[N109] Electrocardiography
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
Atrial / Ventricular / Ventricular
The P wave represents ________ depolarization, while the QRS complex represents ________ depolarization, and the T wave represents ________ repolarization.
Sino-atrial (SA) node
It is the heart’s physiologic or dominant pacemaker; center of automaticity and discharges an impulse between 60 and 100 times per minute
c) 60–100 bpm
The SA node is the physiologic pacemaker of the heart. What is its normal firing rate?
a) 20–40 bpm
b) 40–60 bpm
c) 60–100 bpm
d) 100–120 bpm
AV junction (40–60 bpm)
You see a rhythm strip with absent P waves and narrow QRS complexes at 45 bpm. Which pacemaker is likely in control?
AV junction (AV node and bundle of His) (40-60 bpm)
Ventricles (20-40 bpm)
Atria (80 bpm)
What are the potential pacemakers of the heart if SA node fails and their respective impulse?
False (they only record activity, no electricity delivered)
True/False:
ECG leads transmit small electrical currents into the patient’s body to stimulate the heart.
BONUS: Conduction system of the heart
The ECG's P-wave, QRS complex, and T-wave correspond to atrial depolarization (contraction), ventricular depolarization (contraction), and ventricular repolarization (relaxation), respectively.
Enumerate the sequence in the cardiac cycle and how each mechanical event corresponds to an ECG.
Lead
This provides a view of the heart’s electrical activity between one positive pole and one negative pole.
Electrodes; waveforms
_______________ placed on the skin measures the direction of electrical currents discharged by the heart. These currents are then transformed into _____________.
Deflection
This pertains to a wave or deflection seen on an electrocardiogram (ECG) that represents the electrical activity of the heart, specifically the movement of a depolarization or repolarization wavefront
When a wave of electrical activity moves towards a positive electrode on the ECG, it causes an upward (positive) deflection;
whereas movement away from it causes a downward (negative) deflection.
What is the main difference between the positive and negative electrodes in terms of deflection?
A bipolar lead system means that each displayed ECG lead has a positive and a negative pole. (one lead acts as a ground)
Explain the bipolar lead system in ECG.
FALSE: Leads do not transmit any electricity to the patient; they record electrical impulses.
True/False:
Leads have electricity that is transmitted to the patient which helps record the electrical impulses.
Plane
This refers to the cross-sectional prospective of the heart’s electrical activity.
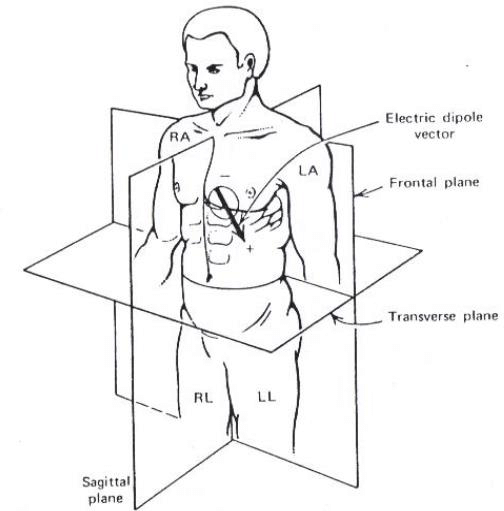
Frontal plane (picture ng puso mula sa harap)
Vertical cut through the middle of the heart, shows anterior to posterior view.
Horizontal plane (picture ng puso mula sa taas)
transverse cut through the middle of the heart, shows either superior or inferior view.
3-lead ECG placement
5-lead ECG placement
12-Lead ECG placement
Diluted plain alcohol with PNSS
cotton
wet the electrodes before placing them onto the patient
What is the specific solution used for the conduction system?
Place the lead nearest to the stump
Paano if phantom limb?
18-lead ECG
This lead ECG is usually used in pediatric patients due to anatomic differences
Dextrocardia (12-lead ECG is used)
This is a rare condition where the heart is positioned on the right side of the chest instead of the left.
Einthoven’s triangle
This is a theoretical triangle formed by placing electrodes on the right arm (RA), left arm (LA), and left leg (LL). These three points correspond to the locations of the limb leads in a standard ECG (leads I, II, and III).
identify indication (brief NHH)
Patient should be well-rested
Patient should avoid activities/food that affect heart activity (coffee, running, alcohol, etc.)
Minimize anxiety by saying to the patient na walang electricity na dadaloy sa patient
Remove metals in the patient’s body (generally no effect, but to secure no interruption in electric readings)
Enumerate at least two nursing considerations prior to performing ECG
Relaxed, extended extremities (dapat hindi nakadikit sa wall or sa railings), expose the area only, hindi nakadikit yung foot sa foot ng bed.
Diluted 75% alcohol and sterile water in cotton balls
Acts as liquid conductor and makes is more easier to place the suctions
Nursing responsibilities during ECG
No, unless ordered by the physician in special circumstances
Do you need to hold medications prior to ECG?
The lead is placed on the nearest left lower limb or on top of the slump
Where should the left lower lead be placed in patients with above the knee amputation?
BONUS: 12-lead placement
b) It follows the heart’s natural conduction pathway
Lead II is considered the most important monitoring lead because:
a) It best reflects lateral LV wall
b) It follows the heart’s natural conduction pathway
c) It shows anterior wall activity
d) It is least prone to artifact
ground
In Einthoven’s Triangle, the right leg electrode acts as a _________.
b) V1, V2 → V4 → V5, V6 → V3
Correct order for placing chest leads in a 12-lead ECG is:
a) V1–V6 in numeric order
b) V1, V2 → V4 → V5, V6 → V3
c) V1, V2 → V3 → V4 → V5, V6
0.04 sec / 0.20 sec
On ECG paper, 1 small box horizontally = ______ sec; 1 large box = ______ sec.
c) Bundle branch block or ventricular rhythm
A QRS duration of 0.14 sec (normal: 0.06-0.10 sec) indicates:
a) Normal ventricular conduction
b) Narrow complex supraventricular rhythm
c) Bundle branch block or ventricular rhythm
d) Artifact
AV block
A PR interval of more than 0.20 seconds indicate?
Wolff–Parkinson–White syndrome (pre-excitation)
A PR interval of less than 0.12 seconds indicates?
Ischemia or MI (ST segment should normally be flat)
What should you suspect if there is an elevation/depression of the ST segment?
Hyperkalemia
Peaked T wave may indicate?
Ischemia
Inverted T wave may indicate?
When the patient is in haloperidol with the risk for Torsades de Pointes
When should we strictly monitor the QT interval?
Normal: <0.44 sec (men), <0.46 sec (women)
What are the normal values of QT interval for men and women?
True
(True/False):
ST elevation in ≥2 contiguous leads is diagnostic for myocardial infarction.
Hypomagnesemia → Narrow PR interval (wrong; it prolongs QT → Torsades)
Which electrolyte imbalance matches the wrong ECG finding?
Hyperkalemia → Peaked T waves
Hypokalemia → Flattened T waves / U waves
Hypercalcemia → Short QT
Hypomagnesemia → Narrow PR interval
BONUS: ECG notes
P Wave (is there a P wave?)
Rhythm (Is the rhythm regular?)
Heart rate (compute)
PR Interval (is it constant? does it vary?)
QRS Complex (is it narrow <0.12 sec; or wide >0.12 sec?)
QT Interval (prolonged or normal?)
ST Segment (elevated, depressed, or isoelectric?)
T Wave (upright, peaked, or inverted?)
What are the steps in ECG interpretation? (RRPPRQRSSTQT)
0.12–0.20 / 0.06–0.10 / 0.44
Normal PR interval: ______ sec. Normal QRS: ______ sec. Normal QT: ≤______ sec.
Second-degree AV block, Mobitz I (Wenckebach)
You see progressive PR prolongation until a QRS is dropped. This is most consistent with:
b) Sinus bradycardia
A 25-year-old athlete has HR 45 bpm, regular rhythm, upright P waves before every QRS. Diagnosis?
a) Sinus tachycardia
b) Sinus bradycardia
c) Junctional escape rhythm
d) 1st-degree AV block
Ventricular fibrillation
Which rhythm is always pulseless?
Ventricular fibrillation
Pulseless VTach
Asystole
Supraventricular tachycardia
Sawtooth / Irregular chaotic
Atrial flutter shows ______ wave pattern, while atrial fibrillation shows ______ baseline.
Supraventricular Tachycardia (SVT)
Your patient’s ECG shows a rapid, narrow-complex tachycardia at 180 bpm, no visible P waves. What’s the most likely diagnosis?
b) Atrial fibrillation
Which arrhythmia carries the highest risk of stroke due to embolism?
a) Atrial flutter
b) Atrial fibrillation
c) Sinus bradycardia
d) PVCs
Narrow QRS
Which is not a PVC characteristic?
Wide QRS
Absent P waves
Narrow QRS
Can appear as bigeminy/trigeminy
b) V-tach
A run of ≥6 PVCs per minute may progress to:
a) Asystole
b) V-tach
c) Atrial flutter
d) Junctional tachycardia
QT / Magnesium
Torsades de Pointes is a polymorphic ventricular tachycardia usually caused by prolonged ______ interval, often due to low ______.
False (always pulseless)
(True/False):
Ventricular fibrillation can sometimes have a pulse.
a) 1st degree
Which AV block is described as “PR interval >0.20 sec, but every P followed by QRS”?
a) 1st degree
b) 2nd degree Mobitz I
c) 2nd degree Mobitz II
d) 3rd degree
Mobitz I (Wenckebach)
“PR progressively lengthens, then a QRS drops” = ______ AV block.
2nd degree AV block, Mobitz II
Your patient has constant PR intervals, but some P waves are not followed by QRS. Diagnosis?
3rd degree
Which block has no relationship between P waves and QRS complexes?
1st degree
Mobitz I
Mobitz II
3rd degree
c (Tall peaked P = right atrial enlargement)
Which of the following is NOT a sign of left atrial enlargement?
a) Notched P wave in lead II
b) Wide, biphasic P wave in V1 (terminal negative deflection)
c) Tall peaked P wave in lead II
d) P wave duration > 0.12 s
True
True/False: ST depression can represent myocardial ischemia OR reciprocal changes of an MI.
Anterior MI / Lateral MI / Inferior MI
ST elevation in V1-V4 → _______
ST elevation in V5-V6, I, aVL → _______
ST elevation in II, III, aVF → _______
b) Atrial fibrillation
Which rhythm is “irregularly irregular” with no P waves?
a) Atrial flutter
b) Atrial fibrillation
c) SVT
d) Junctional rhythm
c) Hypothyroidism
Which is NOT a cause of sinus tachycardia?
a) Fever
b) Anxiety
c) Hypothyroidism
d) Pain
Ventricular tachycardia
Wide QRS (>0.12 s), tachycardia, no P waves → ___________.
True
True/False: V-fib is shockable, but asystole is not.
a) atrial fibrillation
“Holiday Heart Syndrome” arrhythmia after binge drinking?
a) Atrial fibrillation
b) VT
c) Junctional rhythm
d) WPW
c (asystole → CPR + epi, NOT defibrillation)
Odd-one-out: Which rhythm requires IMMEDIATE defibrillation?
a) Ventricular tachycardia (pulseless)
b) Ventricular fibrillation
c) Asystole
d) Torsades de pointes (pulseless)
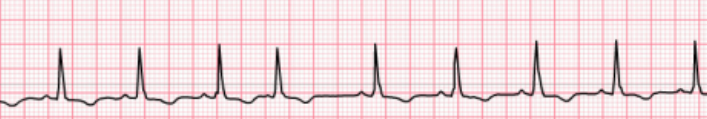
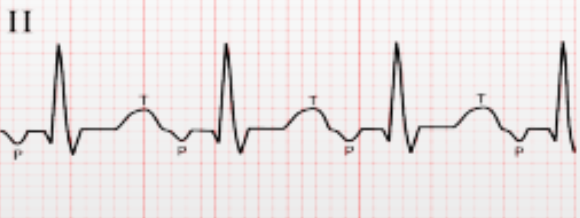
1st step: P wave present
Each P wave has QRS complex
2nd step: Regular
3rd step: 75 HR
1500 / 21 = 71.429 or 72 bpm
4th step: 0.12 seconds (normal)
PR interval
4 x 0.4 = 0.16
5th step: 0.04 seconds
QRS duration
1 x 0.04 = 0.04
6th: 0.4 seconds
QT interval
9 x 0.04 = 0.36
7th: slightly depressed
INTERPRETATION: Normal sinus rhythm with a heart rate of 75 BPM, slightly slightly depressed ST segment, and upright T-wave
Interpret the ECG strip:
Sinus bradycardia
A slower-than-normal heart rate, usually <60 bpm, but rhythm remains regular
SLOW RATES (From Registered RN)
Sick Sinus Syndrome (SA Node damaged)
Low Thyroid Hormone
Older Adult
Weak/Damaged Heart Muscle
Raised ICP (Part of Cushing’s Triad)
Athlete
Toxicity (beta-blockers, calcium channel blockers, clonidine, digoxin)
Electrolyte imbalance (hyperkalemia)
Stimulation of vagal response
Causes
Can occur naturally in athletes, during sleep, or due to increased vagal tone.
Also caused by medications (beta-blockers, calcium channel blockers)
Hypothyroidism
Hypothermia
Associated Conditions: Often benign but may lead to dizziness or fatigue if too slow. Common in well-conditioned individuals, but can indicate issues in older adults.
Treatment
If asymptomatic:
Does not have any treatment
Assess signs and symptoms
If symptomatic
Medications (ADE)
Atropine
Dopamine
Epinephrine
Temporary pacemaker
Determine the sinus node arrhythmia:
slower-than-normal heart rate, usually <60 bpm, but rhythm remains regular

A faster-than-normal heart rate, usually >100 bpm, with regular rhythm.
Causes
Often due to exercise, stress, fever, pain, dehydration, anemia, or stimulants like caffeine.
Also seen in hyperthyroidism and heart failure.
From Registered RN (TACHY HEARTS)
Temperature elevation
Aerobic exercise
Cardiac disease
Hyperthyroidism
Yelp
Hemorrhage (Hypovolemic Shock)
Associated Conditions: Usually a normal response to stress or exercise, but chronic tachycardia can indicate a compensatory mechanism for conditions like heart failure or hypovolemia.
Determine the sinus node arrhythmia:
A faster-than-normal heart rate, usually >100 bpm, with regular rhythm.

Sinus arrhythmia
Determine the sinus node arrhythmia:
abnormal rhythm and irregular

Sinus arrest/block
Determine the sinus node arrhythmia:
Sinus node stops resulting in a missing beat. Rhythm is irregular

Normal sinus rhythm with occasional premature atrial complex
Premature atrial complex
Premature = occurred earlier than usual
May P wave
Comes from atrial origin kaya premature atrial complex
Ventricular complex = walang P wave, QRS is wide
Problems lies within the T wave
Normal sinus rhythm with occasional premature atrial complex
Isearch → PQRST cardiac cycle
Interpretation: Normal sinus rhythm with heart rate of _ with occasional atrial premature complex
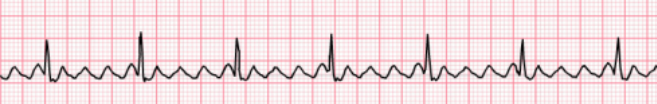
Determine the atrial dysrhythmia
Wandering atrial pacemaker
P waves ay different yung presentation every PQRST which makes it wandering
WAP (60 to 100/100)or MAT (>100/100)- difference is the rate
Does not happen usually sa mga pasiyente (at most 2 pa lang na-eencounter ni sir)
Mosty atrial tachycardias are irregular in nature
Atrial contractions ay paiba-iba, irregular
Less than 60 bpm
60-100 kasi kapag more than 100 = multifocal atrial tachycardia
Determine the atrial dysrhythmia:
Different presentation of P waves every PQRST
Multifocal atrial tachycardia
P waves ay iba iba ang shape and more than 100 rate
More than 100 bpm
Multifocal kasi iba-iba ang focus ng atria kasi wandering
Irregular
Tapos more than 100 bpm
6-second strip ang pang-measure kasi irreg
Determine the atrial dysrhythmia:
Different P wave shapes with more than 100 bpm rate, irregular

Atrial Tachycardia
120-250 bpm
Regular unless may variable
Compared to WAP and MAT, ito ay tachy arrhythmias that are 120-250 bpm pero regular rhythm
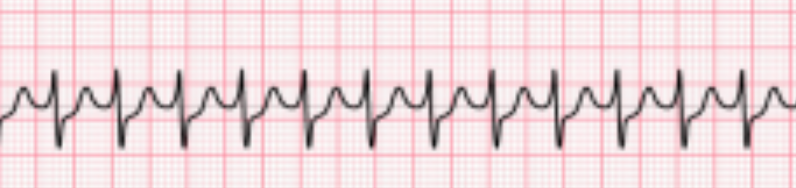
Determine the atrial dysrhythmia:
Atrial rate is 120-250 bpm, regular unless there is a variable block at the AV node; P waves with different shapes, precedes each QRS complex but may be hidden in preceding T wave.
Atrial Flutter
Usually regular in nature compared to atrial fibrillation which has small S waves and is irregular
Big letter F wave, saw like patterns
Defined and regular
4:1 / 3:1 - P to QRS
Mataas atrial rate - F waves ang counting
Galing ang problem sa atrium (big F waves)
Saw tooth pattern
There is a ratio of P to QRS (2:1 dapat)
Pero this is 4:1 or 3:1
Mas konti atrial rate compared sa A-Fib
Determine the atrial dysrhythmia:
Usually regular in nature compared to atrial fibrillation which has small S waves and is irregular; with big letter F waves that are in saw-like patterns; atrial rate varies between 250-350 bpm, most commonly 300.
Atrial Fibrillation
Small and erratic / irregular rhythm: F waves (Fibrillation)
400 to 600 p waves
Dahil irreg, ang ventricular rate ay normal lang
Pero ang atrial rate ay umaabot ng 40-60 x 10 = 400-600
Common in the area, not effective yung pagpupuno ng heart chambers
Irregular compared sa Aflutter
At risk:
Embolic stroke
Hindi maganda ang pagkaka-pump ng blood kaya there is possibility of embolism
We give:
Blood thinners
Digoxin (anti-arrhythmia)
Pulse is reflection of ventricular heart rate
Mahalaga malaman ang ventricular rate ni px lalo na if naka-Digoxin siya
Kapag 50 bpm na lang ang ventricular rate ni px, huwag ibibigay muna ang Digoxin → dec HR (dahil anti-arrhythmia nga) = REFER to adjust dose
We don’t stop abruptly
Wean off din
Determine the atrial dysrhythmia:
Atrial rate is 400-600 bpm or faster, irregular, with the marked irregularity of the ventricular response. P waves not present while atrial activity is chaotic with no formed atrial impulses visible. Small and erratic with F waves that vary in size from coarse to very fine.
Atrial fibrillation with slow ventricular response
This type of atrial fibrillation has:
Slow ventricular response → brady → systole → cardiac arrest
Below 60 QRS
Atrial fibrillation with controlled ventricular response
This type of atrial fibrillation has 60-100 QRS
Atrial fibrillation with rapid ventricular response
This type of atrial fibrillation has:
> 100 QRS
Supraventricular tachycardia
Identify the Above A-V Arrhythmia:
above 150s-170s HR
burrowed P waves (no atrial depolarization)
narrow QRS complex
Premature junctional rhythm
*Inverted P wave
Determine the Junctional dysrhythmia:
rate: 60-100 bpm
rhythm is regular except for occurrence of premature beats
P waves are usually inverted; may occur before, during, or after the QRS complex of the premature beat

Premature ventricular contractions
Prematurely occurring
QRS complex wide
No P-waves
Unlike PAC and PJC, may P waves kasi both galing sa atrial origin
Ito ay VENTRICULAR origin
Kaya ventricular contraction ang problem
Commonly seen sa patients because sa QRS
From the ventricles, QRS complexes are wide → more than 0.1
Walang P-wave
They have wide QRS complexes
Determine the ventricular dysrhythmia:
Rate is 60-100 bpm
Rhythm is irregular due to the early beats
QRS complex is wide and “bizarre” or “weird”; > 0.10 second in duration, varying in morphology (size, shape)
Every second → Bigeminy
Every third → Trigeminy
Every fourth → quadrigeminy
Dumadami ang PVC – occasional
Identical (magkamukha) → Unifocal
Different appearance (magkaiba ang itsura; inverted, upright) → Multifocal
two → Couplet
three → Triplet
four → Quadruplet
more than four → Runs of PVCs
Naming of PVCs:
Every second →
Every third →
Every fourth →
Dumadami ang PVC →
Identical (magkamukha) →
Different appearance (magkaiba ang itsura; inverted, upright) →
two →
three →
four →
more than four →
Run the code already, 6 max lang PVCs in 1 minute.
E-cart, code for ACLS → clinical forethought, plan, recommend.
It may lead to Vtach
What should the team do if there are runs of PVCs or with more than 6 PVCs per minute?
Ventricular tachycardia
VTACHS
First thing to do is to check for pulse (pwedeng may pulse, pwedeng wala)
Pulse rate!!!
Can be
Monomorphic
Iisa yung shape
Polymorphic
Iba-ibang shape
Most common: Torsades de Pointes
Can be
Pulseless
(unlike V-Fib, laging pulseless)
With pulse
Determine the ventricular dysrhythmia:
Ventricular rate is faster than 100 bpm
can be monomorphic or polymorphic
can be pulseless or with pulse
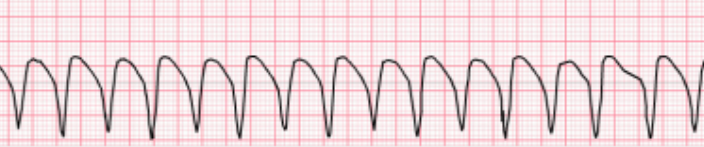
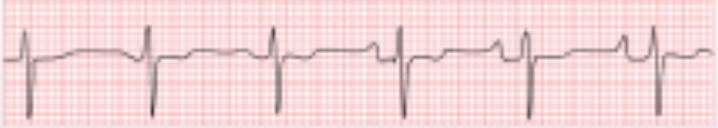
Torsades de Pointes
QT interval is lengthening → VTachs sa pic sa baba (hypomagnesemia)
Name based on morphology
Same and uniform shape - monomorphic
Polymorphic VTachs - Sample torsades de pointes (TDP), malalaking QRS complexes
Interventions: MgSO4, magnesium sulfate
TDP patients often have hypomagnesemia
Determine the ventricular dysrhythmia:
potentially fatal type of polymorphic ventricular tachycardia (a rapid, irregular heart rhythm)
QT internal is lengthening
QRS complexes appear to twist around the ECG baseline, a sign of a prolonged QT interval
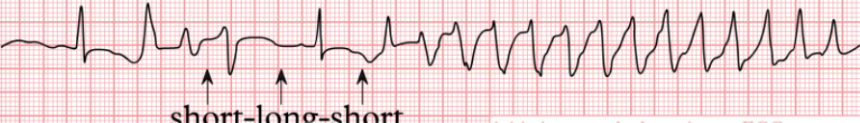
Magnesium sulfate (they often have hypomagnesemia)
What should you prepare for patients with torsades de pointes?
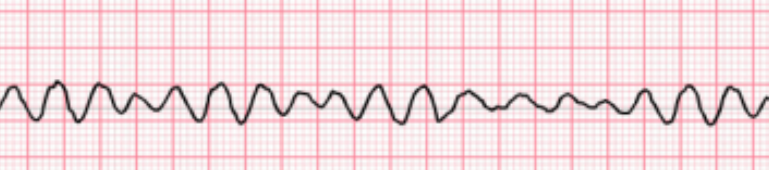
Ventricular fibrillation
Puro QRS complexes
ALWAYS PULSELESS
Unlike vtach which can either be pulseless or with pulse
Fine
Coarse - higher
V-Fib may appear like V-Tach minsan pero sa V-Tach may monomorphic pattern
V-Fib paiba-iba ang shapes
V-Fib → no pulse → cardiac arrest
Do cardiac arrest algorithm
Pulseless electrical activity (PEA)
normal sinus rhtyhm, no pulse
Run cardiac arrest algorthim
Mostly in patients na may hypovolemia, sepsis
Give fast drip PNSS to elevate the blood volume
Determine the ventricular dysrhythmia:
Rate is rapid, uncoordinated, and ineffective
Rhythm is chaotic and irregular
P waves: none
Always pulseless
Ventricular Asystole
Assess the patient first
Check the leads first
Baka na-disconnect lang naman
HUWAG KA MAG CARDIAC THUMP AGAD BHIE
Determine the ventricular dysrhythmia:
Flatline
No rate, rhythm, PR interval, QRS complex
First degree AV block
Kaya mahaba ang PR interval - atrial ventricular depolarization.
7 x 0.4 = 0.28 (mas mataas sa 0.2 secs so prolonged)
Mukhang normal pero mas mahaba pala
May delay sa AV conduction, may “block”
Mgt: Transcutaneous pacing
Determine the A-V dysrhythmia (blocks):
Prolonged PR interval (above 0.20 second)
Rate can occur at any sinus rate, usually 60-100 bpm
P waves are normal, precede every QRS

Second degree AV block: Mobitz Type 1 or Wenckebach
Both type 1 and 2 have drops.
Increasing prolonged PR interval → Then drop
Gradual increase / prolong tapos biglang drop
Mgt: Transcutaneous pacing
Determine the A-V dysrhythmia (blocks):
Increasing prolonged PR interval → Then drop
Rhythm is irregular, overall appearance of the rhythm demonstrates “group beating”
P waves are normal, some P waves are not conducted to the ventricles, but only one at a time fails to conduct to the ventricle
PR interval gradually lengthens in consecutive beats. The PR interval preceding the pause is longer than that following the pause

Second degree AV block: Mobitz Type 2
Prolonged-same-prolonged-same- drop of QRS (PR interval length
Mgt: OR agad kasi need ng transvenous pacing
Mas masakit daw Type 2
Consistent tapos bigla kang iiwan (jan naman kayo magaling)
Type 1 may buildup so medyo sanay ka na, pawala na bago ma-drop
Determine the A-V dysrhythmia (blocks):
Prolonged-same-prolonged-same- drop of QRS (PR interval length
Rate can occur at any basic rate
Rhythm is irregular due to blocked beats
P waves are usually regular and precede each QRS
PR interval is constant before conducted beats. The PR interval preceding the pause is the same as that following the pause
QRS complex is usually wide due to associated bundle branch block

Third degree AV block
Wala ng relationship yung drops and the PR interval
Mgt: Transvenous pacing
Determine the A-V dysrhythmia (blocks):
Atrial rate usually normal; ventricular rate is <45 bpm
rhythm is regular
P waves are normal but dissociated from QRS complexes