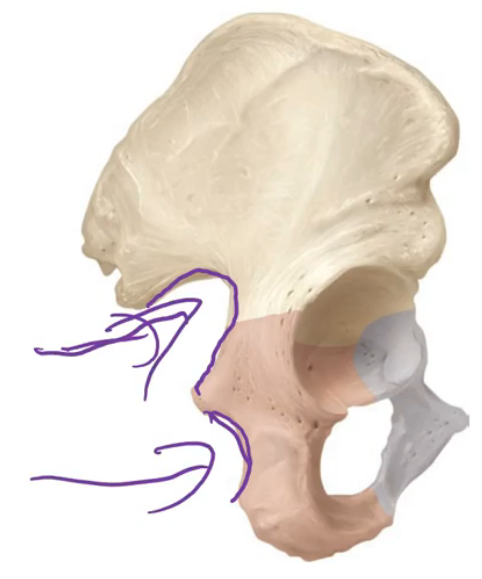
Pelvic girdle
Location: Encircles and supports the lower abdominal organs
Primary bones:
Hip bones (also called pelvic bones):
Each side consists of 3 fused bones (in adults):
Ilium: Superior part
Ischium: Posterior part
Pubis: Inferior anterior part
Connections:
Posteriorly attached to the sacrum
Anteriorly joined to each other at the pubic symphysis
Lower limb bones
a. Thigh
Femur: Single long bone in the upper leg
b. Leg (Below the Knee)
Tibia: Larger, medial bone
Spelling: Tibia, not Tivia
Fibula: Smaller, lateral bone
Common mistake: Fibia is incorrect; the correct spelling is Fibula
c. Kneecap
Patella: Small, triangular bone at the front of the knee
d. Ankle and Foot
Tarsal bones: Equivalent to wrist bones (carpals), 7 in total
Metatarsals: Long bones in the middle of the foot
Phalanges: Toe bones (same name as finger bones)
Tip: "T for Toes" can help remember the difference between carpal (upper limb) and tarsal (lower limb)
Summary of bone name comparisons
Upper Limb | Lower Limb |
|---|---|
Clavicle | Pelvic bone |
Scapula | |
Humerus | Femur |
Radius & Ulna | Tibia & Fibula |
Carpals | Tarsals |
Metacarpals | Metatarsals |
Phalanges | Phalanges |
Patella (knee) |
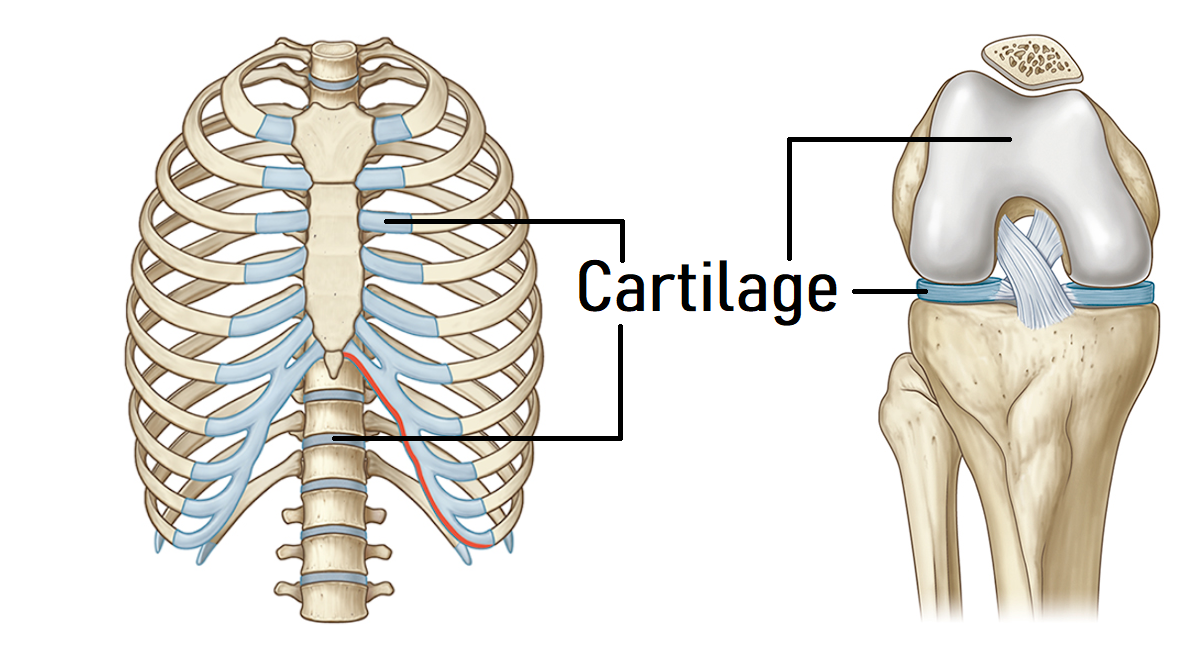
Cartilage
Like bone tissue, cartilage is a type of connective tissue. It is less rigid than bones and is mostly found in areas of the skeleton where more flexibility is required
A good example of this is in the rib cage, which is required to constantly expand and contract as you breathe. Cartilage also forms a major part of many joints
Cartilage can also be found in areas of the body that are not part of the skeletal system. The epiglottis is a good example of this. It is a plate of cartilage in the back of your throat that has roles consistent with both the digestive and respiratory systems
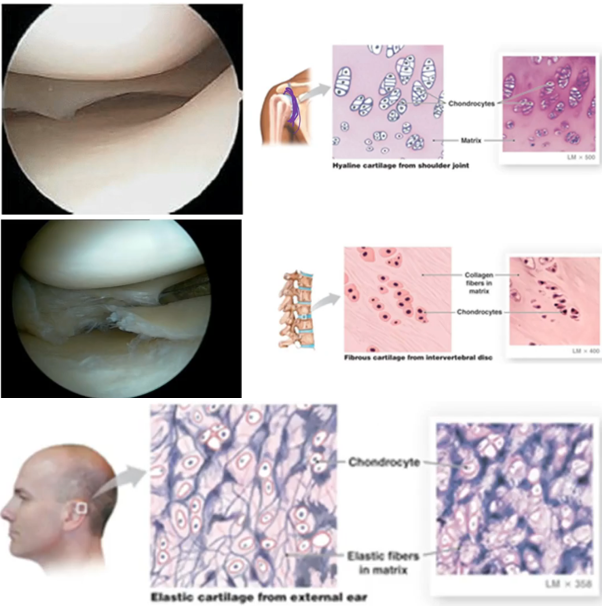
Types of cartilage
3 types of cartilage can be found in the human body:
Hyaline cartilage - shiny, smooth, white type of cartilage that is the most abundant type of cartilage in the body. This type of cartilage is flexible but relatively weak
Fibrocartilage - a very strong and rigid type of cartilage. The many thick collagen fibres present give it these properties
Elastic cartilage - somewhat rigid, yet flexible and elastic. The elastic fibres present give it these properties
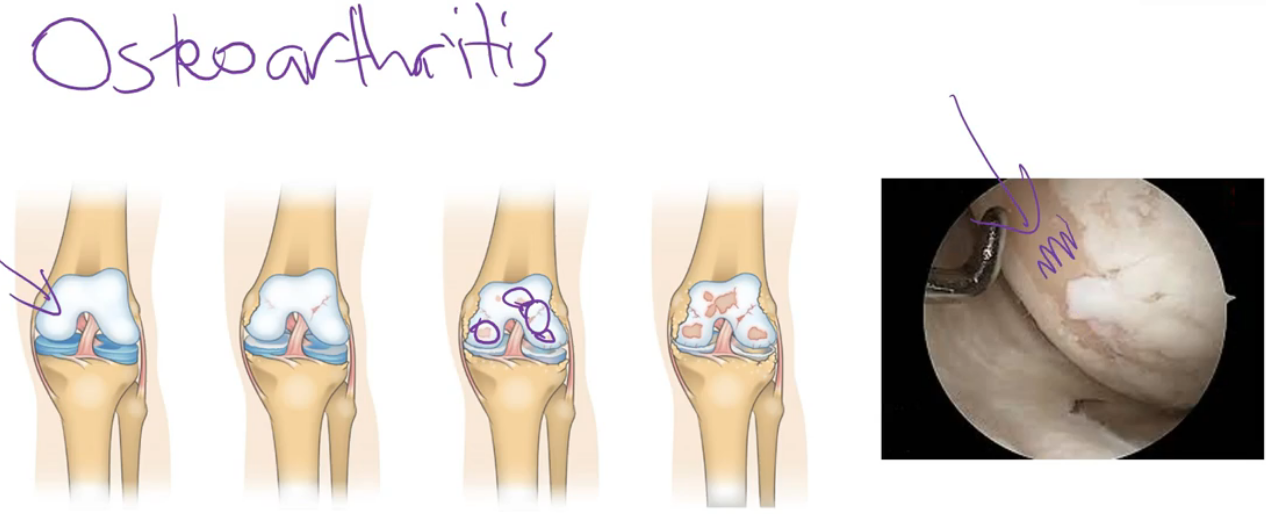
Joints
Movement is permitted through the formation of joints. Joints, also known as articulations or arthroses, are points where two or more bones meet
Although bones are a key component of joints, there are other contributing elements such as cartilage, ligaments and other membranes or tissues
There are a few different types of joints in the body, each with a unique structural make-up that permits a specific function. Some allow a significant degree of movement, whereas others are strong structural unions between bones
joint classifications
The functional classification relates to how much movement is available for the joint
The structural classifications relative to whether or not a joint cavity (space) is present, and the type of tissue that binds the joints if there is no cavity
The three structural classifications of joints are:
Fibrous joints
Cartilaginous joints
Synovial joints
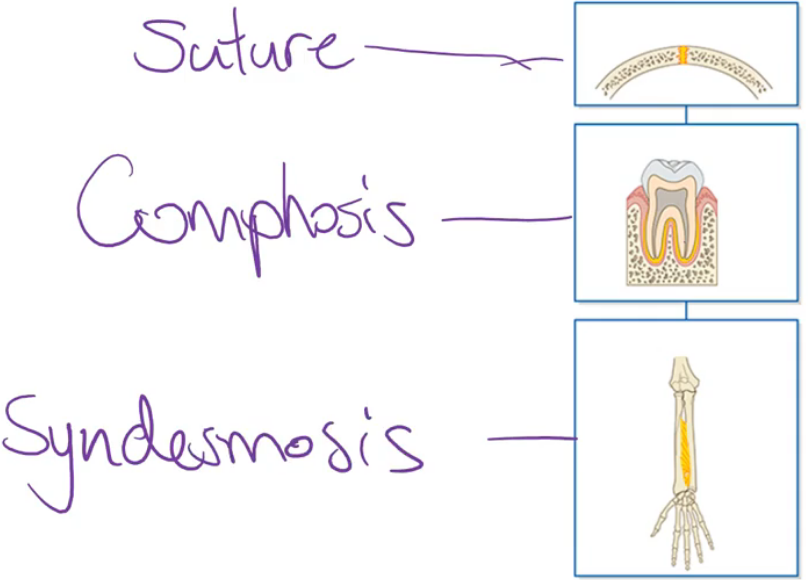
fibrous joints
Do not have a joint cavity. The bones that participate in a fibrous joint are held together by strong connective tissue elements that are rich in collagen fibres
There are fibrous joint subtypes:
Sutures
Syndesmosis
Gomphosis joints
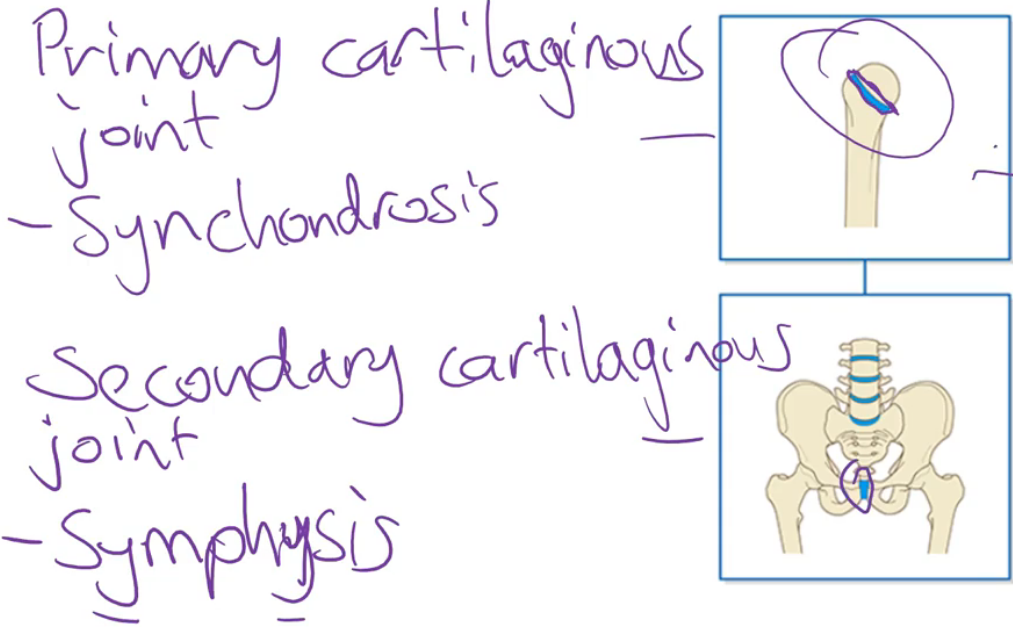
Cartilaginous joints
Lack a joint cavity. Consists of bones (or parts of bones) that are united by a cartilage plate. There are two subtypes of cartilaginous joints:
Primary cartilaginous joints (also called synchondrosis joints)
Secondary cartilaginous joints (also called symphysis joints)
Synovial joints
DO have a joint cavity and are the most movable type of joint. They contain several common features that allow for this free movement
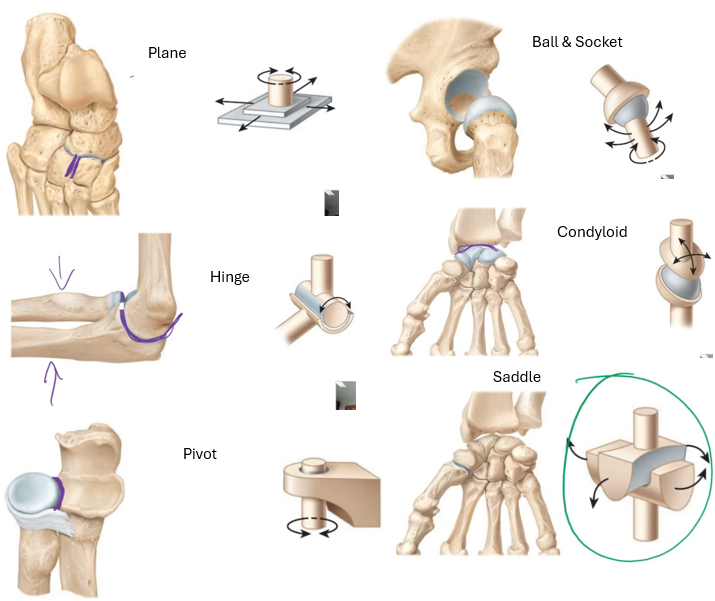
There are 6 subtypes of synovial joints:
Plane (also called gliding) joint
Hinge joint
Pivot joint
Ball and socket joint
Condyloid joint
Saddle joint
fibrous joints REVIEW
cartilaginous joints REVIEW
synovial joint features
Composed of two (or sometimes more) bones that are covered in articular cartilage where they contact each other, a joint capsule which encloses the joint to create a joint cavity (space), synovial fluid which occupies the joint cavity and supporting ligaments
Many synovial joints also have additional structures that aid in their stability and function
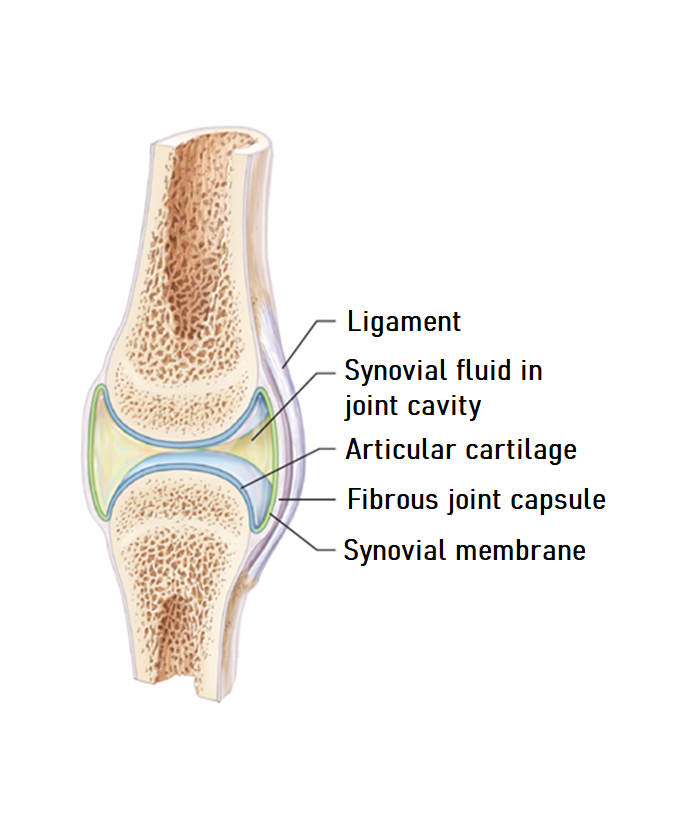
articular cartilage
Made from hyaline cartilage. This smooth, glass cartilage reduces friction between the contact surfaces. It also acts as a shock absorber in some of the major weight-bearing joints of body
joint capsule
Contains two layers: an inner synovial membrane and an outer fibrous capsule. The inner synovial membrane synthesises and secretes synovial fluid into the joint cavity
The outer fibrous aspect is flexible yet strong, which allows movement in the joint while also giving it stability to prevent dislocation
Collectively, the joint capsule also makes the joint cavity fluid-tight

joint cavity
The space between the two bones (and associated articular cartilage) that is inside the joint capsule. It is filled with synovial fluid
synovial fluid
A thin, slippery fluid that is similar in appearance and consistency to uncooked egg white
It occupies the joint cavity and acts as a lubricant between the joint surfaces (surfaces of the articular cartilage)
The primary purpose of the synovial fluid is to reduce friction between the articulating surfaces; however, it also nourishes the articular cartilage
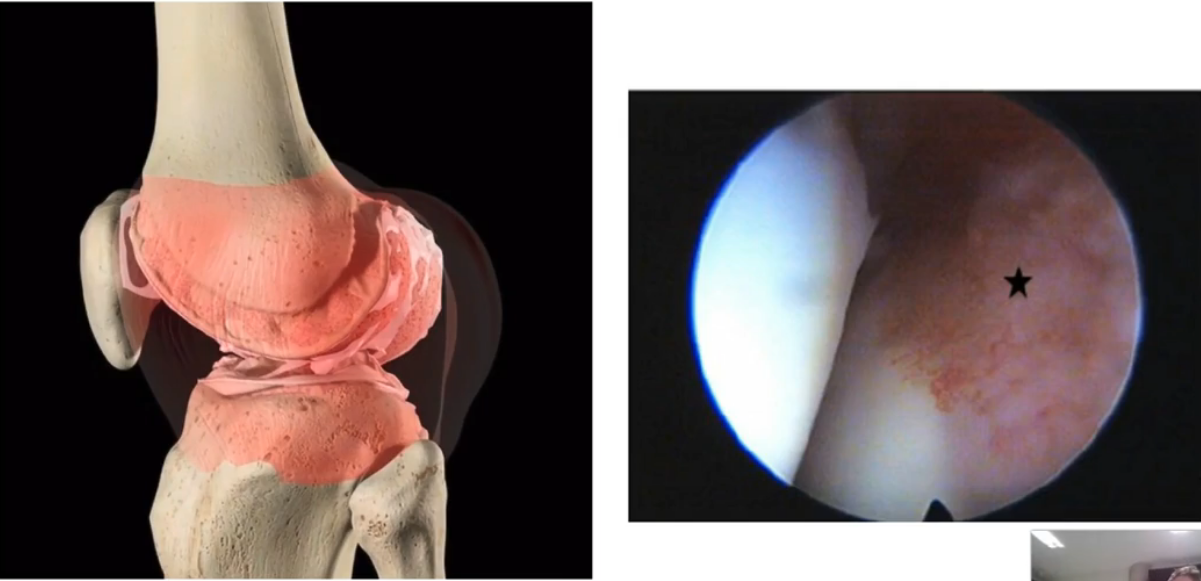
supporting ligaments
The primary role of these connective tissue structures is to support the stability of the joint and reduce the likelihood of dislocation
Ligaments can be a thickened part of the fibrous joint capsule (capsular ligaments), or they can be their entity, either located inside the joint cavity (intracapsular) or completely outside the joint (extracapsular)
additional synovial joint features
Some also contain labrum, meniscus or bursa
Ligaments can be:
Intracapsular - meaning they are inside the fibrous joint capsule (however outside the synovial membrane)
Capsular - meaning they are thickened parts of the fibrous joint capsule
Extracapsular - meaning they are completely outside the joint and have no attachment to the fibrous capsule
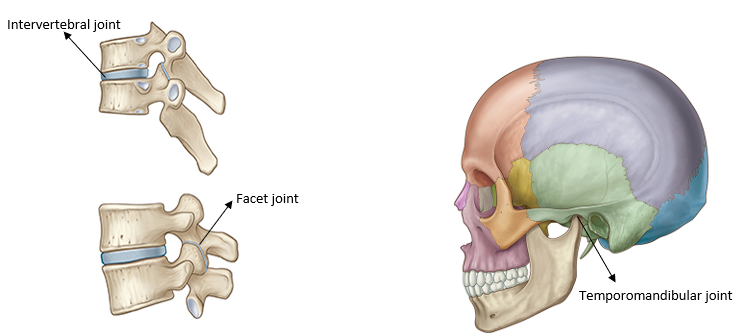
Axial skeleton joints
Intervertebral joints - symphysis joint
Facet joints
Temporomandibular joints
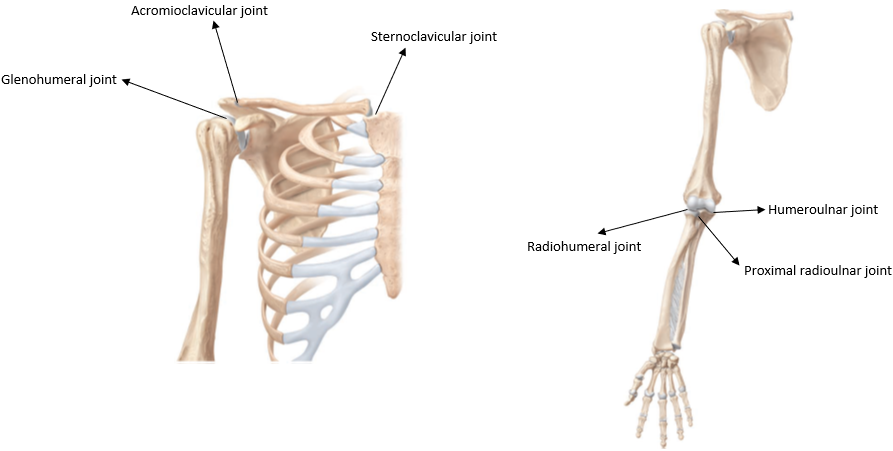
pectoral girdle & upper limb joints
Sternoclavicular joint
Acromioclavicular joint
Glenohumeral joint
Radiohumeral joint
Humeroulnar joint
Proximal radioulnar joint
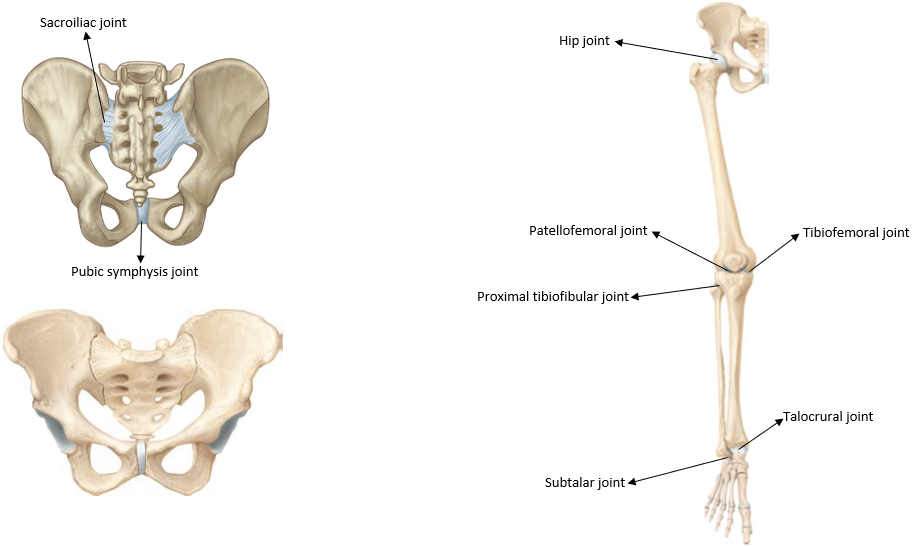
Pelvic girdle & lower limb
Sacroiliac joint - Compound joint: synovial and syndesmosis
Pubic symphysis joint - Symphysis joint
Hip joint (also called the femoroacetabular joint)
Tibiofemoral joint
Patellofemoral joint
Proximal tibiofibular joint
Talocrural joint
Subtalar joint
SHOULDER
Highlight the clavicle bone and on the model's right hand side
Q1 - Which two other bones does the clavicle form a joint with?
Q2 - What are the names of these joints?
Q3 - You have just listed two of the three shoulder joints. What is the name of the third shoulder joint (between the scapula and the humerus)?
Q1 - Scapula & Sternum (manubrium is the specific part of the sternum)
Q2 - Acromioclavicular joint & Sternoclavicular joint
Q3 - Glenohumeral joint
SPINE
Select the L3 vertebra of the spine. A tab will appear on the left.
Tap the 'Parts' icon (next to the highlighted 'Info' icon.
Use the aspects to learn the locations of the following bony landmarks of the vertebrae:
Vertebral body
Transverse processes
Spinous process
Pedicles
Lamina
Superior articular processes
Inferior articular processes
Vertebral foramen
Q4 - Which above bony landmark participates in the intervertebral joint?
Q5 - What type of joint is the intervertebral joint?
Q6 - What are the names of the two different parts of the intervertebral disc?
Tap 'Back' (top left corner of screen)
Rotate the model and zoom to identify the facet joint between the L3 vertebra and the L2 vertebra on the left side.
This is a plane/gliding type of synovial joint. Can you see how the joint surfaces are two flat areas in contact with each other?
Q4 - Vertebral body
Q5 - Symphysis, also known as a secondary cartilaginous joint
Q6 - Annulus fibrosus & Nucleus Pulposus
ELBOW
The three joints around the elbow are the radiohumeral joint (between the humerus and the radius), the humeroulnar joint (between the humerus and the ulna), and the superior radioulnar joint (between the proximal aspects of the radius and ulna).
Q7 - Which of these two joints contributes to the hinge joint of the elbow?
Try and appreciate that the ulna hooks onto the humerus whereas the radius just sits below it
Identify the left superior radioulnar joint (also called the proximal radioulnar joint)
Tap the search button near the top right of screen. Search for 'annular ligament of radius (left)' and tap on this to add it to the model.
Q8 - Which of the three elbow joints is a pivot type of synovial joint?
Can you see how the annular ligament that you added circles around the proximal radius? This essentially forms most of the ring that makes this joint a pivot joint. The radius then spins within this ring as you twist your forearm.
Q7 - Radiohumeral joint (between the humerus and the radius) & Humeroulnar joint (between the humerus and the ulna)
Q8 - Superior radioulnar joint (also called the proximal radioulnar joint)
HIP
Tap on the 'Connective T.' icon at the bottom of the screen and add up to layer 3.
Locate the right hip joint
Q9 - What type of joint is the hip joint?
Tap on the fibrous layer of the joint capsule of the hip to select it. Remove this structure by tapping 'HIDE' (this is near the top of the info box that appears when you select the structure).
Underneath the fibrous layer of the joint capsule is the synovial membrane layer of the joint capsule.
Q10 - What is the role of the synovial membrane?
Q9 - Synovial, ball & socket joint
Q10 - The synovial membrane synthesises and secretes synovial fluid into the joint cavity. This fluid lubricates the joint surfaces to reduce friction when the joint moves.
KNEE
Remove all of the Connective Tissue layers
Locate the left knee joint
Q11 - What are the names of the two joints that are part of the modified hinge joint of the knee?
Identify these two joints
Q12 - What is the name of the other joint at the knee region?
Q11 - Tibiofemoral joint, Patellofemoral joint
Q12 - Superior tibiofibular joint (also known as the proximal tibiofibular joint)
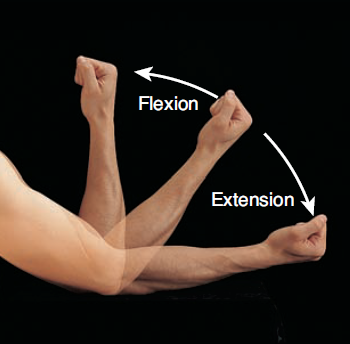
Flexion & Extension
Flexion = movement that results in decreasing the angle between 2 body parts
Extension = movement that results in increasing the angle between 2 body parts
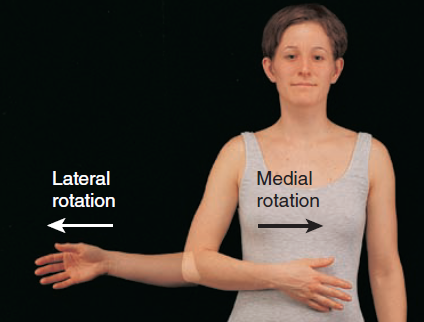
Medial/Internal rotation & lateral/external rotation
Medial rotation = anterior aspect rotating towards the midline
Lateral rotation = anterior aspect rotating away from the midline
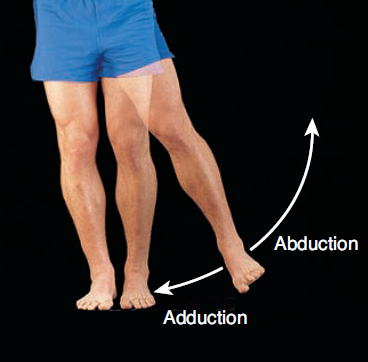
Abduction & Adduction
Abduction = distal aspect moving away from the midline
Adduction = distal aspect moving towards the midline
Dorsi & plantar flexion
Movement Term | Area term applies | Image | Description of movement |
Dorsi flexion | Ankle |
| Dorsum of the foot moving superiorly |
Plantar flexion | Ankle | Plantar aspect of the foot moving inferiorly |
Inversion
Movement Term | Area term applies | Image | Description of movement |
Inversion | Foot |
| The sole is moved towards the midline (inwards) |
Eversion
Movement Term | Area term applies | Image | Description of movement |
Eversion | Foot | The sole is moved away from the midline (outwards) |
Elevation
Jaw and shoulder | The body part moves vertically superiorly |
Depression
Jaw and shoulder | The body part moves vertically inferiorly |
Protraction
Jaw and shoulder | Body part moves horizontally anteriorly |
Retraction
Jaw and shoulder | Body part moves horizontally posteriorly |
Lateral flexion (also called side bending)
Trunk |
| Movement of the trunk towards one side |
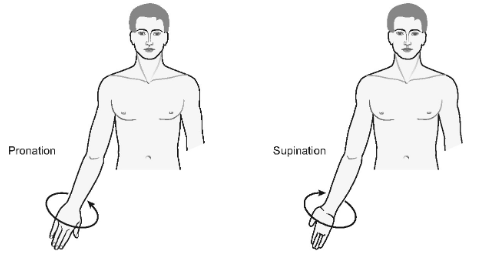
Supination & Pronation
Supination | Forearm/hand |
| The forearm/hand moves to face anteriorly |
Pronation | Forearm/hand | The forearm or hand moves to face posteriorly |
Opposition
Thumb and little finger |
| Specialised movement where the pad of the thumb moves towards the the pad of another finger to meet it (complex and important movement!) |
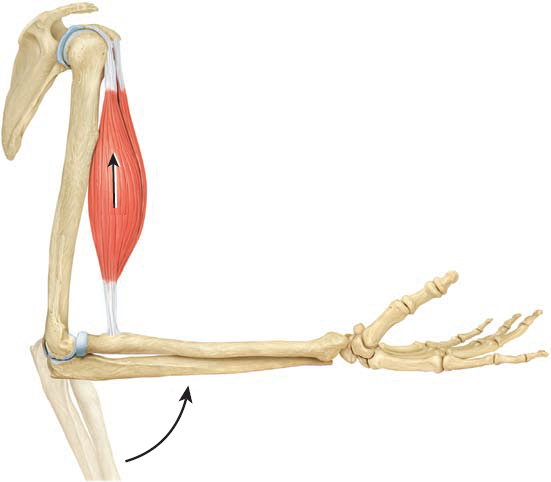
functions of the muscular system - producing body movements
When skeletal muscles activate, they generate a force that pulls on bones, creating the capacity to move joints
The picture shows the biceps brachii muscle contracting to pull on the radius and flex the elbow joint
Functions of the muscular system - stabilising body positions
Skeletal muscle contractions can also stabilise joints. For example, when you are standing up, gravity is constantly trying to collapse you
Many of your skeletal muscles are resisting the force of gravity to stabilise your posture and keep you upright
The picture shows an example where this person’s muscles are activating to stabilise her in a pose

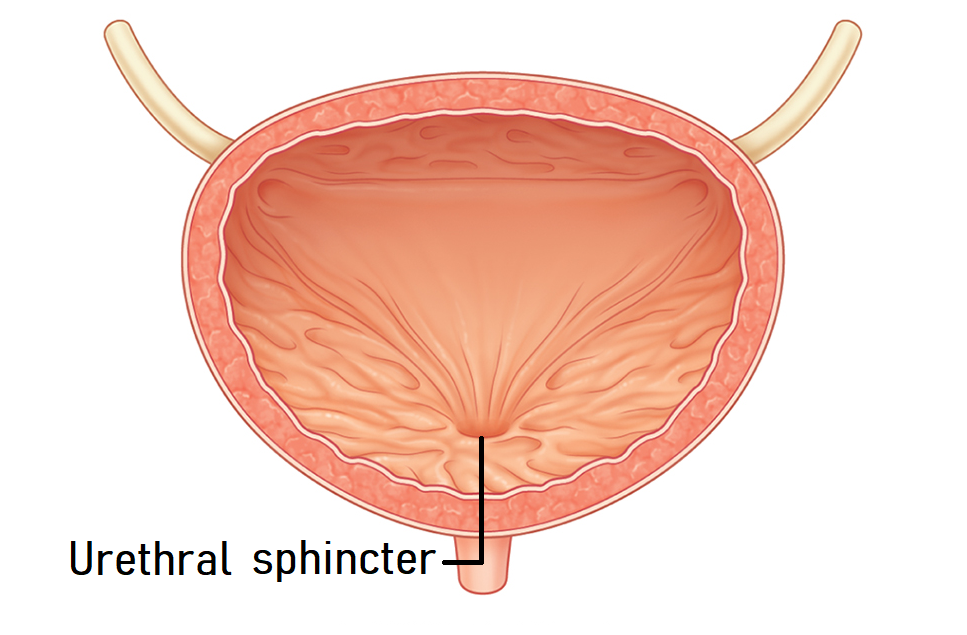
functions of the muscular system - storing substances in the body
Muscles often work to close off the opening of an organ to ensure substances are temporarily stored in this organ until it is time for them to be released
For example, the picture shows the bladder and highlights its sphincter. The urethral sphincter is a ring of muscle that surrounds one of the openings of your bladder
When the muscle is contracted, this opening is closed off, and urine is stored in the bladder
When this muscle relaxes, the urine flows through the opening and is excreted from your body. Usually, it is smooth muscle tissue that is involved in this function
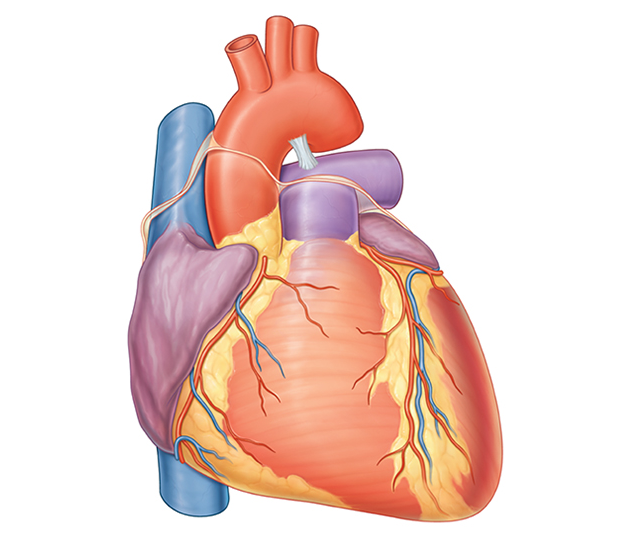
functions of the muscular system - moving substances around the body
The cardiac muscle of the heart, which pumps the blood around the body, is a great example of this
The heart muscle contracts, which forces blood through the body’s vessels
Another example is the smooth muscle in the wall of the intestines, which helps propel food through them
functions of the muscular system - generating heat
Some of the chemical reactions involved in the overall muscle contraction process release heat as a by-product
This is why you get hot when you exercise, or why your body automatically decides to start shivering when you get cold

common muscle tissue properties
Electrically excitable - like neurons, the plasma membrane of muscle cells can establish an action potential that can move across the entire plasma membrane of that cell
Contractility - once excited, muscle cells can generate force by significantly altering their size and shape
Extensibility - muscle tissue can be stretched (to a point) without being damaged, sort of like an elastic band
Elasticity - the muscle tissue springs back to its original length once the force that stretches the muscle tissue is removed. Again, think of an elastic band springing back to its original shape after it has been stretched
muscle tissue comparsion
Muscle Tissue | Appearance | Description | Voluntary/Involuntary |
Skeletal
| Cells and tissues have a striated appearance Multiple nuclei per cell are located near the edge of the cell Cylindrical-shaped cells Can be very long cells - the cells can be 40cm long | Voluntary - the activation and relaxation of skeletal muscle tissue is under conscious control | |
Cardiac | Cells have a striated appearance Branched cells that usually have one central nucleus
| Involuntary - you cannot choose to contract or relax your heart wall | |
Smooth | NO straited appearance, hence the name 'smooth' muscle Single central nucleus Thin, spindle-shaped cells | Involuntary - you cannot choose to contract or relax smooth muscles |
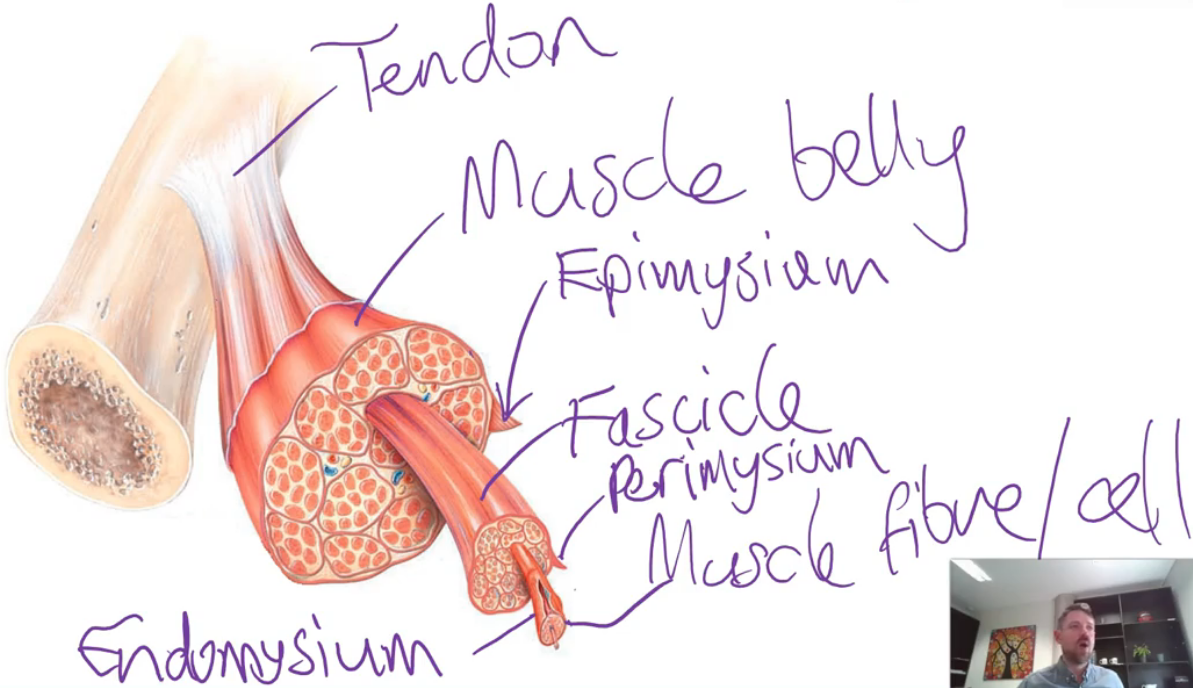
gross anatomy of skeletal muscles
The two main parts of a skeletal muscle are the muscle belly and the tendons. The muscle belly contains the muscle fibres, which are the cells capable of activating
The tendons are connective tissue structures that attach the muscle belly to a bone. Tendons achieve this by blending with the periosteum of a bone
The muscle belly and its fibres are arranged into structures called fascicles. This arrangement is achieved through 3 layers of connective tissue sheaths called the:
Epimysium - surrounds the whole muscle
Perimysium - surrounds a fascicle
Endomysium - surrounds each muscle fibre
These connective tissue sheaths converge to form the tendon at either end of the muscle belly
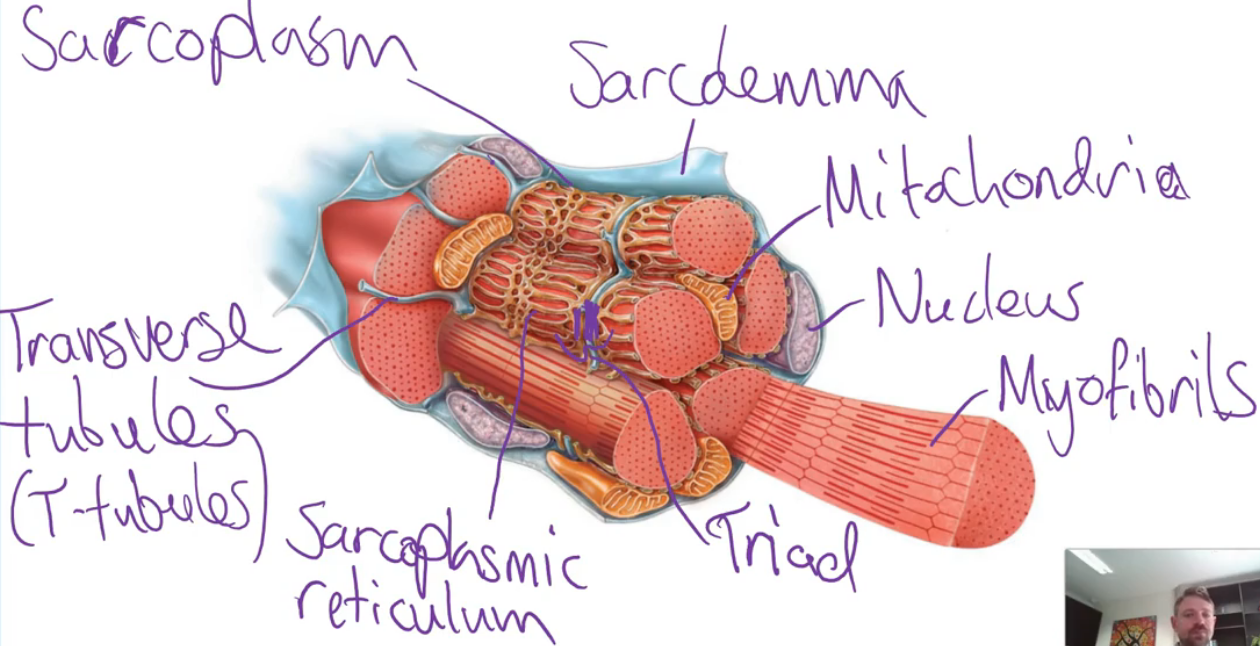
skeletal muscle fibres (cells)
The functional unit of a skeletal muscle. They are long cells (hence the name ‘fibre’) that can generate a pulling force when excited by a motor neuron
Skeletal muscle fibres are multinucleated cells with lots of mitochondria
They have many unique components, with each of these unique components having an important function:
Sarcolemma - the plasma membrane
Transverse tubules - tube-like extensions of the plasma membrane that penetrate through the fibre
Sacroplasm - the cytoplasm of the muscle fibre
Sacroplasmic reticulum - fluid-filled membranous sacs that store calcium ions (Ca2+)
Terminal cisterns - enlarged parts of the sarcoplasmic reticulum that are nested against the transverse tubules
Triad - a transverse tubule with a terminal cistern on either side
Myofibrils - microfilament components that move to generate the pulling force by changing the shape of a muscle fibre
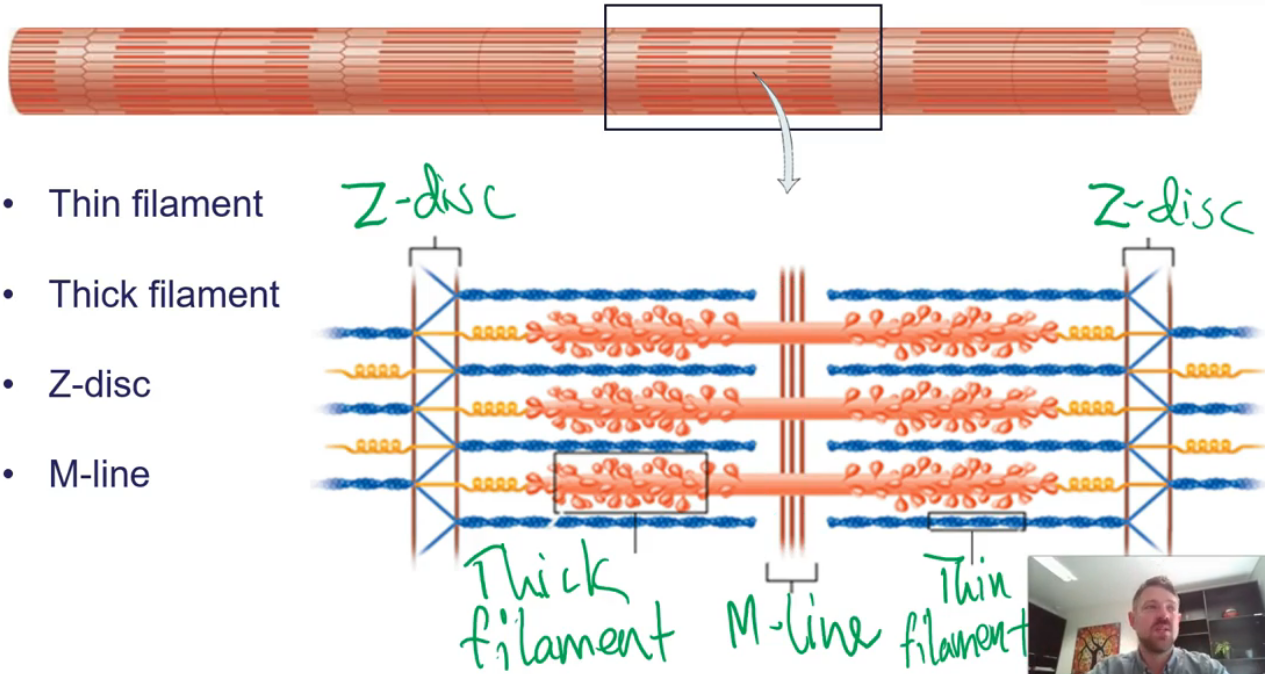
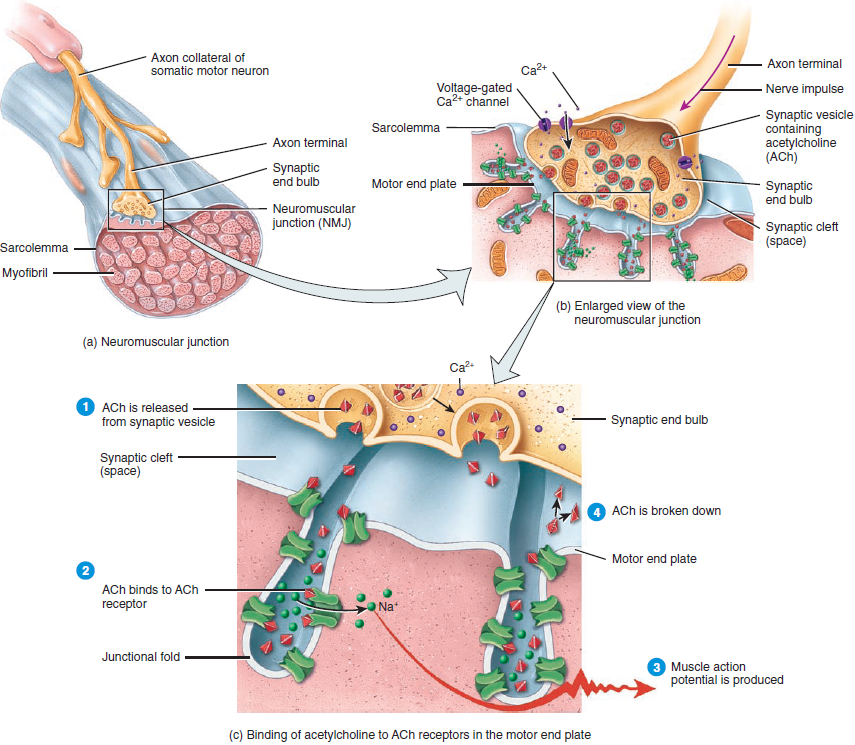
sarcomeres
Each cylindrical myofibril contains lots of small protein filaments, with the two primary filaments being the thick filament and the thin filament
These filaments (and other myofibril elements) are arranged into repeating subunits called sarcomeres
It is the overlapping and non-overlapping parts of these filaments within a sarcomere that create the striated appearance of skeletal muscle tissue
Each sarcomere is separated from its neighbours by narrow plates of dense protein material called Z-discs
There is another protein plate in the centre of the sarcomere called the M-line
The thin filaments are attached to the Z-disc, and the thick filaments are attached to the M-line
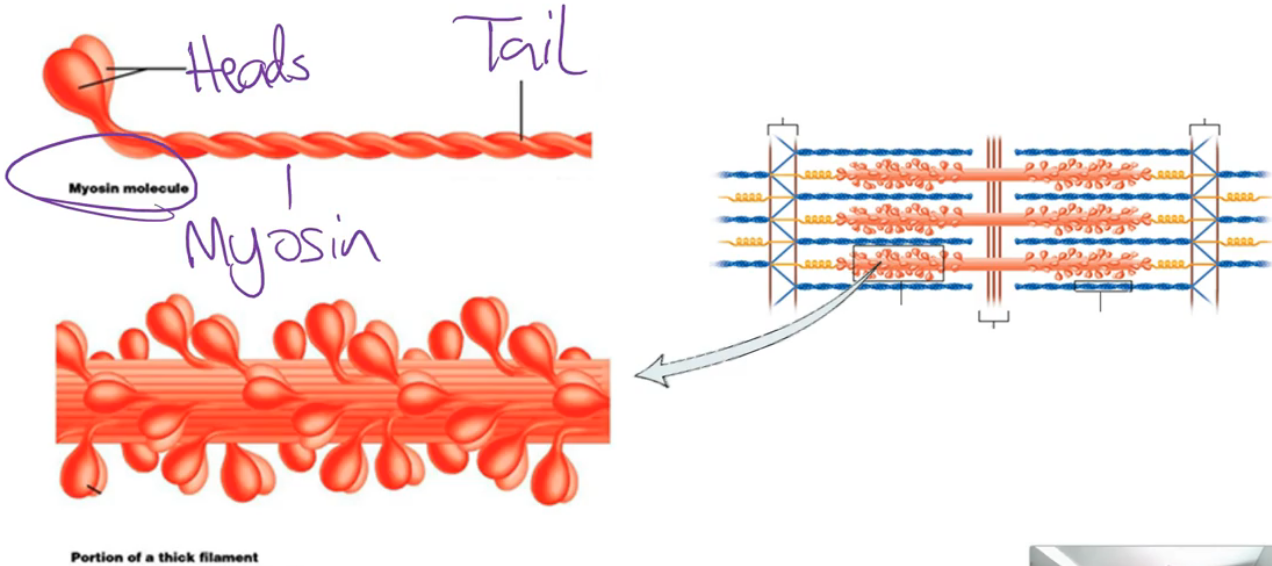
sarcomere - thick filament
Primarily composed of a long contractile proteins called myosin molecules
Myosin is the structure with the ability to convert energy liberated from ATP hydrolysis into mechanical energy - it is the actual structure that generates the force when a muscle activates
Each myosin molecule contains 2 myosin tails which are twisted together. A head then extends outwards from the molecule (towards an adjacent thin filament)
sarcomere - thin filament
Has a contractile protein component, which is called actin
However, the thin filament also contains other parts we need to know about, including the troponin complex and tropomyosin
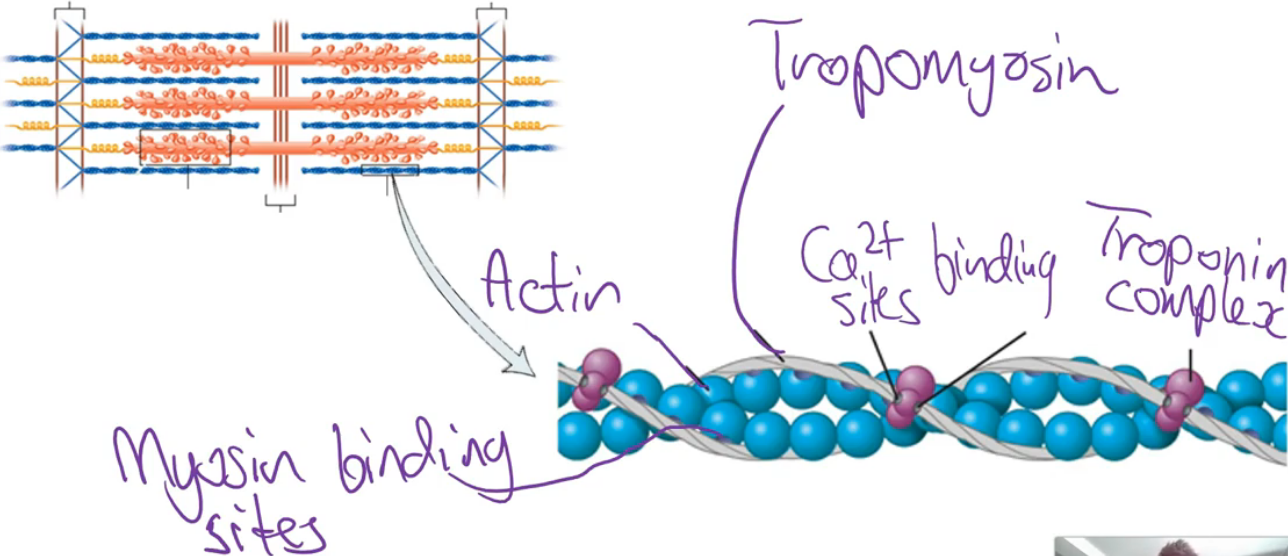
sarcomere - thin & thick filament REVIEW
Skeletal muscle activation
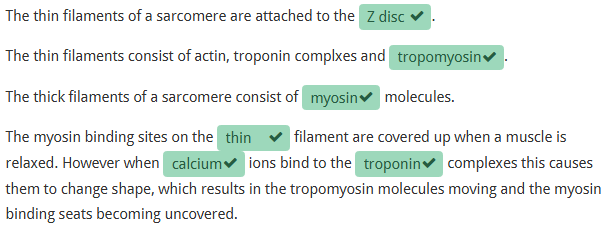
Muscles can activate to move joints or stabilise joints. To achieve these functions, a muscle activates (contracts) in one of three ways:
Isometric activation - the muscle stays the same length as it activates
Isotonic concentric activation - the muscle shortens as it is activated
Isotonic eccentric activation - the muscle lengthens as it is activated
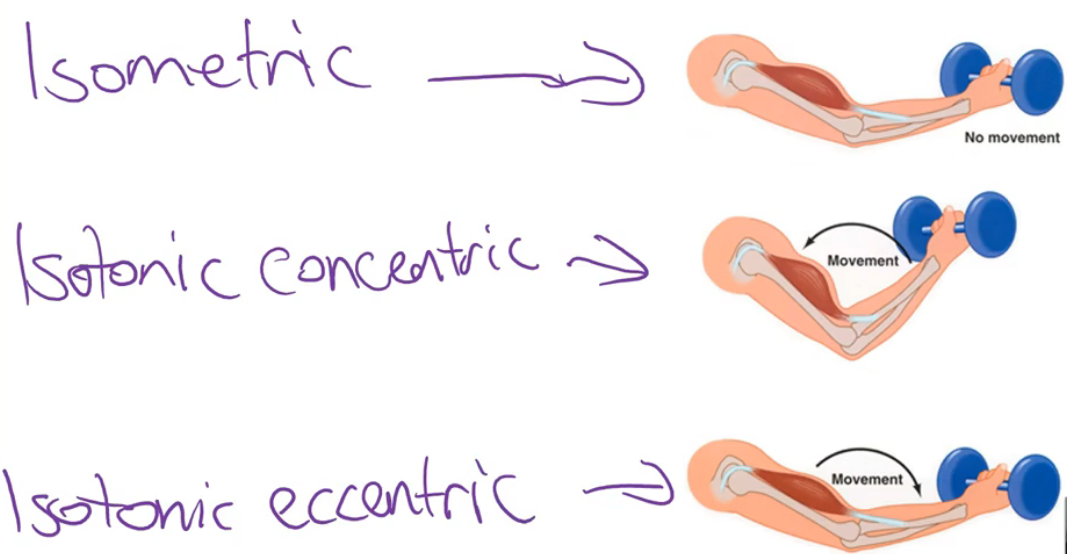
neuromuscular junction
The point where a neuron meets a muscle cell. At this junction, an action potential is essentially transferred from a motor neuron to a muscle fibre, electrically exciting it
Neuromuscular junction components involved include:
Somatic motor neuron
Axon terminals
Action potential
Motor end plate
Synaptic cleft
Voltage-gated calcium channels
Acetylcholine vesicles
Ligand-gated cation channels
process at the neuromuscular junction
Action Potential Arrival: An action potential travels down the motor neuron to the axon terminal
Calcium Channel Activation: Voltage-gated calcium channels open, allowing calcium ions to enter the axon terminal
Acetylcholine Release: Calcium entry triggers synaptic vesicles to release acetylcholine (ACh) via exocytosis
ACh Binding: ACh diffuses across the synaptic cleft and binds to receptors on the muscle fibre’s motor end plate
Channel Opening: ACh receptor binding opens ligand-gated cation channels
Ion Movement: Sodium enters and potassium exits the muscle fibre, leading to membrane depolarisation
Muscle Action Potential: If the threshold is reached, an action potential propagates along the sarcolemma (muscle membrane)
Signal Termination: ACh is removed from the synapse by diffusion and breakdown via acetylcholinesterase; choline is recycled
neuromuscular junction process Qs
1. Which ion enters the muscle fibre in great quantities during this process?
Sodium
2. The action potential in the axon terminal of the motor neuron triggers the _______ gated _______ channels to open.
voltage, calcium
3. True or False - Acetylcholine exits the axon terminal via a process called exocytosis. This is triggered by calcium ions attaching to the acetylcholine vesicles in the axon terminal.
True
4. What is the name of the enzyme that breaks down acetylcholine once it is in the synaptic gap?
Acetylcholinesterase
excitation contraction coupling
We learned that an action potential is eventually simulated on the plasma membrane (sarcolemma) of the skeletal muscle fibre
Now, we will learn how that action potential spreads across the plasma membrane and what impact it ends up having on the cell
This process looks at how the initial excitation of the muscle fibre (which occurred at the neuromuscular junction) ends up causing the contraction of the muscle fibre
Action potentials occur on a plasma membrane and move across this plasma membrane once they are initiated
Transverse tubules are tube-like extensions of the sarcolemma (plasma membrane of the muscle fibre) that penetrate through the fibre
The inside of a transverse tubule is filled with extracellular fluid
Calcium ions are stored in the sarcoplasmic reticulum of a muscle fibre
process of excitation contraction coupling
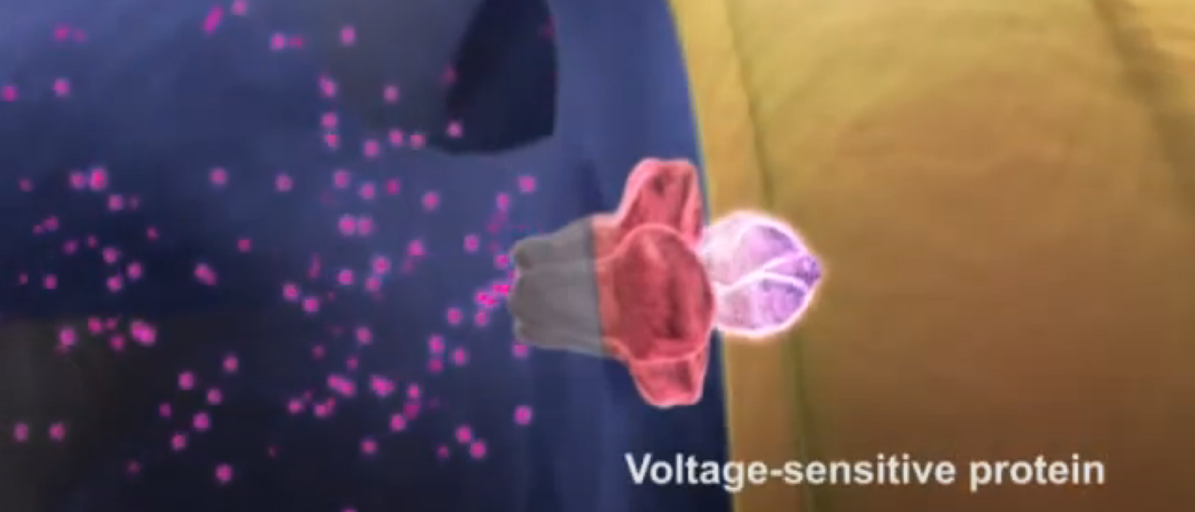
There is only one step in this process, which is that the action potential travelling down a transverse tubule causes a voltage-sensitive protein to change shape, opening a calcium release channel in the sarcoplasmic reticulum, which allows lots of Ca2+ to enter the sarcoplasm
sliding filament mechanism
Up until this point, the activation process for all types of contraction (isometric, concentric and eccentric) is the same. However, once excitation-contraction coupling occurs, the process for each contraction type changes slightly. We are just going to look at the mechanisms that occur in a muscle fibre during an isotonic concentric contraction. This mechanism is called the sliding filament mechanism
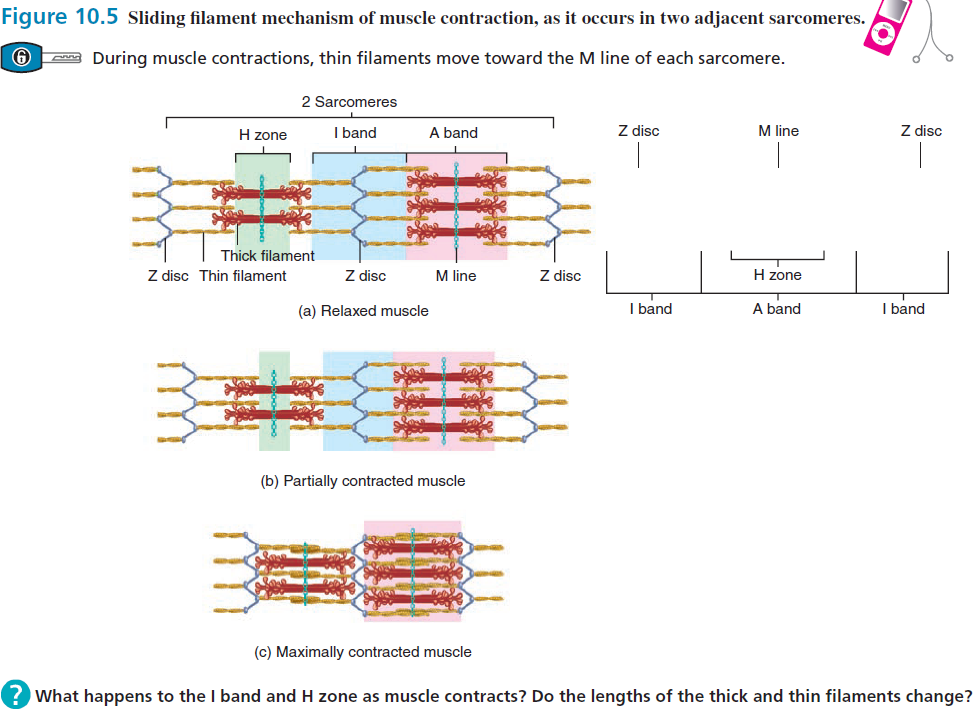
The sliding filament mechanism involves the thin filaments sliding along the thick filaments. This occurs because the myosin heads of the thick filaments 'walk' along the thin filaments, pulling them closer to the centre of the sarcomere. This process causes the Z-discs to be pulled towards the M-line, shortening the overall length of the sarcomere
cross bridge cycle
Each 'step' a myosin head takes as it 'walks' along the thin filament is known as a cross bridge cycle. This is because the myosin head forms a bridge between the two filaments with each of these 'steps'. In order to understand this cycle we need to remind ourselves of ... fundamental pieces of information:
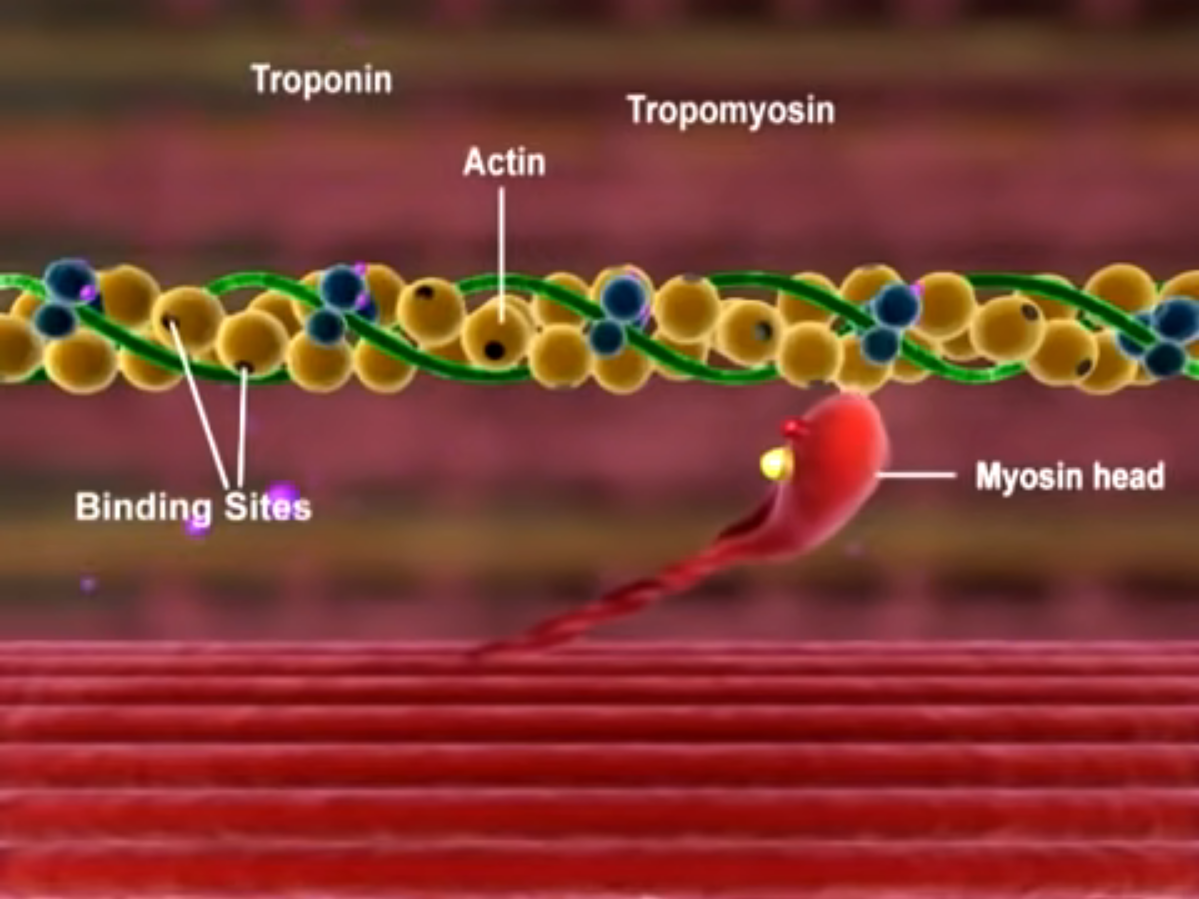
The thin filament contains actin, troponin complexes and tropomyosin
Ca2+ ions that have been released from the sarcoplasmic reticulum during excitation contraction coupling bind to troponin complexes
Actin monomers have a myosin binding site on them which is covered by tropomyosin when the muscle fibre is at rest
ATP hydrolysis is a reaction that releases energy which the body can use
steps occurring in the cross bridge cycle - preparation phase
Preparation Phase (Before the Cycle Begins):
Calcium Release: Calcium ions are released from the sarcoplasmic reticulum
Troponin Activation: Calcium binds to troponin, causing a shape change
Tropomyosin Movement: This shifts tropomyosin, exposing myosin-binding sites on actin
Myosin Head Activation: ATP binds to the myosin head, is hydrolyzed to ADP + Pi, energizing (cocking) the head
steps occurring in the cross bridge cycle - main steps
Cross Bridge Cycle (4 Main Steps):
Cross Bridge Formation
Activated myosin head binds to actin.
Inorganic phosphate (Pi) is released, strengthening the bond
Power Stroke
ADP is released
Myosin head pivots, pulling the actin filament toward the sarcomere centre
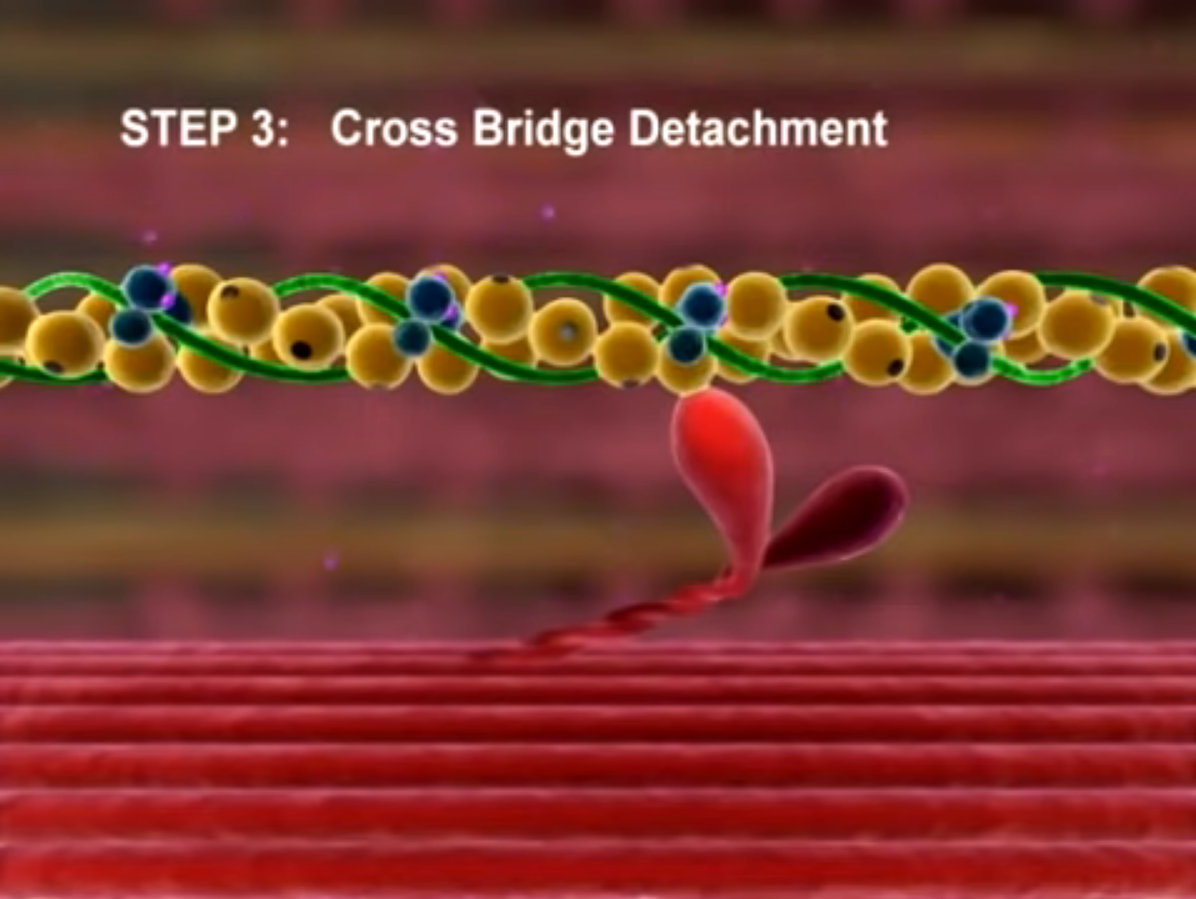
Cross Bridge Detachment
A new ATP binds to the myosin head
This causes the myosin head to detach from actin
Reactivation of Myosin Head
ATP is hydrolysed again to ADP + Pi
Energy from hydrolysis re-cocks the myosin head
steps occurring in the cross bridge cycle - cycle continuation/end
Cycle Continuation or End:
As long as calcium remains and ATP is available, the cycle repeats
Muscle contracts as sarcomeres shorten through repeated cycling
When calcium is actively pumped back into the sarcoplasmic reticulum:
Troponin returns to its original shape
Tropomyosin covers the binding sites on actin
Cross-bridge cycling stops, and the muscle relaxes
Which which part of the cross bridge cycle process actually uses the energy liberated by ATP hydrolysis?
Cocking of the myosin head
It is NOT the power stroke that uses the energy
True or False? Each cross bridge cycle results in the two M-lines being pulled towards the central Z-disc
False - it is the Z-discs that are pulled towards the centre of the sarcomere which is where the M-line is
This occurs because the Z-discs are attached to the actin filaments which are the elements being pulled in each cross bridge cycle
Which part of the myofibril do the calcium ions attach to?
The troponin complexes
What is meant by the term 'cross bridge'?
A cross bridge means a bridge being formed between the thick and thin filaments
That is, these two elements are normally not attached however they become attached momentarily when this cross bridge forms
motor units
Defined as a somatic motor neuron with all the muscle fibres it supplies
A motor unit consists of:
One motor neuron (originating in the spinal cord)
All the muscle fibres (cells) that it innervates
So, a single motor neuron may control several muscle fibres, but each muscle fibre is only innervated by one motor neuron