PSY260 Lecture 11: Plasticity in Damage/Injury
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
Terminology Surrounding Brain Damage
“Damage“ is a relative term, and what we usually mean is change
Our brains are constantly changing tin response to their environments
Sometimes good: learning, growing adapting
Sometimes bad: damage, injury, deterioration
Some wear-and-tear to our brains is inevitable
Brain Damage: Causes
Congenital/developmental
Genetic disorders; prenatal infections, exposure to toxins in utero, nutritional deficits during development
Trauma
Birth trauma, falls/accidents, concussions, blast/penetration, injuries
Vascular
Stroke, high/low blood pressure
Metabolic
Nutrition deficits, includes drug abuse
Infections
Tumours
Inflammation
Even when activated by the body as a defense
Brain Damage: Distribution
Focal
Diffuse
Mixed
Focal Brain Damage
Damage contained to a specific area or region
Ex. stroke, tumour, focal ifections
Can be easier to find relationships between damage and symptoms
Because the damage is localized
Often better prognosis because other undamaged regions can take over functions
Compensation with plasticity
Diffuse Brain Damage
Widespread across multiple brain regions
Ex. traumatic brain injury (shakes whole brain), hypoxia, infections, neurodegenerative diseases
More complex symptom profiles → multiple systems affected
Harder to target rehabilitation
Located in multiple places
Mixed Brain Damage
A combination of focal and diffuse damage
Can originate in one place, then spread outwards
Brain Damage: Timing (During Gestation)
1st trimester:
Damage tends to affect development of major structures
Disrupts foundational development, tends to be most severe
BUT maximum potential for alternative development pathways due to extreme plasticity
2nd trimester:
Damage tends to affect cortical organization
Recovery depends a lot on extent and location of damage
3rd trimester:
Damage tends to be more focal
More areas are developed
Still significant plasticity, but more constrained than earlier periods
Brain Damage Timing: Infancy
Very high plasticity, especially in sensorimotor areas
Language can still lateralize to the right hemisphere if the left is damaged at this stage
Can still compensate
Brain Damage Timing: Childhood
Early (2-7):
Strong plasticity
Recovery potential remains very good
Late (7-12):
Plasticity starts to decline
Recovery more dependent on targeted interventions
Greater need for good treatment
Brain Damage Timing: Adolescence
Plasticity slows
Frontal regions still highly modifiable
Keep developing until mid-20s
Frontal and PFC
Brain Damage Timing: Adulthood
Brain development completed at mid-20s
Gradual decline in natural plasticity
Recovery requires more active intervention and practice
Increasing importance of cognitive reserve
Building up alternative pathways BEFORE brain damage to help with compensation if there ever is any
Brain Damage Timing: Older adulthood
Higher vulnerability to damage
Plasticity still present, but even more reduced
Recovery often takes longer
Recovery focused on functional compensation
Trying to use what’s still working better
Instead of trying to recover what is damaged
Cognitive reserve very important for outcomes
Building up alternative pathways BEFORE brain damage to help with compensation if there ever is any
Brain Reorganization
Equipotentiality
Vicariation
Equipotentiality
When an area in one hemisphere of the brain is damaged, the corresponding area in the other hemisphere can take over its function
Ex. language development in infancy can switch to right if left is damaged
Vicariation
Reorganization of other (adjacent) brain areas take over function of a damaged area
Same hemisphere → nearby brain regions
Structural Reorganization
Angiogenesis
Spinal neuroplasticity
Angiogenesis
Formation of new blood vessels
Especially following vascular damage
↑ O2 carrying ability
Can increase with aerobic exercise
Spinal neuroplasticity
Growth of new synaptic spines
Changing network
Rare to see new neurons (neurogenesis) outside of gestation-infancy
Functional Reorganization
Ipsilesional reorganization
Contralateral reorganization
Crowding effect
Ipsilesional Reorganization
Same side as lesion → like vicariation
Ex. right premotor cortex taking over right primary motor functions following rM1 damage
More likely following mild/moderate damage, focal damage
Contralateral Reorganization
Opposite side of lesion → like equipotentiality
Ex. right hemisphere taking over language processing following left hemisphere damage in utero/infancy
Crowding effect
More likely following moderate/extensive damage, diffuse damage
Crowding effect
Deficits in the functions typically supported by the repurposed hemisphere
Ex. right hemisphere normal function may suffer because it takes on additional responsibility of lef hemisphere functions
Adaptive Neuroplasticity
Refers to any structural or functional change that is beneficial
Changes that improve function
General examples
Learning new skills
LTP
Strengthening/increasing efficiency of useful circuits
Recovery of function following injury
Maladaptive Neuroplasticity
Refers to structural or functional changes that are harmful
Changes that worsen function/cause problems
General examples
Phantom limb pain
Other forms of chronic pain
Trauma flashbacks
Critical Periods
Both timing of damage AND treatment factor into effectiveness
Trying to force rehabilitation too early → can have adverse effects
First 24-48 hours after stroke → not recommended
Most rapid recovery occurs first 3-6 months after damage/injury
This is where the greatest gains are made
Not to say that there can’t be recovery after
Recovery can continue for months or years after injury
Promoting Plasticity
Task-specific training/practice
Environmental enrichment
Non-invasive brain stimulation
Medications
Promoting Plasticity: Task-specific training/practice
Do the thing you’re struggling with
Try to directly restrengthen damaged pathway
May also inhibit use of compensatory strategies
Constraint-Induced Movement Therapy (CIMT)
Ex. stroke recovery → restrain working arm to force use of damaged arm
Can be frustrating
Promoting Plasticity: Environmental enrichment
Sensory stimulation, social interaction, cognitive challenges
Use of tools and other stuff to challenge brain
Promoting Plasticity: Non-invasive brain stimulation
TMS, tDCS
Use to manipulate brain activity
Relatively new
Increase plasticity in affected areas
Inhibit compensatory areas
Like CIMT for brain
Promoting Plasticity: Medications
Certain stimulants, SSRIs, cholinesterase inhibitors
Relatively new
Psychedelics: ayahuasca, DMT, psilocybin, and LSD
Can increase neurotransmitters (serotonin) which promote plasticity
“AL“ Phantom Limb Pain: Damage
35 year old man whose right leg was amputated after a car crash
Activity in the part of his primary somatosensory cortex (S1) that corresponded to the missing leg → experienced as phantom pain
Could light up as part of other pathways
Said it felt like his foot was flexed and he couldn’t unflex it
“AL“ Phantom Limb Pain: Symptoms
Touching thigh above amputation point elicited sensations in phantom toes
Researchers had a volunteer (V) place her right leg near the phantom lef
Seeing V’s leg touched → could feel sensation in his phantom leg
When V pointed her foot → felt relief in his phantom leg, as if it was unflexed
Also felt relief when V’s foot was massaged
Mirror Visual Therapy (MVT) offered temporary relief
“AL“ Phantom Limb Pain: Treatment
Pain medications were NOT effective
Mirror Visual Therapy (MVT) → temporary relief
Psilocybin → temporary relief
Helps ↑ plasticity → S1 area of missing limb can remap over time
MVT + psilocybin → lasting relief from the pain
AL felt less pain with time
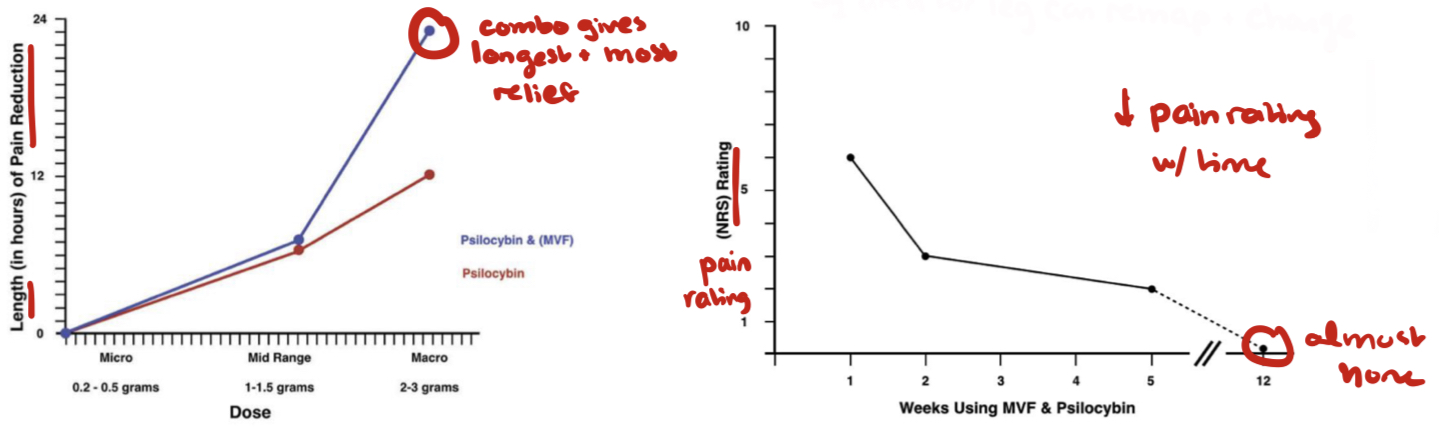
“AL“ Phantom Limb Pain: Conclusions
~95% of people who undergo amputations experience phantom pain or itching
Very common, almost expected
Effectiveness of MVT helps us understand the role of mirror neurons
Neurons that respond to watching someone else undergo a sensation
Involved in empathy
Effectiveness of psilocybin helps us understand the role of serotonin in promoting neuroplasticity
May make brain more receptive to MVT
When used in combination with MVT, can lead to lasting pain relief
“Anonymous Frenchman“ Hydrocephalus: Symptoms
44 year old male went to hospital with mild weakness in his left leg
Lived a normal life, worked, had a family
IQ was 75ish (below average but normal still)
Diagnosed with hydrocephalus (extra fluid in brain) as an infant
Treated with a stent to drain fluid,
Was removed at age 14
No other physical or cognitive symptoms reported
“Anonymous Frenchman“ Hydrocephalus: Damage
Significantly enlarged ventricles
HUGE and filled with CSF, took up ~90% of the space within his skull
Remaining brain matter compressed to the areas right around his skull
SEVERE squishing
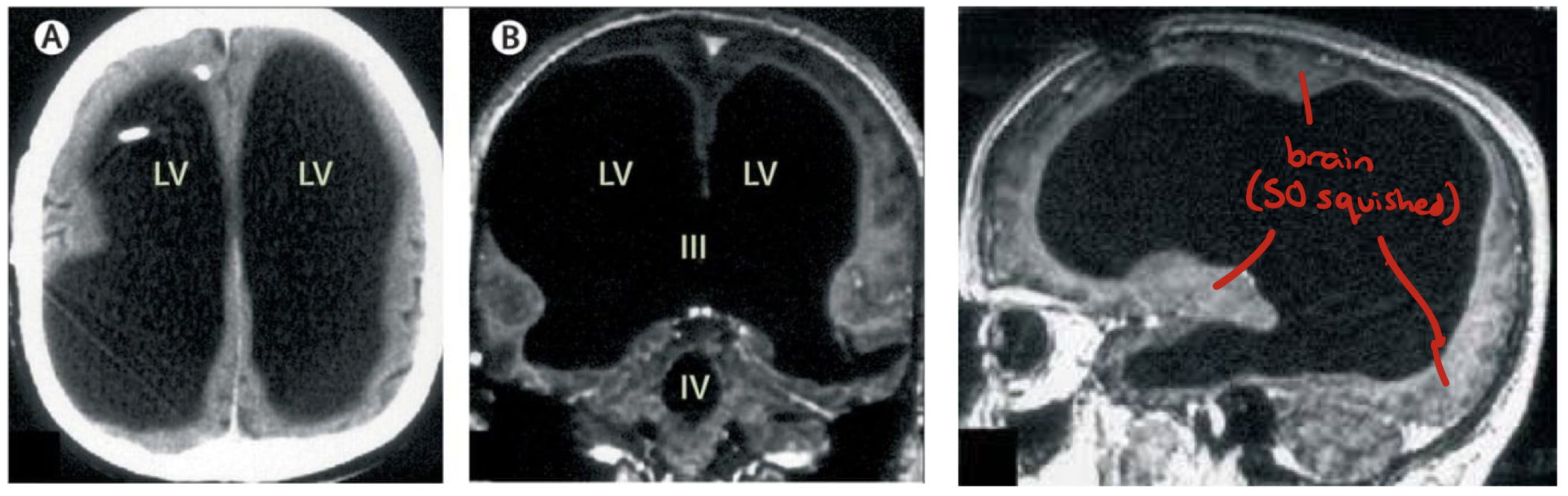
“Anonymous Frenchman“ Hydrocephalus: Conclusions
Unclear whether his neurons had died or been squished over time
Likely a combination
If damage occurs gradually enough, the brain has a remarkable ability to find ways to continue functioning normally
Speed matters → faster will cause a lot more damage
His brain had likely been having to constantly rewire and form new compensatory networks as more fluid collected in the 30 years after his stent was removed
Constant compensatory plasticity
Amount of damage doesn’t necessarily correlate with severity of symptoms
Jason Padget (“Math Guy“) Acquired Savant Syndrome: Damage
Suffered blow to the back of his head while getting mugged
Suffered a concussion
Damage was primarily in temporal and parietal lobes
Mostly in the left hemisphere
Ended up being beneficial
Jason Padget (“Math Guy“) Acquired Savant Syndrome: Aftermath
Developed OCD and PTSD after injury
Also began to see the world through the lens of advanced math
Began to perceive geometric patterns that mapped onto patterns in math and physics
Jason Padget (“Math Guy“) Acquired Savant Syndrome: Considerations
Reliance on self-report
Told his own story via social media, could be exaggerated
Intuitive understanding of geometric patterns sometimes overstated as a general genius across all math
May be more accurate to think of it as a perceptual phenomenon, more like synesthesia (pairing sensory types)
Math Guy: Similar Cases
Orlando Serrell:
Hit with a baseball → developed calendar calculating abilities
Anthony Cicoria:
Struck by lightning → developed sudden musical abilities
Tommy McHugh:
Stroke → artistic abilities
All seem to gain less verbal abilities (mathematical/artistic)
Damage is often on left, new abilities often associated with right hemisphere
Jason Padget (“Math Guy“) Acquired Savant Syndrome: Conclusions
Only 30-40 cases diagnosed with acquired savant syndrome
Often resulting from left hemispheric damage
Often involved acquisition of new abilities related to math, music and art
Functions typically associated with right hemisphere
Theory of Paradoxical Functional Facilitation
Damage may release right hemisphere areas from interference, uncovering latent abilities
TMS that inhibits left hemisphere → can produce similar improvements in perception/artistic ability
Effects are much more transient/temporary with TMS
tDCS is not powerful enough to last
“Jan“ Broca’s Aphasia: Overview
Stroke at age 31 in the left frontal cortex
Affected language production (Broca’s aphasia)
Could still understand and knew what he wanted to say
Couldn’t produce the words to say it
Affected strength and coordination in right side of the body
Contralateral
Struggle with planning
With lots of rehab, gradually gained back ability to walk and talk