SNAB biology topic 6
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
How can the time of death of a mammal be measured?
- Body temp
heat-producing metabolic reactions stop, body temp cools down to reach ambient temp. (only useful up to 24hrs after death) Also depends on size of the body, covering and weather.
- Degree of Muscle Contraction
Rigor mortis (aerobic reactions cannot take place) therefore ATP is depleted. Without ATP the cross bridges between actin and the globular myosin heads cannot be broken, therefore muscle remains contracted
- Insects/entomology
type of insect in life cycle stage shows extent. Determination of age of insects present enables determination of time of death
- Stage of succession
As body decays the species colonising the body change. Therefore analysis of the community present can be used
- Extent of decomposition → carried out by decomposers (bacteria and fungi) → contribute to the recycling of carbon
Role of decomposers in the carbon cycle
Decomposers break down organic material
When they respire they release CO2 back into the atmosphere
Explain how microorganisms break down organic material such as wheat stems which are ploughed into soil
The stems contain starch or cellulose
The microorganisms release enzymes which break down the glyosidic bonds
This releases glucose which is then used by the microorganisms in respiration
Extent of decomposition
Decomposers break down cells and tissue after a few days. Skin will appear greenish in colour
Over the next few days or weeks is the breakdown of tissue and organs. This process produces gases which will lead to bloating. Skin will blister and fall off the rest of the body
A few weeks after death the remains of the soft tissue will turn to liquid which becomes visible as it leaves the body
This continues for months or years until just a skeleton remains. Then after a few decades the skeleton will disintegrate until nothing remains
Ambient temperature on the rate of decomposition
When the body reaches ambient temperature it is at the temperature of its surroundings therefore the at its lowest body temperature.
This means rate of decomposition will decrease
Enzyme activity will decrease
Growth rate of decomposers (bacteria/fungi) will decrease
Describe the changes that occur within the body in the first week after death (PPQ)
Body temperature falls
Break down of cells by enzymes in the body (autolysis)
Rigor mortis (stiffening of the muscles)
Discolouration
Bloating
how is DNA profiling used and what is it used for
- used to identify and determine genetic relationships between organisms
- profiling through gel electrophoresis
Before a sample can be analysed via DNA profiling, the sample needs to be amplified using….?
Polymerase chain reaction
DNA Revision: What does DNA being antiparallel mean?
The 2 strands are parallel to each other but run in opposite directions
One strand runs from 5’ to 3’, while the other runs from 3’ to 5’.
Where does DNA Polymerase bind to and in what direction does it work in?
DNA Polymerase binds to the 3’ end of the template strand
It adds complementary nucleotides to the 3’ end of the 5’ to 3’ growing strand
Therefore it moves in the 3’ to 5’ direction in relation to the template strand
And in the 5’ to 3’ direction in relation to the synthesis of the new strand
What is a nucleotide?
Building block of DNA consisting of:
A nitrogenous base (Adenine, Guanine, Cytosine or Thymine)
Deoxyribose or ribose
A phosphate group (which provides the energy for reactions involving the nucleotide)
Polymerase chain reaction (one cycle)
A reaction mixture of the DNA sample, primers, free nucleotides and DNA Polymerase is set up
Denaturing - The mixture is heated up to 95 degrees to break the hydrogen bonds between the 2 strands of DNA (sample DNA), this is done for about 30 seconds
Annealing - Mixture is then cooled to a temperature between 50-60 degrees depending on the type of primers used so that they can anneal (bind) to the single stranded DNA templates. Cool enough for hydrogen bonds to form between the primer and strand (20 seconds)
Elongation - Temperature is increased to 72 degrees (which is the optimal temp of DNA Polymerase). DNA Polymerase forms the complementary strand of DNA by forming phosphodiester bonds between the free nucleotides.
This produced 2 double strands of the the sampled DNA effectively doubling the quantity of DNA every cycle
Temperatures used in the marks schemes were 95, 55, 70
In a PCR one of the reagents must always be in excess
How would you determine the optimum number of cycles for the PCR used to amplify the DNA (PPQ)
One of the reagents should be in excess e.g. mononucleotides, to ensure optimal amplification
Make sure the control the temperatures 95, 55, and 70 degrees during the cycle
Start with one cycle, then use gel electrophoresis to measure the quantity of DNA produced
If the bands are not observable then you must increase the number of cycles
Choose the smallest number of cycles that produce a clear observable band.
Primers (PPQ)
Primers have a specific base sequence
They bind to complementary bases at 3’ end of a DNA strand
This is to provide a site for the DNA Polymerase to bind and form a complementary strand
Restriction enzymes
Restriction enzymes cut at a specific DNA base sequence
This allows for comparison of fragment sizes which can be used to identify differences between samples due to the variation in DNA sequences of the 2 samples
For example, if a restriction site is present in one sample and absent in another, the sample with the site will have more fragments and potentially different fragment sizes
Explain the steps of gel electrophoresis
1) obtain sample of DNA from organism
2)PCR - DNA amplified so 20-40 copies made. Primers anneal to strands, free nucleotides bind. Mixture heated to break H bonds, and then reduced so complementary base pairing
3) fragment of DNA cut using restriction enzymes (cuts at SPECIFIC DNA base sequences)
4) Fluorescent markers placed in mixture
5) DNA samples loaded into wells in agarose gel which is then placed into the electrophoresis tank with buffer
6) Electric current is passed through the agarose gel by a potential difference being applied across
7)Position of the bands produced can then be compared
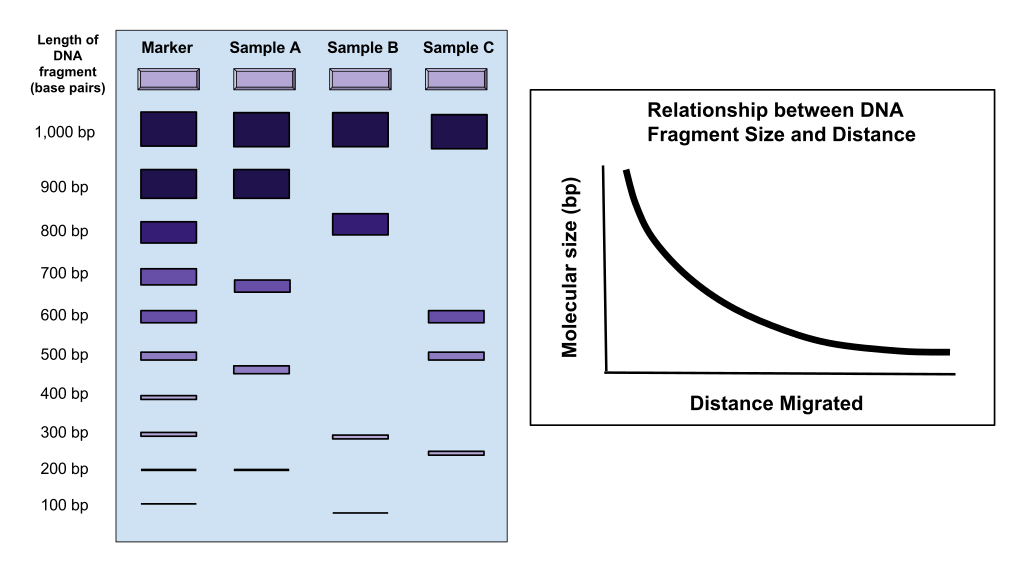
Charge of DNA?
DNA has a negative charge therefore it moves from cathode to anode
How DNA profiling can be used to show that 2 populations are a different species
Obtain the DNA from the two different populations
Use restriction enzymes on the DNA to produce fragments of DNA
Use gel electrophoresis (the use of agarose gel and an electric current) to analyse the samples of DNA by separating the fragments
More differences in the pattern of bands produced from the 2 samples would indicate that the 2 organisms from the 2 separate populations are different species
Compare the structures of bacteria and viruses
virus:
-lyptic or lysogenic (HIV is both)
- protein coat
- no flagellum
- nucleic core contains DNA or RNA
- needs host to survive
- smaller than bac.
- no organelles
- no membrane bound organelles
- linear DNA
- don't have plasmids
bacteria
- contains cell wall made of polysaccharides
- has flagellum
- Circular loop of DNA in cytoplasm
- no host needed
larger
- contains organelles
- no membrane bound organelles
- Circular DNA
- have plasmid
-pilli involved in gene transfer
Explain the sequence of events which occur when the HIV virus is introduced to the body
- HIV has attachment proteins (GP120), which attach to CD4 receptors on cell membrane of T-helpers
- viral envelope fuses with the cell membrane of the T helper cell
- capsid releases RNA and the enzymes into cell cytoplasm
-Reverse transcriptase uses the viral RNA template to synthesise a strand of DNA for both strands of viral RNA, then the 2 strands combine to produce double stranded viral DNA.
-Viral DNA then moves to the nucleus of the cell
- Integrase integrates viral DNA into host's DNA.
-transcription of the DNA within the nucleus now results in the production of viral RNA
- This viral RNA can serve as the genome for new viruses
- viral proteins are assembled into more HIV virus particles which replicate further causing the T helper cell to burst and release the HIV particles into the bloodstream to infect more T helper cells
Why does destruction of T helper cells cause AIDS
Lack of T-helper cells reduces cytokine production
Thus reducing activation of B cells
Thus reducing antibody production
Thus increasing the risk of opportunistic infections e.g. TB
Active natural/artificial immunity
Active natural immunity: Specific immune response was triggered due to infection. Memory T and B cells are produced providing immunity to the antigen e.g. gaining immunity to chickenpox
Active artificial immunity: Achieved through vaccination where body is exposed to an inactive form of a pathogen to stimulate an immune response and develop memory cells providing protection if exposed to the antigen in the future.
Passive natural/artificial immunity
Passive natural immunity: acquired when a fetus or infant receives antibodies from its mother - through the placenta during pregnancy (placental transfer) or through breast milk during infancy. Antibodies are short term but breast milk is constantly supplied during infancy so the antibodies are basically renewed
Passive artificial immunity: acquired by receiving pre-formed antibodies from another source rather than the bodies own immune system producing them. Antibodies are shortly broken down and not replaced
E.g. receiving a shot of immunoglobulin (antibodies) when bitten by a rabid animal
This shot of pre-made antibodies is given to immediately fight the rabies virus rather than the body having to produce them on its own.
Explain the role of antigens and antibodies in the body's immune response
2 types of response:
pathogen attacks, macrophage are antigen presenting cells & have CD4 receptors which bind to the pathogen. T-helper cells then bind to the APC and are activated.
- cell mediated
T-helper activates T-killer
T-killer are cytotoxic, bind to antigen presented on infected body cells, perforates membrane and causes cell lysis.
- humoral
T-helper binds to B-cell, releases cytokines
Clonal selection of B-cell (B-memory and plasma cells produced)
Plasma cells secrete antibodies which bind to the antigen, form antigen-antibody complex.
How does TB infect human cells
Macrophages engulf M.TB and form a granuloma (= tubercles + respire anaerobically).
M.TB can survive within macrophages since they have thick waxy walls that are difficult to break down.
It prevents the lysosome from fusing with the phagocytic vacuole
Bacteria lie dormant for years. Weakened immune system = active bacteria.
Non-specific response
1) Inflammation
Histamine is released by damaged WBCs and mast cells. Vasodilation of arterioles occur so increased blood flow to surface of skin. Capillaries = more permeable so plasma can diffuse through walls, forming swelling/oedema. Antibodies leak out.
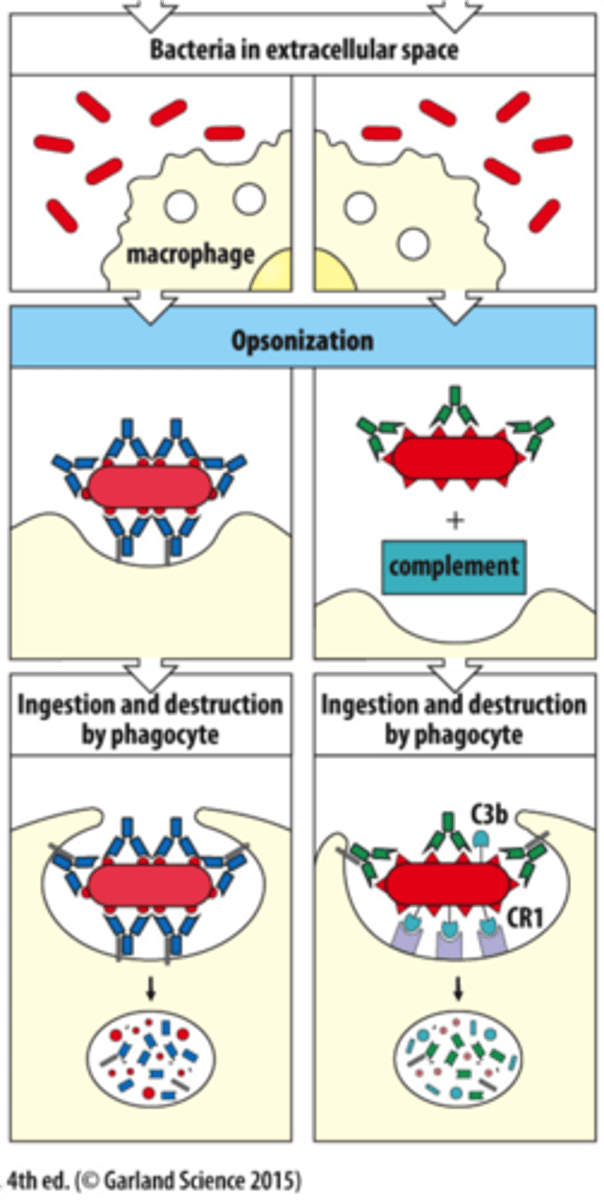
2) Phagocytosis
Bac. release chemicals, and damaged cells at site attract phagocytic WBCs.
- Neutrophils 1st -engulf a few bac. and die, forming pus.
- Macrophages 2nd - larger so engulf more bac.
Ingested material in vacuole of macrophage
Lysosomes fuse with vacuole, exocytosis to release enzymes, breaks down bacteria.
Macrophages present in lymph nodes prevent bacteria from spreading.
Interferon produced by microbe-infected cells. Diffuses to surrounding cells, preventing microbes from multiplying. Inhibits microbial protein synthesis so prevents viral replication.
Specific response
Lymphocytes: T and B cells are responsible for recognising and specific antigens
B cells produce antibodies that neutralise pathogens or target them for destruction
It is slower than a non-specific response and memory cells develop for future infections.
What is an antigen?
a toxin or other foreign substance that triggers an immune response in the body, including the production of antibodies.
MHC proteins
MHC proteins act as markers to distinguish between self and non-self antigens
MHC class I proteins are found on the surface of all nucleated cells in the body. It binds to the antigen in the cell and displays it on the surface. If the cell is infected with a virus or is cancerous it will signal to a T killer cell to destroy the cell
MHC class II proteins are found on antigen presenting cells (APCs) such as macrophages and B cells. T helper cells recognize these MHC II-antigen complexes and activate other immune cells starting a specific immune response against the pathogen
Overall MHC I and II are essential for antigen presentation to T cells
What is an antibody?
Made of glycoprotein, held together by Disulphide bridges. They are present on B-cells. Antibodies bind to antigens for opsonisation, agglutination and neutralisation.
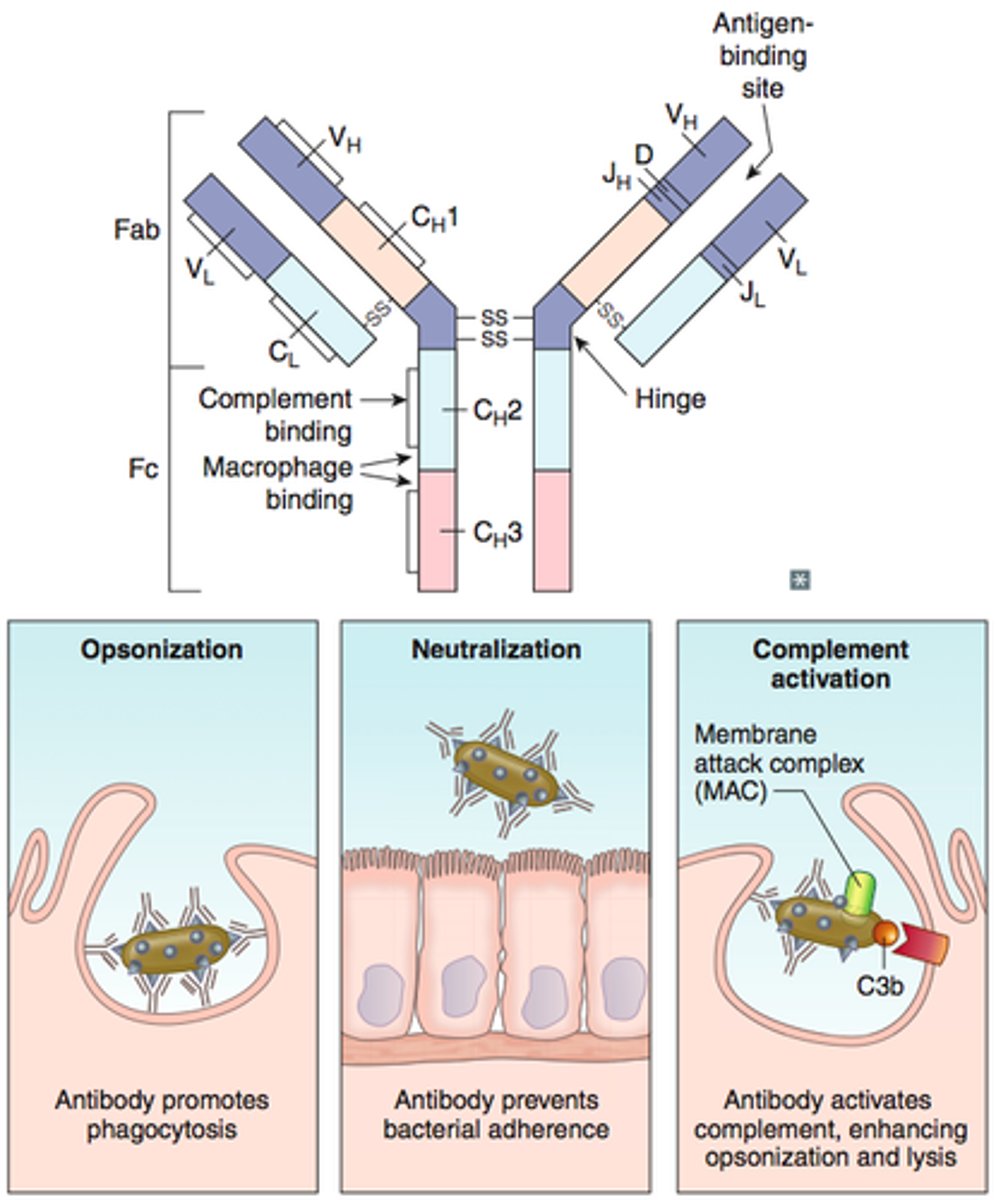
Structure of an antibody
Amino acid sequences in the variable region are different for very antibody
The variable region is where an antibody binds to the antigen
AT the end of the variable region is the antigen binding site
There are 5 classes of mammalian antibodies each class with a different constant region and different roles
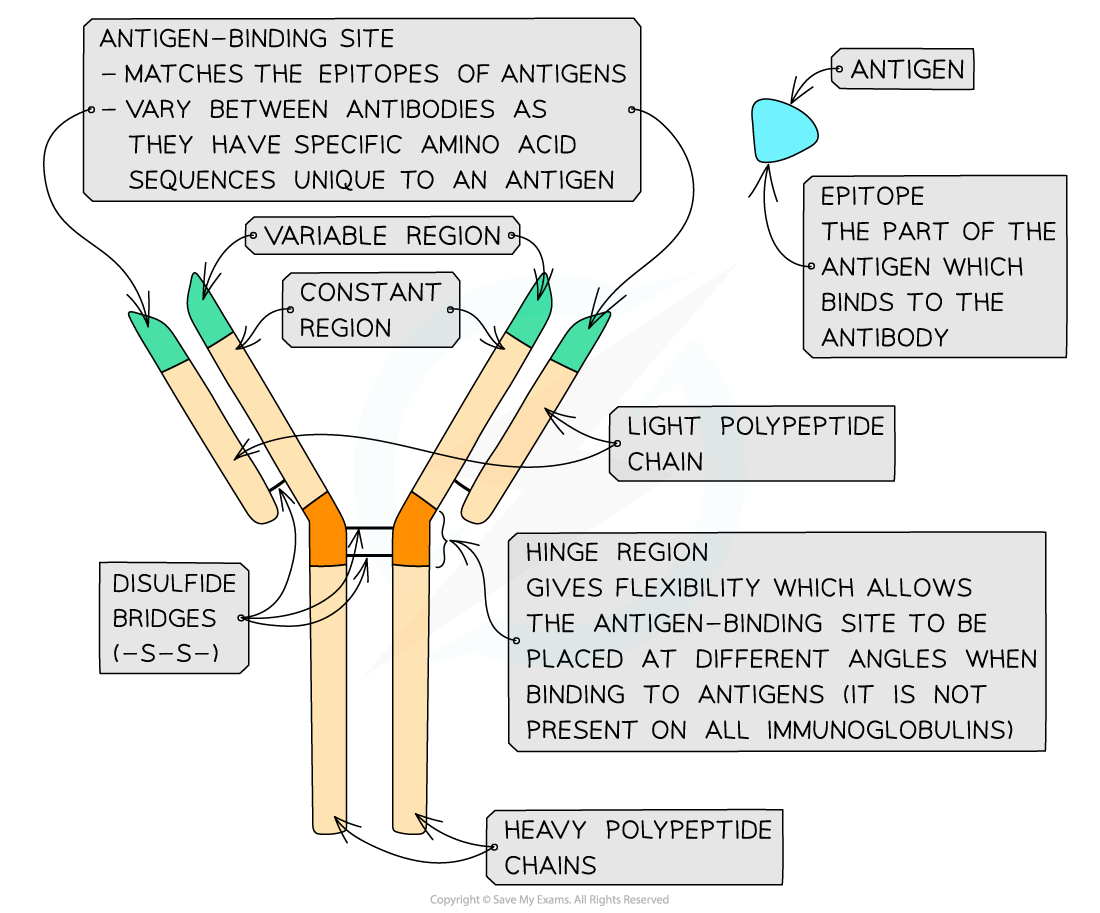
Membrane bound vs NMB antibodies
Membrane-bound antibodies are attached to the surface of lymphocytes
The membrane-bound antibodies have an extra section of polypeptide chain within their heavy chains which forms the attachment to lymphocytes
This extra section of polypeptide is not required in antibodies that are not bound to lymphocytes
The gene which codes for the antibody’s heavy chains can undergo a process called alternative splicing to remove this extra section in non-bound antibodies
Describe how antibodies can help fight infection
Opsonisation: Phagocytes bind more easily to antibodies on pathogen surface, increasing effectiveness of phagocytosis.
Agglutination:
Antibody binds to 2 antigens. Many pathogens bound together, forming an immune complex, so pathogens cannot enter cells.
Neutralisation:
Antibodies bind to pathogen, making path. incapable of attaching to cell.
How does one gene give rise to more than one protein?
This is due to post-transcriptional changes to mRNA.
Exons - contain coding info
Introns - non-coding strands that are removed by splicing (spiceosomes).
pre-mRNA contains both introns and exons.
Exons are spliced together, forming a single coding strand.
Exons can be spliced in different ways, so many different proteins can be formed (i.e. alternative splicing - some non-coding regions skipped altogether.
Alternative splicing vs splicing
Splicing removes non-coding sections (introns) of the pre-mRNA and exons are joined together to form the mature mRNA → this must be done otherwise a non-functioning protein is produced.
Alternative splicing removes coding sections of mRNA (exons)
Inclusion or exclusion of exons can alter the sequence of amino acids in a protein leading to different protein isoforms with possibly different functions
How can pathogens enter the body?
Vectors: organism transmits infection
Inhalation: transmitted by coughing/sneezing (like in TB with droplet nuclei containing MTB)
Food: Exotoxins/endotoxins from bacteria
Inoculation: via break in skin i.e. a wound
Water: i.e. cholera
How is the body able to prevent the entrance of pathogens into the body?
Skin:
keratin/dead skin layer to prevent microorganisms from entering
Blood clots form over cuts in skin, prevents path. from entering
Skin flora: large # of microbes on skin, so prevents colonisation of bac. due to competition. (Keratin in the skin is a physical barrier)
Stomach acid:
HCl = low pH, kills bacteria that enter with food, but still optimum pH for enzymes in body (Chemical barrier)
Gut flora:
Bacteria in gut - secrete lactic acid for defense against pathogens
Flora = competition + benefit from gut
Mucous Membranes:
lack keratin, entry of pathogens limited by ciliated cells, which brush path. away in airways/lungs.
How do vaccinations prevent us from contracting disease?
Stimulates immunity without the disease (non-virulent)
Contains small amount of antigen, stimulates memory cells to develop. Immune system will be able to attack this pathogen since it is altered so that it is harmless.
Why might a vaccine not work on someone?
- defective immunity
- diseases develop before immunity is build
- mutations in the pathogen/variety
How can HIV evade antiviral medication
protein coat constantly changing, so immune cells reduced as they can't target.
High mutation rate in genes for antigen protein so cells cannot recognise so many diff. antigens.
Mycobacterium Tuberculosis
Infects phagocytes in the lungs
Bacteria lie dormant in the tubercles. Not destroyed by the immune system as the tubercles are covered with a thick waxy coat
When the immune system is compromised e.g. the patient develops AIDs, the bacteria become active again
The bacteria slowly destroy the lung tissue, thus leading to breathing problems, coughing, weight loss as well as fevers
TB can then spread to other areas of the body at which stage it can be fatal
How does TB evade antibiotics?
TB have waxy coat on cell walls, protecting them against enzymes in macrophages. This disrupts the antigen presentation by macrophages, so prevents the lysosome from exocytosing.
Bacteriocidal Antibiotics
Kill bacteria
Bacteriostatic Antibiotics
Prevent bacterial from multiplying (host immune system destroys remaining bac)
herd immunity
protection provided to a population when a large percentage of individuals are vaccinated against a specific disease
Making it difficult for the disease to spread to those who have not been vaccinated
T cells and B cells
T helper cells release cytokines that either activate B cells to become plasma cells or cytotoxic T killer cells
T killer cells responsible for directly killing infected or cancerous cells. They recognize and eliminate cells displaying specific antigens, including viral proteins or tumour-associated antigens
B cells differentiate into plasma cells which produce antibodies against a specific antigen. Each B cell produces antibodies with the same unique antigen binding site for a specific antigen
T and B memory cells remain in the bloodstream after the infection has cleared and provide long-term protection against the specific antigen
When would T helper cells activate B cells over T killer cells
Usually when the immune response is directed against an extracellular pathogen, B cells are activated
When the immune system needs to eliminate intracellular pathogens or infected cells T killer cells are activated.
Intracellular pathogens grow and reproduce inside a host cell