Pathology of Bone Marrow
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
What are the two types of hematopoietic neoplasia?
Myeloproliferative disorders
Lymphoproliferative disorders
How to differentiate between the two types of hematopoietic neoplasia
Myeloproliferative disorders
neoplastic proliferation of non-lymphoid blood cells (erythrocytes, granulocytes, monocytes, megakaryocytes)
neoplasia typically originates in bone marrow as these cells are produced in the bone marrow
lymphoproliferative disorders
neoplastic proliferation of lymphoid cells
lymphocyte development occurs mainly outside of bone marrow → neoplasia originates both in bone marrow & outside of bone marrow
Classify the types of leukemia based on cell lineage & disease progression
Myeloid progenitor
Neutrophils, monocytes, eosinophils, basophils
Dysplastic neutrophils/early myeloid precursors indicates myeloid neoplasia
Lymphoid progenitor
dysplastic lymphocytes & plasma cells indicates lymphoid neoplasia
What are the common CBC changes associated with leukemia? Why do these changes occur?
Differentiate between the two main causes of lymphoid leukemia
Compare the prognoses of the two main causes of lymphoid leukemia using blood smear images
Distinguish between lymphoma & lymphoid leukemia based on clinical & pathological features
List the 4 key diagnostic features of plasma cell myeloma & apply them to make a diagnosis
Define myeloproliferative disease & discuss its incidence & clinical reference
What are two most common causes of non-regenerative anemia in domestic animals
anemia of chronic disease/inflammation
Anemia due to chronic kidney disease
what are diagnostic techniques for cell lineage confirmation?
morphology assessment
Bone marrow aspiration & cytology
Peripheral blood smears → insufficient for Ddx alone
cytochemical staining
Determines if leukemic cells originate from myeloid lineage (myeloid & lymphoid look similar at very young stages)
immunophenotyping (flow cytometry or immunohistochemistry)
Useful for lymphoid cells
PCR for clonality (PARR)
Detects clonality in lymphoid populations
genetic & molecular testing
Classification of leukemias
acute leukemia
Aggressive cancers that involve proliferation of immature blast cells
Blast cells = medium to large round blue cells
Rapid & severe course
Progression = days-weeks if left untreated
Chronic leukemia
Proliferation of more mature cells that resemble normal, differentiated blood cells that can often be identified based on morphology alone
Progression = months-years
Some animals may be asymptomatic at diagnosis, may be found incidentally during routine blood testing
What is the most common chronic leukemia encountered in vet med?
chronic lymphocytic leukemia
Leukemic leukemia
marked increase in circulating neoplastic cells (high nucleated cell count)
Subleukemic leukemia
small numbers of malignant cells in circulation (normal or mildly increased nucleated cell count)
Aleukemic leukemia
no malignant cells detected in peripheral blood, diagnosis relies on bone marrow evaluation
What is the definition of leukemia?
cancer of circulating or bone marrow resident hematopoietic cells
Involves malignant hematopoietic cells found in the blood or bone marrow
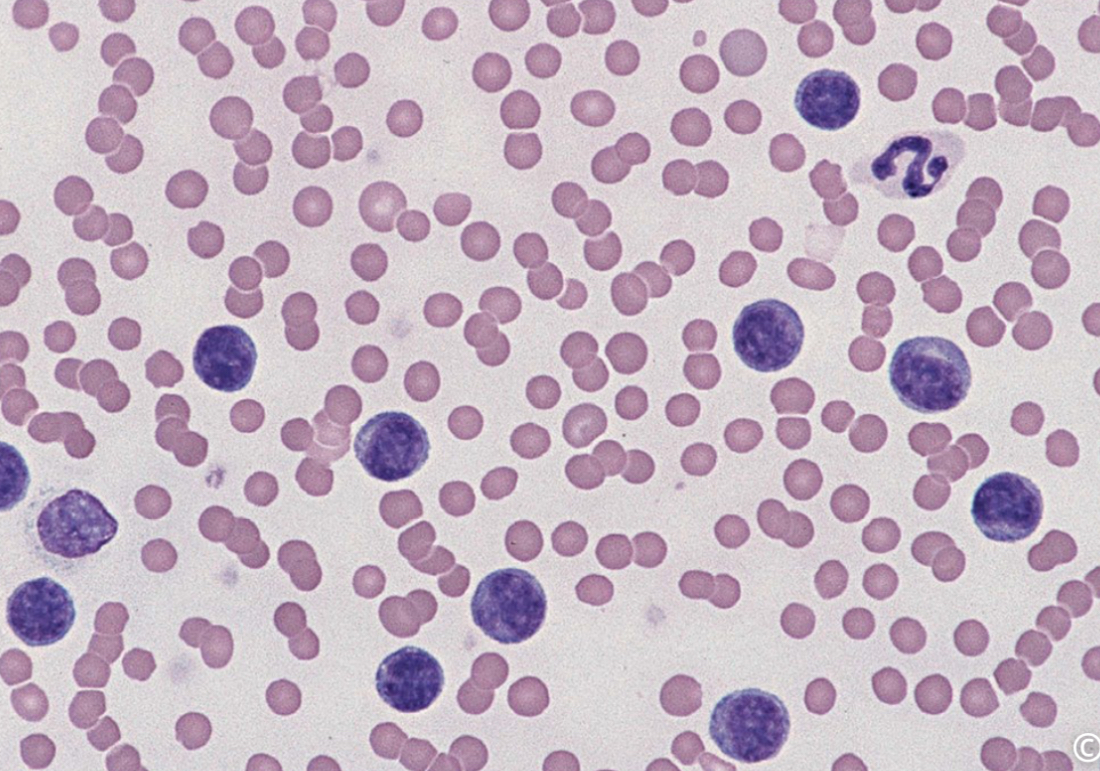
Based on the predominant cell type seen in the image, would you suspect a myeloid or lymphoid neoplasm?
Lymphoid neoplasm
predominance of small, mature lymphocytes
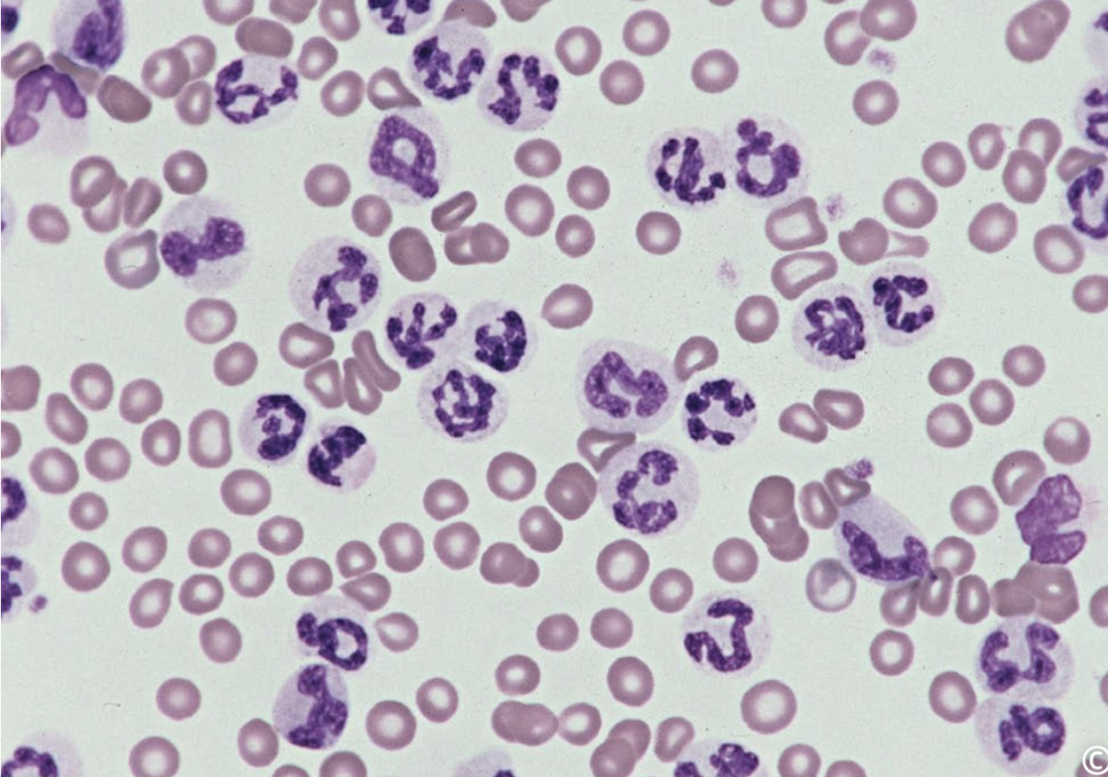
Based on the predominant cell type seen in the image, would you suspect a myeloid or lymphoid neoplasm?
myeloid in origin due to predominance of numerous segmented neutrophils
chronic granulocytic leukemia
In acute leukemia, what would be expected cell maturity, cell appearance on blood smear, speed of clinical progression, & likely outcome if untreated?
Cell maturity - immature blasts cells
Cell appearance on blood smear - medium to large round cells, hard to identify lineage
Speed of clinical progression - rapid (days to weeks)
Likely outcome if left untreated - often fatal within weeks
In chronic leukemia, what would be expected cell maturity, cell appearance on blood smear, speed of clinical progression, & likely outcome if untreated?
Cell maturity - more mature, differentiated cells
Cell appearance on blood smear - smaller cells with more identifiable features (looks more like a lymphocyte or neutrophi)l
Speed of clinical progression - slower (months to years)
Likely outcome if left untreated - may remain stable for months-years, but progress to more significant disease
Are lymphoid or myeloid neoplasms more common in domestic species?
lymphoid
what are the different disorders of lymphoid neoplasms?
lymphoma - forms solid tumors in organs (lymph nodes, spleen)
Lymphoid leukemia - involves bone marrow, often spills over into blood
Plasma cell neoplasia - multiple myeloma or plasmacytomas, arise from antibody-producing plasma cells
Where does primary lymphoid leukemia originate?
in the bone marrow
what are the two classifications of lymphoid leukemia?
acute lymphoblastic leukemia
Large, immature lymphoblasts
Chronic lymphocytic leukemia
Small, mature lymphocytes
CBC changes that can occur with acute lymphoblastic leukemia (ALL)
lymphocytosis with immature cells
Anemia
Marked thrombocytopenia
Blood smear - Large, immature lymphoblasts
prognosis of ALL
poor - limited survival time
Chemotherapy may induce temporary remission but is usually short lived
CBC findings of chronic lymphocytic leukemia (CLL)
Blood smear - small, well-differentiated lymphocytes
Marked lymphocytosis
Moderate anemia, moderate thrombocytopenia
Prognosis of CLL
better than ALL
treated dogs must have an MST (median survival time) of 1-3 years
Treated cats must have MST of approximately 450 days
What would you expect to see in CBC for a dog diagnosed with advanced hematopoietic neoplasia? (WBC, RBC, Platelets)
WBC
variable depending on the disease stage
Early stages = WBC may be increased
Advanced myelophthisis = leukopenia
RBC
Decreased (non-regenerative anemia)
Replacement of normal narrow with neoplastic tissue prevents normal RBC production = non-regenerative anemia
Platelets
Decreased (thrombocytopenia)
Platelet producing megakaryocytes are affected by bone marrow replacement = reduced platelet count, increased bleeding risk
What blood cell line would be affected first & which order would the impact occur
WBC (shortest lifespan)
Platelets (slightly longer lifespan = 5-10 days)
RBCs (longest lifespan, weeks)
4 key diagnostic features of plasma cell myeloma
Radiographic evidence of osteopathic bone lesions
Neoplastic plasma cells in bone marrow
Monoclonal gammopathy → sharp spike in gamma region of serum protein electrophoretogram - represents excess production of single immunoglobulin class
Bence-jones proteinuria → free immunoglobulin light chains may be filtered into urine & detected by urine protein electrophoresis
What is plasma cell myeloma & what does it commonly arise from?
malignant neoplasm of plasma cells
Commonly arises in bone activity involved in hematopoiesis (especially vertebrae, ribs, pelvis, & femur) → leads to multiple osteopathic lesions
other associated clinical features & lab abnormalities of plasma cell myeloma
hyperglobulinemia → rouleaux formation, increased TP, interference with blood cross matching
Hyperviscosity syndrome → cases with excessive IgM or IgA, may impair platelet function & clotting → bleeding tendency
Myelophthisis → non regenerative anemia, granulocytopenia, thrombocytopenia
Hypercalcemia → bone resorption due to osteolysis
Cutaneous plasmacytoma
solitary, well-circumscribed dermal or SQ mass located in digits, head, limbs
Usually benign, have a good prognosis
What is myeloproliferative disease?
rare, non-lymphoid blood cancers originating from the colonial proliferation of stem cells in the bone marrow
Affect various myeloid cell lines (granulocytes, monocytes, erythroid cells, megakaryocytes)
Proliferation often extends beyond bone marrow to spleen, liver, & sometimes lymph nodes
what species is MPD most commonly seen in
cats but uncommon in animals
Accurate diagnosis of MPD
unexplained leukocytosis or blast type cells on CBC
Bone marrow aspirate, cytochemistry, immunophenotyping or molecular diagnositcs
Challenging to diagnose due to vague & non specific clinical signs