Biomechanics/Intro Name what is going on by theName what is going on by the
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
Name what is going on by the
distal segment on the proximal segment
Big four
squat, lunge, plank, single limb stance
Hip ADD/ABD OKC
Relationship of the distal segment relative to the midline of the proximal segment
Frontal plane motion around sagittal axis
hip rotation
IR/ER
Hip ADD/AB CKC
Add= CL pelvic drop
Weak glute med
Ab= Cl pelvic rise
QL activity
Tib ab/ad
Ab= valgus
Ad= varus
Lean towards stance limb
if you have a weak glute med also decrease compressive forces
Hit and go inward at the knees = unloading the knee-pain response
With OA the compensations will not exactly line up with the pain
Acetabulum positioned
Positioned laterally with inferior and anterior tilt
Provides over coverage
Periphery is covered by
hyaline cartilage
Hyaline cartilage is strong- smooth
In acetabulum and the femur
deepened by
fibrocartilaginous labrum
Also supported by ligaments and capsule too
Orientation- frontal plane
Center edge angle / center edge angle of Wilberg
Center edge angle / center edge angle of Wilberg
Amount of acetabulum that covers the femur
Highly variable
Average 35 deg in adults
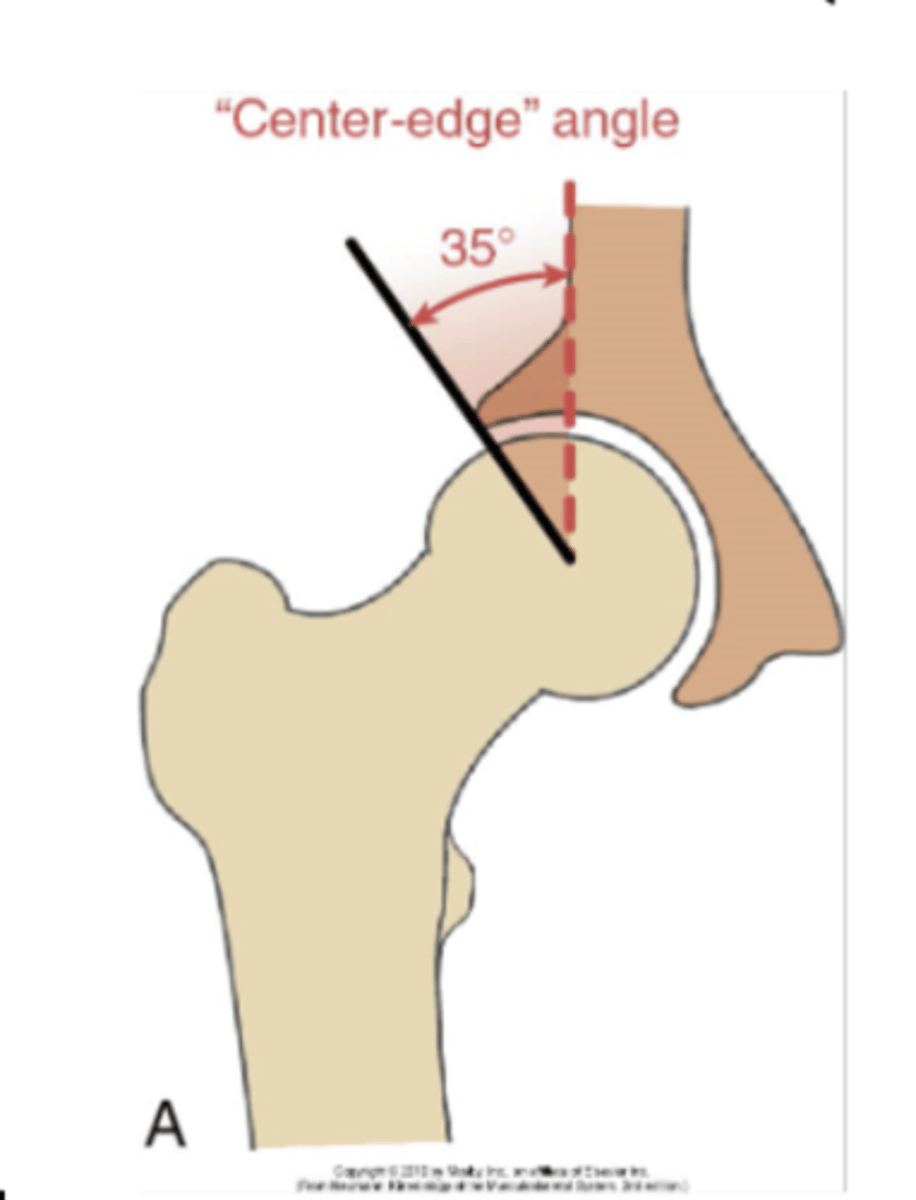
inc/dec wiberg
Inc angle = less mobility, joint loading
Dec angle= less and unstable coverage
Over coverage - hip impingement
Under coverage - hip instability or hip dysplasia
Orientation- horizontal transverse plane
Acetabular anteversion angle
Acetabular anteversion angle
Orientation of the acetabulum within the horizontal plane in relation to the pelvis
Extent which acetabulum projects anteriorly in horizontal plane
Average 20 deg
Males 18.5
Females- 21.5
inc dec Acetabular anteversion angle
Increased angle = less coverage of the femoral head
Inc ER, Dec coverage, Dec stability
Dec ante-version angle= inc coverage and inc stability
Aka could be retroverted
Femur- Fovea capitus by way of ligamentum teres supplies blood
But this is only in childhood
As we age its taken over my medial and lateral circumflex arteries which are branches off femoral artery
femur characteristics
Largest and strongest bone in the body
Head of femur is covered by hyaline cartilage (2/3)
hip capsule
Irregular dense fibrous structure
Attached to periphery of acetabulum to base of femoral neck
Thickened anterior superiorly
Supported by ligaments
Hip labrum
Deepens socket and increase concavity of acetabulum
Maintain negative intraarticular pressure
Nerve endings provide proprioceptive as well as nociceptive feedback
Very innervated decent blood flow
Free nerve endings and nociceptive so can produce pain
Tears can decrease the stability of the joint
illiofemoral
Y= supports hip anterior
Resist extension, IR, and some ER
pubofemoral
resist abduction, ER
Loose during flexion - can be taut on extension
ischiofemoral
Resist extension
Ankle of inclination
Kids have higher angles
125 is normal angle of inclination
What causes the shift- starting to load the limb- gravity pull of muscles ect.
coxa vara
Inc moment arm for hip abducotrs
Alignment may improve joint stability
more bending force higher risk of fractures , inc shear force on femoral neck
Dec functional length of hip abductors
This is more stable compared to valga
Angle less then 105
coxa valga
Lots of point contact in a smaller area
Dec bending moment arm- Dec benign movement - Dec hear force on femoral neck
Angle over 140
Alignment may favor dislocation
Adductor moment worse - abductors shorter length and may not have to work as hard
Abductors dec moment arm
Dec shear force - less fractures
Alignment may favor dislocations
Inc functional length of hip abductor muscles
closed packed hip
max hip extension, medial IR, abduction
Max congruency is actually frog like butterfly position
Reason doesn't follow is the angle of the acetabulum
capsular pattern
IR>Ext>Abd>flex>ER
Ext is first thing a pt notices
Congenital hip dysplasia
Abnormal contact of the hip in utero
More shallow acetabulum
Lower center angle on imaging
Developmental dysplasia of the hip - DDH
No known etiology
Familial link
Bilateral - can be unilateral but may not get picked up until child starts to walk
Usually first born children
More prevalent in females
breech
More creases on limbs- one leg lower then the other
Different leg lengths
Ligaments that maintain head are lax
Femoral head can sublux or dislocate
1-2 cases per 1000 births
Physicians screen for this after birth
degrees for possible dysplastic
16 deg or less of Wiberg angle is dysplastic
16-25 is possible dysplastic
How's it diagnosed
Asymmetry limb and skin folds
Infant = ortolanis sign / Barlow test
Diagnosed in older children - walking is usually delayed, once walking abnormal gait (limp, waddling)
barlow
flex femur and push down while adducting
Sublux
ortolani
opposite and then this reduces it
Treatment birth to 6 months
Dislocation reduced and the hip then maintained in a Flexion, abduction , ER (frog leg), with harness or spica casted
90% success if discovered within 6 weeks of birth
treatment up to 3
will attempt conservative treatment, will attempt to utilize traction and progression of abduction to try and reshape acetabulum
Often times will result in a closed reduction
4-8 years old
Reduction done surgically
Periacetabular osteotomy
Breaking femur and pelvis and rotating them to allow more coverage of the joint
Very significant procedure - 6 month rehab
Showing promising result if done earlier - before they are skeletally mature
Good to get back ADLs not really to be athlet
Don't exactly know the long-term effects
The short term outcomes are promising
Slipped capital femoral epiphysis (SCFE)
Older child
Early adolescents with rapid growth
Female= 10-13 y/o
Male= 12-16 y/o
2-10/100,000 adolescents
risks scfe
Males higher risk - 60-65%
Obesity
Coxa vara due to high shear forces
Head slips off posterior
Grade it by how much is posterior or how much has slipped off
S&S Scfe
poorly localized pain over the thigh, groin, knee (often medial knee pain may by only symptom)
Intermittent limb
LE goes into ER in supine and with hip flexion
Ortho red flags is that excessive ER
Gradual onset
Pain and stiffness over time
Referred pain into the knee - aka medial knee pain
Could have some gluteal pain
No MOI- based over time - body habits and inclination angle can push femoral head
consequences scfe
growth plate wont heal, avascular necrosis (impacts the medial and lateral circumflex arteries)
treatment scfe
percutaneous pinning- screw going through neck into the head - does not rotate not it all can move as one thing liek its supposed to
Early diagnosis allows greater chance for successful stabilization
Femoral torsion
Twist between the neck of the femur and the shaft
Estimated in infants to be 30-40 deg
Angel decreases 1.5 deg per year
Normal - 10 to 20 deg
Male=15
Female=18
Femoral anteversion -
angles greater than 15-20
Inc IR greater then ER they have more space to do that
If they IR they can compensate and line the dots up- compensation only occurs at eh hip
If you toe in- you can compensate at the hip but its not compensated at the tibia
Femoral retroversion
angles are less then 15-20
Just less in the anterior direction
Femoral torsion test
craig test
Males = 8-12 deg
Females= 12-18 deg
Q angle
Males= 12, females=15
Angle of the pull of the quad
ASIS to center patella to the tibial tuberosity
Why patellar femoral pain syndrome is more in females then males
Compensation at hip with IR and tibia stays same - more of the increases the q angle
Results excess anteversion
Internally rotated toeing in gait- pigeon toed
Tibial ER to get toes straight
Foot might be a little more pronated
Medial long arch job to be stable and is a mobile adapter and will follow the IR and pronate more
Appearance of genu valgus
Increased lumbar lordosis- due to the inc anterior tilt of the pelvis
Causes inc anteversion
W sitting position
Weight of body turning into that position
Toe in= inc anteversion
toe out
Toe out= dec anteversion or retroversion
The hip is always going to be compensated, uncompensated usually talking about femur and tibia
Results of excess retroversion
If they don't compensate of the tibia= bow legged appearance more valgus
Tibial torsions
Twist in tibial bones themselves
Leg calve perthes disease (LCP)
Flattening of the femoral head
Positioning but also damage to blood flow
Idiopathic
Ages 4-10
Very active
Small for age
Osteonecrosis of the femoral head
Leads to flattening of the femoral head
Usually unilateral: 10-12% bilateral
1 in 12,000 children
LCP causes
trauma, inflammation of the capsule or synovitis, dec blood flow
LCP symptoms
limping slight dragging of leg
Limited hip Abd and IR
Due to adductor spasms
Feel very tonic compared to the uneffected side
Pain in groin, thigh, medial knee
Treatment LCP
Prevent lasting deformity of the femoral head and keeping the femoral head in the acetabulum
Restrict activities
ROM and strengthening exercises
Dec WB- crutches/walker
Usually, WBAT
Early diagnosis = femoral head has potential to remodel if caught early enough