Upper digestive system
1/23
Earn XP
Description and Tags
From mouth to stomach
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
Oral cavity (buccal cavity) → functions
Functions:
Sensory analysis: taste, temperature, texture, touch
Mechanical processing: teeth, tongue, palate
Lubrication: mucous and saliva → helps with movement through alimentary canal
Chemical digestion (limited): salivary enzymes
Teeth and mastication → types of teeth and mastication
Primary and secondary dentation
Types of teeth:
Incisors (8): blades; clipping/cutting
Cuspids (4): cones; tearing/slashing
Bicuspids (8): bi-pronged; crush/grind/mash
Molars (12): flattened: crush and grind
Mastication:
Breaks down tough connective tissues
Mixes food with saliva
Regulated by muscles of the jaw
Up/down and side to side
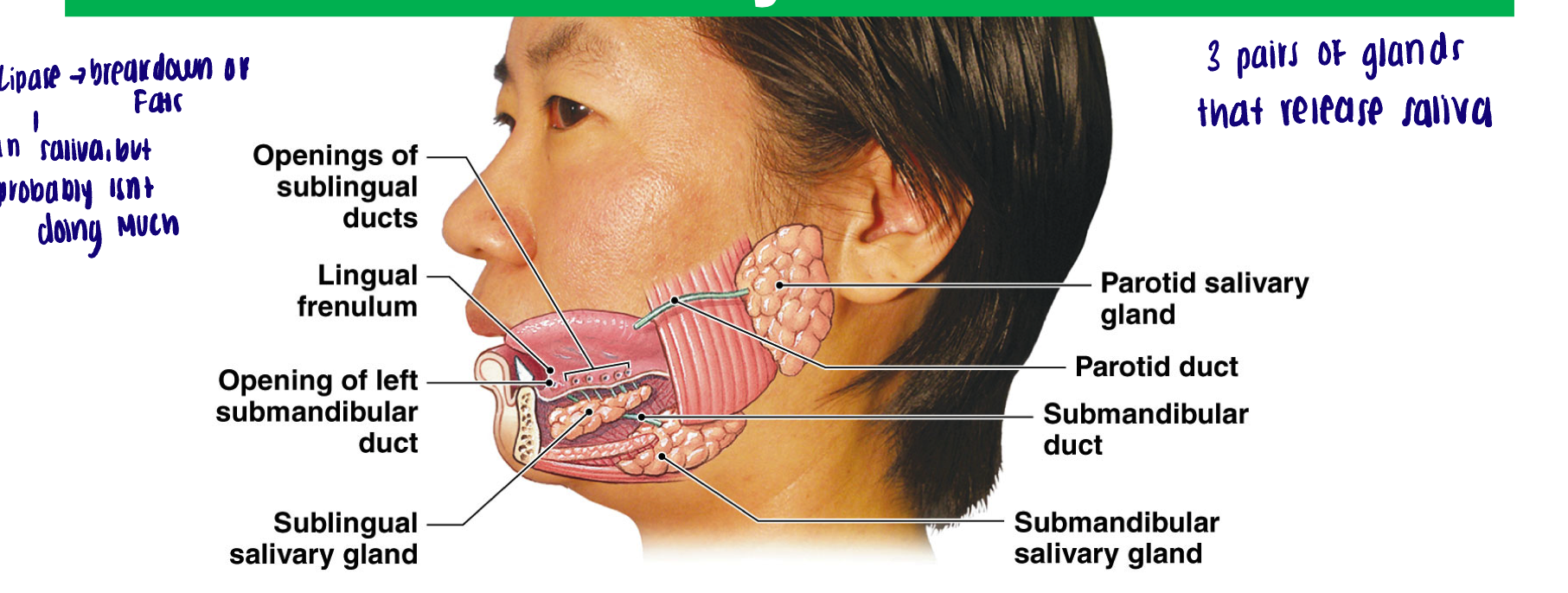
Salivary glands
2 parotid glands → largest salivary glands (production of amylase, an enzyme that breaks down carbohydrates, an example of chemical digestion)
2 sublingual glands (below tongue) → buffers and lubricant - mucin to mucous
2 submandibular glands → buffers, mucin, amylase
Lysozymes
Innate immunity: antimicrobial, break down peptidoglycans (protein sugar coat on bacteria)
Highest level in sublingual saliva
What are salivary glands regulated by
ANS
Salivatory nuclei in the medulla oblongata
Each gland has PNS and SNS innervation
PNS activation leads to increase in saliva production
SNS activation - unclear roles, small amounts of very thick, less watery saliva
Salivatory nuclei influenced by…
Cranial nerve sensory afferents
Any oral stimuli - increased production
Higher centers and other brainstem nuclei
Smelling food, chewing motions, thinking about food, nausea
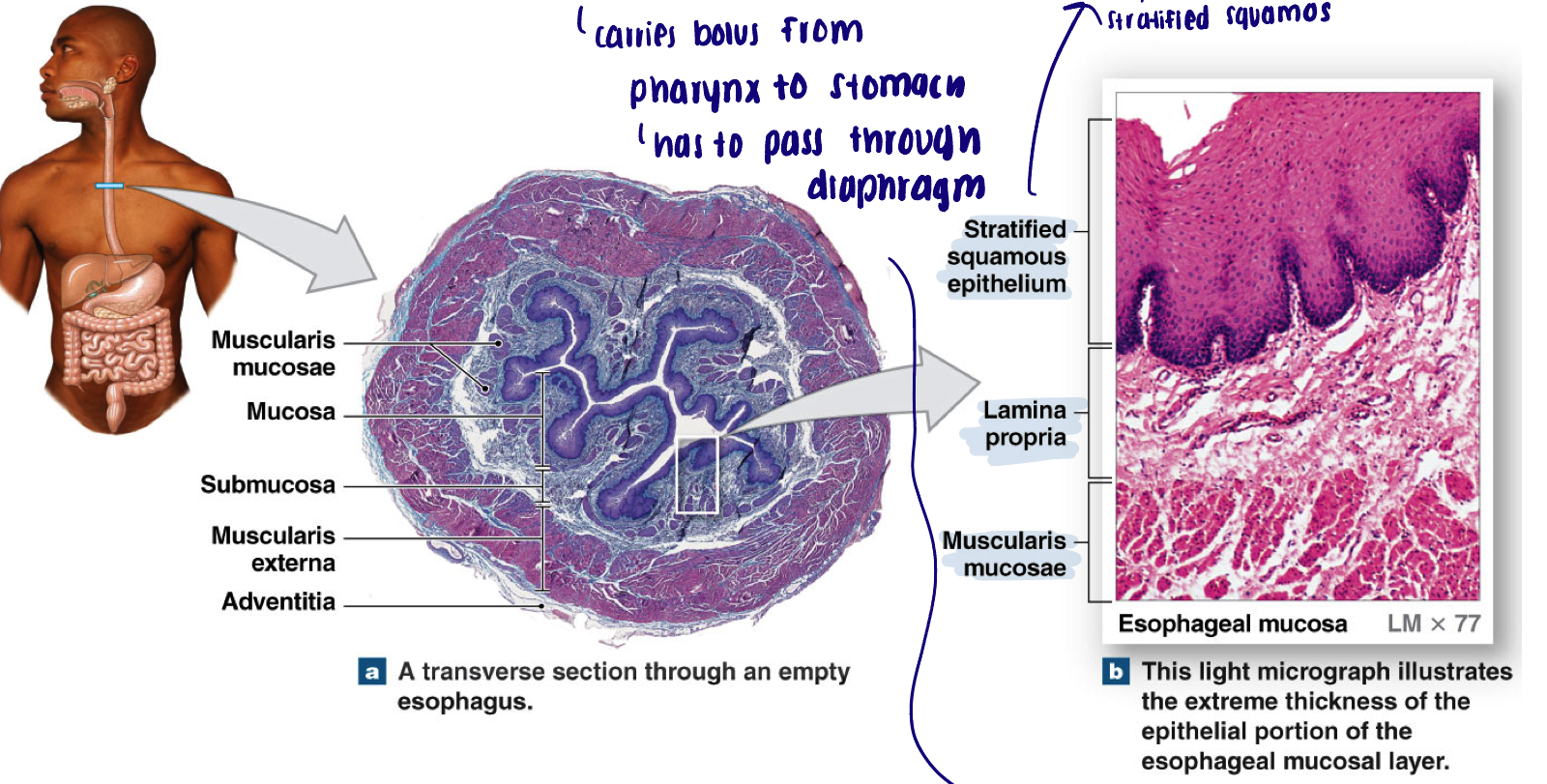
Esophagus
How long
Upper 1/3 is what type of muscle
Carries…
Muscular tube: 10 inches long; 0.8 inches in diameter
Upper 1/3 of the esophagus → striated muscle
Carries bolus from pharynx to stomach, has to pass through diaphragm
Bolus enters the peritoneum via the esophageal hiatus (an opening in the diaphragm)
Phases of swallowing (a reflex) - overview
Oral (buccal phase): voluntary
Pharyngeal phase: involuntary
Esophageal phase: involuntary
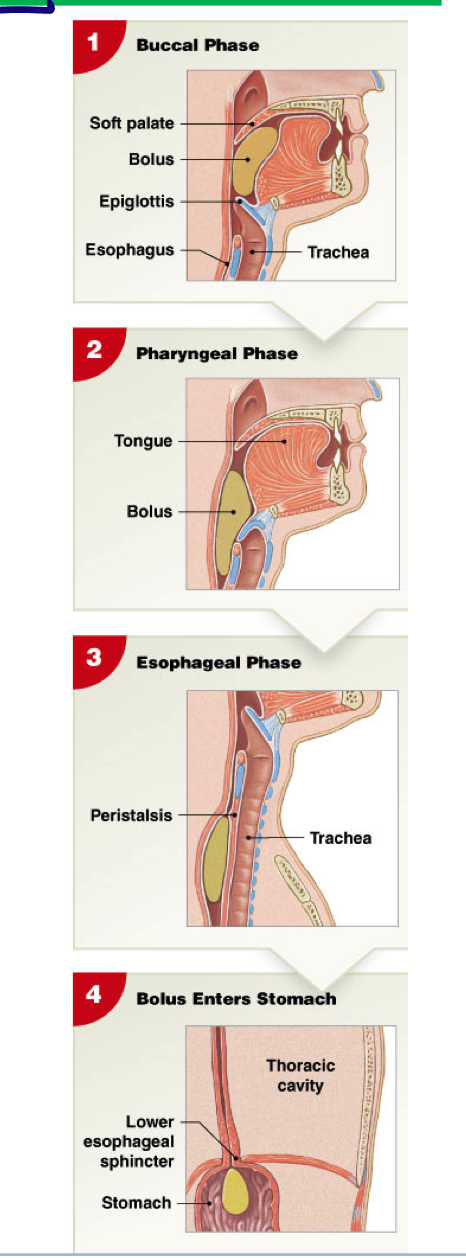
Oral (buccal phase)
Tongue against
Bolus pushes towards
Bolus enters… and stimulates
Voluntary
Tongue against hard palate - bolus pushed towards pharynx
Bolus enters oropharynx and stimulates touch receptors
Pharyngeal phase
Whats inhibited
Activation of touch receptors send…
Closure of
What raises
Relaxation of
Contraction of
Uvula
Involuntary
Respiration inhibited
Activation of touch receptors sends afferent signals to swallowing center (medulla oblongata) to coordinate the following:
Closure of entrance to nasopharynx
Larynx raises and epiglottis classes off entrance to the trachea
Relaxation of UES → skeletal but involuntary
Contraction of pharyngeal muscles to move bolus through UES
Uvula → flap to close nasopharynx
Esophageal phase
Entrances of bolus into esophagus triggers…
Bolus pushed against
Involuntary
Entrance of bolus into esophagus triggers primary peristaltic wave then pushes bolus towards stomach
Bolus pushed against LES which triggers opening of LES
Gross anatomy of the stomach
Cardia: near esophageal entrance; mucus cells
Fundus: superior portion (rounded end)
Body: major portion of stomach; mixing tank
Pylorus: area adjacent to duodenum; mucus and hormones
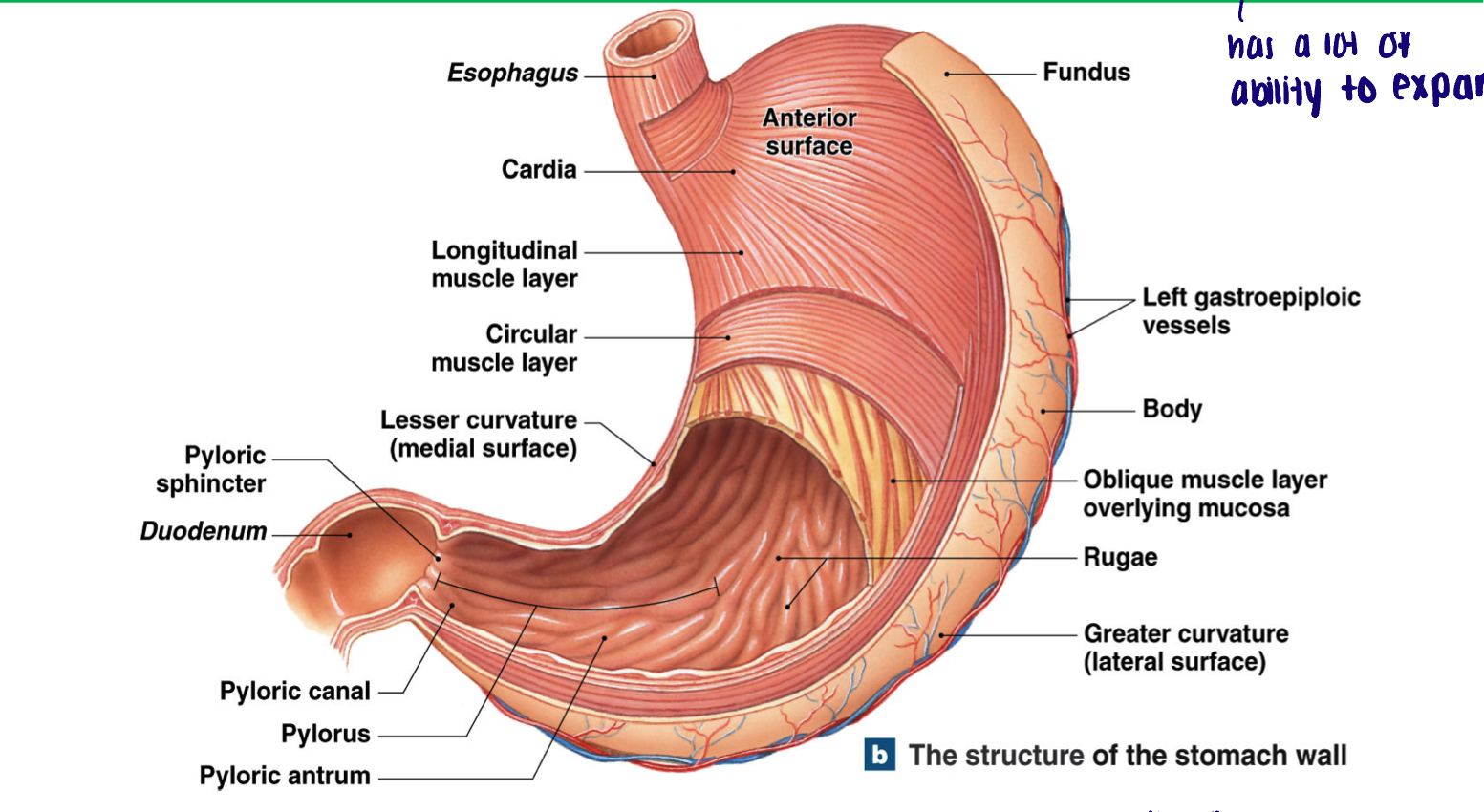
Inner surface and extra muscle layers of stomach
What do they assist with
List them
Inner surface has folds called rugae (when empty)
Can expand up to 50x
Empty → appears as a tube
Full → 1.5 L
Extra muscle layers
Strengthen muscle wall, assist in secretion and mixing
Muscularis mucosae → Extra outer circular layer
Circular
Longitudinal
Circular (extra)
Muscularis externa → extra internal oblique layer
Circular
Oblique (extra)
Longitudinal
Histology of the stomach
Simple columnar cells (mucus surface cells): life expectancy only 3 to 7 days (because they live in HCl)
Abundance of mucus cells
Gastric pits: shallow depressions in surface of stomach lining
Basal cells at the base (neck) continually divide to replace damaged epithelial cells
Gastric glands: glands extending off the neck of gastric pit (each pit communicates with several glands)
Houses important secretory cells
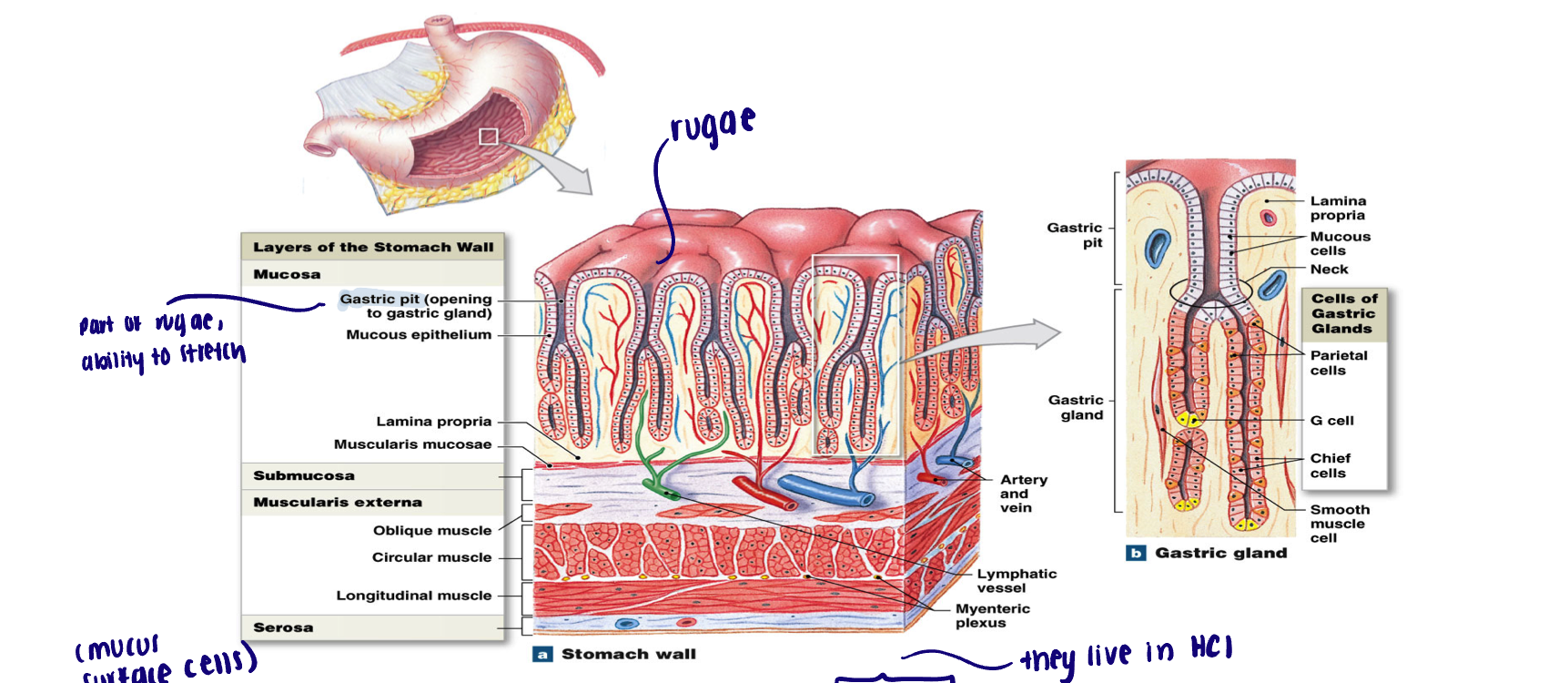
Gastric glands
Parietal cell
Chief cell
Enteroendocrine cells (primary in pylorus)
G and D cells
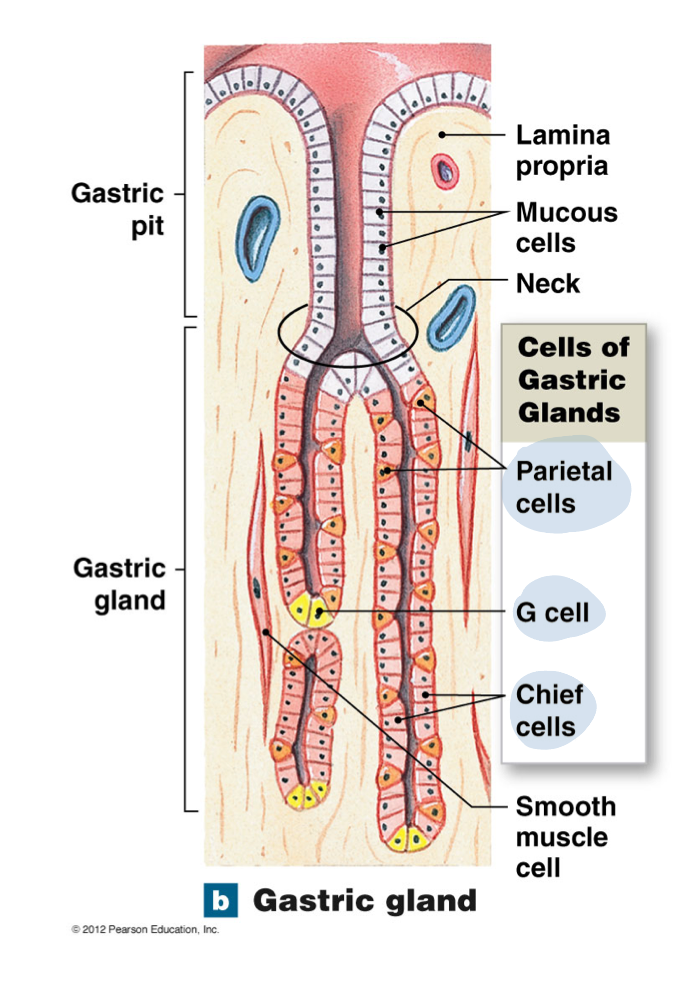
Parietal cell
Secrete
HCl - maintain balance of stomach pH 1.5-2.0
Intrinsic factor - absorption of vitamin B12 (how we get vitamin B12)
Chief cell
Secretes pepsinogen
Inactive precursor of pepsin
Pepsinogen is cleaved into pepsin in low pH
Pepsin is a proteolytic enzyme that BEGINS the process of protein digestion
Enteroendocrine cells
Primary in pylorus
G cells: secrete the hormone gastrin → increases in stomach activity → on plexus → stimulating secretion and motility
Stimulates secretion of parietal and chief cells
Muscle contraction leading to mixing
D cells: secrete the hormone somatostatin (growth hormone inhibiting hormone)
Inhibit the release of gastrin
Acid secretion by the stomach
1) hydrogen ions generated inside a parietal cell as carbonic anhydrase converts CO2 with H2O to carbonic acid (H2CO3) which then dissociates
2) counter-transport mechanism ejects the bicarbonate ions into the interstitial fluid and imports chloride ions into the cell
3) chloride ions then diffuse across the cell and exit through open chloride channels into the lumen of the gastric gland
4) hydrogen ions are actively transported into the lumen of the gastric gland
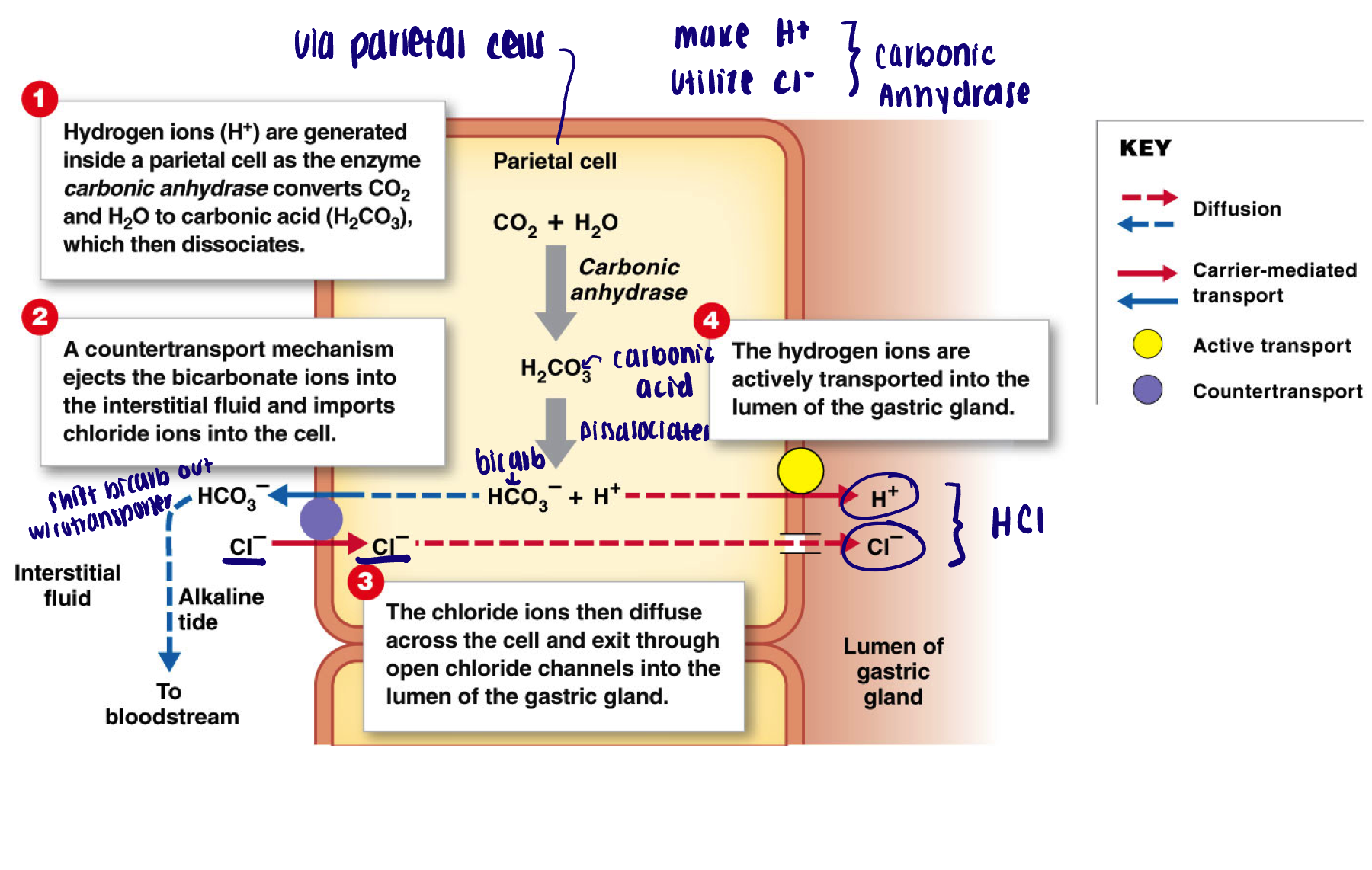
Function of gastric acid
Destroys microorganisms
Denatures proteins and inactivates any enzymes present in the food
Breaks down plant cell walls - cellulose and connective tissues in meat
Conversion of pepsinogen to pepsin
Phases of gastric secretion
Cephalic
Gastric
Intestinal
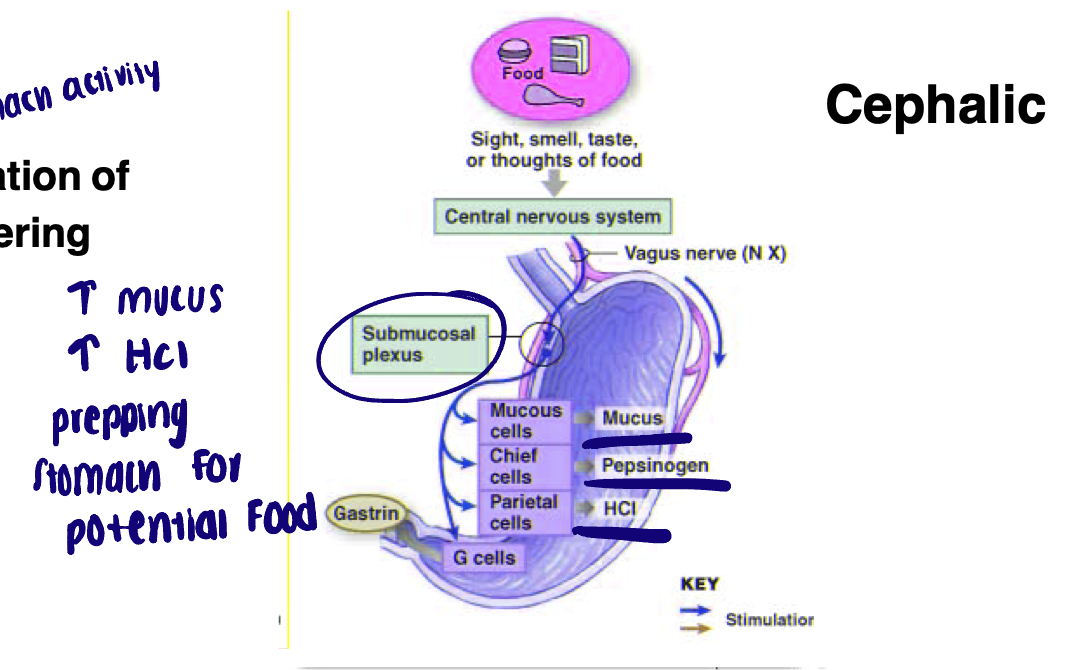
Cephalic phase of secretion
Initiation of
Regulated by
What plexus
Lasts for how long
Initiation of gastric secretion prior to food entering
Regulated by PNS - vagus nerve
Submucosal plexus
Lasts only a few minutes
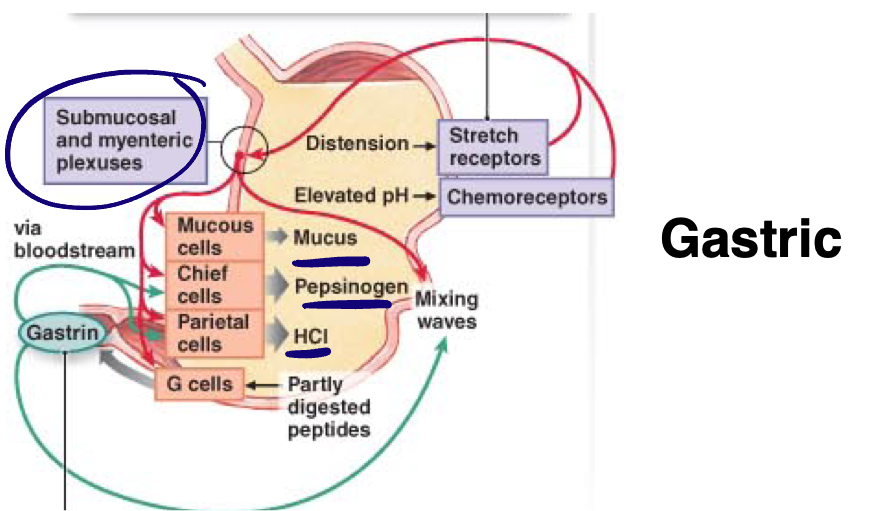
Gastric phase of secretion
Distention
Stimulate plexus…
Lasts
Begins with arrival of food into the stomach; further increases of gastric secretion
Distention - stretch detected by baroreceptors, increased pH, and undigested proteins
Stimulate submucosal plexus (secretion)
Stimulate myenteric plexus (mixing waves)
3-4 hours
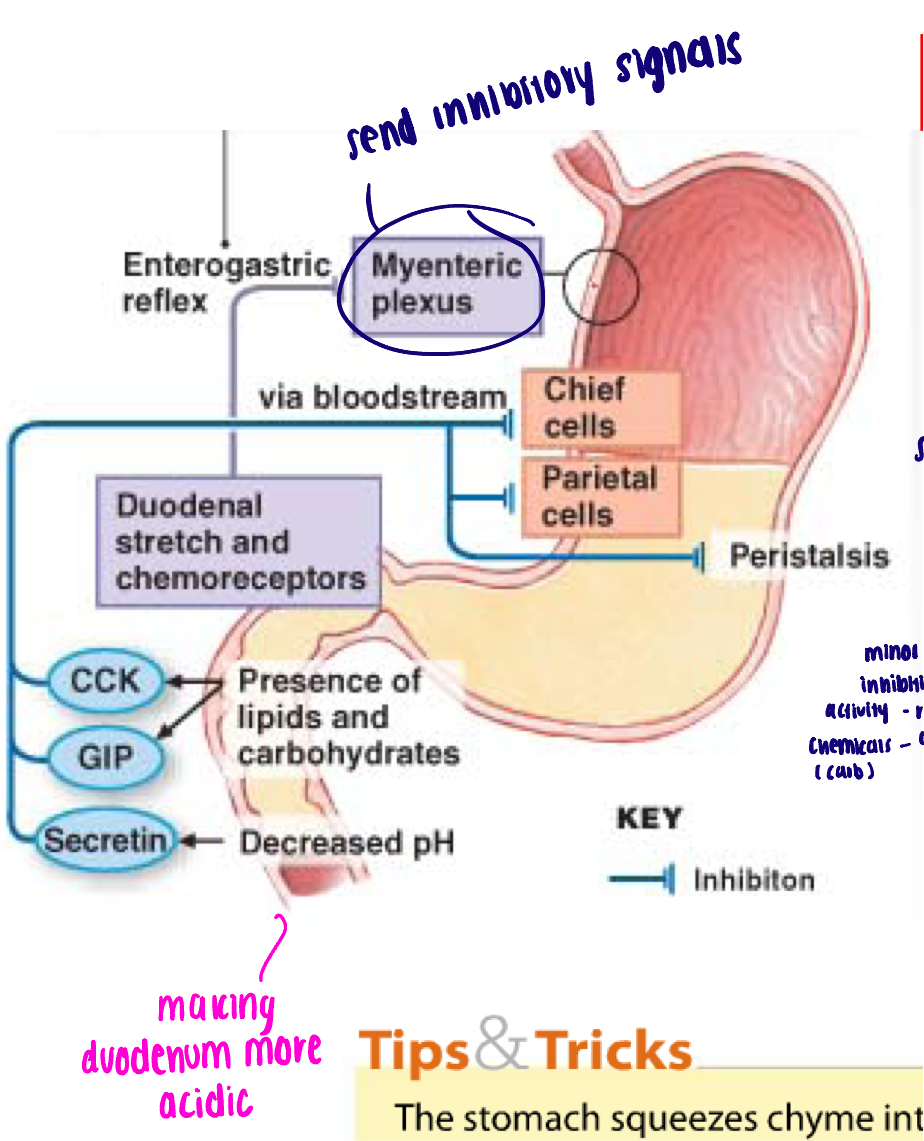
Intestinal phase of secretion
Presence of chyme in small intestine trigger…
Release of hormones
GIP
Secretin
CCK
Overall effect
Presence of partially digested food (chyme) in small intestine trigger:
Enterogastric reflex (neural): afferent nerves carry mechanical signal to ENS of the stomach to inhibit gastric motility and secretion
Release of hormones: decrease gastric secretion and motility
GIP → Minor role in inhibiting stomach activity, released by carbs to cause release of insulin
Secretin → released by duodenum as pH changes
CCK → released by cells of duodenum in presence of proteins/fats, tells stomach to decrease activity
Overall effect: slow the rate of gastric emptying - ensure the small intestine is not overwhelmed and can proceed efficiently