BMS 124: Calcium/Phosphate Metabolism
1/108
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
109 Terms
Calcium
Mineralized tissue (hydroxyapatite in dentin, bone, enamel and cementum)
Hydroxyapetite
Ca10(PO4)6(OH)2; the form of apatite that is the principal mineral component of teeth, bones, and calculus.
Blood clot formation, cell-cell adhesion, intracellular signaling pathway
What are other calcium functions in the body
Cadherin
A calcium-dependent adherence protein, important in the adhesion of cells to other cells.
Phosphate
Component of phosphorylated metabolites (ATP, UDP glucose, glucose 6 phosphate, creating phosphate etc)
DNA/RNA
Phosphate is found in nucleotides including
Phospholipids
Phosphate is found in ____ in cell membranes
Phosphoenzymes
Phosphate can be found in signaling pathways called ______ like receptor tyrosine kinase
99%
About ___ percent of calcium is located in mineralized tissue
Plasma
The remaining 1% of calcium is found in intracellular and extracellular fluid specifically in the ___
85%
About ___ percent of phosphate is mineralized tissue
Intracellular
Remaining phosphate is ______
700 mg
RDA for phosphate
Hydroxyapatite
A calcium and phosphate salt
Lowest
At pH 7, the calcium phosphate solid with the ______ solubility is hydroxyapetite which means the crystal is very stable
Systemic balance
Ca and P ____ directly impacts oral health, disease and treatment success
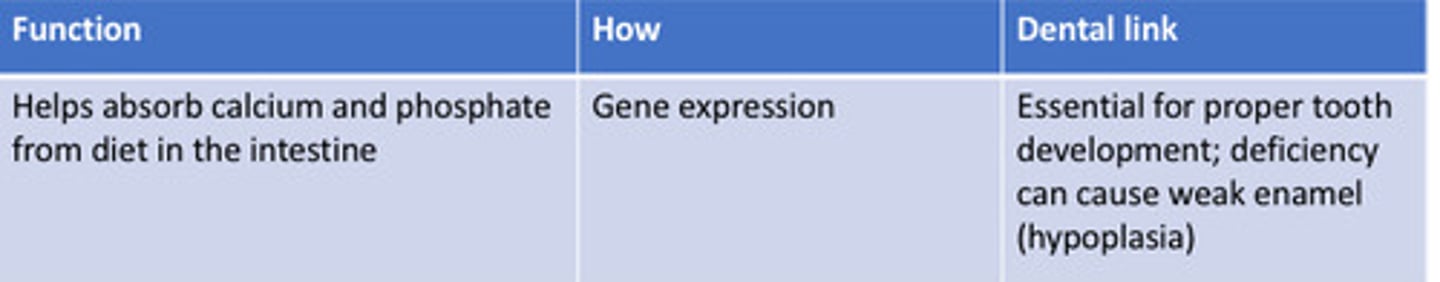
Vitamin D
Is crucial for absorbing Ca and P
Tooth development
A child with vitamin D deficiency can have less _____ and higher susceptibility to caries
Bone metabolism
Adults with vitamin D deficiency have bad ______ and can have periodontal disease progression
Enamel
hard, outermost layer of a tooth, hardest substance in body, is almost entirely hydroxyapetite
Enamel, dentin, cementum, alveolar bone
What structures have hydroxyapatite as a primary structural component
Dentin
Primary material found in teeth. It is covered by the enamel in the crown and a protective layer of cementum in the root.
Cementum
Specialized, calcified connective tissue that covers the anatomic root of a tooth.
Alveolar bone
bone that supports and encases the roots of teeth
Intestine
Absorbs calcium and P
Bone
Stores calcium and P
Kidney
Excretes calcium and P
Tight junction, concentration gradient
1) calcium passes through ___ formed by claudin proteins between epithelial cells through ____
Lumen, enterocytes
2.1) Calcium ions (Ca 2+ ) from the intestinal _____ (inside the gut) enter the intestinal epithelial cells (_____) through TRPV6.
Calbindin D9K
2.2) Once inside the enterocyte, calcium binds to a cytosolic calcium-binding protein called _______. This protein acts like a shuttle, safely transporting calcium across the cell's cytoplasm without causing harmful buildup of free calcium.
PMCA1, NCX1
2.3) Calcium is then actively pumped out of the enterocyte to the bloodstream by the plasma membrane Ca2+-ATPase (______) and, to a lesser extent, the sodium-calcium exchanger (_____).
Endocytosis, exocytosis
Calcium could also be transported by
Vitamin D
All of the pathways of calcium is regulated by
VDR, upregulate
The active form of vitamin D, 1,25(OH)2D could bind to ____ (vitaminD3 receptor) and ________ the gene expression of proteins in the three pathways, including TRPV6, calbindin D9k, Claudin2,12,15, PMCA1, NCX1
Diffusion, NTB2b carrier, PIT1/PIT2 carriers
What are the three pathways of phosphate intestinal absorption
Vitamin D, phosphate
In intestinal absorption of phosphate, NPT2b carrier is regulated by _____ and dietary ___ level
Not
In intestinal absorption of phosphate, PIT1/PIT2 carries are ____ regulated
Kidney
Both Ca and Pi are filtered from the blood and then reabsorbed in the ____ (majority are reasoned)
Transporters, Carrier protein, ion channels
In reabsorption, Some ____ or ___ or ____ in the process are also regulated by PTH.
PTH (parathyroid hormone)
Transporter/carrier/channel reabsorption of calcium/phosphate is regulated by
Demineralizing, increase
In bone resorption, Ca Pi resorption is ______ process, which releases Ca and Pi from mineralized tissue (hydroxyapatite) into blood stream and ____ Ca and Pi level in the blood.
Remineralization, decreases
Ca Pi deposition is ______ process, which forms hydroxyapatite in mineralized tissue and _____ Ca and Pi level in the blood.
Deposition
We still use bone remodeling as an example to explain Ca and Pi ______ process.
Osteoprotegerin, prevents,
To keep bone resorption under control, the osteoblasts also secrete _____, which binds to RANKL and ______ it from activating RANK receptors.
Slows
Osteoprotegerin, which binds to RANKL and prevents it from activating RANK receptors. This ____ down the activation of osteoclasts.
Osteoid seam
Following bone resorption, osteoblasts start secreting _____, a substance mainly made of collagen, to fill in the lacunae created by the osteoclasts.
Hydroxyapatite
Calcium and phosphate begin to deposit on the seam, forming ____.
Deposition, remineralization
In the _______ process, Ca and Pi in blood go down and form hydroxyapatite.
Inactive
We could get vitaminD2 or D3 which are the _____ form of vitamin D from our diets.
Skin, sun
Our _____ could produce 7-dehydro-cholesterol and with ____ becomes pre vitamin D3
Liver
The vitamin D will be absorbed into the blood and carried to the
Kidney
In the liver, it will be changed to 25-OH-D with 25-hydroxylase. Then it will be carried to the _____
kidney
In the _____, it will be modified to the active form 1,25-dihydroxycholecalciferol (1,25-DHCC).
VDR
After calcium becomes active from the kidney (1,25-DHCC), it will go in the circulation to bind the _____ and have its biological activities.
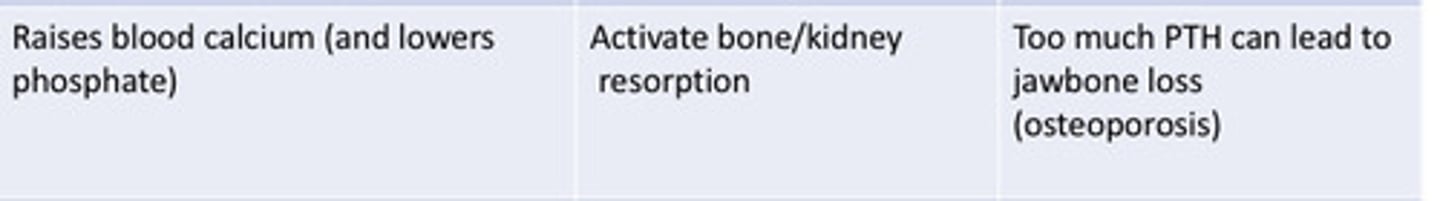
PTH (parathyroid hormone)
___ could upregulate 1alpha-hydroxylase, therefore, increase 1,25-DHCC level in the kidney
Plasma, surface
PTH secretion is sensitive to ____ calcium level. It is because the calcium-sensing receptor which is located on the parathyroid cell ___.
G protein, phospholipase C (PLC)
This calcium-sensing receptor is a ____ receptor and it activates ___ pathway.
ER
When the extracellular Ca level is normal or high, calcium binds to the receptor which activate PLC signaling pathway and then release calcium from ___.
inhibits
Increased intracellular Ca2+ level ___ PTH released from the cells.
less, ER
When the calcium level is high, ___ extracellular calcium binds to the receptor, which means calcium remains in the _____
Released
When calcium levels are low, secretory granules bind to the cell membrane and PTH gets ______!
Parathyroid gland
___ could sense the extracellular calcium level by their surface membrane protein (calcium-sensing receptor).
low
When calcium level is __, PTH gets released.
Increased bone resorption
PTH released will release calcium into the plasma called
Increase kidney reabsorption
PTH released will _____ so less calcium is excreted in the urine and more stay in plasma
Increase production of 1,25-(OH)2D
PTH released will ____ which will increase intestinal absorption of calcium and also increase bone resorption
inhibited
When plasma calcium level is too high, PTH release will be ____. Everything reverses. So lower the plasma calcium level.
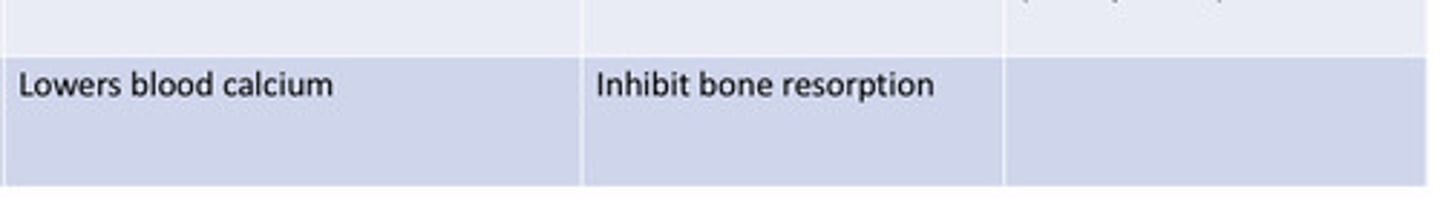
calcitonin
Parathyroid hormone and vitamin D help increase calcium levels, whereas ___ helps lower them.
parafollicular cells
Calcitonin comes from the ____, or C cells.
above, lowering
If the concentration of calcium in the blood goes _____ the normal range, C cells release calcitonin, _____ blood calcium levels.
Osteoclasts
In the bones, calcitonin binds to the ____ and lowers bone resorption
Decreases
In the kidneys, calcitonin _____ Ca/P reabsorption
Vitamin D
PTH
Calcitonin
decrease
Injury, infection, stress-induced hormones (glucocorticoids), parathyroid hormone, and increased pressure on a bone all _______ osteoprotegerin (OCIF) production by osteoblasts, causing greater differentiation of osteoclasts, more bone remodeling, and more demineralization
PTH, Glucocorticoid
What hormonal factors promote bone resorption
Growth hormones, estrogen/testosterone
What hormonal factors promote remineralization
Vitamin D, Ca/P
What nutritional factor promote remineralization
Pressure on bone, immobilization, sedentary lifestyle
What mechanical factors promote bone resorption
Tension on bone, weight bearing exercise
What mechanical factors promote bone remineralization
Inflammation, acidosis
What medical conditions promote bone resorption
Cytokines
____ associated with the repair of tissues after injury or infection, specifically IL-4 and IL13, inhibit mechanisms that stimulate osteoclast differentiation and bone resorption.
Increase, few
Conversely, growth, anabolic and sex hormones, and tension on the bone, all _____ OCIF production by osteoblasts. ____ osteoclasts develop and bone resorption is decreased.
Orthodontic tooth movement
Applying of orthodontic force to the tooth compresses the PDL.
compression
At the ______ side of the tooth, which appears in the direction of the orthodontic force, bone resorption takes place, carried out mainly by osteoclasts.
Tension
At the _____ side, osteoblasts are responsible for the bone formation process.
True
T/F: vitamin D regulates Ca and P levels in blood
Rickets
refers to insufficient mineralization of osteoid at the growth plate, accompanied by an alteration in the growth plate structure. It manifests clinically as skeletal deformation.
osteoid
Rickets is an insufficient mineralization of _____ at the growth plate, accompanied by an alteration in the growth plate structure. It manifests clinically as skeletal deformation.
vitamin D
____ deficiency is the most common cause of Rickets because it leads to low 1,25-DHCC
1,25-DHCC
active form of vitamin D
1,25-DHCC
Vitamin D deficiency will lower ______ which will cause defects in enamel, dentin, and cementum (rickets)
mineralize
In rickets, Osteoclast activity is normal but the bone does not properly _____.
Supplements
Rickets is treated by vitamin D or phosphate _____, depending on the deficiency.
Osteomalacia
Another name for rickets is
Osteoporosis
Trabecular (spongy) and cortical bone lose mass and interconnections despite normal bone mineralization and lab values (serum (Ca2+ and PO43-).
Increase, decrease
Osteoporosis Most commonly due to ______ bone resorption related to ______ estrogen levels and old age.
menopause
In osteoporosis that occurs at ______, osteoclast activity is over-active and osteoblast activity is reduced.
Bisphosphonates
Treatment of osteoporosis is with ________