Lens
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
Cystoid macular edema
Seen six to ten weeks post complicated cataract surgery
Will appear cystic on OCT
Treatment: topical NSAID and steroid
Anterior capsular fibrosis and contraction
Only seen when capsulorhexis is performed
Risk factors: small capsulorhexis and pseudoexfoliation
Treatment: anterior capsulotomy with Nd:YAG
Dysphotopsia
Patients will report dark shadows in temporal periphery, scintillations, halos and central or peripheral flashes
1st 6-10 weeks
Common with multifocal IOL
Treatment: none
Pseudophakia bullous keratopathy
Commonly seen in patients with compromised endothelium prior to cataract surgery
Also seen in complicated cataract surgery, prolonged surgery or intraoperative endothelial trauma
ptosis
malposition of IOL
edema
Rhegmatogenous retinal detachment
post op complication of phacoemulsification
Risk factors include lattice degeneration, retinal breaks, high myopia and vitreal loss during surgery
Refractive “surprise”
post op complication of phacoemulsification
Post operative refractive error does not match pre operative refractive error calculation
Congenital cataracts
lenticular opacities present at birth
Highest prevalence in Asia
May have unilateral or bilateral presentation
Symptoms: infants are unable to express symptoms, parents will present their concerns
Leukocoria (white pupil)
Nystagmus
Strabismus
4 causes: genetic (50%, mostly AD), chromosomal abnormalities, metabolic disorders, intrauterine infections
4 categories: zonular, polar, total/mature, membranous

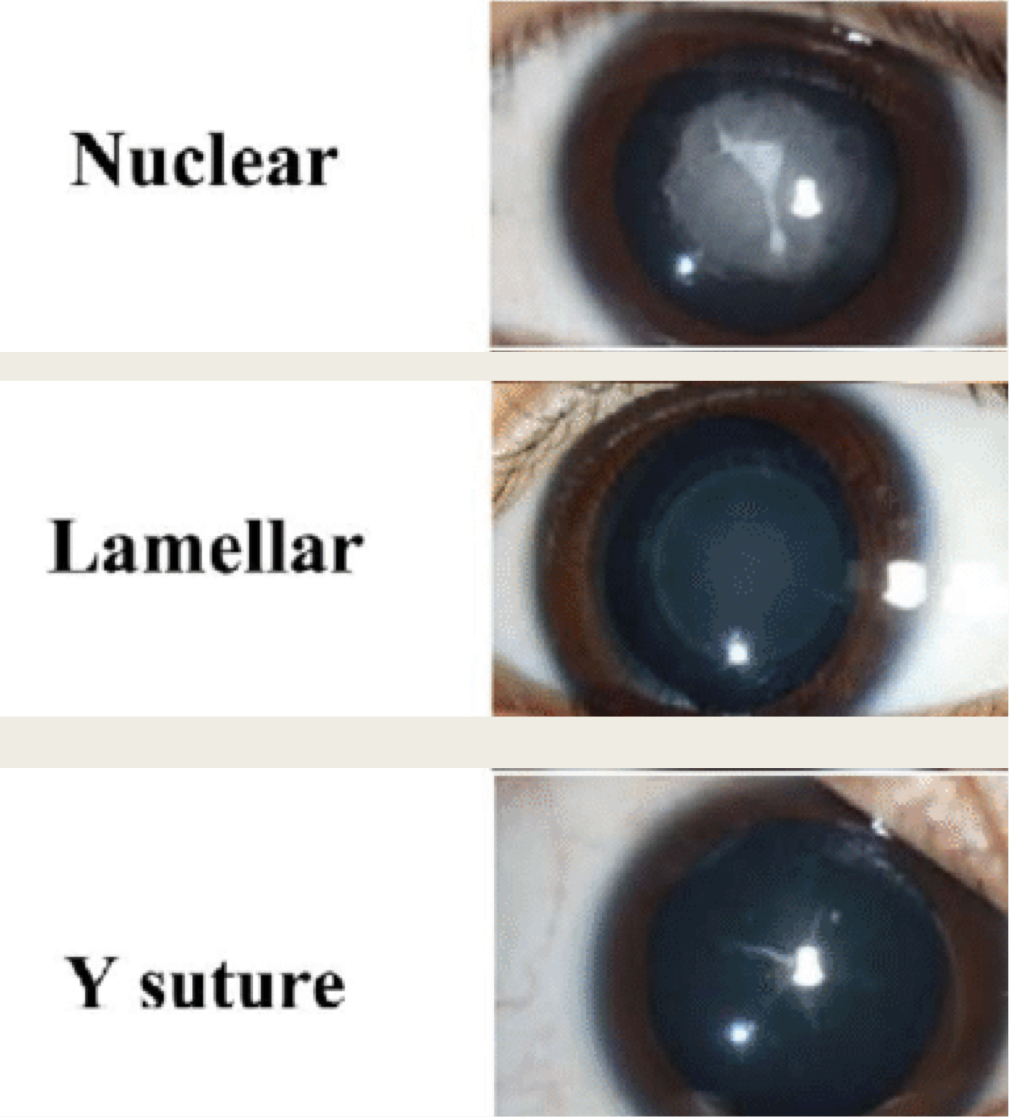
Zonular congenital cataracts
affect one zone of lens
Nuclear: opacities are confined to the embryonic or the fetal nucleus
dense or fine dust-like
dense significantly dec. acuity
tend to be 3mm in size
bilateral
assoc. w/ microcornea
inc risk of developing glaucoma after cataract removal
Cortical lamellar opacities: most common
discrete and round shape
Will affect one or more of the rings in the developing cortex
Nucleus will be relatively clear
5 mm or larger in diameter
Radial extensions or riders
Affect on vision is variable
Sutural: lenticular opacity following anterior or posterior Y suture
slow progression
minimum affect on VA
Cerulean (blue dot):
Numerous small blue opacities in cortex and nucleus
typically non-progressive
minimum affect on VA
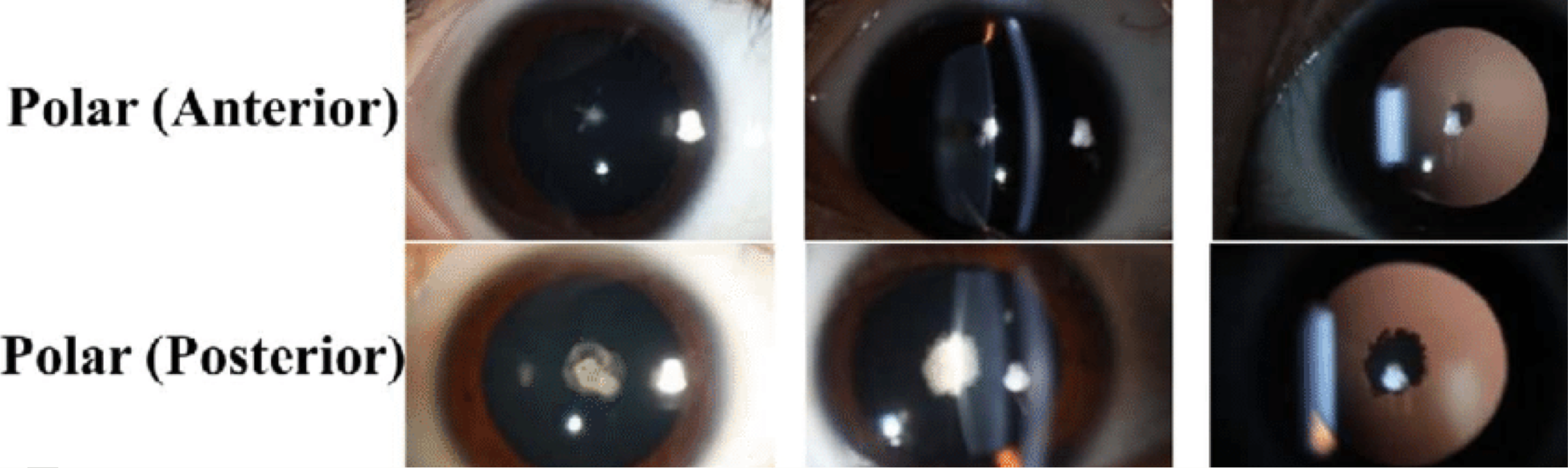
Polar cataracts (congenital)
Anterior polar: small white lenticular opacity of the anterior capsule
May have an associated underlying cortical opacity that is slightly larger than the capsular opacity
can project into anterior chamber
most don’t affect vision
pts do tend to have assoc. hyperopic anisometropia = amblyopia risk
Posterior polar: opacity of the posterior capsule
arise from the end of the hyaloid artery remnant
bilateral
glare and halos
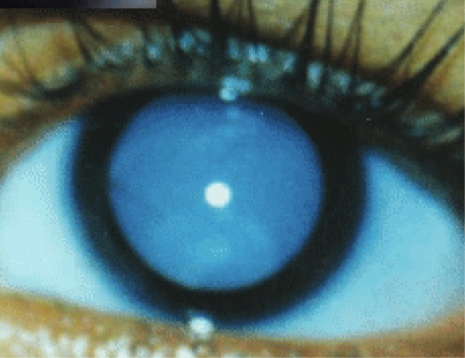
Total cataracts (congenital)
More commonly found in developing countries
entire lens being opaque = VA significantly affected
commonly assoc. with nystagmus
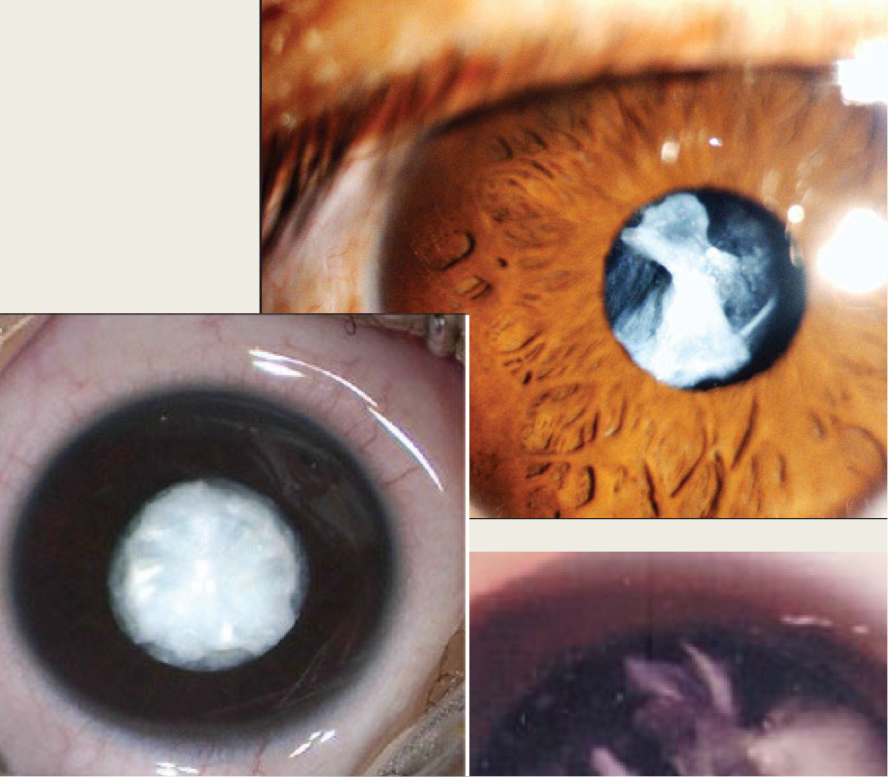
Membranous cataracts (congenital)
lens proteins are resorbed when leaving the anterior & posterior capsule
they fuse together and form a dense white membrane
Congenital cataracts treatment
Lens extraction w/ IOL Implantation
Time of lens extraction is critical (earlier = higher risk of developing juvenile glaucoma)
Bilateral dense cataracts require surgery between 4-10 weeks of age (prevent AMBLYOPIA)
Bilateral partial may not require surgery until later in life
Unilateral dense require surgery between 4-10 weeks of age (prevent AMBLYOPIA)
Unilateral partial may be observed
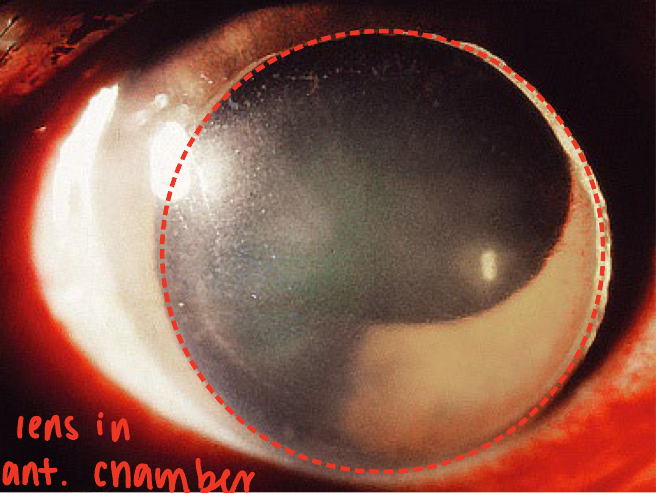
Ectopia lentis
displacement of the lens from its normal position
Will occur due to broken zonular fibers
Can be hereditary or acquired
seen in Marfan’s syndrome
Superior temporal subluxation of the lens
Bilateral presentation will be seen 80% of the time
Luxated: complete dislocation of the lens
Subluxated: partial dislocation of the lens
portion still seen in pupillary area
Phacodonesis: early sign of lens subluxation
The lens will wobble when the eye rapidly moves and returns to primary gaze
Treatment: cataract surgery
Acquired ectopia lentis
displacement of lens d/t blunt trauma
Pathophys:
Blunt trauma compresses the eye in the anterior-posterior direction
compression causes the eye to expand laterally, superior and inferior
zonules to stretch and eventually rupture
Lens movement will be dependent on:
Complete zonular rupture = dislocation
Incomplete zonular rupture = subluxation, lens will move towards intact zonules
Symptoms:
Monocular diplopia (diff focusing pts)
Distant blurred vision due to increase in astigmatism and myopia
high hyperopia may also be seen
Near blurred vision due to loss of accommodation
Presentation: lens subluxation or dislocation
lens can free float in the posterior chamber or migrate to anterior chamber
When the lens moves to the anterior chamber, the patient is at risk for glaucoma
Treatment:
Refractive error correction
lens extraction
tx of complications - glaucoma
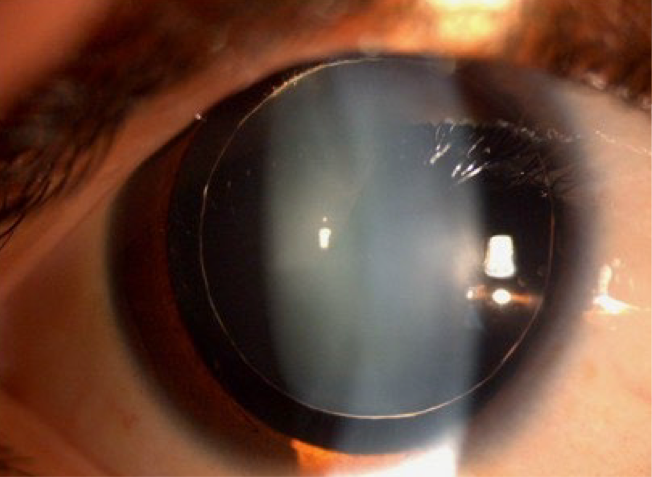
Microspherophakia
small, spherical lens
Systemic condition association: Marfan, congenital rubella
Presentation:
Refractive error: high myopia
Accommodation dysfunction
Lens: thick crystalline lens with small diameter
Entire equatorial margin will be seen with dilation
Movement of lens with change in posture
ectopia lentis
Complications: glaucoma (51%)
d/t pupillary block, angle blockage, or angle abnormalities
Treatment:
Surgical management: lens extraction
Surgical management of glaucoma
Vossius ring
pigment on the anterior capsule of the lens from posterior aspect of the iris
Cause: blunt trauma
Presentation: circle of iris pigmentation on the anterior capsule of the lens
Circle may be complete or incomplete
Treatment: none
As the pupil constricts and dilates, the iris will rub the pigment off the anterior capsule
