Class 18- Trace minerals, nutritional anemia
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
40 Terms
Trace mineral content in food varies with..
Trace mineral content in food varies with SOIL and WATER composition and food processing
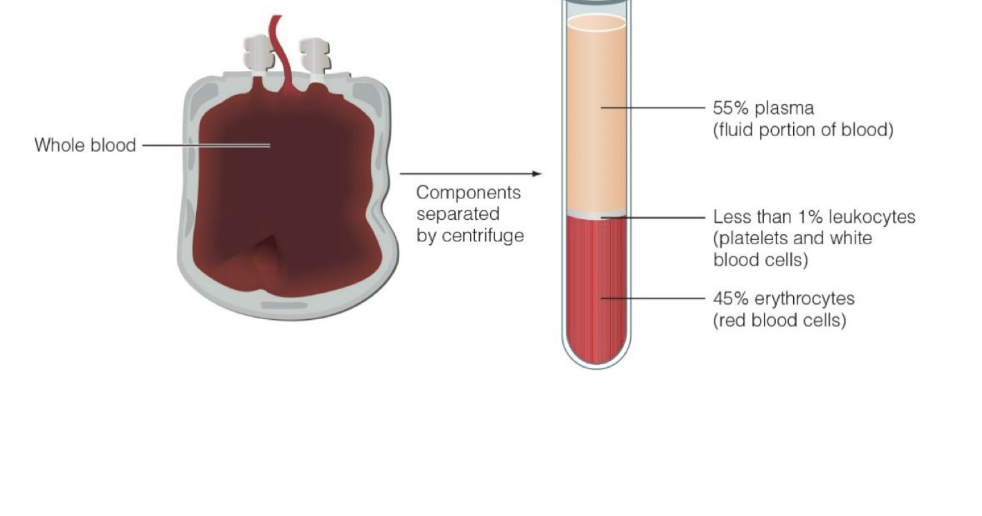
key info about blood
continually moving
delivers pr circulate oxygen and nutrients
removal of waste
only fluid tissue in body
Key nutrients:
iron, vit k, folate, b12
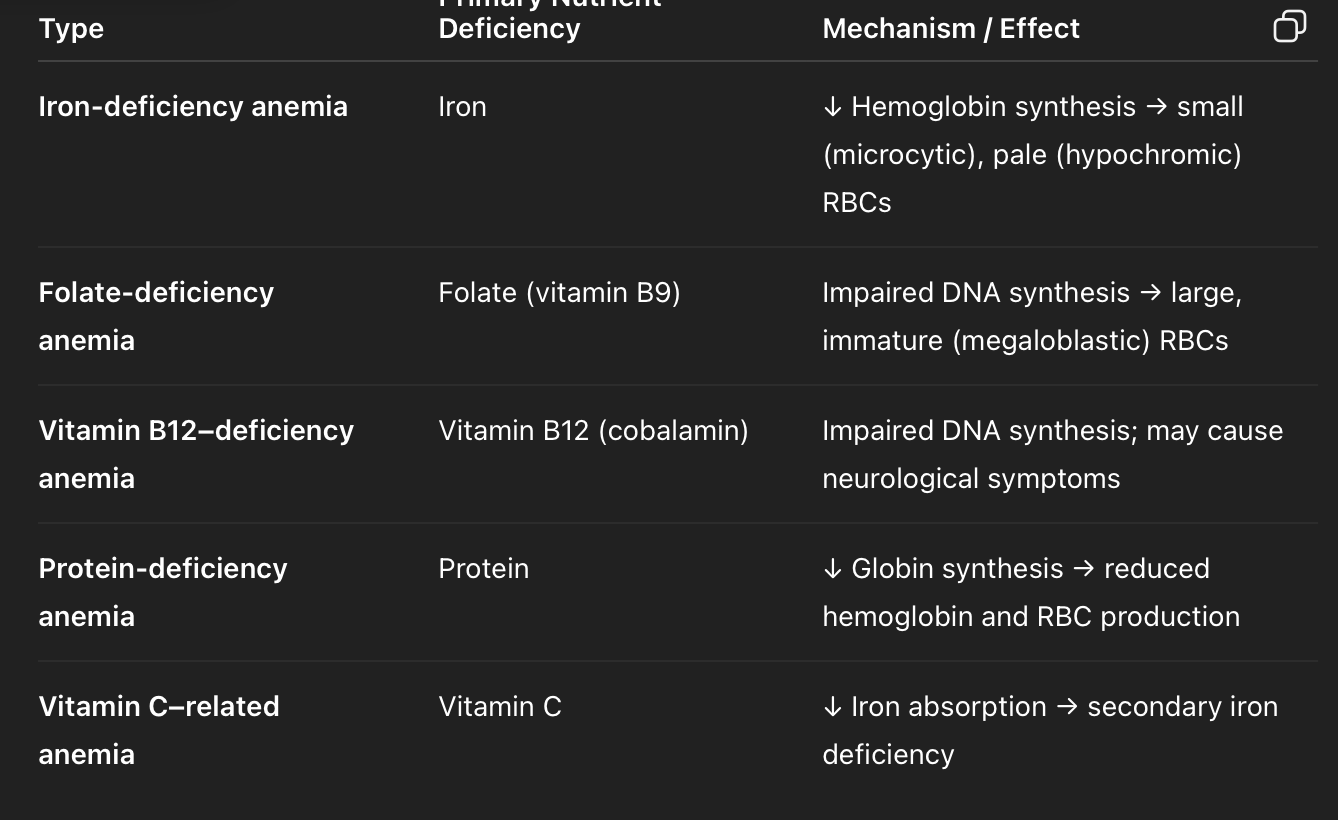
what are Nutritional anemias
Nutritional anemias are a group of anemias caused by inadequate intake, absorption, or utilization of nutrients that are essential for red blood cell (RBC) production and hemoglobin synthesis.
result in decreased oxygen delivery to tissues, leading to fatigue, weakness, pallor, and poor concentration.
Anemia is a condition where the blood has a reduced capacity to carry oxygen to the body’s tissues.
This happens when there is:Too few red blood cells (RBCs),
Too little hemoglobin (the oxygen-carrying protein inside RBCs),
orAbnormal RBCs that can’t function properly.
Particularly concerning in women of reproductive age, pregnant women, infants, and vegetarians/vegans.
3 main types of nutritional anemias
iron deficiency—> hypo chromic or microcytic anemia
Folat or B12 deficiency—> Megaloblastic or
Pernicious Anemia
iron forms, function
FORMS= Ferrous (Fe++), Ferric forms(Fe+++)
FUNCTIONS=
1) Oxidation-reduction reactions
o Part of electron transport chain to make ATP
o Cofactor to many enzymes such as peroxidase, myeloperoxidase, catalase
2) To transfer oxygen: part of Heme group
in a protein
Hemoglobin for transport of oxygen to tissues
Myoglobin for muscle storage of oxygen
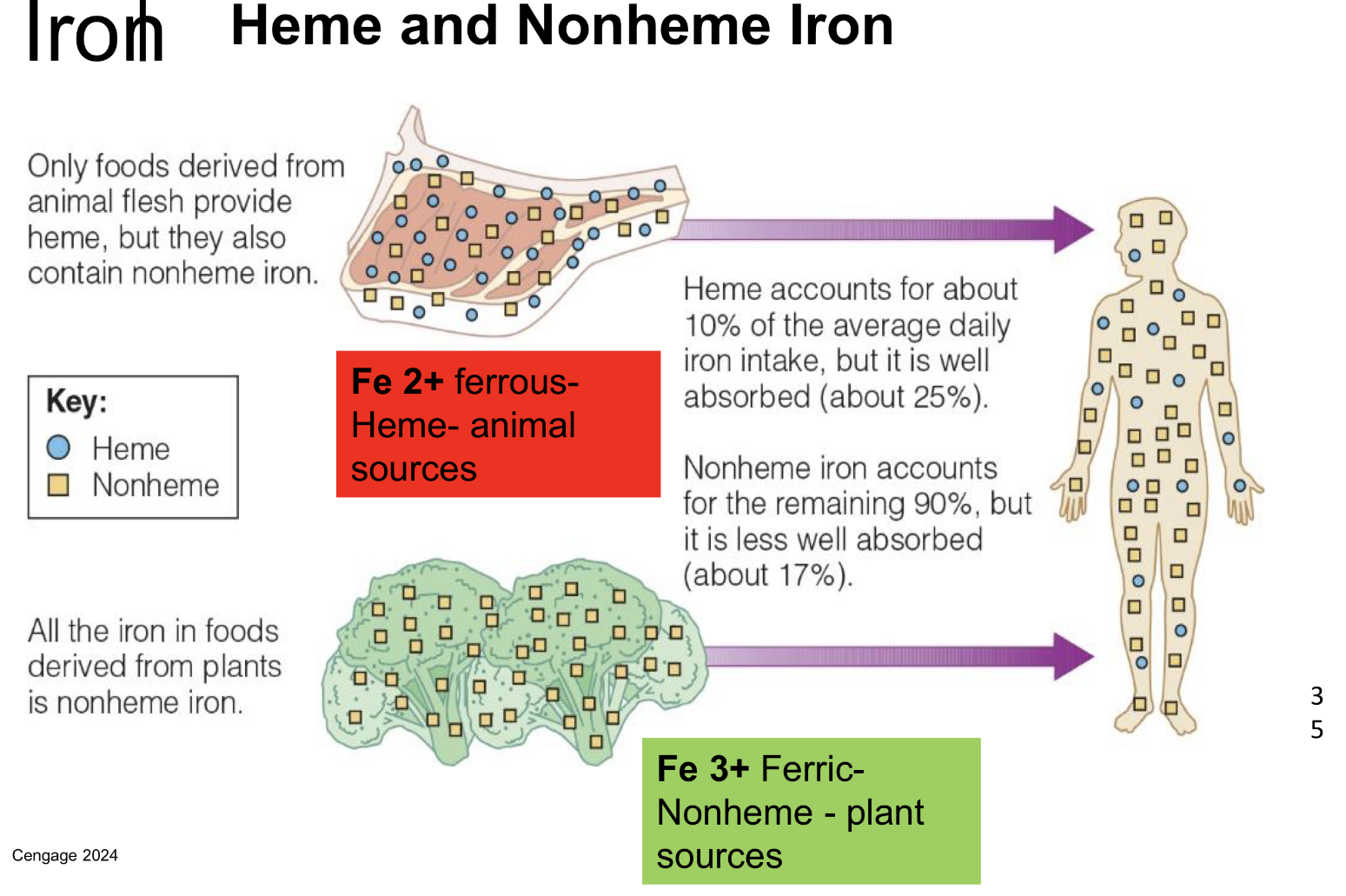
Heme vs nonheme iron
Heme iron → animal-based, more bioavailable.
Non-heme iron → plant-based, less efficiently absorbed, but absorption can be improved by combining with vitamin C–rich foods (like citrus, bell peppers, tomatoes).
what are some iron enhancers vs inhibitors
Enhancers
• Meat factor protein (MFP)
• Vitamin C
• From iron cookware; ↑ acidity of food and cook time = ↑ iron
Inhibitors
• Phytates
• Vegetable proteins
• Calcium
• Polyphenols (e.g., tannic acid)
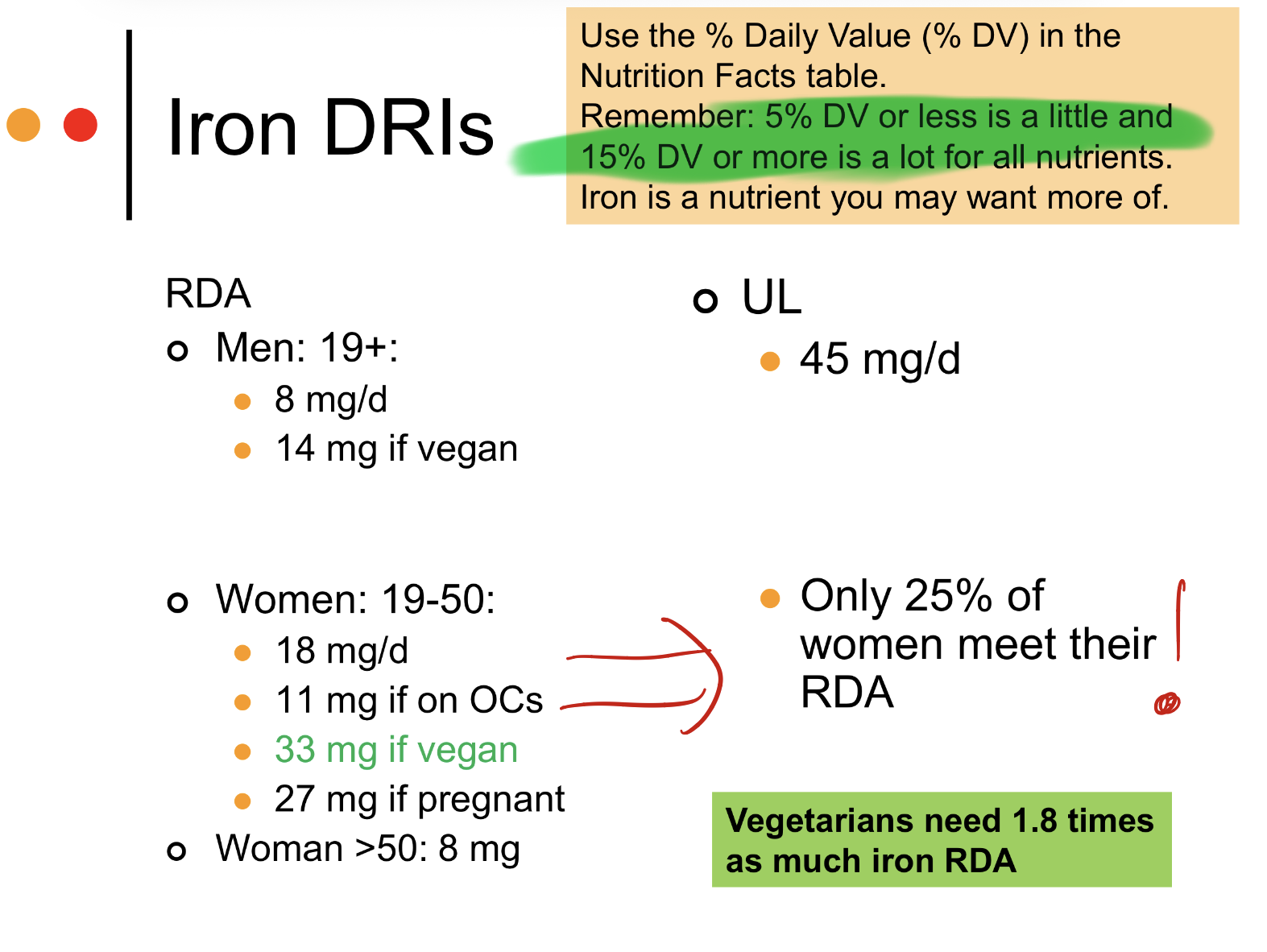
heme vs nonheme iron sources, what are vegetarian needs for iron
Mixed diets: 18% dietary iron
Vegetarian: 10%, so need 1.8 X RDA

what ia iron absorption process
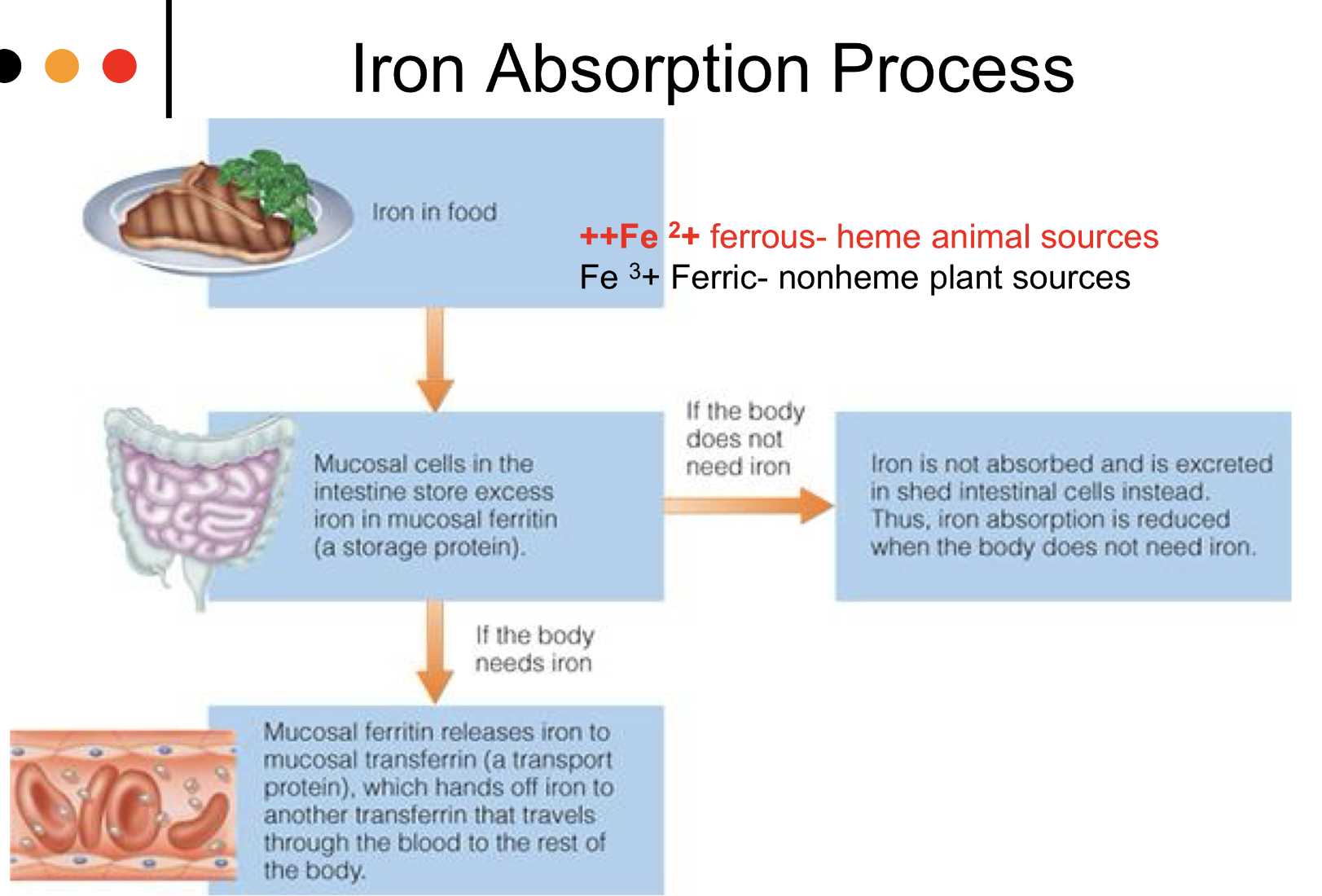
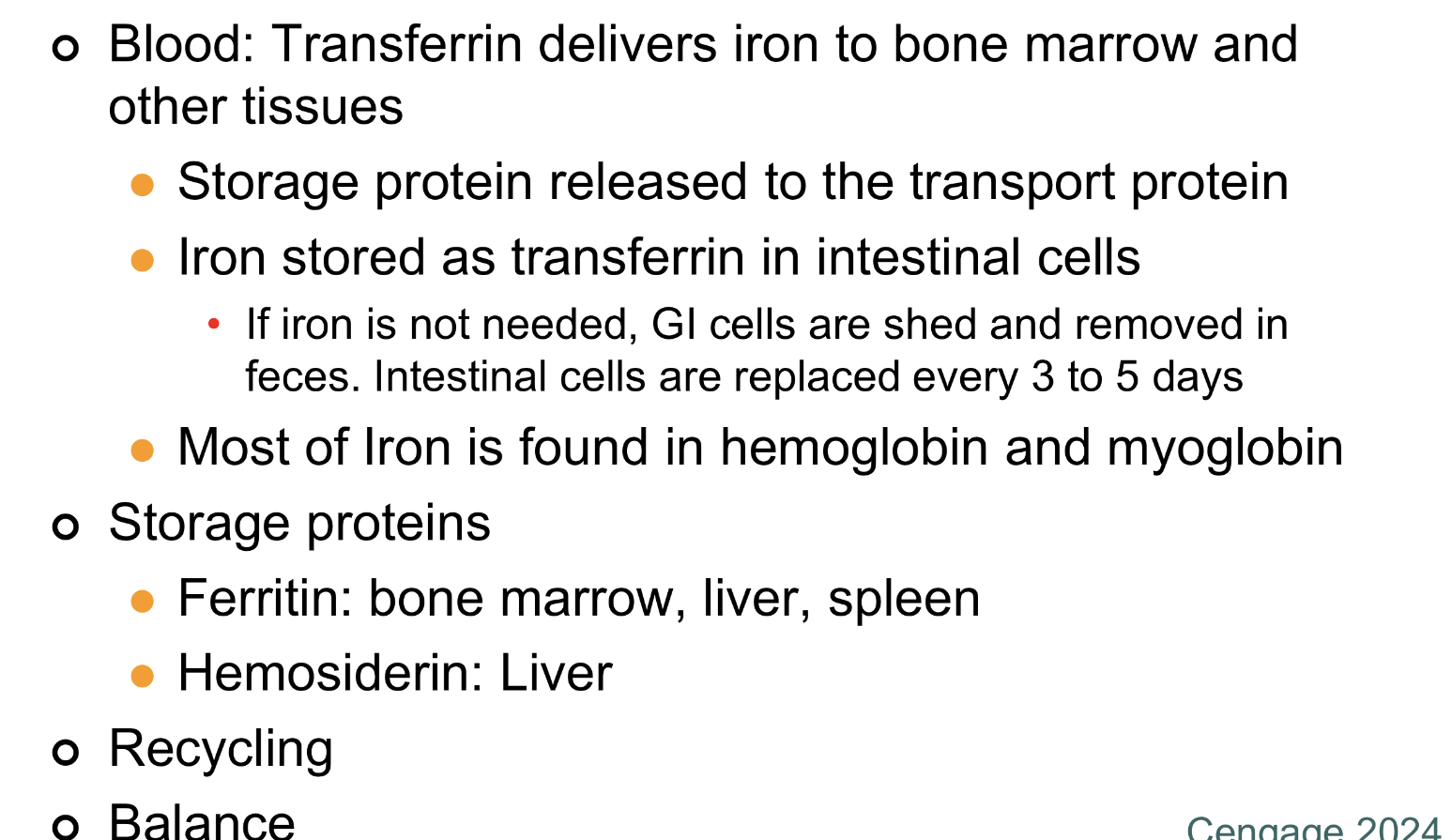
Iron transport and storage, what delivers iron to things? what is it totes as and where? what form is it found?
overview of iron metabolism, what are total daily iron losses and where do they occur in body?
Total:
1.0 mg (men)
1.4 mg (premenopausal women)
GI losses:
GI blood (Hgb 0.35 mg)
GI mucosal (ferritin 0.10 mg)
Bile (0.20 mg)
Desquamated skin cells and sweat (0.2-0.3 mg)
Urinary losses (<0.1 mg)
Menstrual losses (0.5 mg)
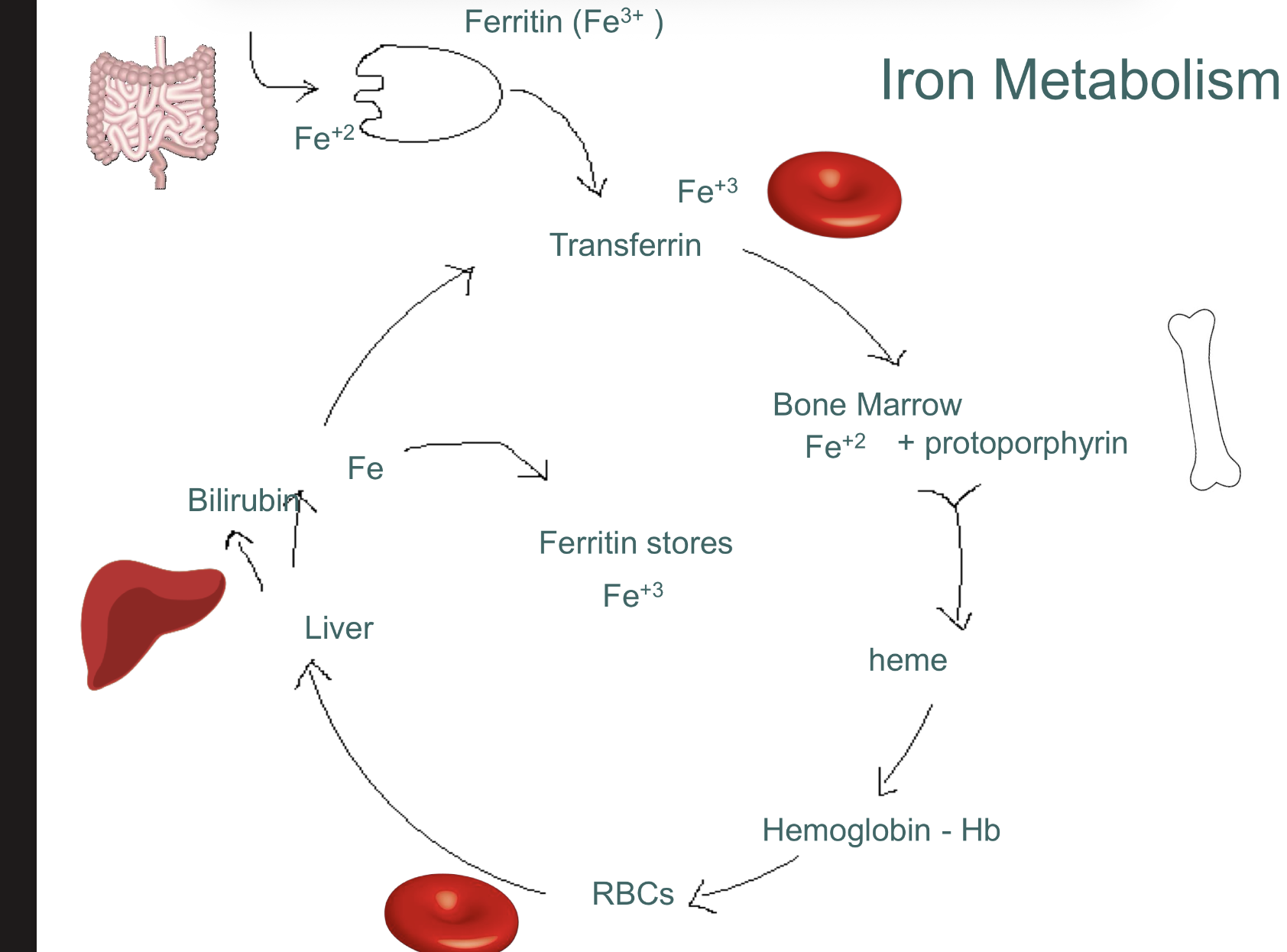
how is iron recycled in the body?
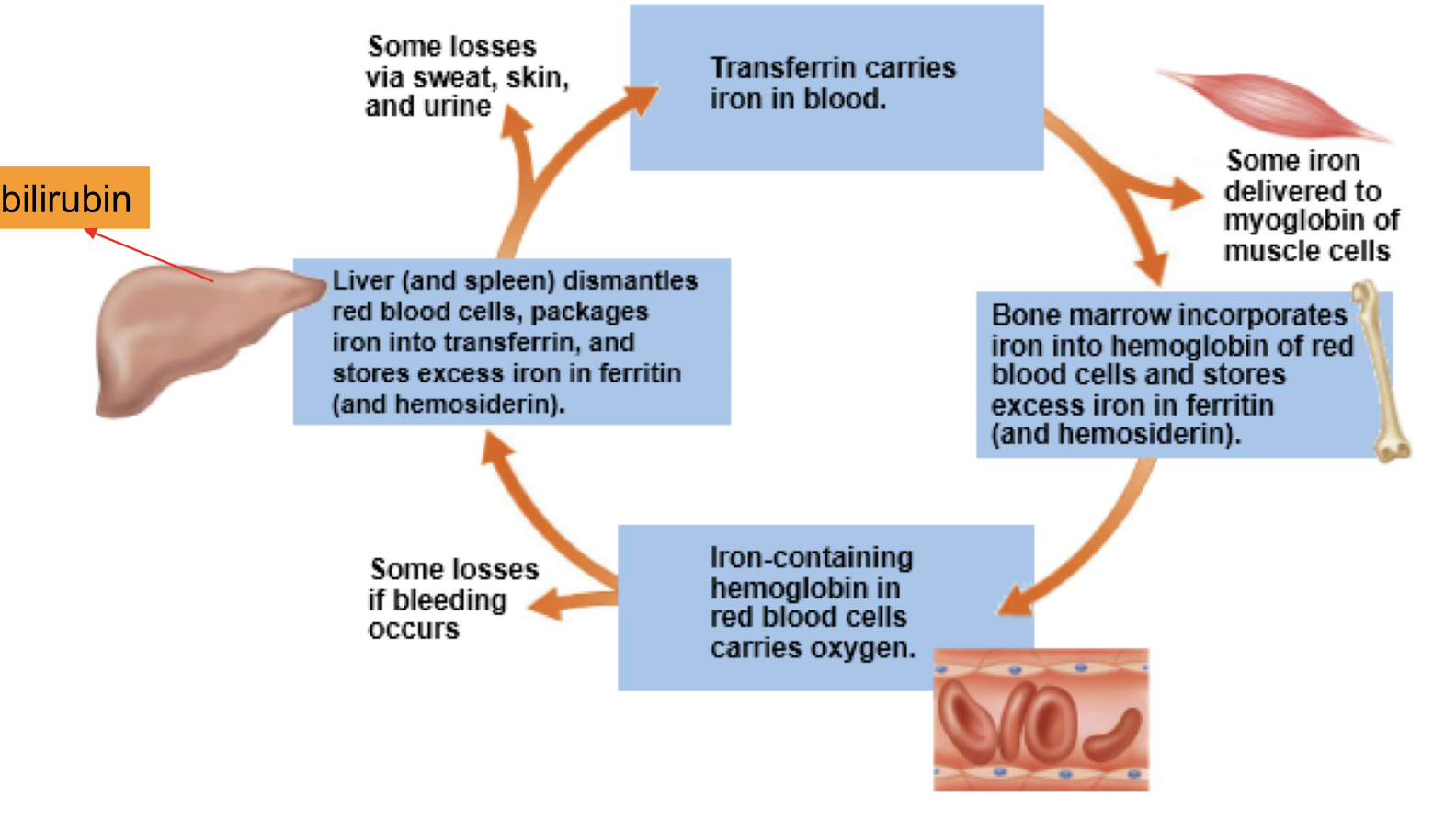
what hormone regulates iron balance? where does it come from?
HEPCIDIN produces from liver inhibits Fe absorption in mucosa if too much iron
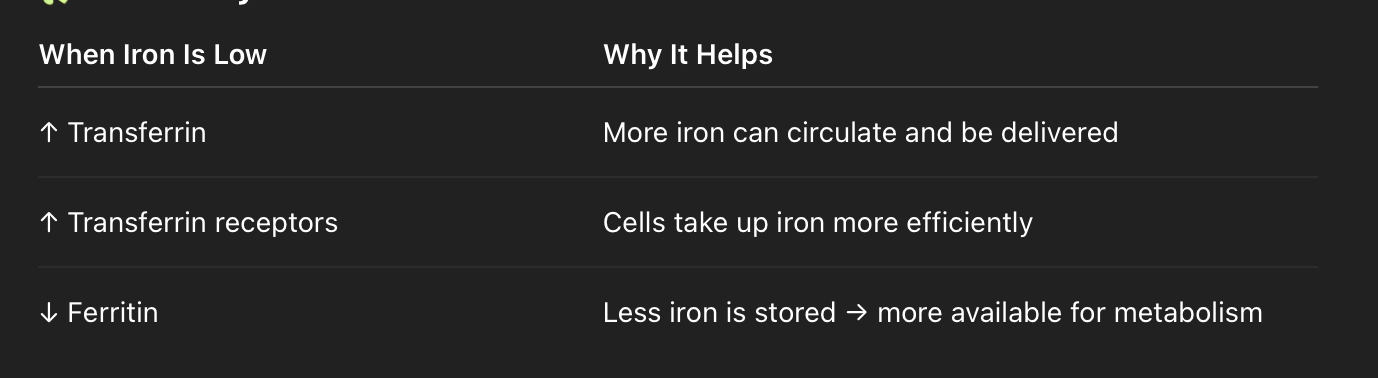
what are some adaptations to increase Fe availability during a deficiency?
Increase efficiency of absorption and
release from intestinal epithelial cells
Increase transferrin synthesis and
transferrin receptors
Decrease ferritin synthesis
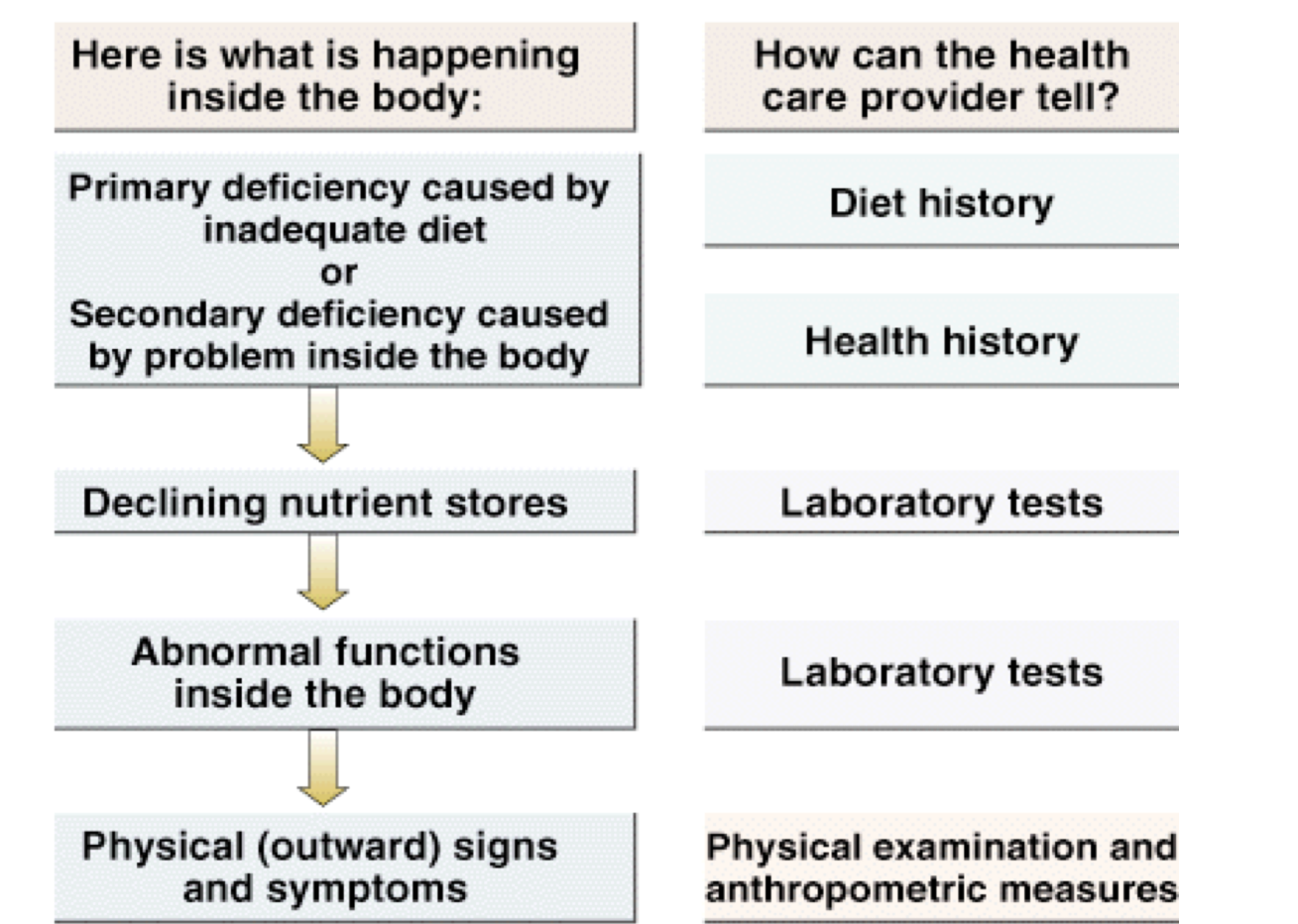
how can iron status be assessed? what are test at each point in deficiency ?
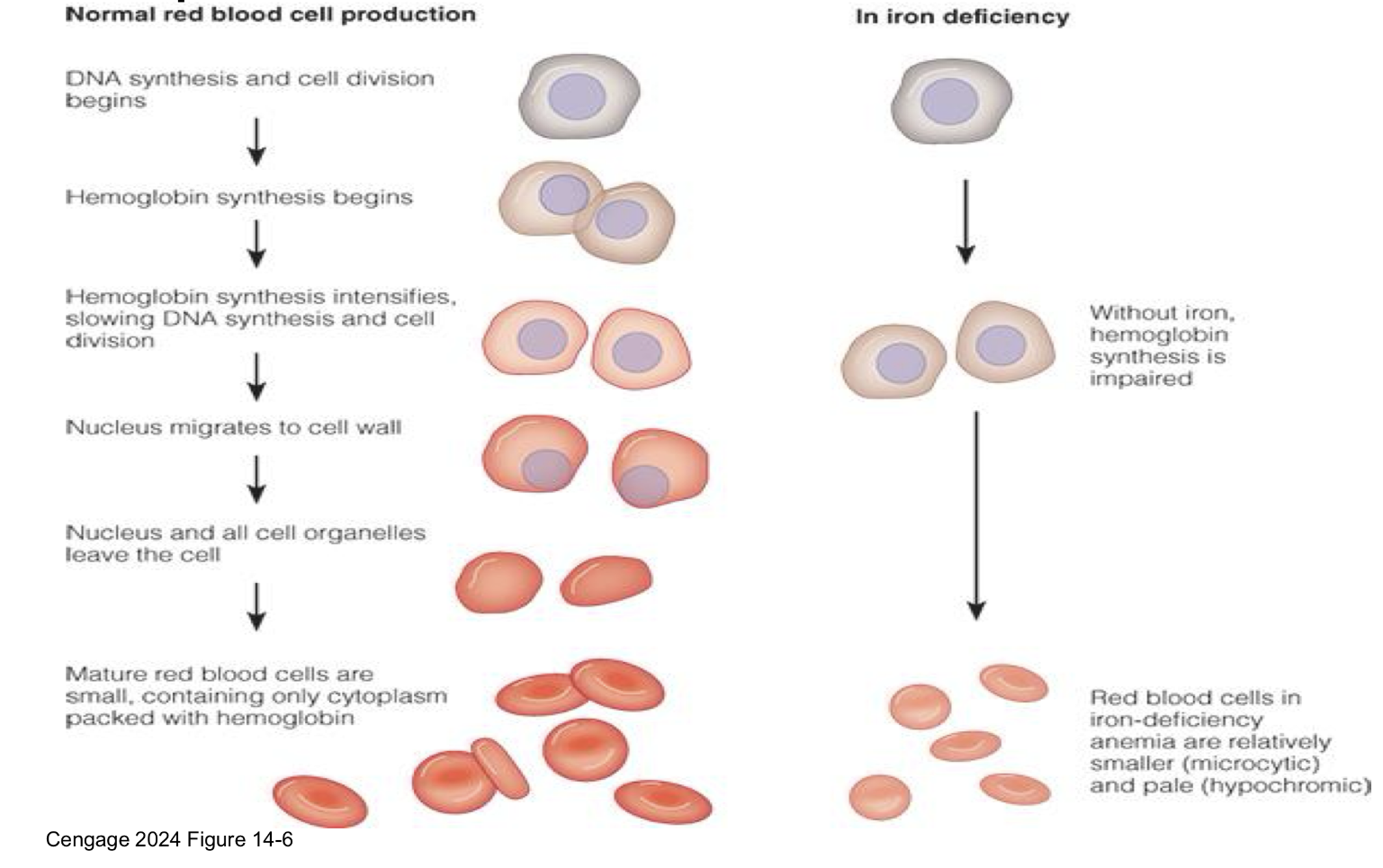
what does normal red blood cell look like vs when there’s iron deficiency?
what are 3 stages before full on iron deficiency anemia?
Stage 1: Depletion of iron stores
dec. serum ferritin blood levels
Stage 2: Changes in iron transport
inc. absorption efficiency, inc. transferrin receptors
inc. transferrin iron binding capacity
dec. transferrin saturation %, dec. serum ferritin in Blood
Stage 3: Defective erythropoiesis
dec serum iron
inc. Erythrocyte protoporphyrin, can’t make Hgb/Hct so it dec.
Iron Deficiency Anemia: Microcytic hypochromic erythrocytes
Associated behavioral signs get worse
Reduced stores: Blood: dec. Hgb/Hct, dec .MCV
what are iron deficiency anemia symptoms? what are the Hgb lvls for men vs women?
- Tired and pale
- work performance & mental productivity
- childhood development-psychomotor and
intellectual
- Pica- unusual food cravings
- lead poisoning susceptibility
Men: Hgb < 140 g/L
Women: Hgb < 120 g/L
what are 4 common causes of iron deficiency ?
1. Decreased dietary iron
Less iron absorbed
Vegetarian diets lack heme
2. Inhibition of absorption
Mineral Interactions: Calcium, zinc
supplements can dec. iron absorption
Absorption inhibitors
3. Increased red cell mass
Pregnancy, growth
4. Increased losses
GI bleeding (occult)
Heavy menstrual losses
Blood donation
what are Iron DRIs? what is treatment and prevention
Treatment=
diet, supplementation
BUT supps—> Less well absorbed than food
• Best forms: ferrous sulphate
or iron chelate, eat between meals or on empty
stomach with liquids
• note Vitamin C has no effect on absorption
Prevention=
improve diet quality, fortify foods
are there iron toxicity?
-there can be acue toxicity or poisoning!!
Megadoses of Vitamin C – Pro-oxidant (increases oxidative species -ROS)
the can reduce ferric iron bound to transferrin to free ferrous iron
free iron is a powerful oxidant: Fenton reaction=>BAD
what is Hemochromatosis? what can it lead to? symptoms? treatment?
= accumulation of iron in organs, joints… Can be fatal
Autosomal recessive, most common genetic disorder in US
More common in men than iron deficiency
- Can lead to Hemosiderosis (deposits of excess Fe)
Unneeded iron is absorbed (hepcidin)
Hemosiderosis = iron build-up
Hemochromatosis = iron overload disease
Symptoms: apathy, lethargy, and fatigue
Causes tissue damage (free radicals), infections
treatment= phlebotomy, chelation therapy, low iron diet…Vit.
what is microcytic vs macrocytic anemia?
Micro = small → iron issue (hemoglobin problem)
Macro = large → folate/B12 issue (DNA problem)
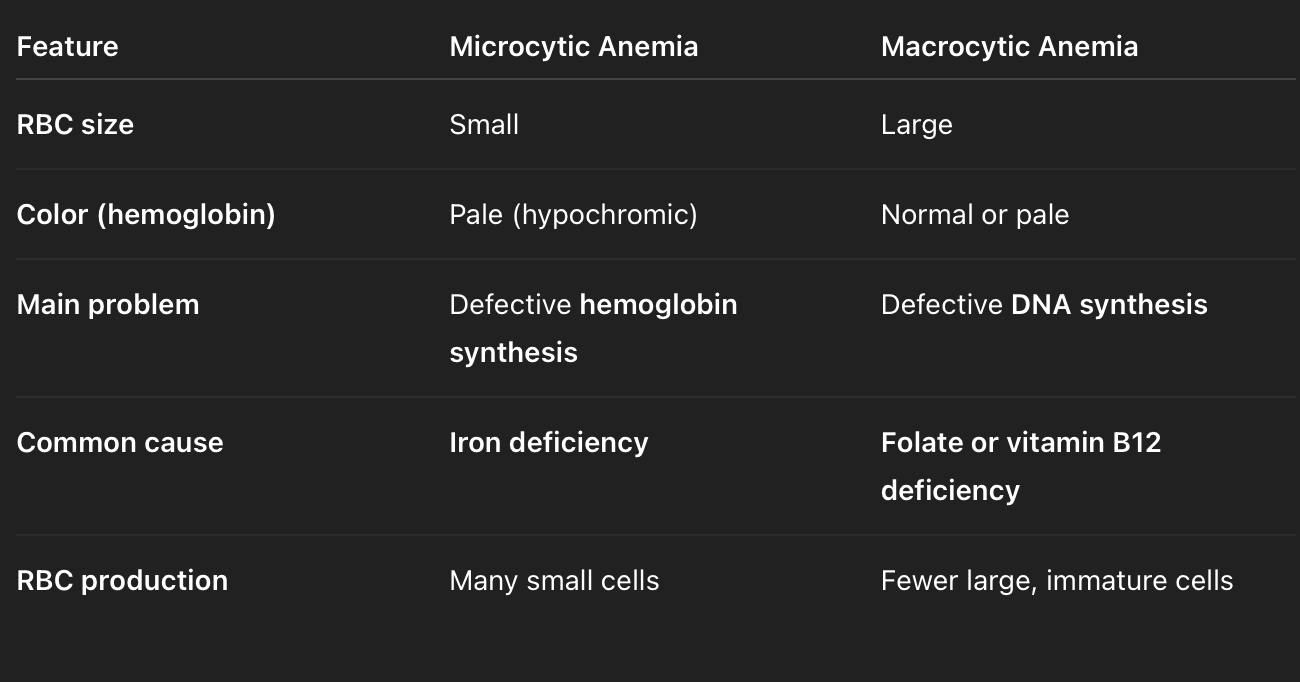
what is macrocytic anemia? what vit. deficiency is it linked with?
= when red blood cells (RBCs) are larger than normal (“macro” = large) and often fewer in number.
- Even though they’re big, they don’t function properly because they’re immature — they didn’t divide enough during development.
Cause | How it affects RBCs |
|---|---|
Folate (vitamin B9) deficiency | Needed for DNA synthesis → fewer, larger RBCs |
Vitamin B12 deficiency | Same mechanism (also causes neurological symptoms) |
Alcoholism or liver disease | Interferes with RBC production |
Certain drugs (e.g. chemotherapy) | Inhibit DNA synthesis |
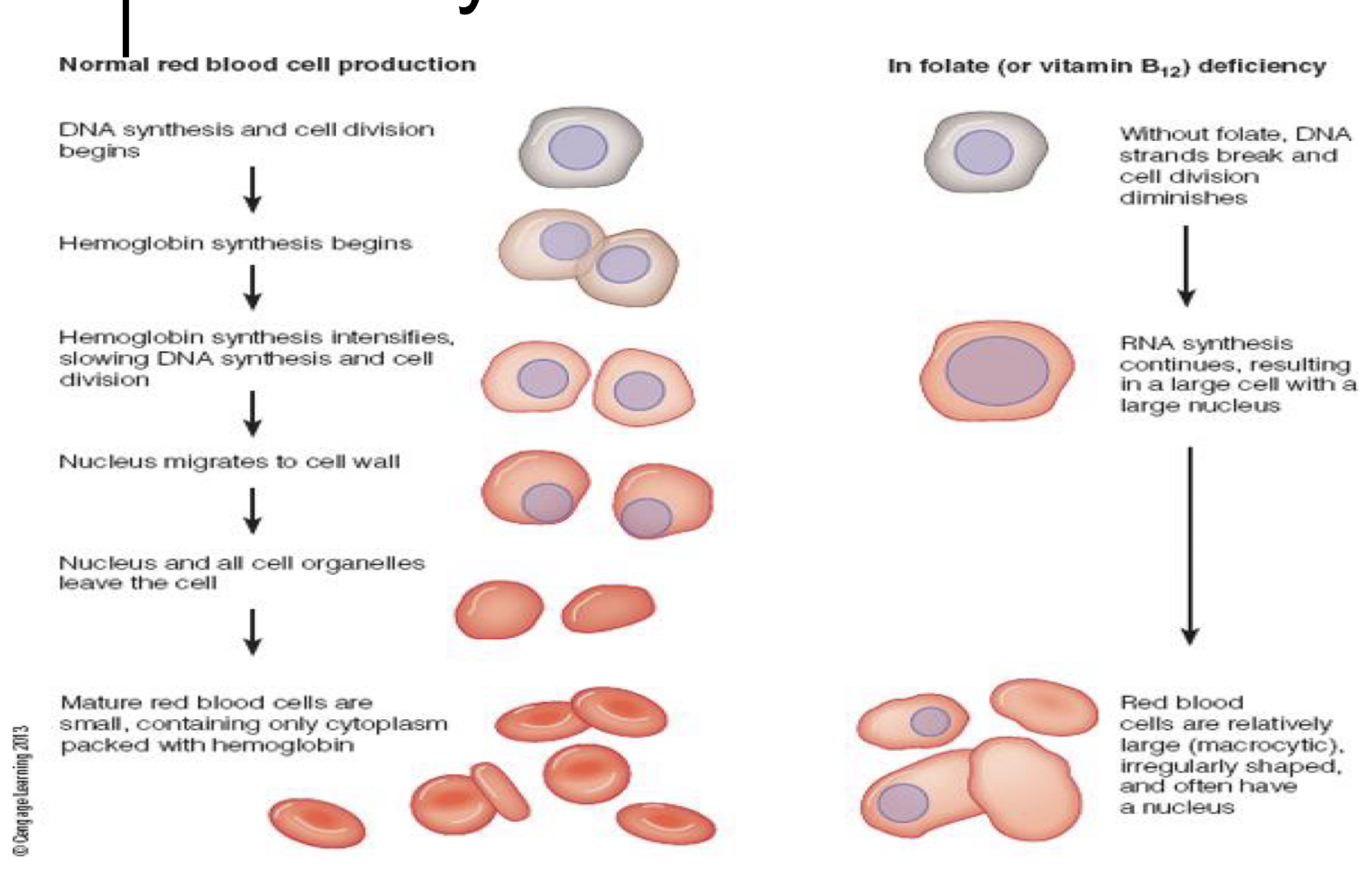
is megaloblastic anemia the same ad macrocytic?
Term | Meaning | Relationship |
|---|---|---|
Macrocytic anemia | General term for anemia where red blood cells (RBCs) are larger than normal (↑ MCV) | Broad category — describes size only |
Megaloblastic anemia | Specific type of macrocytic anemia caused by impaired DNA synthesis, usually due to vitamin B12 or folate deficiency | Subtype of macrocytic anemia |
Why Megaloblastic Happens
Folate or B12 deficiency → DNA synthesis slows down
RBC precursors in bone marrow keep growing but don’t divide normally
Result: large, immature “megaloblasts” in marrow and large RBCs in blood
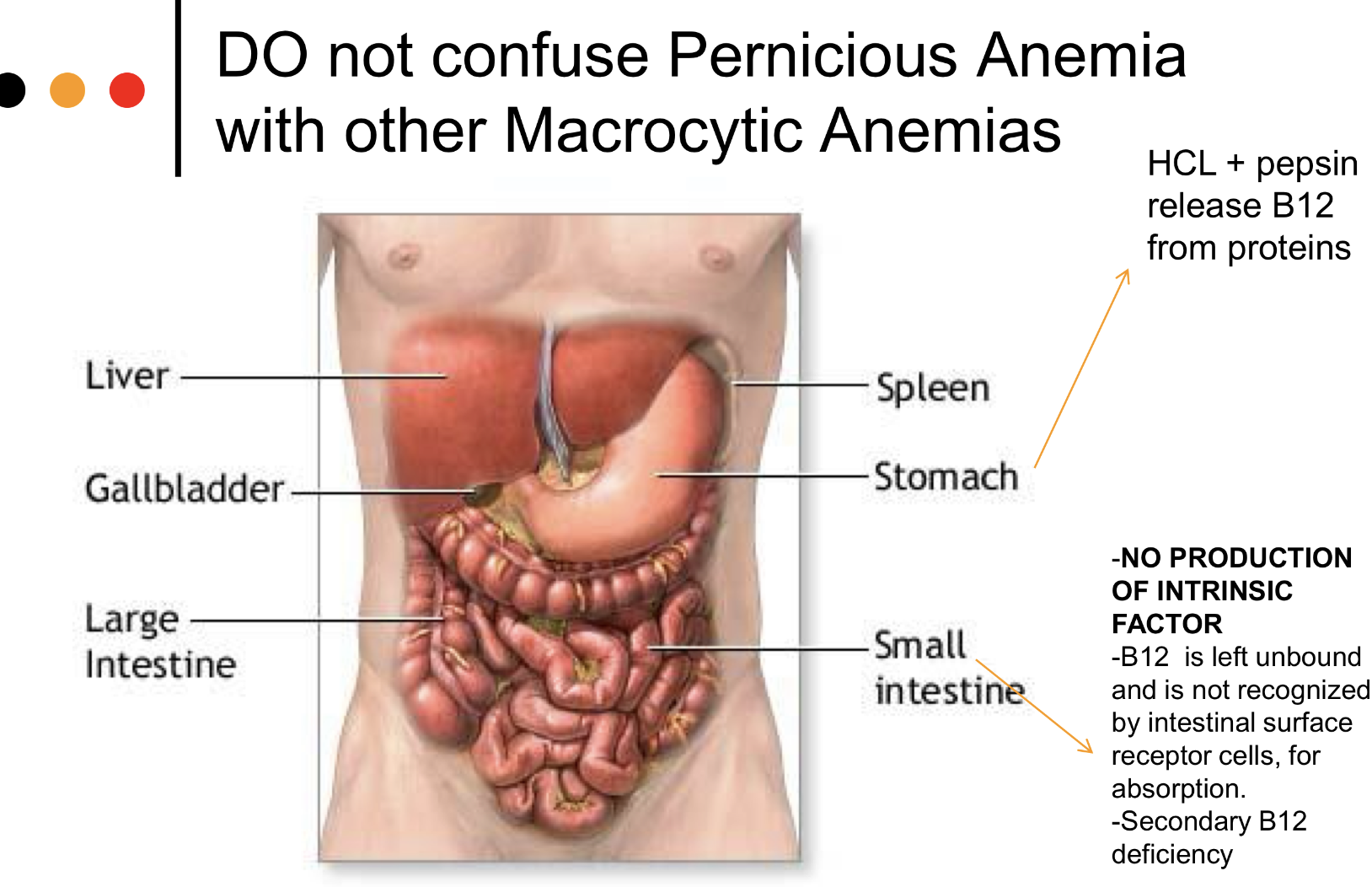
megaloblastic VS pernicious anemia? which one is primary vs secondary?
MEGA:
a primary deficiency, lack of dietary folate OR b12—> impairs DNA synthesis
very large mega RBCs
not common, slow development
PERNI:
a secondary deficiency, also causes large immature RBS
has a neurological component
CAUSE= intrinsic factor OR atrophic gastritis
ppl over 50 @ risk
what is Vit. B12 relationship to pernicious anemia?
Pernicious anemia is a type of megaloblastic anemia caused by a vitamin B₁₂ deficiency, not because of poor intake — but because the body can’t absorb B₁₂ properly, so caused by b12 secondary deficiency
B₁₂ absorption requires “intrinsic factor” (IF) — a protein made by parietal cells in the stomach.
In pernicious anemia, the immune system destroys these parietal cells or produces antibodies against intrinsic factor.
Without intrinsic factor → B₁₂ can’t bind and be absorbed in the ileum (small intestine).
This leads to B₁₂ deficiency, which → impaired DNA synthesis → megaloblastic anemia.
what are zinc functions?
works with proteins in every organ!!
Stabilizes cell membranes and DNA
Synthesis, storage, and release of insulin
Taste perception
Blood clotting, RBC synthesis
Thyroid hormone function
Immune function, wound healing
release of vitamin A from stores
Growth and development, reproduction – sperm development
influences behavior and learning performance
explain zinc absorption and enteropancreatic circulation

what are some zinc absorption enhancers vs inhibitors?
ENHANCERS= acids, amino acids
INHIBITORS= phytates, oxalate, polyphenols, insoluble fibers, folate
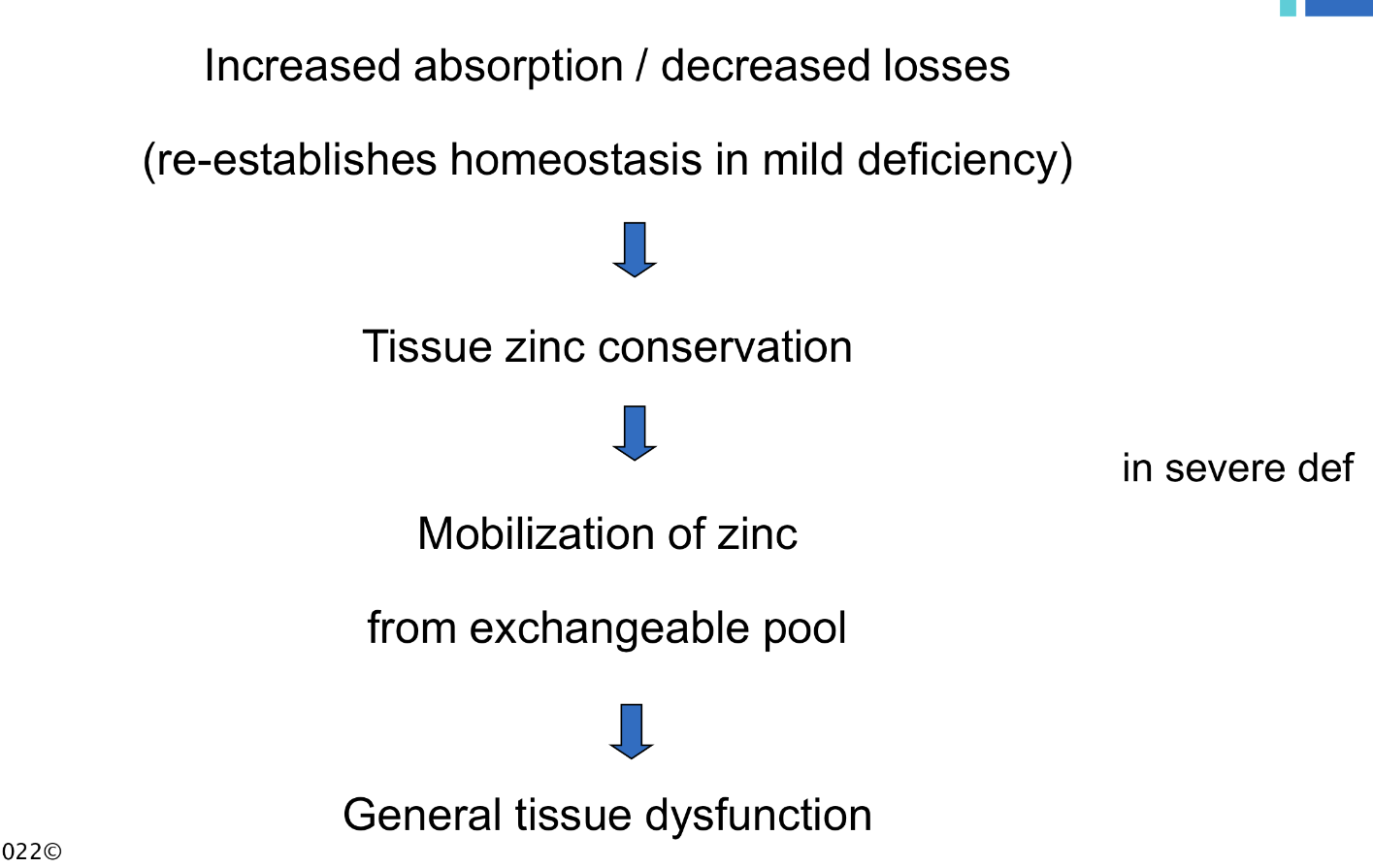
what are stages of zinc deficiency? info on zincdeficiency, who’s most vulnerable?
Difficult to diagnose
No sensitive and specific test
affects Thyroid and Pancreatic function, GI function,infections
Children most vulnerable!!
Compromised growth and development
- stunting
Poor appetite, diarrhea
Poor cognitive and motor development
Impaired immunity
Poor wound healing
Widespread in developing world
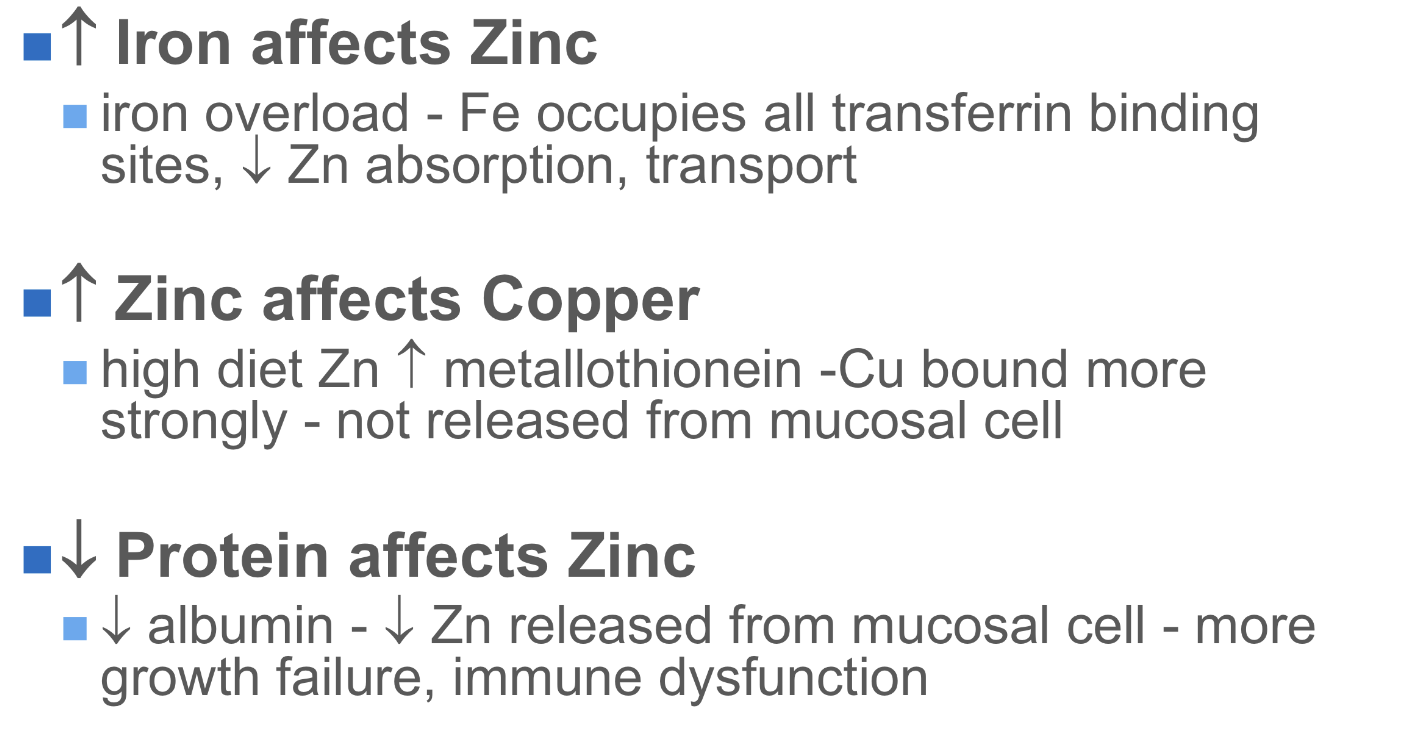
zinc toxicity symptoms, what could Zn interfere with?
Rare!
UL= 40 mg Zn
Zn excess interferes with copper(Cu) and Fe metabolism
Symptoms:
Acute toxicity: Nausea, vomiting, diarrhea
Chronic Zn Toxicity:
causes Cu deficiency, alter Fe function and conversion Fe2+ to Fe 3+
Increased intestinal metallothionein
Copper not released into blood, lost in shed mucosal cells
Reduced immunity, urinary problems
May decrease HDL (“good”) cholesterol in the blood
chromium info, what does it work with? what are some food sources?
Works with insulin to regulate and release energy from glucose
Food sources:
Unrefined foods, whole grains, liver, nuts, cheese
copper info, what doe sit help form?
Helps form hemoglobin and collagen and defense against oxidation, in many enzymes: E.g., ferrous to ferric iron
Food sources:
Organ meats, seafood, nuts, seeds
Genetic disorders that affect copper status
Menkes disease
Wilson’s disease
how does inc. iron affect zinc? how does inc zinc affect copper? how does dec protein affect zinc?
Iodine vs iodide, what hormones is it a part of? important for?
Iodine = found in foods, GI tract converts iodine in food to iodide
Iodide = the form found in the body Dietary, readily absorbed by the body
Needed in miniscule amounts
Part of thyroid hormones (i.e., thyroxine)
Important for:
Regulate body temperature
Regulate metabolic rate
Control rate at which cells use oxygen
Nerve and muscle function and brain development
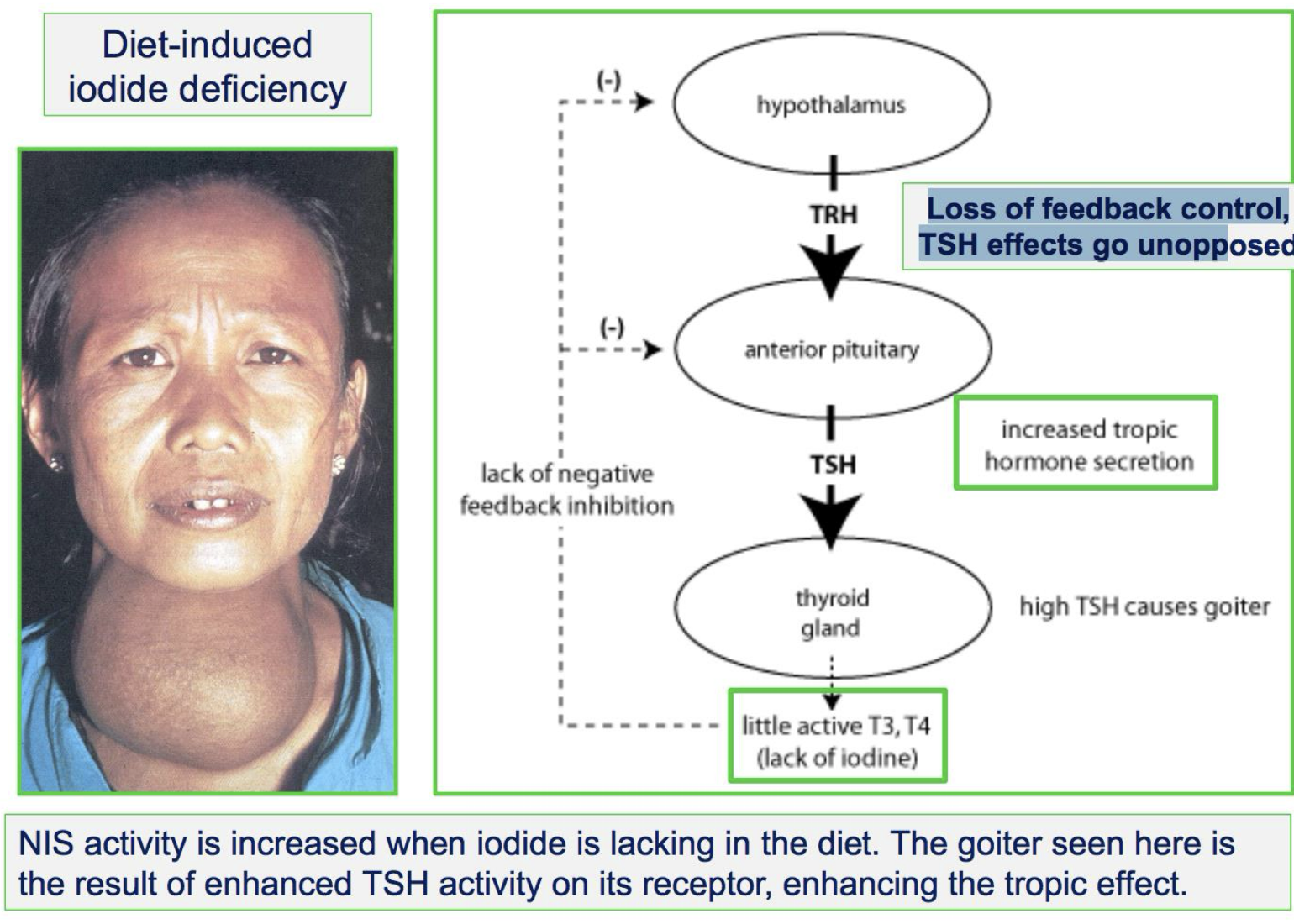
what does iodine deficiency look like?
goiter, enlarged thyroid gland bc Increases uptake of iodide causing goiter
Other signs include mental impairment and brain
damage, irreversible if not treated
During pregnancy, leads to cretinism
Goiter—> Continued deficiency
Cretinism—> Severe deficiency in pregnancy, Irreversible physical and mental retardation
iodine toxicity, what does it interfere w and what does it look like
-UL= 1100 ug
Interferes with thyroid function: Enlarges thyroid gland, just like with deficiency
Pregnancy: exposure to high intakes
from supplements, foods, meds
dangerous: goiter formation
Goiter in an infant exposed to toxic
amounts – blocks airways - death
what are trace mineral in low quantities in body?
no DRI values
Nickel: a cofactor for enzymes
Silicon and vanadium: important in bone
health
Cobalt: part of vitamin B12
Boron: important in bone health, brain
activity, and immunity
are all trace mineral beneficial? what are ‘bad’ ones
Contaminant minerals!
Interfere with nutrient functions; diminishes health
Heavy metals—> Enter food supply via soil, water, and air pollution
lead:
Indestructible, chemistry remains unchanged
Displaces iron, calcium, and zinc
Children with iron deficiency especially vulnerable
Mercury
Cadmium