Brain & Spinal Cord Injuries
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
50 Terms
Head Trauma
Over 69,000 TBI-related deaths in the United States in 2021
Injuries to the brain are more likely to cause death or permanent disabilities when compared to other injuries
Direct cost of TBI direct care: > $25 billion annually
People < 5 years old & > 75 years old
Adolescent & young adults - most severe cases
Vulnerable populations:
Racial/ethnic minorities, service members, veterans, individuals who are unhoused or incarcerated, survivors of intimate partner violence and whose living in rural areas – ↑risk for TBI
Considered a public health issue
Head Injuries: Traumatic Brain Injury (TBI)
Result of an external force; is of sufficient magnitude to interfere with daily life and warrants treatment.
Leading causes:
Falls (48%)
MVCs (14%)
Being struck by objects (15%)
Assaults (10%)
Primary vs. Secondary injury:
Primary injury: consequence of direct contact to head/brain during instant of initial injury → extracranial focal injuries & focal injuries from sudden movement of the brain within cranial vault (subdural hematomas, concussions, DAI)
Secondary injury: evolves over time after initial injury; d/t inadequate delivery of glucose & oxygen to cells
Intracranial pathologic processes -- intracranial hemorrhage, cerebral edema, intracranial hypertension, hyperemia, seizures, vasospasm
Other things that could affect this: hypotension, hyperthermia, hypoxia, hypercarbia, infection, electrolyte imbalances, anemia → further complicate an already complex injured brain
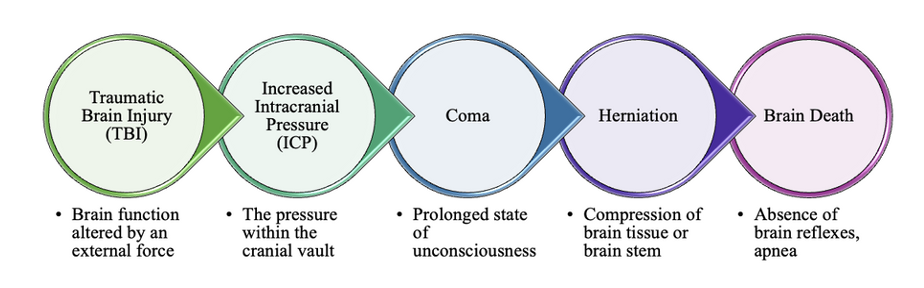
Monroe-Kellie hypothesis:
Volume in blood, brain or CSF ↑ → other 2 have to compensate to prevent ICP
Pressure → displaces brain against or through skull → restriction of blood flow to brain → decreased oxygen delivery & waste removal → anoxia; inability to metabolize properly → ischemia, infarction, irreversible brain damage → brain death
Head Injuries: Scalp Injury
Trauma from abrasion, contusion, laceration, or subgaleal hematoma.
Minor injury but can bleed profusely due to poor blood vessel constriction.
Large avulsion (injury) → possibly life-threatening.

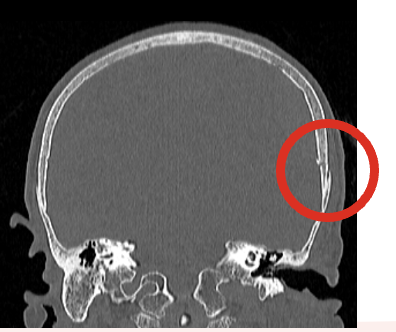
Head Injuries: Skull Fracture
Forceful trauma → break in the continuity of skull with or without damage to the brain; classified by types and location.
Simple (linear): break in continuity of bone.
Comminuted: splintered or multiple fracture.
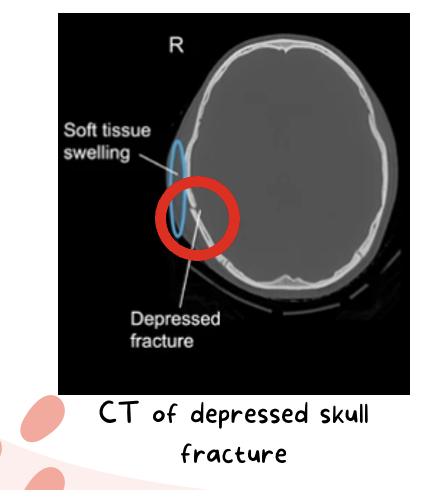
Depressed: skull bones displaced by force downward.
Open vs. Closed Fractures: Open = scalp laceration or tear in dura; Closed = dura intact
Head Injuries: Clinical Manifestations
Symptoms depend on severity and atomic location of underlying brain injury.
Persistent, localized pain = possible fracture
Amnesia before or after injury
Loss of consciousness—how long were they down?
Glasgow Coma Scale – verbal response, eye-opening response, motor response
Swelling in region of fracture possible
Bleeding/hemorrhage from nose, pharynx, ears or conjunctiva
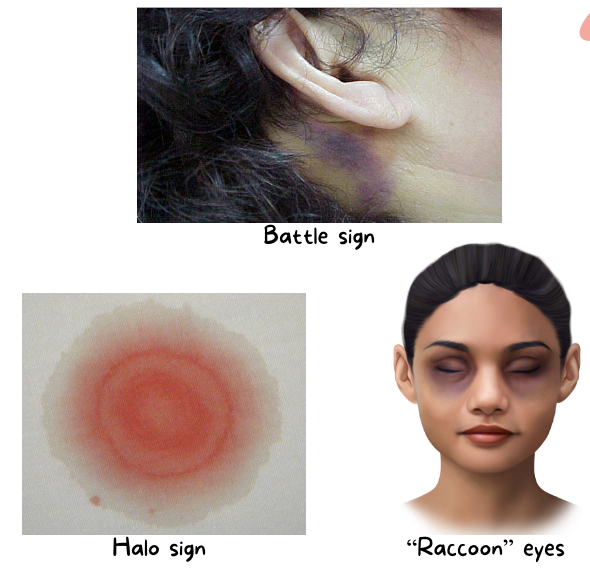
Ecchymosis over mastoid (Battle sign)
“Raccoon” eyes
CSF leak from eyes, ears, or nose with basal skull fractures
Infection risk—pathways for organisms
Meningitis
Halo sign—let drainage leak onto pad/towel
Can observe clear/yellowish separate around blood indicating CSF leakage
Seen with basilar skull fracture
What are the 3 indicators of a basilar skull fracture?
Battle sign (ecchymosis/bruising over mastoid)
Halo sign (leakage from the CSF—light gray color)
“Raccoon” eyes
Head Injuries: Assessment & Diagnostics
Assessment:
Respiratory status (airway)
Hypoxia → brain injury/death after 3-5 min
GCS= earliest indicator of neurological deterioration
Cranial nerve function—eye blink response, gag reflex, tongue & shoulder movement
Level of consciousness, responsiveness
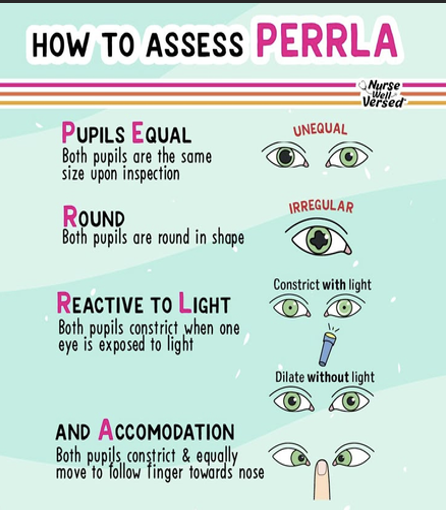
Pupillary response (PERRLA)
Unequal = possibly head trauma
Sensory and motor function (make sure equal and reactive bilaterally)
Signs of increased ICP
Irritable, restless, confused, pupillary changes, headache, changes in speech, ↓ motor function, projectile vomit w/o nausea → vital changes, abnormal reflexes
Cushing’s triad: bradycardia, irregular respirations, hypertension (widening pulse pressure)
Diagnostics:
ABGs (objective indicator of how patient is oxygenating)
CBC w/ diff
Blood glucose level
Electrolyte level
Blood and urine osmolarity
Toxicology screen
CT scan
Fracture present? → was the brain injured?
Cervical spine
MRI scan
Head Injuries: Management
Non-depressed fractures: close observation for signs of brain injury.
Discharge education for family.
Depressed fractures: requires surgery with elevation of skull and debridement.
Consequential injuries from fracture (scalp laceration, dural tears, lacerations from bony fragments, etc.)
Patient/Family Education on Prevention:
Always wear helmets when skateboarding, riding a bike, motorcycle, skiing, playing football, etc.
Wear your seatbelt and use approved car seats/booster seats.
Avoid dangerous activities
Firearm safety
Avoid riding in the back of a pick-up truck
Fall prevention at home
How can you prevent falls in the inpatient setting?
bed alarms, grip socks, bed at a lower setting, call light near patient, hourly rounding, etc.
Head Injuries: Considerations for Unique Populations
Veterans:
Common causes of TBIs: combat-related blast injury, which can cause 4 levels of injury.
Same treatment as civilians but more complex needs.
Older Adults:
Head injuries look very different in relation to the cause of the injury, increased mortality rates, increased lengths of hospital stays and worse functional outcomes.
Difficulties with assessments
Physiologic changes of aging can affect type and severity of injury or lead to complications. (brain atrophy, more fragile bones, etc)
Anticoagulants (can make the fall a lot worse → brain bleeds; bruise → hemorrhage)
Routine eye exams & Medication reconciliation
Routine check-ups of eyes, med rec. to reduce number of meds that cause dizziness or sleepiness

A. Battle Sign —Battle sign (or Battle’s sign) is characterized by bruised over the mastoid process due to a fracture of the middle cranial fossa. It is considered a strong indicator of a basilar skull fracture.
What clinical sign is most indicative of a basilar skull fracture?
A. Battle Sign
B. Hemiparesis
C. Nuchal Rigidity
D. Decerebrate posturing
Brain Injuries: TBI
Closed (blunt) TBI: head accelerates, then rapidly decelerates or collides with another object → brain tissue is damaged but there’s no opening through the skull and dura.
Open (penetrating) TBI: object penetrates the skull, enters brain, damages adjacent soft brain tissue or blunt trauma to head so severe that it opens the scalp, skull, and dura → brain exposed.
Brain Injuries: Focal Injuries
Are isolated injuries to small parts…(specific area)
Contusion: brain is bruised and damaged d/t impact of brain against skull.
S/sx vary on size, location, and extent of cerebral edema:
Loss of consciousness + stupor and confusion
Hemorrhage & edema (peak at 18-36 hrs) → increased ICP & possible herniation
Coup and Contrecoup
coup = actual impact
countercoup = the brain hitting the skull (the rebound)
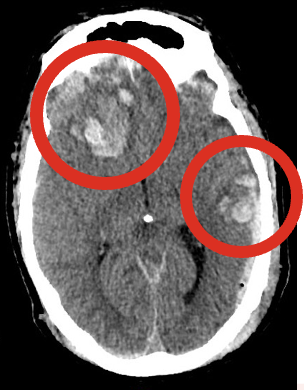
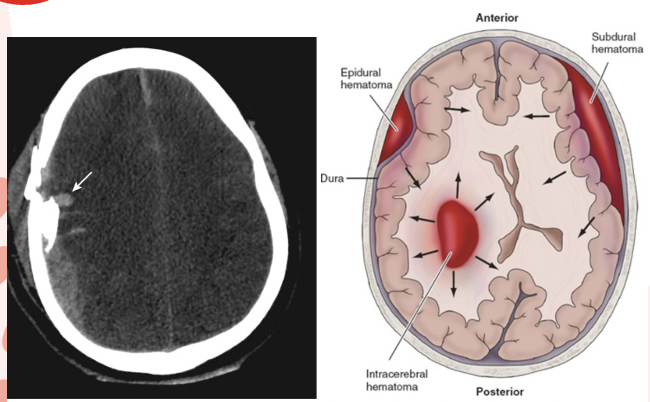
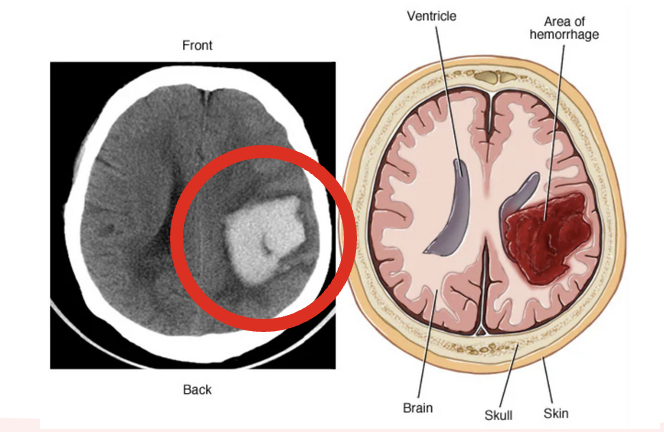
Hematoma: collection/pooling of blood in brain may be:
Symptoms can be delayed until damage is significant but even small, rapidly developing hematomas can be fatal.
Image—(R) Contusion (L) Hematoma
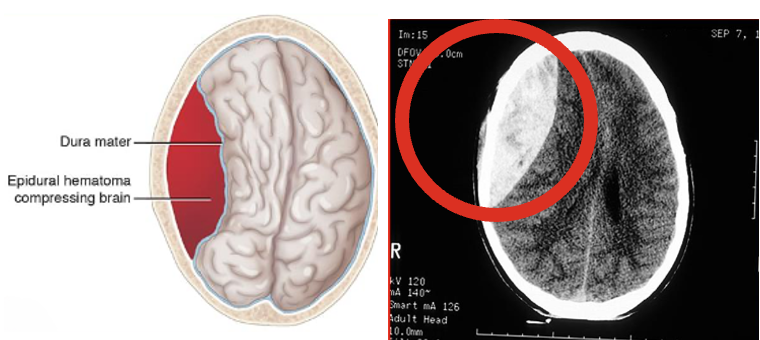
Brain Injuries: Epidural Hematoma (above dura)
Can result from fracture → rupture/laceration of middle meningeal artery (between dura & skull inferior to thin portion of temporal bone)
Clinical Manifestations:
Symptoms progress r/t expanding hematoma.
Hallmark: (lucid interval)—Brief loss of consciousness then awake & aware; Later restless, agitated, confused → coma
Lucidity d/t rapid absorption of CSF to compensate
Herniation: dilation and fixation of pupils or paralysis of extremity
Significant neurological deficits & respiratory arrest within minutes
MEDICAL EMERGENCY
Management:
Burr holes—openings through the skull to decrease ICP
Craniotomy—to remove clot and control bleeding (make room for the brain to swell)
Drain placement—to prevent blood accumulation (EVD)
Brain Injuries: Intracerebral Hematoma (within the brain)
Bleeding into parenchyma of brain; commonly from force to head over a small area (missile injuries, bullets, etc.); can also be a result of non-traumatic origin.
Clinical Manifestations:
Subtle onset of symptoms
Starts with new neurologic deficits then headache
Nausea/Vomiting (b/c of brain stem compression)
Management:
Supportive care (pain, N/V, noise reduction, cluster care, low stimulation)
Control of ICP
Administration of fluids, electrolytes and anti-hypertensives
Surgery (craniotomy or craniectomy)—to remove clot and control hemorrhage but not always possible
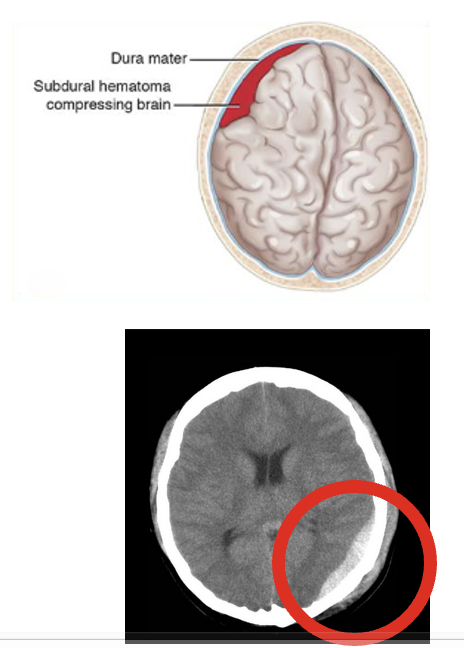
Brain Injuries: Acute Subdural Hematoma (SDH) (below the dura)
Collection of blood between the dura & brain, most commonly d/t trauma; typically from venous sources. (usually from falls)
Clinical Manifestations:
Changes in LOC
Pupillary signs
Hemiparesis (unilateral weakness)
Coma, increased BP, decreased HR & RR (cushing’s triad) = rapidly expanding mass → immediate intervention
Management:
Immediate craniotomy — to allow subdural clot to be removed.
Outcome is dependent on control of ICP & close monitoring of respiratory function
High mortality rate d/t brain damage
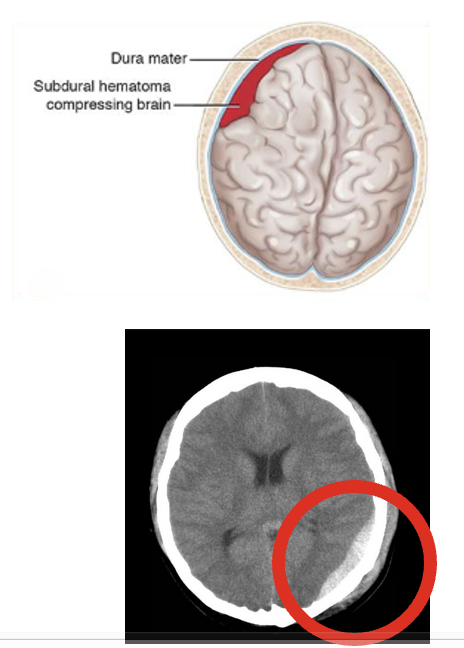
Brain Injuries: Chronic Subdural Hematoma (SDH) (below the dura)
Collection of blood between the dura & brain, most commonly d/t trauma; typically from venous sources. (common in elderly)
Clinical Manifestations:
Time between injury and onset of symptoms can be lengthy (weeks to months)
Could be mistaken as a stroke
Intermittent, severe headaches, alternating focal neurological signs
Personality changes, mental deterioration, focal seizures
Management:
Surgical evaluation for clot removal
Coagulopathies and anticoagulation
Why are epidural hematomas more emergent than subdural hematomas?
Epidural hematomas are more emergent because they often involve an arterial bleed (typically from the middle meningeal artery), leading to rapid expansion and increased intracranial pressure, while subdural hematomas usually result from slower venous bleeding.
Brain Injuries: Concussion
Temporary loss of neuronic function with no apparent structure damage to brain; known as a mild TBI.
Result of blunt trauma from acceleration-deceleration force, direct blow, or blast injury.
Location may affect presentation.
Repeated concussive incidents → Chronic Traumatic Encephalopathy (CTE)
Frontal lobe injury → abnormal behavior
Temporal lobe → amnesia or disorientation
Watch Out For:
Decreased level of consciousness
Worsening headache
Dizziness
Seizures
Abnormal pupil response
Vomiting
Irritability
Slurred speech
Numbness
Weakness in arms or legs
Medical Management:
Physical and neurological assessments
Admission to inpatient floor for observation
CT, MRI
PET
C-Collar/C-Spine precautions
Goal: to preserve brain homeostasis and prevent any secondary brain injury
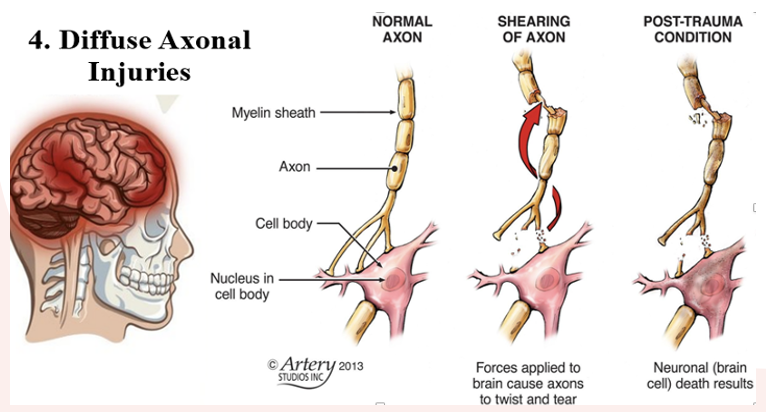
Brain Injuries: Diffuse Axonal Injury (DAI)
Caused by widespread shearing and rotational forces that create damage throughout the brain and axons in cerebral hemispheres, corpus callosum, and brain stem.
Injury could be diffuse with no identifiable focal lesion.
Prolonged traumatic coma; associated with poor prognosis than focal lesion.
Can also experience decorticate and decerebrate posturing, global cerebral edema in severe cases.
Recovery is dependent on severity of axonal injury.
Prognosis:
Dysautonomia - common complication; disruptions in autonomic body functions (HR, RR, temperature, BP, sweating, muscle tone, posturing, digesting) – chronic, long-term (baseline)
Neurostorming – sudden, episodic hyperactivity of the nervous system in possible effort to “reboot brain” post injury but is ineffective
Medical Management:
Physical and neurological assessments
CT, MRI (MRI > CT)
PET
C-Collar/C-Spine precautions
Goal: to preserve brain homeostasis and prevent any secondary brain injury.
Stabilization of cardiovascular and respiratory function
Control of hemorrhage and hypervolemia
Maintenance of optimal blood gas values
Complications of Brain injuries
DI & SIADH
Herniation
Displacement of brain tissue d/t pressure, injury, etc. → tissue hypoxia from lack of perfusion → tissue death
Increased ICP
Hematoma/hemorrhage
Clinical Manifestations:
Severe headache
Nausea/vomiting
Decreased LOC, restlessness, irritability
Dilated or pinpoint non-reactive irritability—(fixed & dilated; blown)
Cranial nerve dysfunction
Altered breathing pattern —Cheyne-Stokes respirations, central neurogenic hyperventilation, apnea
Deterioration in motor function
Cushing’s triad (late finding)—HTN + widening pulse pressure, bradycardia, irreg. breathing
Seizures
Brain Injuries: Interventions
Ongoing assessment of secondary injuries (other things that are going on in the body)
CSF in nose & ears – report to provider
Wounds
Under the influence – responsiveness & appropriate monitoring
Still talk to your patients even if they’re not responsive – hearing is affected last after a brain injury
Immobility
C-spine precautions, splints, specialty beds
Monitor fluid and electrolytes (issues with ADH, etc.)
Seizure precautions (suction, o2, railing pads, bed lowest position, etc.)
Nasogastric tube insertion (↓ gastric mobility & reverse peristalsis → prevent regurgitation & aspiration)
Craniotomy—removal of dead brain tissue; tx for intracranial hemorrhages & hematomas, tumor removal
Burr holes
External ventricular drain (EVD) (temporary)
Family support
Brain death and organ donation
3 cardinal signs of brain death = coma, absence of brain stem reflexes, & apnea
EEG, cerebral blood flow studies, transcranial doppler, brain stem auditory-evoked potential for confirmation
End-of-life care
Medications:
Mannitol (decreases ICP)—complications = pulmonary edema
Dexamethasone (decreases brains swelling)
Barbiturates, Propofol
Puts patient in medically induced coma to help decrease cellular metabolic demand of the brain until ICP decreases
B/c altered neurological status → difficulty assessing neurological status
Tx to avoid secondary injury d/t hypoxia
Phenytoin, Diazepam (seizure prophylaxis)
Opioids (not ideal for patients on the ventilator because of respiratory depression)

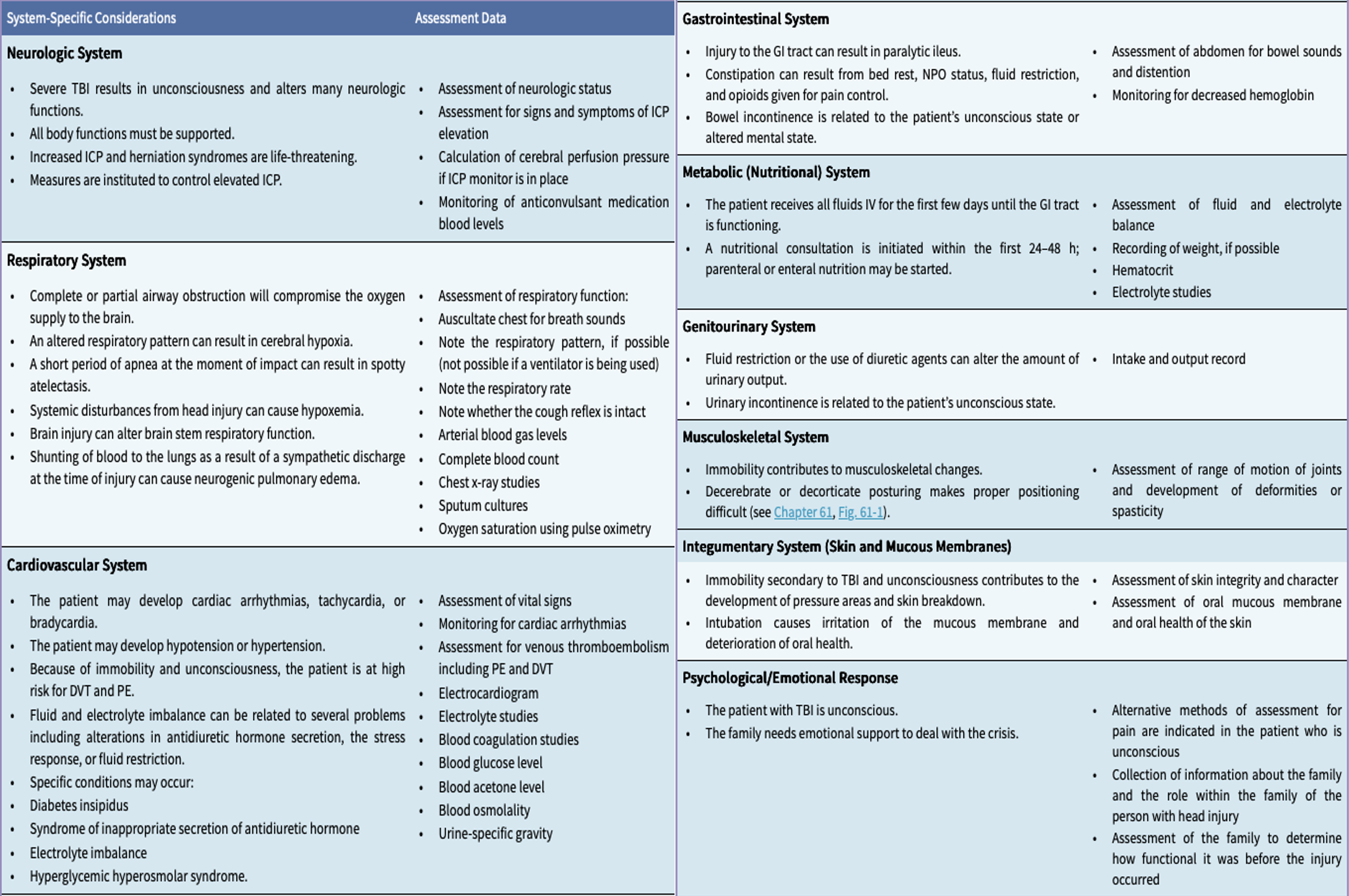
Multi-System Care for a Patient with a TBI (image)
B. Epidural hematoma—Epidural hematomas are caused by a rupture from a torn artery due to a fracture. This injury is considered a medical emergency because the torn arteries are more forceful and bleed faster, increasing intracranial pressure on the brain. This leads to quick progression of symptoms such as brain herniation, loss of consciousness, permanent brain damage or death.
Which hematoma is typically arterial in origin and considered a medical emergency?
A. Subdural hematoma
B. Epidural hematoma
C. Intracerebral hematoma
D. Chronic subdural hematoma
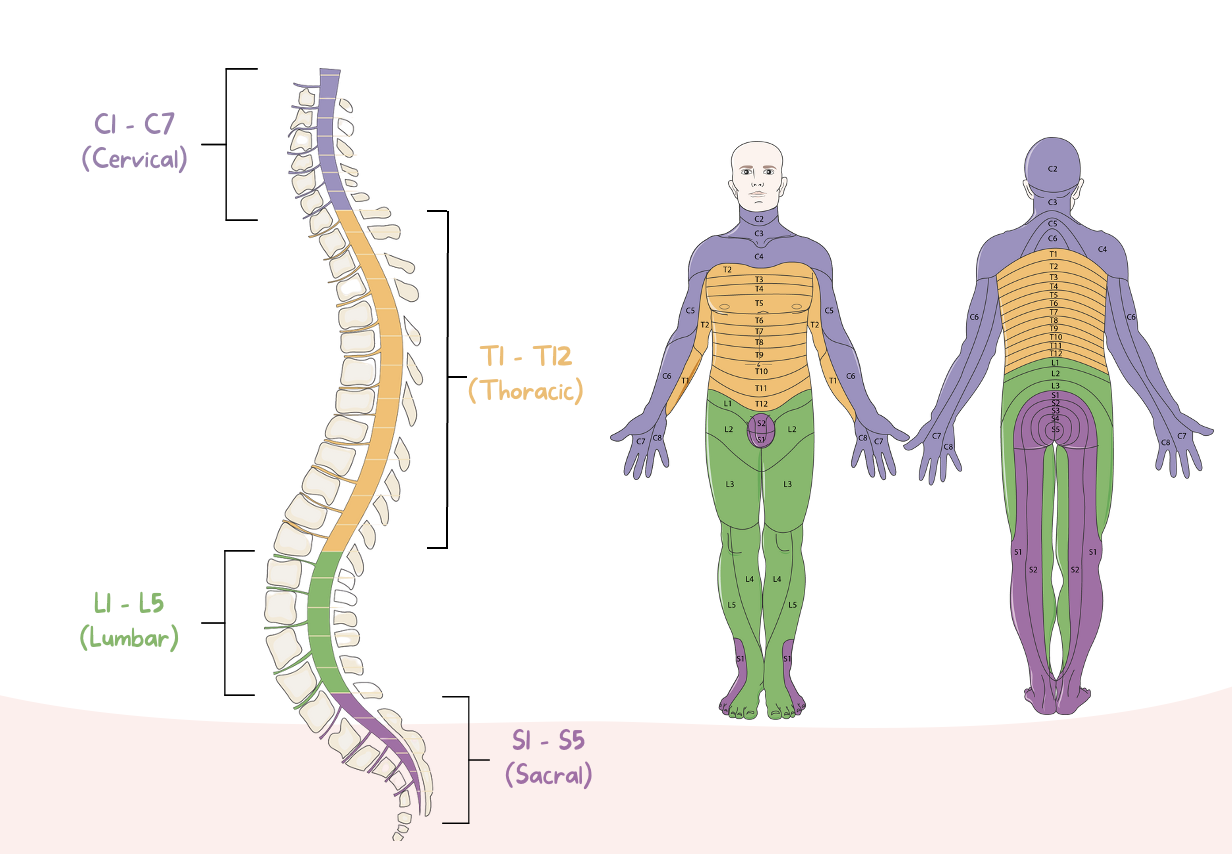
Spinal Cord Injuries occur when there is an….
Injury to the spinal cord, vertebral column, supporting soft tissue, or intervertebral discs caused by trauma.
Most common causes:
MVCs
Falls
Violence (most GSWs)
Sport-related injuries
In 2019, indirect patient cost for care - over $77,000/year
Risk factors: younger age, males, alcohol, and illicit drug abuse
Major causes of death: pneumonia, pulmonary embolism (PE), sepsis

Spinal Cord Injuries cause a….
Wide range of damage
Transient concussion → Contusion, laceration, compression of spinal cord ⟶ Complete transection
Paraplegia - paralysis of lower body (below T1)
Tetraplegia - paralysis of all 4 extremities (formerly quadriplegia)
Primary & Secondary Injuries
Primary - result from initial insult or trauma; usually permanent
Secondary - caused by edema & hemorrhage
CTLS
Cervical (C1-C8)
Thoracic (T1-T12)
Lumbar (L1-L5)
Sacral (S1-S5)
Incomplete Spinal Cord Syndromes
Central Cord
Lateral Cord (Brown-Séquard)
Anterior Cord
Spinal Cord Injuries: Central Cord Syndrome
Cause:
Injury or edema of central cord, typically cervical area.
Characteristics: (varies)
Motor deficits (upper vs. lower extremities)
Sensory loss (usually more pronounced in upper extremities)
Bowel/bladder dysfunction
*typically the most common resulting from hyper-extension of the neck; prognosis favorable but not for hand function
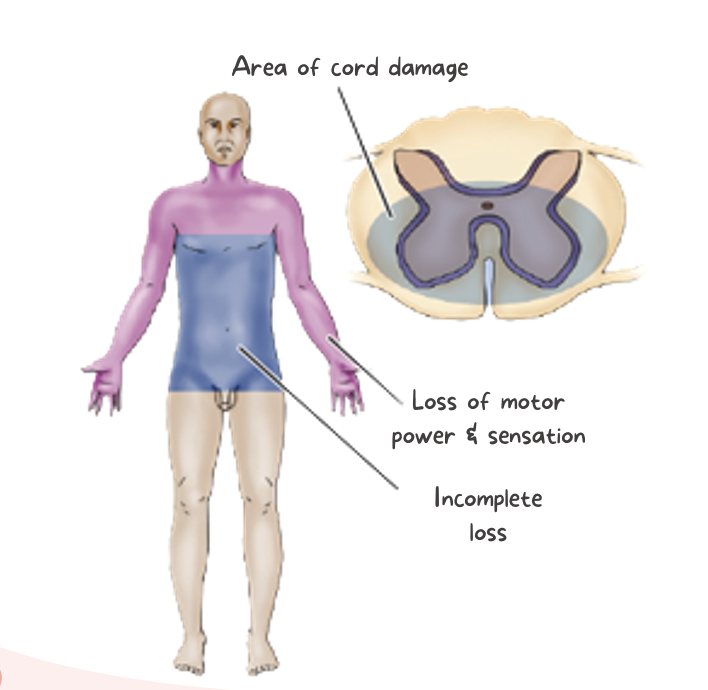
Spinal Cord Injuries: Anterior Cord Syndrome
Cause:
Acute disc herniation or hyper-flexion injuries r/t fractures/dislocation of vertebra
Result of injury to anterior spinal artery (supplies 2/3 of the spinal cord)
Characteristics:
Loss of pain, temperature, motor function below level of lesion.
Light touch, position, and vibration sensation = intact
*rare; complete motor paralysis but come intact sensory function; lower extremities more affected
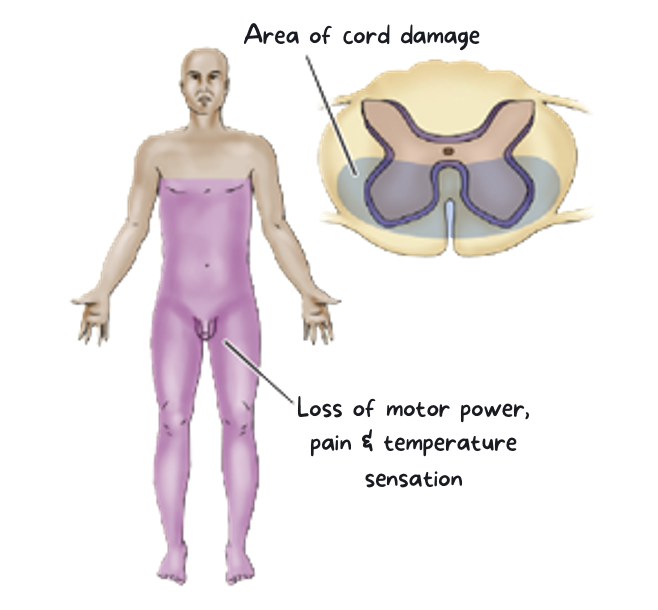
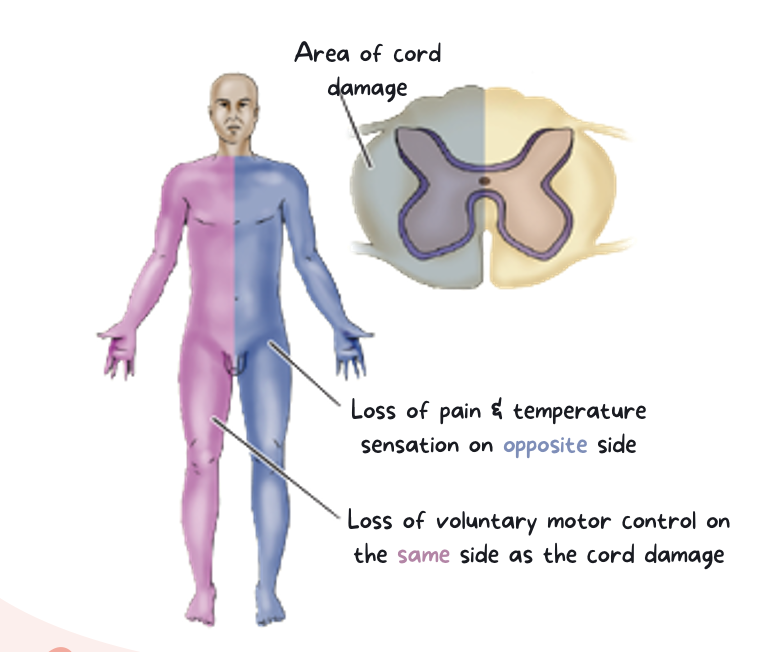
Spinal Cord Injuries: Lateral Cord Syndrome (Brown-Séquard)
Cause:
Transverse hemi-section of cord (north to south), usually from
a knife or missile injury
fracture/dislocation of a unilateral articular process, or
possibly an acute ruptured disc
Characteristics:
Ipsilateral paralysis or paresis + loss of touch, pressure and vibration (same side)
Contralateral loss of pain and temperature (opposite side)
Spinal Cord Injuries: Clinical Manifestations
Dependent on type and level of injury.
Lowest level with intact sensory or motor function
Total or partial
Loss of bladder and bowel control
Loss of sweating and vasomotor tone
Marked reduction of blood pressure (from loss of peripheral vascular resistance)
Acute pain
Respiratory dysfunction:
Injuries at or above C4 → paralysis of diaphragm.
Ventilator support (required)
Nerves at C4 innervate the phrenic nerve which is involved in the movement of the diaphragm
Injuries of T12 and above
involves the abdominal muscles—for them to have an effective cough, to clear their lungs of any gunk—so if that nerve is damaged or severed, they aren’t able to cough effectively.
Cough assist! (Compressing the stomach lightly)
Muscles involved in respiration:
C4 – diaphragm (due to phrenic nerve involvement)
Injuries at C4 or above → paralysis of diaphragm → acute respiratory failure = requiring mechanical ventilation
T1-T6 – intercostals
T6-T12 – abdominals
C1
Little or no sensation or control of head and neck; no diaphragm control; requires continuous ventilation.
C2-C3
Head and neck sensation; some neck control; independent of mechanical ventilation for short periods.
C4
Good head and neck sensation and motor control; some shoulder elevation; diaphragm movement.
C5
Full head and neck control; shoulder strength; elbow flexion
C6
Fully innervated shoulder; wrist extension, or dorsiflexion.
C7-C8
Full elbow extension; wrist plantar flexion; some finger control.
T1-T5
Full-hand and finger control; use of intercostal and thoracic muscles.
T6-T10
Abdominal muscle control, partial to good balance with trunk muscles.
T11-L5
Hip flexors, hip abductors (L1-L3); knee extension (L2-L4); knee flexion; and ankle dorsiflexion (L4-L5).
S1-S5
Full leg foot, and ankle control; innervation of perineal muscles for bowel, bladder, and sexual function (S2-S4).
Spinal Cord Injuries: Assessment & Diagnostics
Detailed neurological assessment
Light touch with cotton ball
Sharp vs dull discrimination with a safety pin
Hot vs cold with container of hot/cold water
Deep tendon reflexes – elbows, knees
Muscle flaccidity – hypo, hypertonia, spastic, etc.
—————————————
Secondary injuries
X-ray of suspected injury
Lateral cervical spinal x-rays & CT/CAT
Cervical neck collar (C-collar)—no pillow
Pt should not be able to move neck left to right, to prevent any further damage to cervical area
In place until cleared by neurosurgery, trauma - usually with confirmation with CT/MRI
Immobilization
Thoracic & lumbar precaution
HOB at 0 degrees
Strict bed rest
Log roll
MRI, if ligamentous injury is suspected
Myelogram (if contraindicated)
Continuous EKG monitoring
Bradycardia and systole
Respiratory support
Urinalysis
ABGs, CBC
Hemoglobin (might be an indicator of internal bleeding!)

Spinal Cord Injuries: Emergency Management
Oxygenation and ventilation
Provide oxygen PRN
Shallow breathing → inadequate oxygenation → need for intubation & mechanical ventilation
Assume that there is a SCI until it is ruled out!
Rapid assessment, immobilization, extrication, and stabilization
Spinal (back) board + head and neck in neutral position
Movement could also cause damage to spinal cord that wasn't already there with bone fragments
Make sure someone is stabilizing the head specifically during movement or transport
No sitting up, no twisting & turning of the body
Transfer and movement:
Head blocks (as shown in picture)
Stays on transfer board
Once cleared by imaging & the extent of damage is known → can moved to traditional bed if harm, specialty bed or C-collar & firm mattress if no specialty bed available
Admission to intensive care unit (ICU)

Spinal Cord Injuries: Management in Acute Phase
Pharmacological Therapy
Norepinephrine, dopamine (treats hypotension)
Atropine (treats bradycardia)
Dextran (volume expander—helps with hypotension, but monitor for fluid overload)
Baclofen, dantrolene (reduces muscle spasticity; monitor for drowsiness and muscle weakness)
Bethanechol (helps with bladder spasticity; monitor for urinary retention)
Opioids, non-opioids, NSAIDs
Heparin (DVT prophylaxis)
Docusate sodium, polycarbophil
Hydralazine, nitroglycerin (treats episodes of hypertension)
Spinal surgery
Immobilization Devices & Traction
Halo Devices
Respiratory
Aggressive Pulmonary Toilet!
helping flush that gunk out of their body (cough assists, abdominal pressure, incentive spirometry (deep breathing)
Bowel & Bladder function
NPO
Neurogenic bladder
Spastic bladder: hypertonia (injuries above L1 - upper motor neurons) – frequent contractions → urinary incontinence
Flaccid bladder: hypotonia (lower motor neurons) – inability to contract → urinary retention
Ongoing neurological assessment
Muscle strength and tone
Range of motion exercises (passive and active)
Mobility
Family education
Psychological
Sexual function (education)
Skin
Hourly turns
Monitor for complications
Pneumonia and sepsis
Orthostatic hypotension

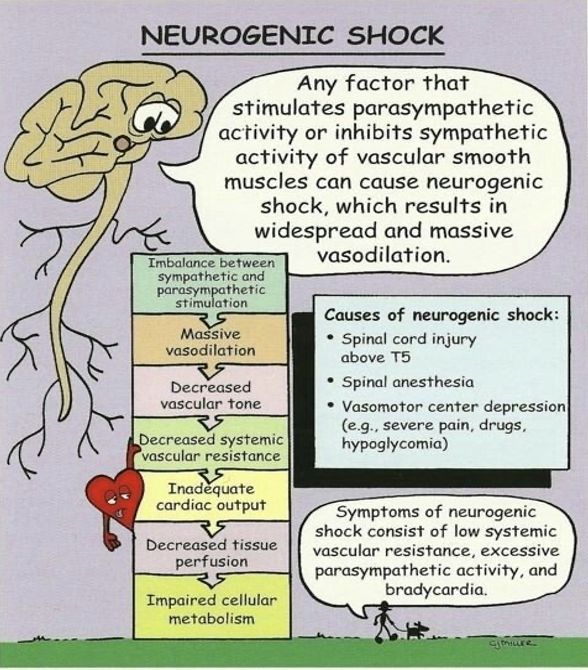
Spinal Cord Injuries: Acute Complications—Neurogenic Shock
Loss of muscle tone in blood vessel walls below the level of injury due to loss of communication within sympathetic nervous system. (affects the nervous system and is usually sustained)
Clinical Manifestations:
Hypotension
Bradycardia
↓ cardiac output ⟶ dependent edema, peripheral vasodilation, venous pooling
Loss of temperature regulation
Greater risk of developing venous thromboembolism (VTE)
Treatment: Vasopressors or atropine, IV fluids
Loss of temperature regulation - no sweating d/t sympathetic activity
Risk for abrupt onset of fever
Distributive shock - mass vasodilation → ↓ systemic vascular resistance → ABNORMAL DISTRIBUTION of blood flow → inadequate blood supply to tissues & organs
*T6 or above
Spinal Cord Injuries: Acute Complications—Spinal Shock
Sudden depression of reflex activity in spinal cord that happens below the level of injury d/t inflammation. (affects the spinal cord + temporary/reversible)
Clinical Manifestations:
Flaccid paralysis
Absent reflexes
Autonomic responses
Hypotension, bradycardia ⟶ more damage to spinal cord
Goal = maintain MAP > 85 mmHg
Paralytic ileus—can happen due to a lack blood flow
Mean arterial pressure - keep above 85 to avoid further damage
Paralytic ileus + bowel distention → depression of bladder & bowel function
Treated with intestinal decompression with NG insertion
Usually happens within 1st 2-3 days post injury and resolves within a week
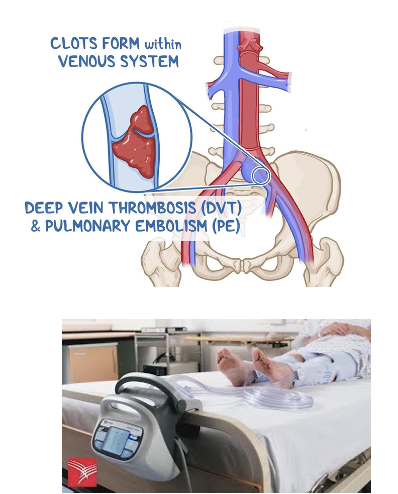
Spinal Cord Injuries: Acute Complications—Venous Thromboembolism (VTE)
Blood clot that develops in the venous vasculature that could develop into a DVT or PE
Greater risk d/t immobility, flaccidity, ↓ vasomotor tone
Presents as pleuritic chest pain, anxiety, shortness of breath, ↑PaCO2 (hypercapnia), ↓PaO2 (hypoxia)
Unilateral swelling, low-grade fever, temp change in affected limb
Prevention: low-dose anticoagulation therapy
Use of sequential pneumatic compressions (SCDs)
Permanent indwelling filters
Range-of-motion exercises
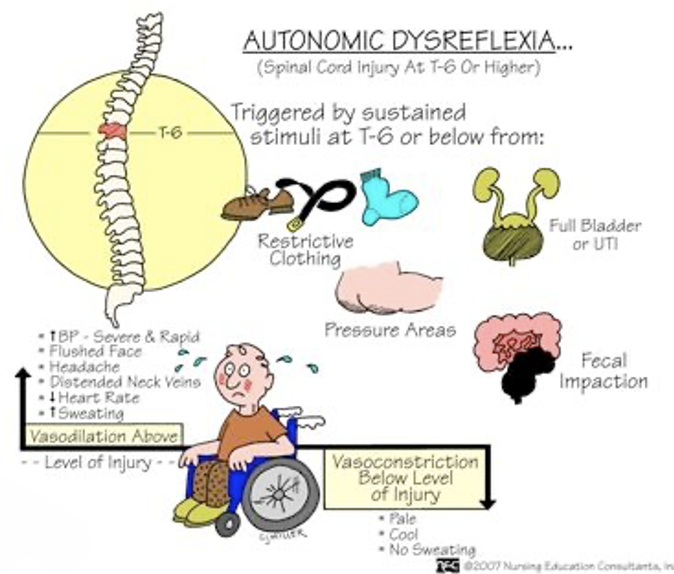
Spinal Cord Injuries: Acute Complications—Autonomic Dysreflexia
Life-threatening emergency in patients with SCI where exaggerated autonomic responses to stimuli that causes hypertensive emergency! (injuries @ T6 or above)
Clinical Manifestations:
Severe, pounding headache with paroxysmal hypertension
Profuse sweating above spinal level of injury
Nausea
Nasal congestion
Bradycardia
Stimuli could be: @ T6 or below
Distended bladder (most common)
Constipation, fecal impaction (distention of contraction of visceral organs)
Tactile pain, thermal pain, pressure injury (stimulation of the skin), ingrown toenail
Sexual stimulation, childbirth
Remove the stimuli & place patient immediately in sitting position to lower blood pressure
Loosen tight clothing
Spinal Cord Injuries: Continuous Management
Adjusting to life with a disability
Ongoing follow-up care
Complications indirectly related to SCI
Disuse syndrome
Bladder & kidney infections
Spasticity
Depression
Pressure Injuries

B. C4—The phrenic nerve, which is responsible for controlling the diaphragm, originates between C3-C5. Impairment of spinal nerves in that area can lead to paralysis of the diaphragm, resulting in respiratory failure. Mechanical ventilation would be necessary for proper oxygenation.
Injuries at or above which spinal level may result in a diaphragmatic paralysis that requires ventilator support?
A. T6
B. C4
C. L1
D. T12