clinically important gram + bacteria II
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
streptococci
diverse group of organisms
may different streptococci may normally colonize mucosal membranes
predominant component of respiratory, GI and genital tract
many of low virulence
however may also invade normally sterile body sites, causing significant disease
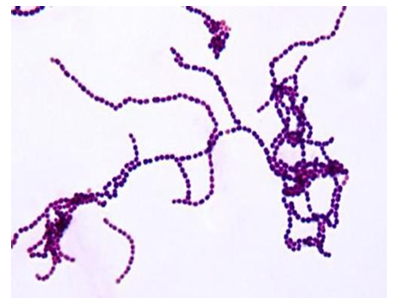
genus streptococci
gram positive cocci that may be in chains or pairs
optimal growth on media supplemented with blood
most are facultative anaerobes - will grow both aerobically and anaerobically
some are strict anaerobes - will only grow in the absence of oxygen
catalase negative - used to differentiate streptococci (also gram positive coccus)
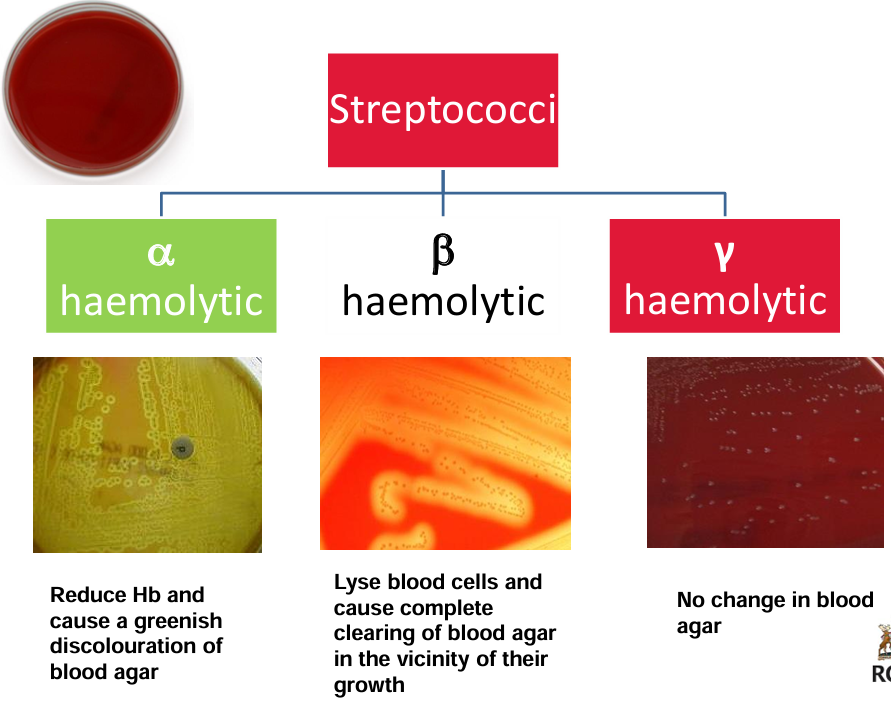
may cause haemolysis
classification
many different streptococci - useful to classify them to aid identification of them
most commonly used classification systems:
based on their on blood-containing agar (hemolysis)
based on antigens contained in their cell walls (Lancefield classification)
molecular classification (newer) - based on emm gene
some clinically important streptococci often referred to by both Lancefield group and hemolysis pattern
Lancefield classification
serological system of grouping streptococci, based on specific antigens present in their cell walls
group A-G of most clinical significance - except for group D, all are also beta hemolytic
basis of test:
antibody/antigen reaction
positive if agglutination is detected
clinically important streptococci
Strep. pyogenes (group A, beta hemolytic)
Strep. agalactiae (group B, beta hemolytic)
Strep. pneumoniae (alpha hemolytic)
viridians streptococci (alpha hemolytic)
enterococci (group D, beta or non hemolytic)
Pepto streptococcus (anaerobic or non-hemolytic)
streptococcus pyogenes
beta hemolytic streptococci that possess the Lancefield gorup A antigen
one of the most virulent of the streptococci species. Large range of clinical presentations. Pyogenic/suppurative (resulting in pus): pharyngitis, scarlet fever, erysipelas, cellulitis, toxic shock syndrome, pneumonia
non-suppurative: post-infectious immune-mediated complications
rheumatic fever
glomerulonephritis
group of streptococci: epidemiology
commonly colonize the oropharynx of children and young adults
transmission via droplets
colonization is transient: influenced by acquired immunity and competition from other organisms in the oropharynx
are the major cause of bacterial pharyngitis: crowding e.g. at day-care centers and schools, facilitates spread
streptococcus pyogenes toxins and virulence factors
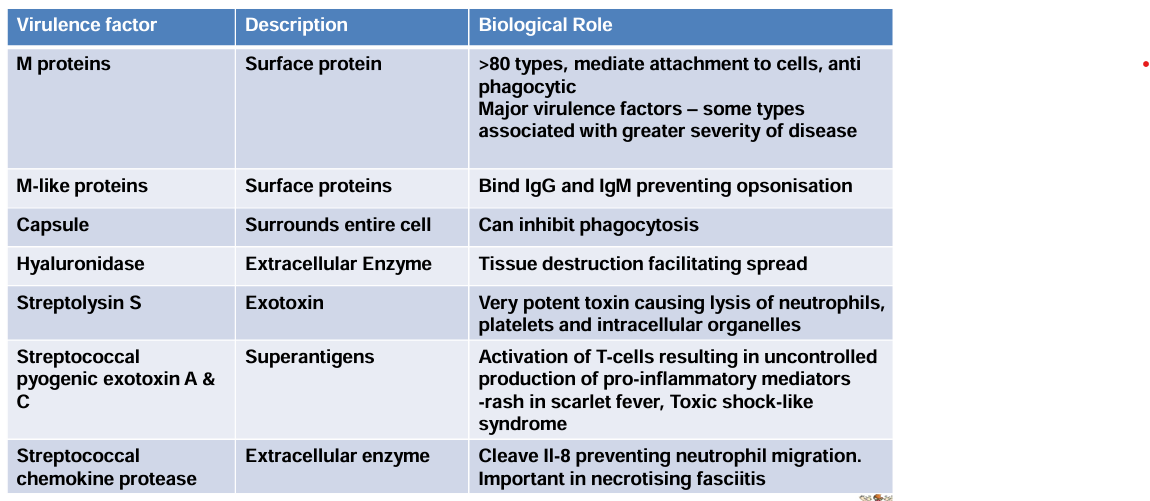
streptococcal pharyngitis
one of the most common bacterial infections of childhood
occasionally due to group C or group G
person-to-person spread by droplets of saliva or nasal secretions - facilitated by overcrowding
incubation period 2-4 days
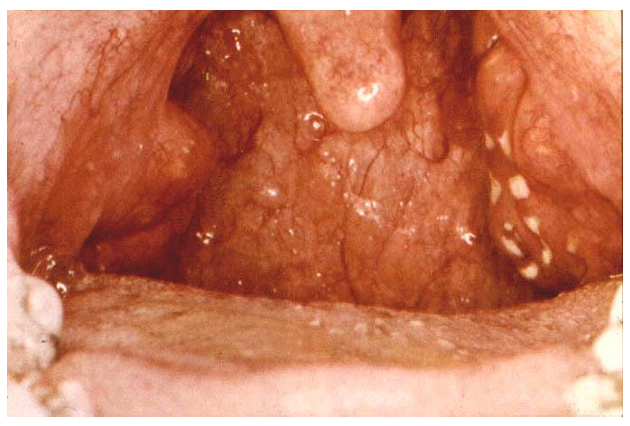
streptococcal pharyngitis clinical features and diagnosis
history: patient complains of sore throat, fever, headache, nausea and vomiting
examination: redness, oedema, lymphoid hyperplasia, enlarged tonsils with exudate, enlarged tender lymph nodes, fever
lab findings: positive throat culture, immunological (antibody) response
scarlet fever
occurs when group A streptococcal strain is lysogenized by a bacteriophage (bacterial virus( that stimulates production of pyrogenic toxin
pharyngitis + rash
scarlet fever complication
supportive complications include: otitis media, acute mastoiditis
non suppurative sequelae include: acute glomerulonephritis, acute rheumatic fever
main reason for antibiotic treatment is to prevent rheumatic fever - appropriate antibiotics include oral amoxicillin or oral clarithromycin if allergic to beta lactams
rheumatic fever and glomerulonephritis
post streptococcal auto immune complications
affect a minority of people who have group A streptococcal infection
type III hypersensitivity reaction
development of antibodies to some fraction of the organism
in rheumatic fever, the antibodies cross react with cardiac tissue → immune complex deposition on the heart
in post streptococcal glomerulonephritis, immune complexes are deposited on the glomerular basement membrane
acute rheumatic fever
associated with streptococcal pharyngitis but not with streptococcal skin infections
fever, joint pains and carditis - may also get neurological involvement (Syndenha’s chorea)
with recovery affected heart valves become thickened and deformed - antibiotic prophylaxis required if undergoing procedure that may put patient at risk of endocarditis
diagnosis is based on the jones criteria
acute glomerulonephritis
associated with streptococcal pharyngitis and sometimes with streptococcal skin infections
the patient develops oedema, puffy face, swollen extremities (due to sodium and water retention)
hypertension, with albumin and blood in the urine
majority of young patients recover completely but may lead to permanent renal damage
erysipelas
acute onset of symptoms with systemic manifestations including fever and chills. Skin is raised and differentiated from uninvolved skin
treat with oral benzylpenicillin (5-7days). if penicillin allergy, 1st gen cephalosporin or a macrolide cold press, hydration

necrotizing fasciitis
blistering, skin discoloration due to necrosis, destruction of skin, subcutaneous and peri muscular fat with necrotic liquefaction of fatty tissue. 20-4-% mortality
once culture is confirmed, treat with high dose IV benzylpenicillin (7-10 days). surgical debridement

streptococcus agalactiae
group B beta hemolytic streptococci
colonize the lower gastrointestinal tract and the genitourinary tract
different serotypes based on capsular polysaccharides; types 1a, 111 to V are most commonly associated with colonization and disease
important cause of neonatal sepsis. Risk factors: maternal colonization, premature delivery, prolonged rupture of membranes, intra partum fever
alpha hemolytic streptococci
viridians streptococci
streptococcus pneumoniae
viridians streptococci
present in oropharynx, GIT and genitourinary tract - normal flora
invasive disease often related to breech in mucosal surfaces
several associated with:
dental caries (strep. mutans)
ineffective endocarditis (strep. mitis, strep. bovis)
brain and liver abscesses (strep. anginosus)
most lack Lancefield antigens
species identified based on biochemical tests
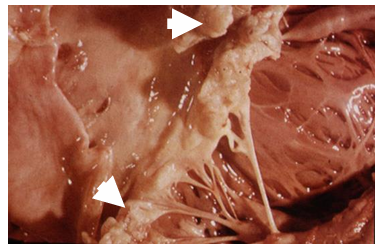
ineffective endocarditis
vegetation on heart valve
drug choice depends on:
causative pathogen
presence of prostheses
drug allergy history
renal function
risk of MDR organism
social history i.e. IV drug use
combination of antibiotics usually required for 4-6 weeks
usually IV amoxicillin + gentamicin for IE caused by alpha-hemolytic streptococci
streptococcus pneumoniae
gram positive cocci in chains or diplococci
carried in the nasopharynx
polysaccharide capsule > 90 serotypes.
allow typing strains
vaccines available against some serotypes
pathogenesis of bacteria
portal of entry colonizes oropharynx mediated by adhesin
attach to cells
defeat/evade immune system: risk factors - immunodeficiency, splenectomy. antibiotic resistance facilitates disease
cause damage to host cells: pneumolysin and cell wall polysaccharide activates complement and cytokine release
get out and spread further: direct person to person via respiratory droplets
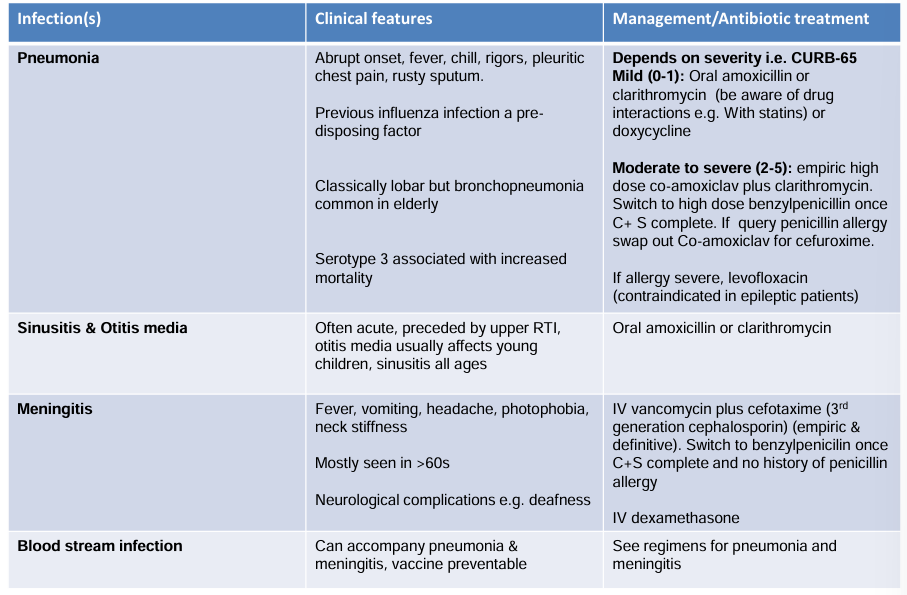
pneumonal infections and management
enterococci
previously classified as group D streptococci; typically seen in short chains on gram stain
facultative anaerobes
hemolytic pattern varies .. alpha or beta
grow in presence of bile salts i.e. grow on Mac Conkey agar
18 species in this genus
commensals with low virulence - bowel flora
enterococcal infection at risk patients
recent surgery
underlying disease - malignancy, burns or trauma
recent antibiotics - cephalosporins or aminoglycosides
prolonged hospitalization especially in ICU
enterococci infection clinical syndromes
urinary tract infection
endocarditis
bloodstream infection
wound infections and intra abdominal infections
important nosocomial pathogen
vancomycin resistant enterococci
problematic, particularly in hospital acquired infection
patients may become colonized ± develop significant infection due to VRE
limited treatment options - linezolid
listeria monocytogenes
gram positive bacillus, non sporing, aerobe/facultative anaerobe
transmitted by animal contact, drinking contaminated milk, eating certain soft cheeses, pate etc.
local epidemics have been associated with this
vertical transmission from mother to fetus
perinatal listeriosis
influenza like illness - usually in 3rd trimester. Fever, myalgia, backache, headaches, arthralgias
perinatal infection may result in: miscarriage or intrauterine death, premature labor and infected infant, neonatal listeriosis
can cause pneumonia, infective endocarditis, blood stream infection in immunocompromised individuals also
treatment: high dose amoxicillin plus gentamicin. resistant to cephalosporins
bacillus anthracis - causes anthrax
commonly found in soil
infection often seen in farm workers and those working with untreated leather and wool
infection depends on route of exposure i.e. wound, inhaled or gastrointestinal
anthrax toxin: 3 components - protective antigen (PA), edema factor (EF), lethal factor (LF). latter two components have enzymatic activity interfering with cAMP levels effecting water homeostasis
can be treated with antibiotics (oral doxycycline or ciprofloxacin) and antitoxin to neutralize toxin
vaccine available
