OPP Semester 2 Exam 1 (study all the other sets too rip)
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
SUE
Method for treating lumbar extension dysfunctions
S = Sims
U = Up
E = extension
What does the U in SUE stand for
The dysfunction side is up and the pt is pushing up
SUE in action
Ex: L5 E RL SL
Have the pt lay on their right side
Have them hug the table (Sims)
Monitor L5 with your hand
(you sit down now!)
Extend their legs and take them off the table
Place your hand on the top of their ankles
Have the pt push up while you push down
Relax, repeat, passive stretch
FDR
Method for treating lumbar flexion dysfunctions
F = flexion
D = down
R = lateral recumbent position
What does the D in FDR stand for?
the dysfunction side is down and the pt pushes down
FDR in action
Ex: L5 F RL SL
Have the pt lay on their left side
Bend their knees to see how the lumbar segment below moves, keep your hand there
Ask them to put their back to the table/chest up (lateral recumbent)
(You keep standing!)
Extend the left leg into the air off the table, and grab underneath the ankle of the right leg
Have the pt push their ankle down while you push up
Relax, repeat, and passive stretch
Type 1 Group Curve treatment
used for neutral lumbar dysfunction
NSDB
N = neutral
SD = side bent down
D = pt pushes down
B = both legs
Type 1 Group Curve treatment in action
Ex: L5 N SL RR
Have the pt lay with their side bent position down (here their left side will be down)
Monitor their L5
Move both their legs off the table, placing your hand underneath their ankle
Have the pt push down while you push up
Relax, repeat, passive stretch
What can cause lumbopelvic pain?
Insufficient stability in the sacroiliac joint
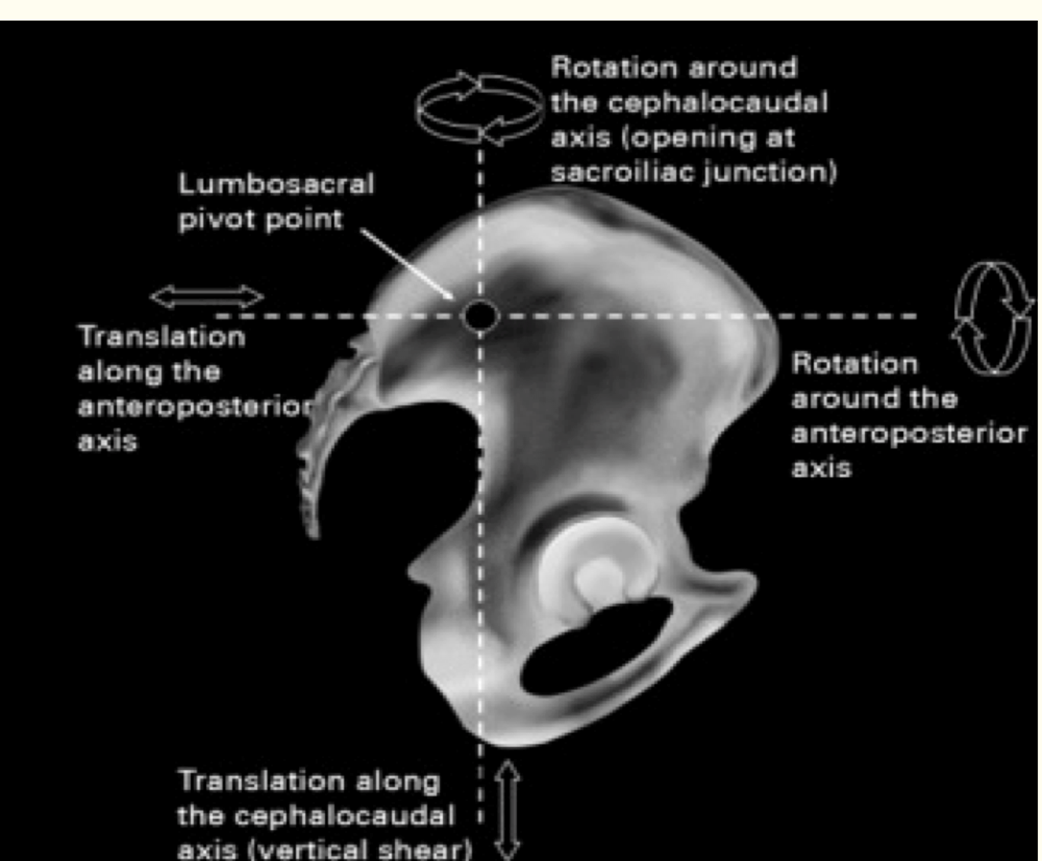
How does the sacroiliac joint move in flexion and extension?
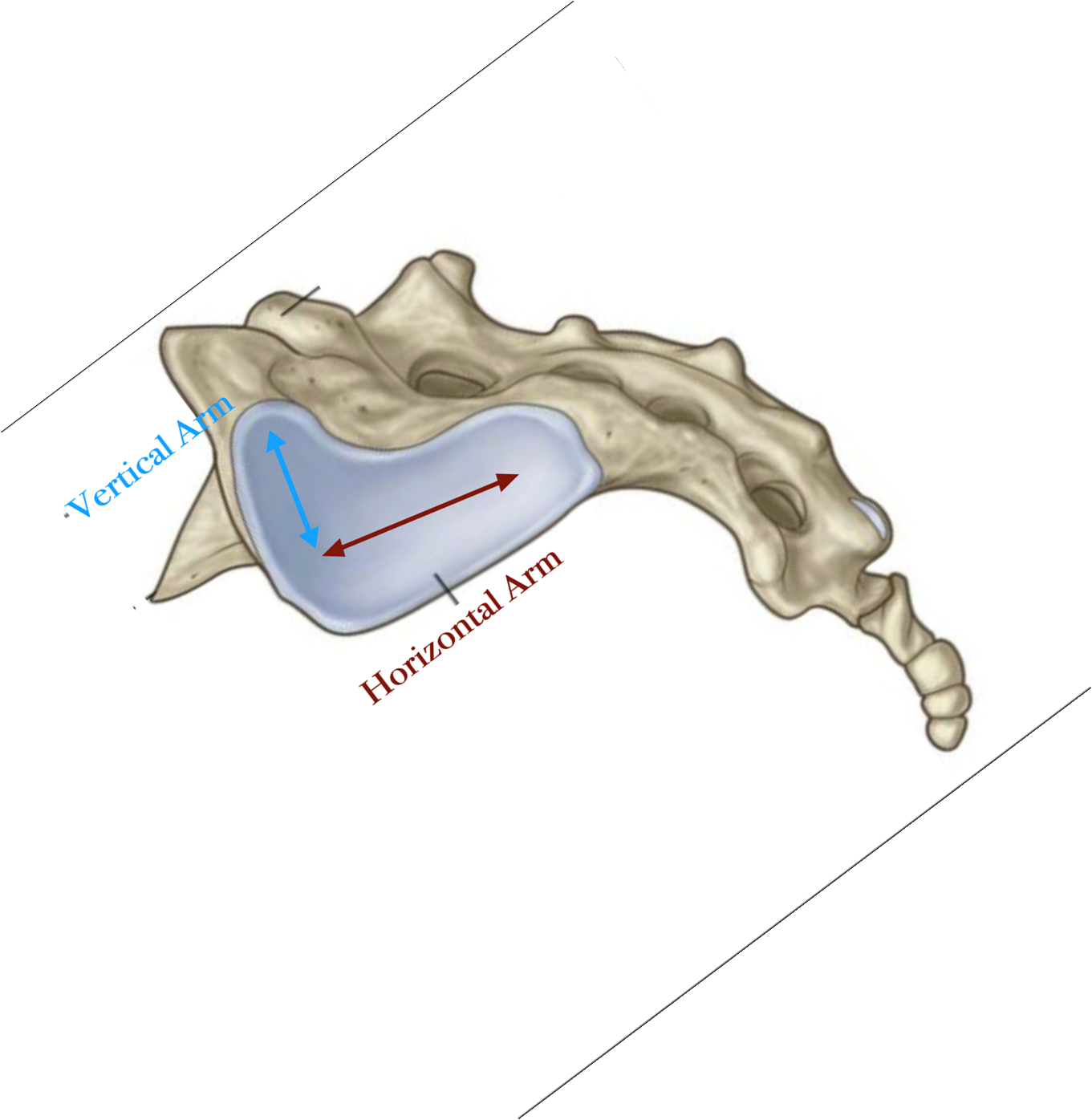
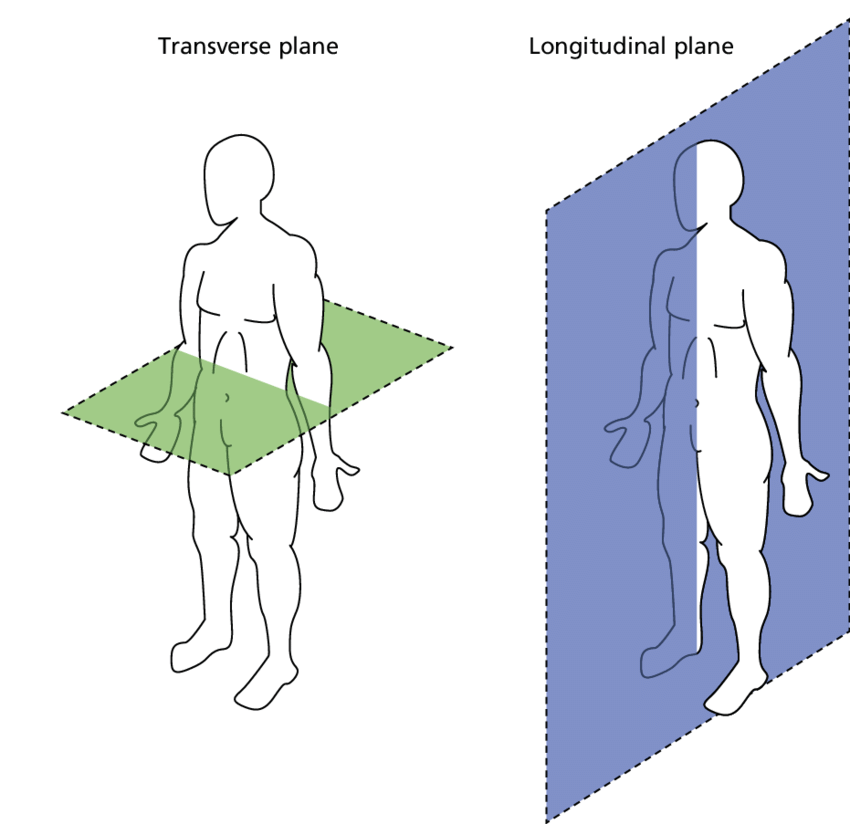
Moves around 2 degrees around a transverse axis at S2 in a sagittal plane
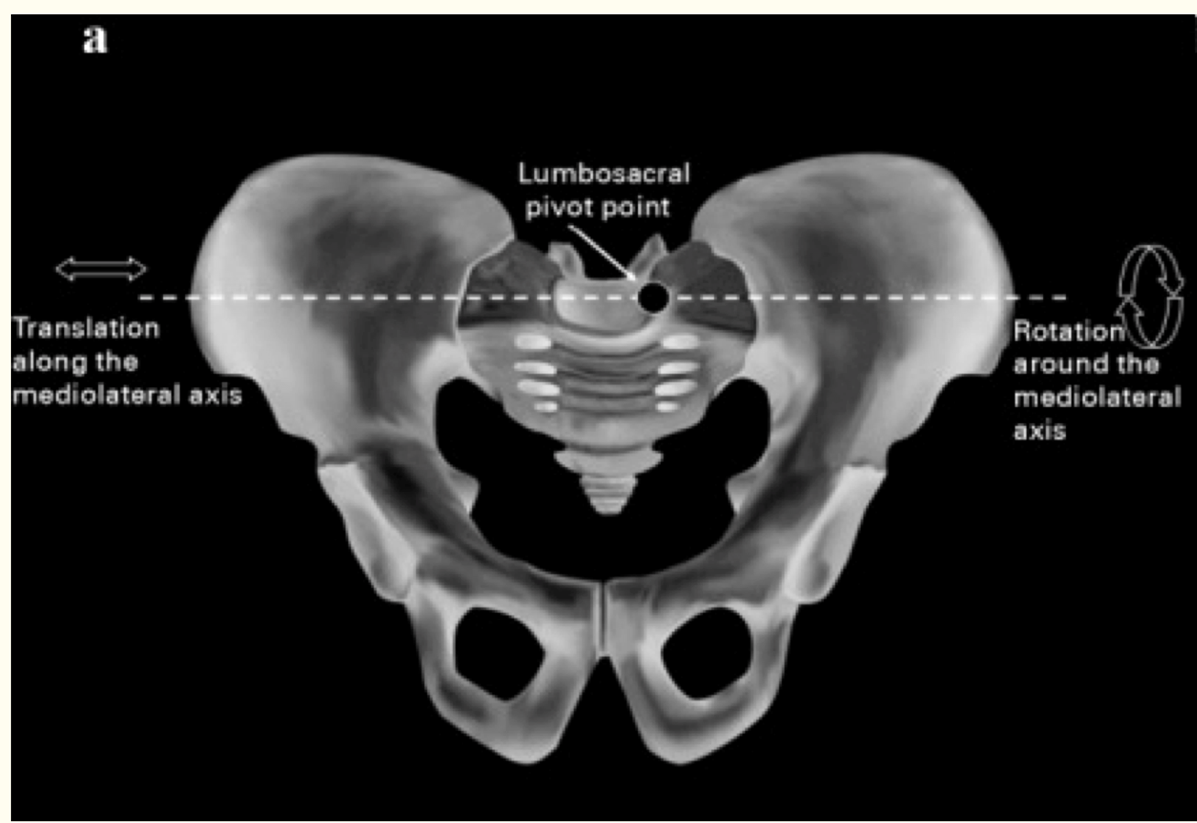
How does the sacroiliac joint move in rotation?
Moves around 1.5 degrees around a vertical axis in a transverse plane
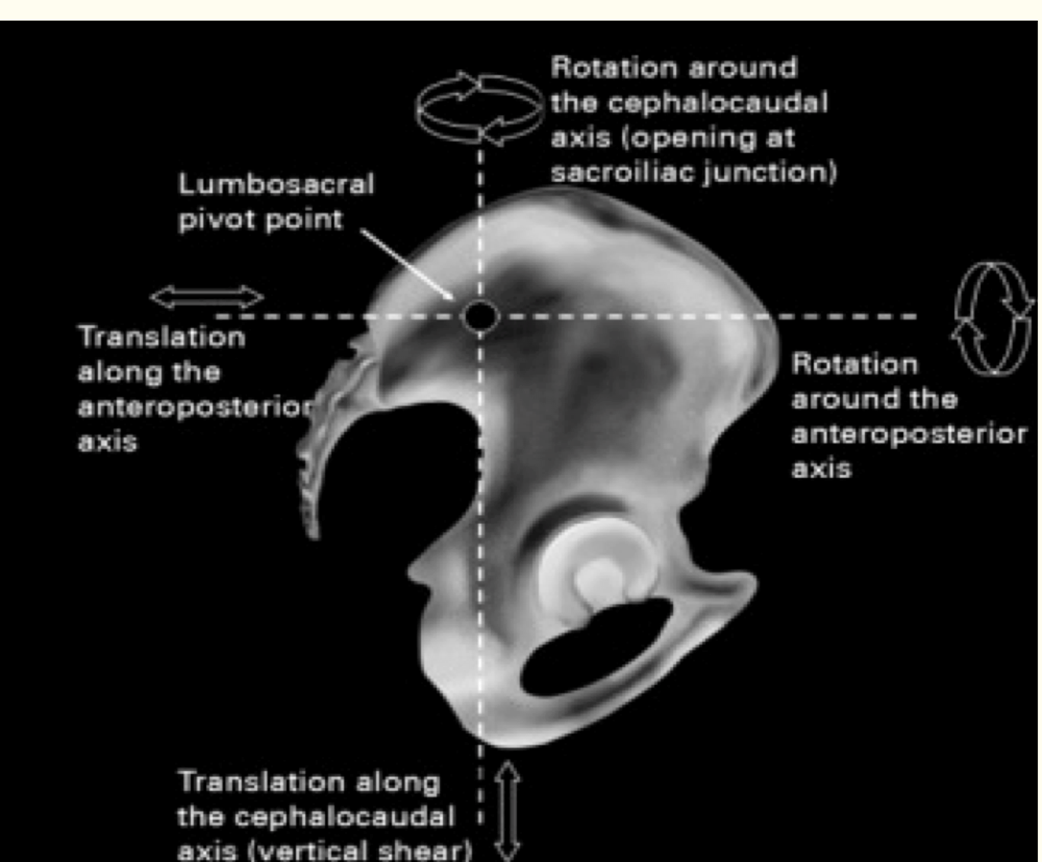
How does the sacroiliac joint move in side bending?
Moves around 0.8 degrees around an anteroposterior axis in a frontal/coronal plane
Nutation
flexion of the sacrum relative to a posterior rotation of the ilia
How to remember nutation?
Nodding = nutation
Sacral base vs apex
Base at the top
Apex at the bottom
Like the heart!
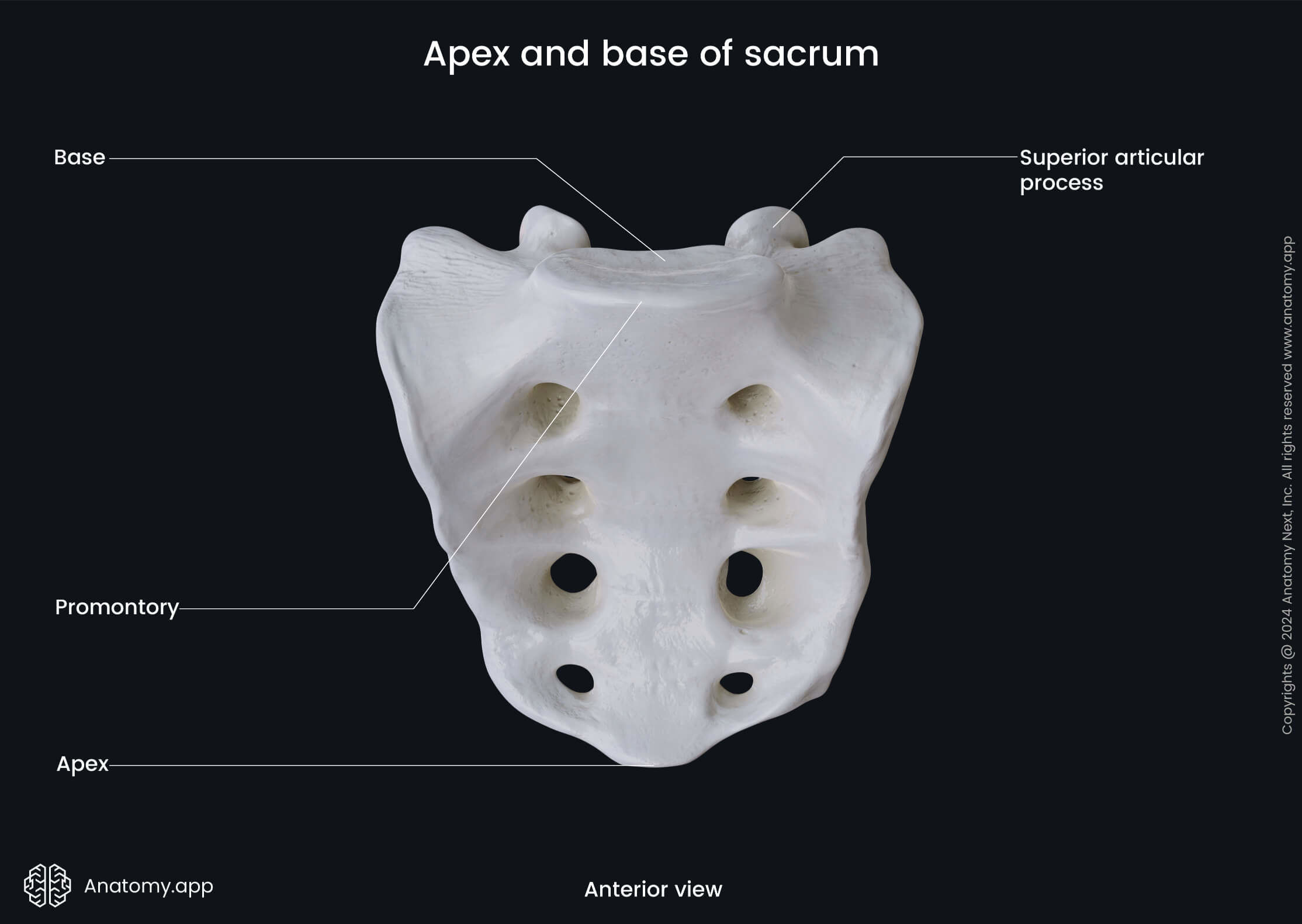
How does the sacral base move in nutation?
The sacral base moves both anteriorly and inferiorly in the sagittal plane on the middle transverse axis located at S2 in a nutation
How does the sacral apex move in nutation?
The apex of the sacrum will move both superiorly and posteriorly in nutation
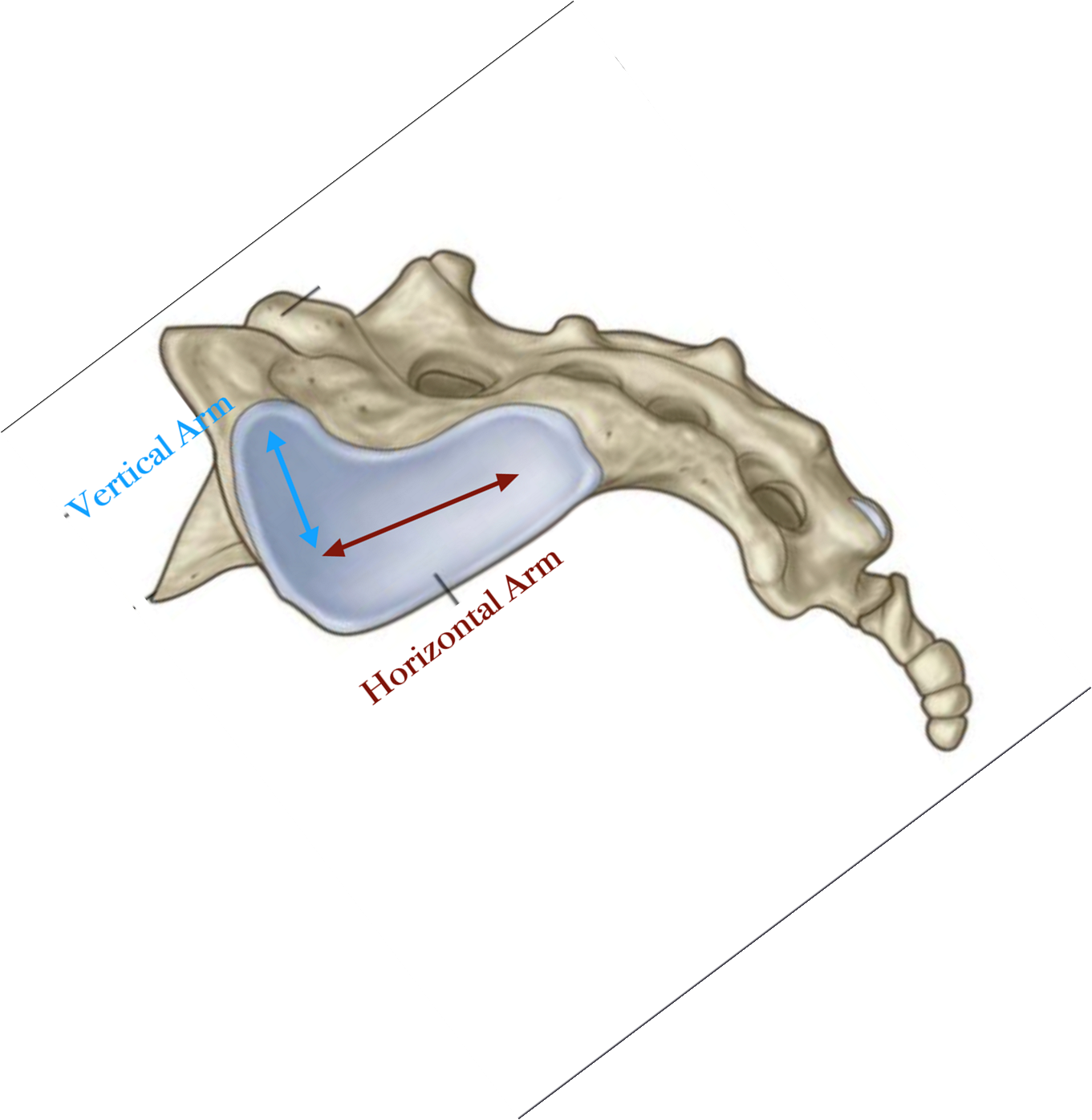
How do the ilia move in nutation?
Both ilia rotate posteriorly in a sagittal plane on an inferior transverse axis located at S2.
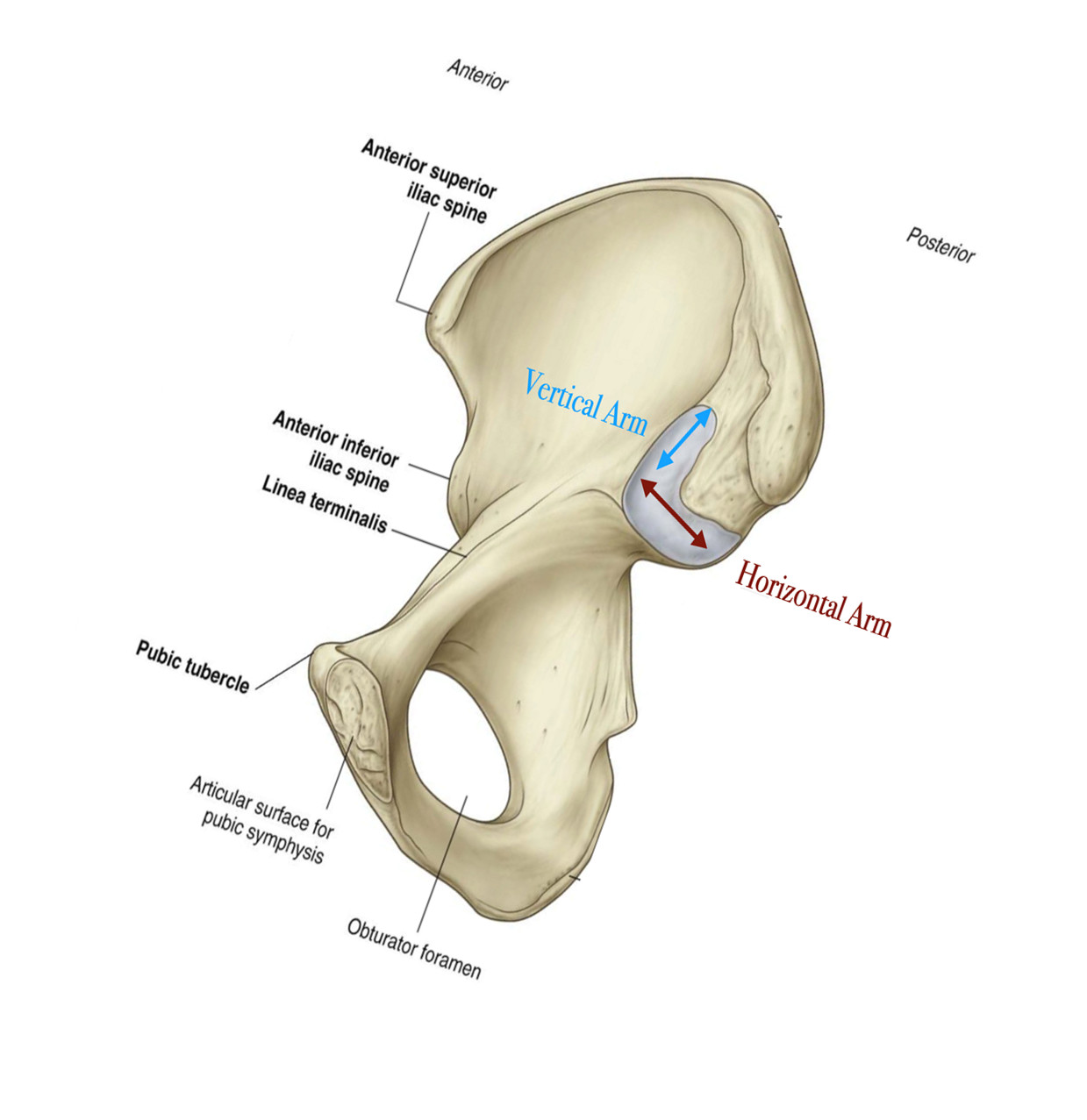
Parts of the ilia and their action during nutation?
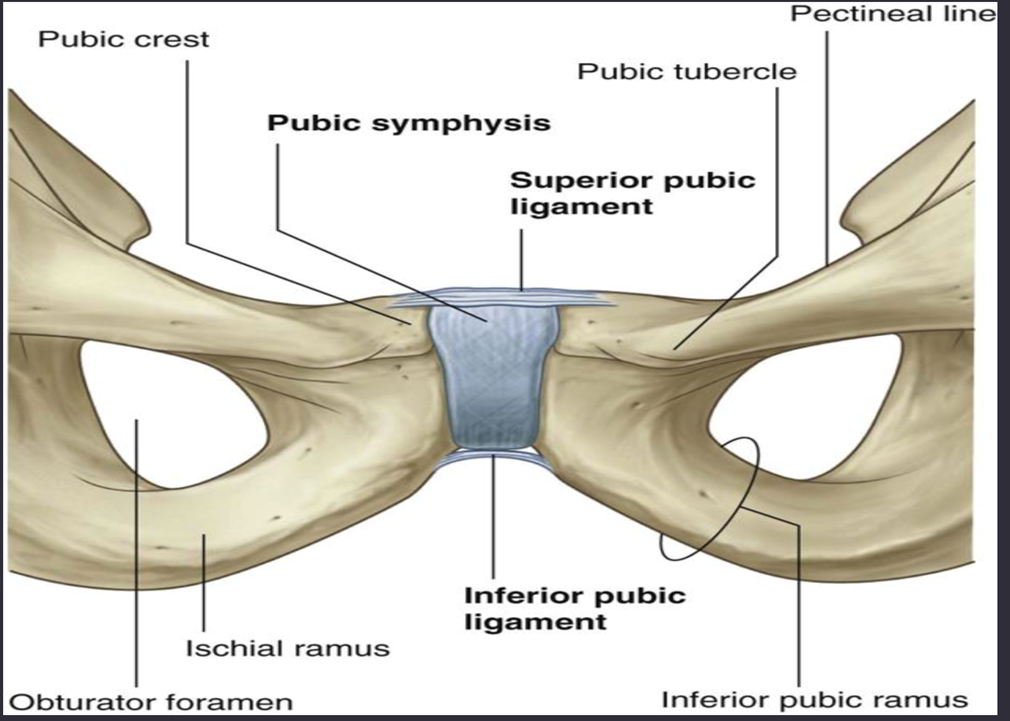
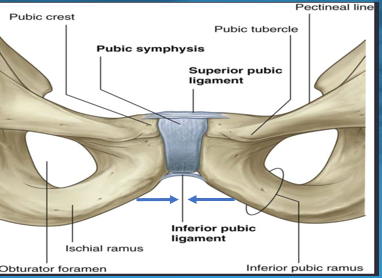
Each iliac crest, ASIS, PSIS and superior aspect of pubic symphysis tilt inward in a frontal/coronal plane on an anterior-posterior axis towards one another.
Simultaneously each inferior aspect of the pubic symphysis moves away from each other.
What does nutation do to the pelvic inlet?
Nutation causes a decrease in the pelvic inlet
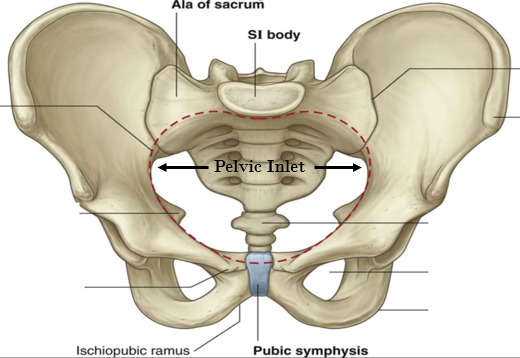
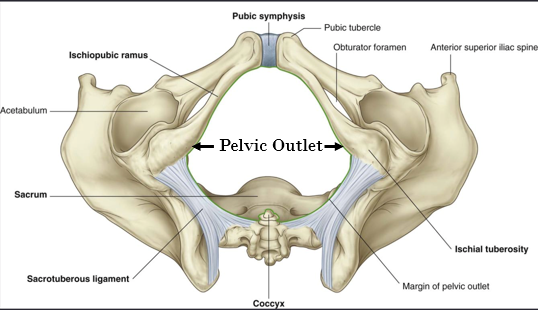
What does nutation do to the pelvic outlet?
Nutation causes an increase in the pelvic outlet
So the pelvis should be in a position of nutation for delivery of the baby through the pelvic outlet.
What happens if the mom’s pelvis gets stuck in excessive nutation?
If the mom’s pelvis gets stuck in excessive nutation after a delivery, it can result in post-partum lumbopelvic pain.
Counternutation
The posterior tilting of the sacrum relative to an anterior rotation of the ilia.
How does the sacral base move during counternutation?
The sacrum extends moving the sacral base superiorly and posteriorly in the sagittal plane on a middle transverse axis located at S2.
How does the sacral apex move during counternutation?
The sacrum extends moving the sacral apex inferiorly and anteriorly in the sagittal plane on a middle transverse axis located at S2.
How does the ilia move during counternutation?
Both ilia rotate anteriorly in the sagittal plane on a transverse axis located at S2.
How do the parts of ilia move during counternutation?
Each iliac crest, ASIS, PSIS and superior aspect of pubic symphysis tilt outward in a frontal/coronal plane on an anterior-posterior axis away from one another.
Simultaneously each inferior aspect of the pubic symphysis moves toward each other.
What does counternutation do to the pelvic inlet and outlet?
Counternutation causes an increase in the pelvic inlet and a decrease in the pelvic outlet
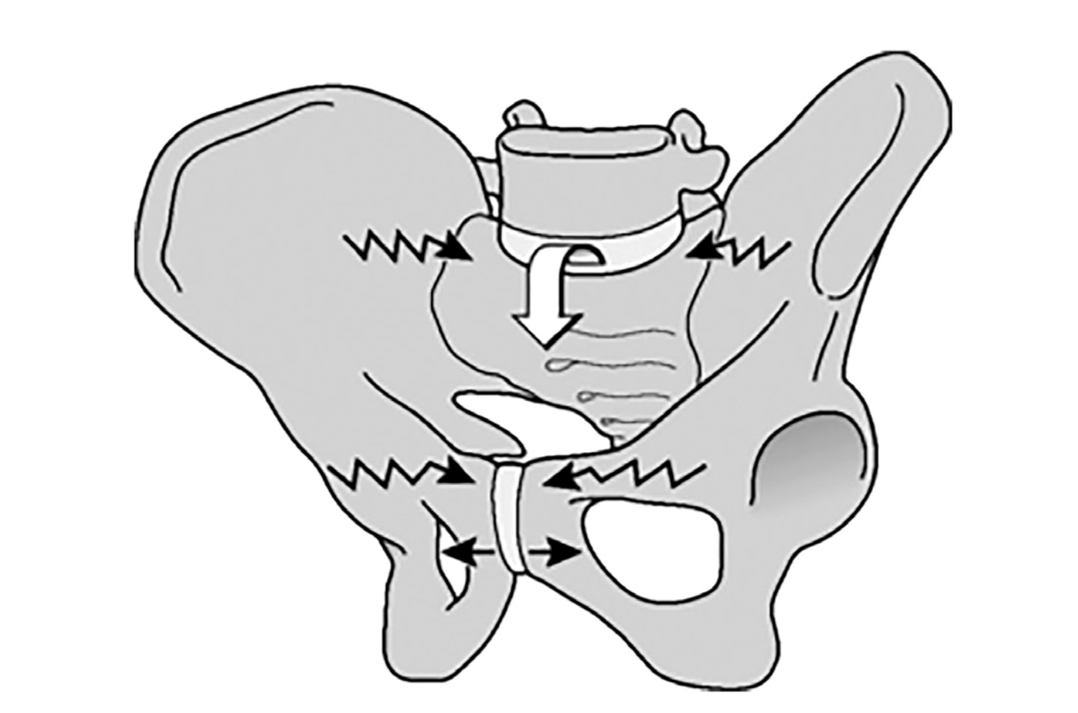
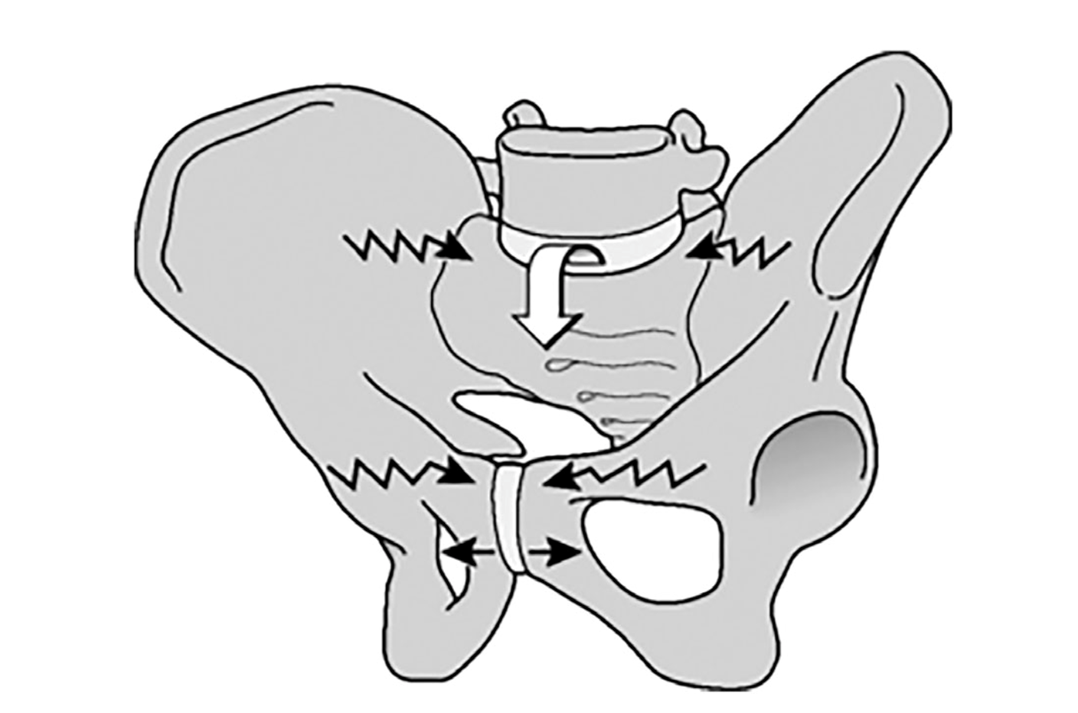
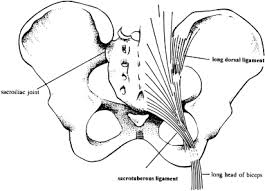
Nutation and pelvic stability
Nutation causes tensioning of SIJ ligaments; therefore, drawing together the posterior iliac bones. The coming together of the posterior iliac bones increases the compression of the SIJ.
This increased compression creates increased friction between the sacrum and the innominate. This combination of compression and
increased friction creates a force closure that allows the SIJ to effectively transfer loads between the trunk, pelvis and lower
extremities.
What can excessive nutation lead to?
Pain
Counternutation and decreased pelvic stability
Counternutation causes slackening of SIJ ligaments (except long dorsal ligament); therefore, allows the posterior iliac bones to be draw away from each other. This slackening, decreases compression in the SIJ and make it less stable; consequently, the patient will be more susceptible for injury and pain.
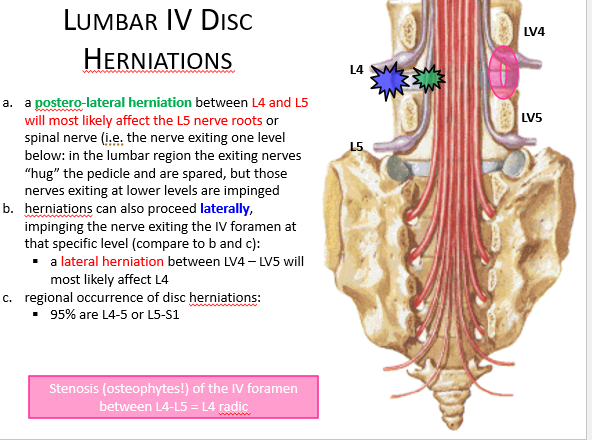
Where are disc herniations more likely to occur?
Herniations are more likely to occur posterolaterally, where the annulus fibrosus is thinner and lacks the structural support from the posterior longitudinal ligament
95% of disc herniations in the lumbar spine occur between L4-L5 and L5-S1
What are the effects of disc herniation?
Disc herniations may cause changes in sensation and muscle strength, if they impinge upon a nerve or nerve roots.
It is imperative that the physician can identify the neurological deficit and work their way backwards to find the protruding disc causing the neurological deficit.
Do symptoms associated with acute herniated disc resolve?
Over 85% of patients with symptoms associated with an acute herniated disc will resolve within 8 to 12 weeks without any specific treatments.
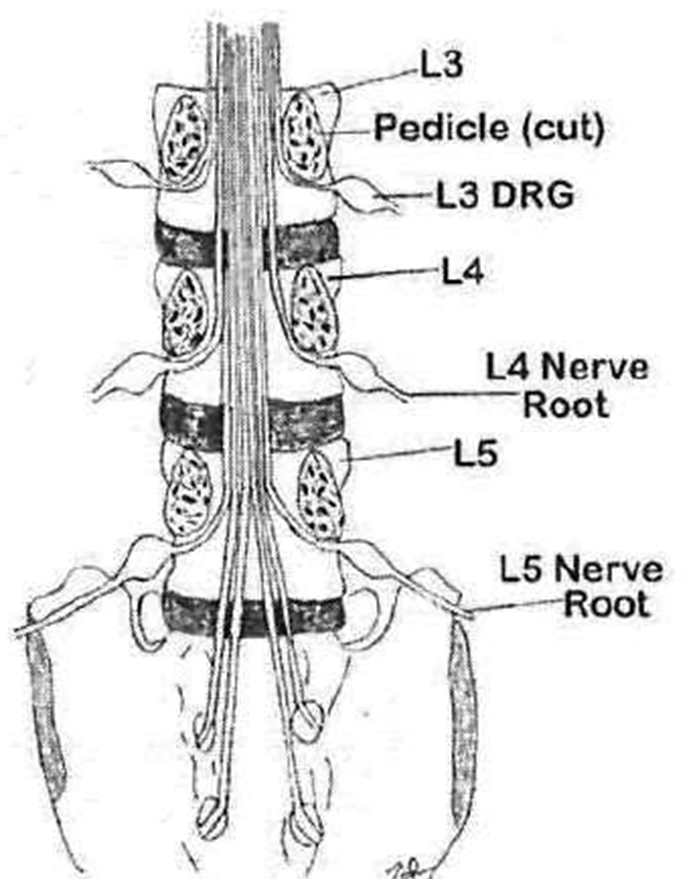
Where do most spinal nerves exit?
Through the intervertebral foramen
C1-C7 exit above the vertebral pedicle
(C8 exits above T1)
T1-S4 exit below the vertebral pedicle
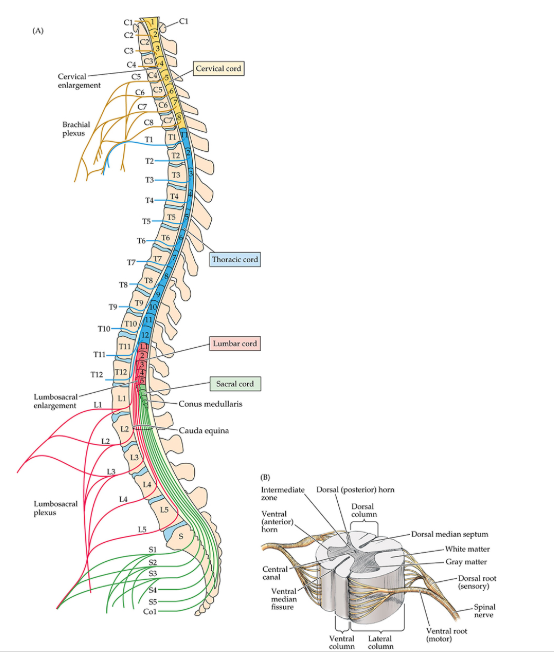
Why does C8 exit above T1?
There are only 7 cervical vertebrae
So T1 will then exit the intervertebral foramen created by T1 and T2
What are the 3 different terms a posterolateral herniation can be called?
Posterolateral
Paracentral
Lateral
What are the symptoms of an impingement upon the C5 nerve root?
difficulty feeling the lateral deltoid region and abducting their arms, that is a C5 nerve dysfunction
The C5 nerve exits through the C4/C5 intervertebral foramen.
A paracentral or far lateral disc C4/C5 herniation will impinge upon nerve root C5.
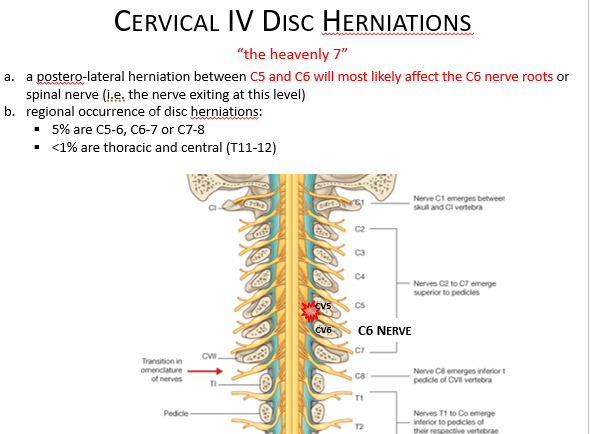
What are the most common cervical disc herniations?
The most common cervical disc herniations are the C5/C6 and C6/C7 discs
Therefore, the patient may present with the following:
•decreased motor strength
•decreased sensation
•paresthesia (feeling of tingling, numbness or “pins and needles)
•hyperreflexia
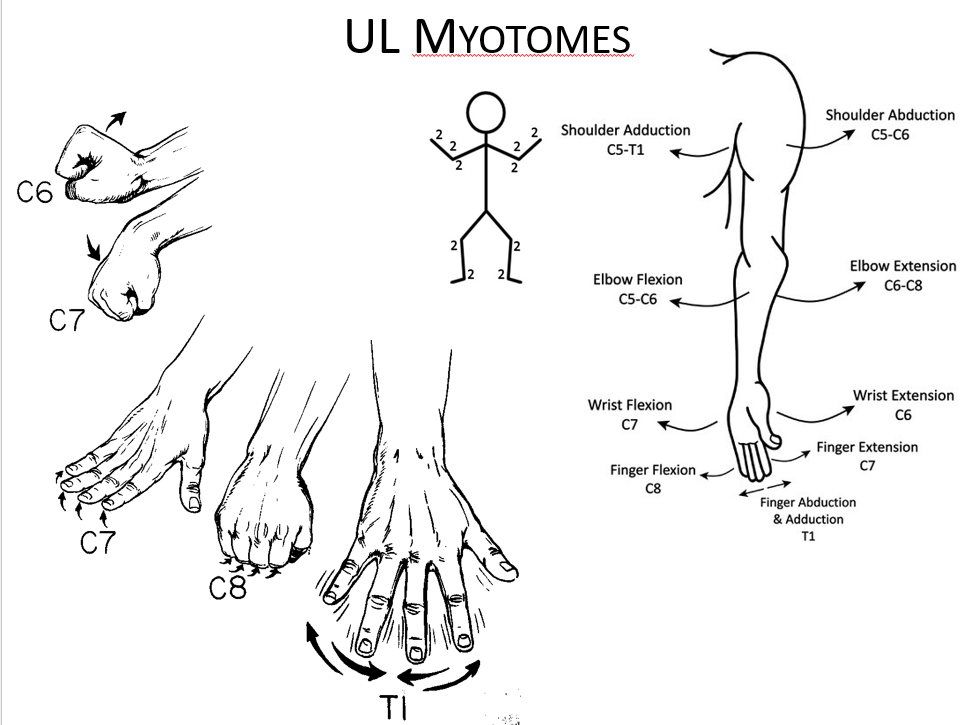
What sensory and motor symptoms would you see with cervical disc herniations of C5 and C6?
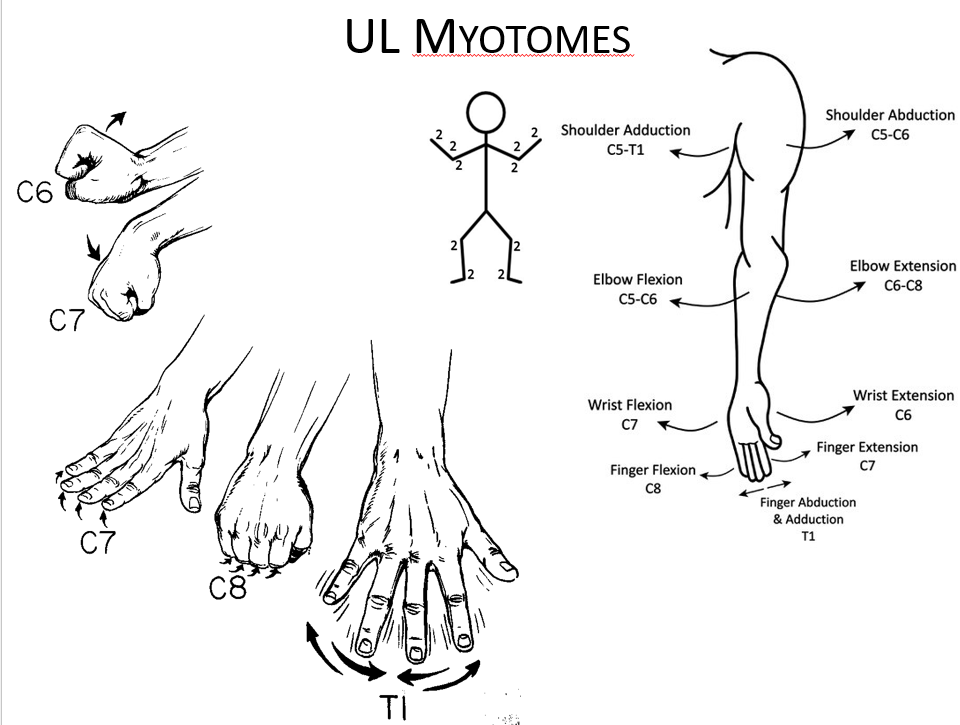
•C5 nerve root: Exits between C4 and C5 foramina, innervates deltoids and biceps (with C6), sensory distribution: lateral arm (axillary nerve) and is assessed with biceps reflex.
•C6 nerve root: Exits between C5 and C6 foramina, innervates biceps (with C5) and wrist extensors, sensory distribution: lateral forearm (musculocutaneous nerve), assessed with brachioradialis reflex.
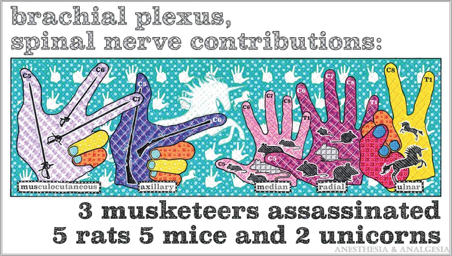
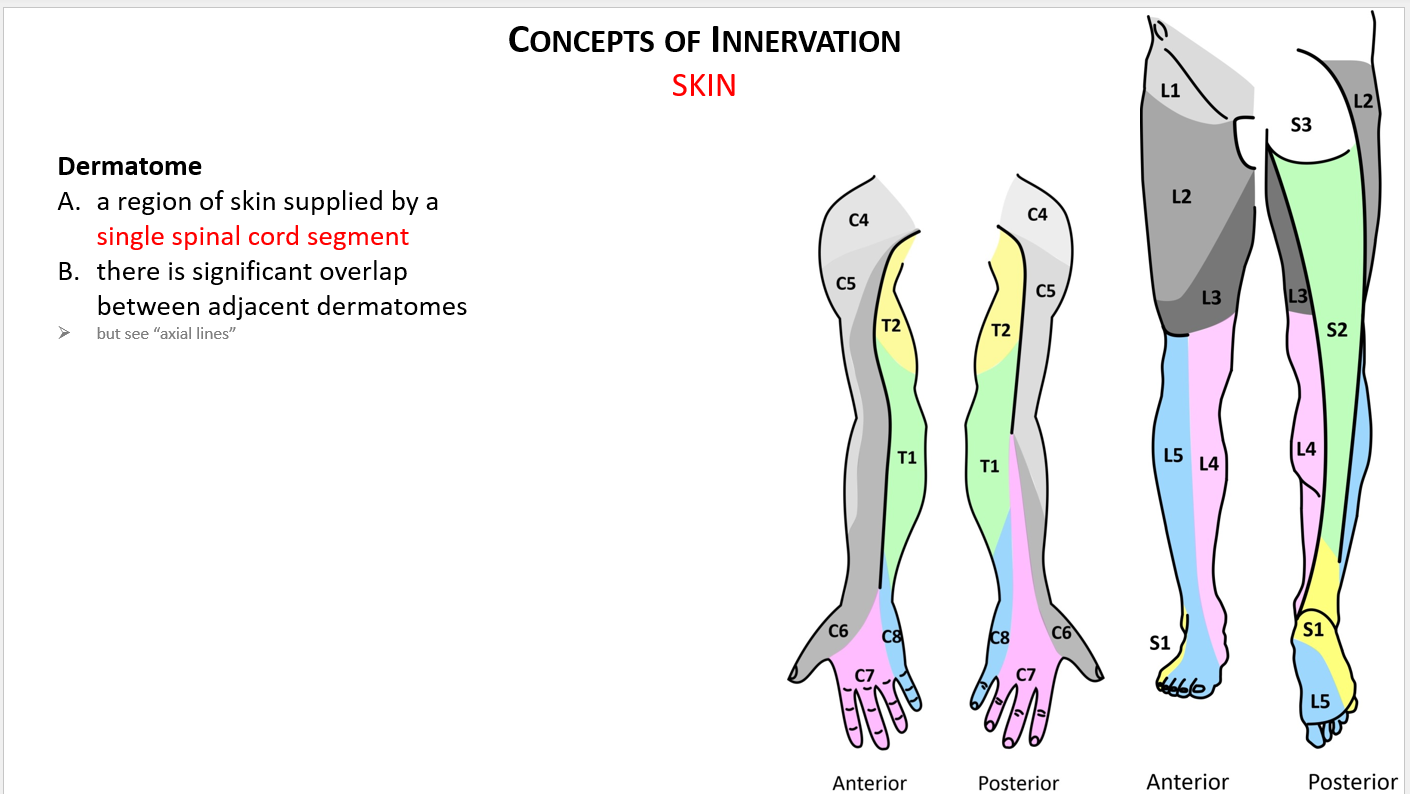
What sensory and motor symptoms would you see with cervical disc herniations of C7 and C8?
•C7 nerve root: Exits between C6 and C7 foramina, innervates triceps, wrist flexors, and finger extensors, sensory distribution: middle finger, assessed with triceps reflex.
•C8 nerve root: Exits between C7 and T1 foramina, innervates interosseus muscles and finger flexors, sensory distribution: ring and little fingers and distal half of the forearm (ulnar side), no reflex.
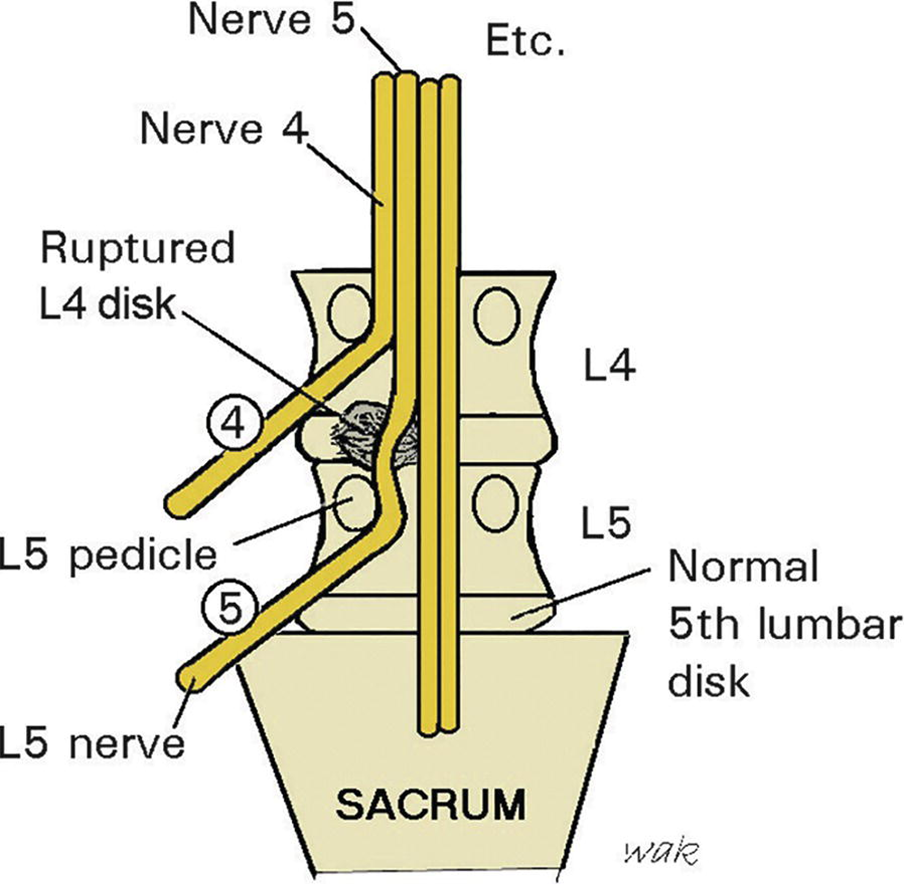
Paracentral/lateral/posterolateral herniation
A paracentral or lateral herniation, will cause the transversing nerve root to be affected.
The L5 nerve root exits between the L5 and S1 foramina.
A lateral herniation of the L4-L5 disc would cause L5 radiculopathy.
L5 radiculopathy would cause sensory loss around the great toe and top of the foot and decreased ability to extend the great toe (extensor hallucis longus)
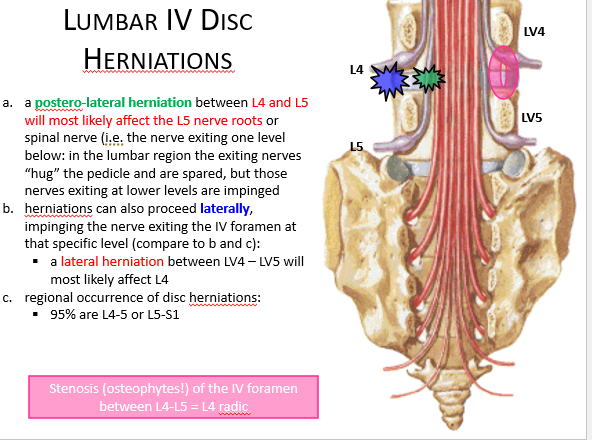
Far lateral herniation
A far lateral herniation, will cause the exiting nerve to be affected int he lumbar spine.
A far lateral herniation of the L4-L5 disc would cause L4 radiculopathy.
L4 radiculopathy would cause sensory loss around medial aspect of the ankle, foot and muscle weakness with inversion of the ankle (tibialis anterior), and diminished patellar tendon reflex.
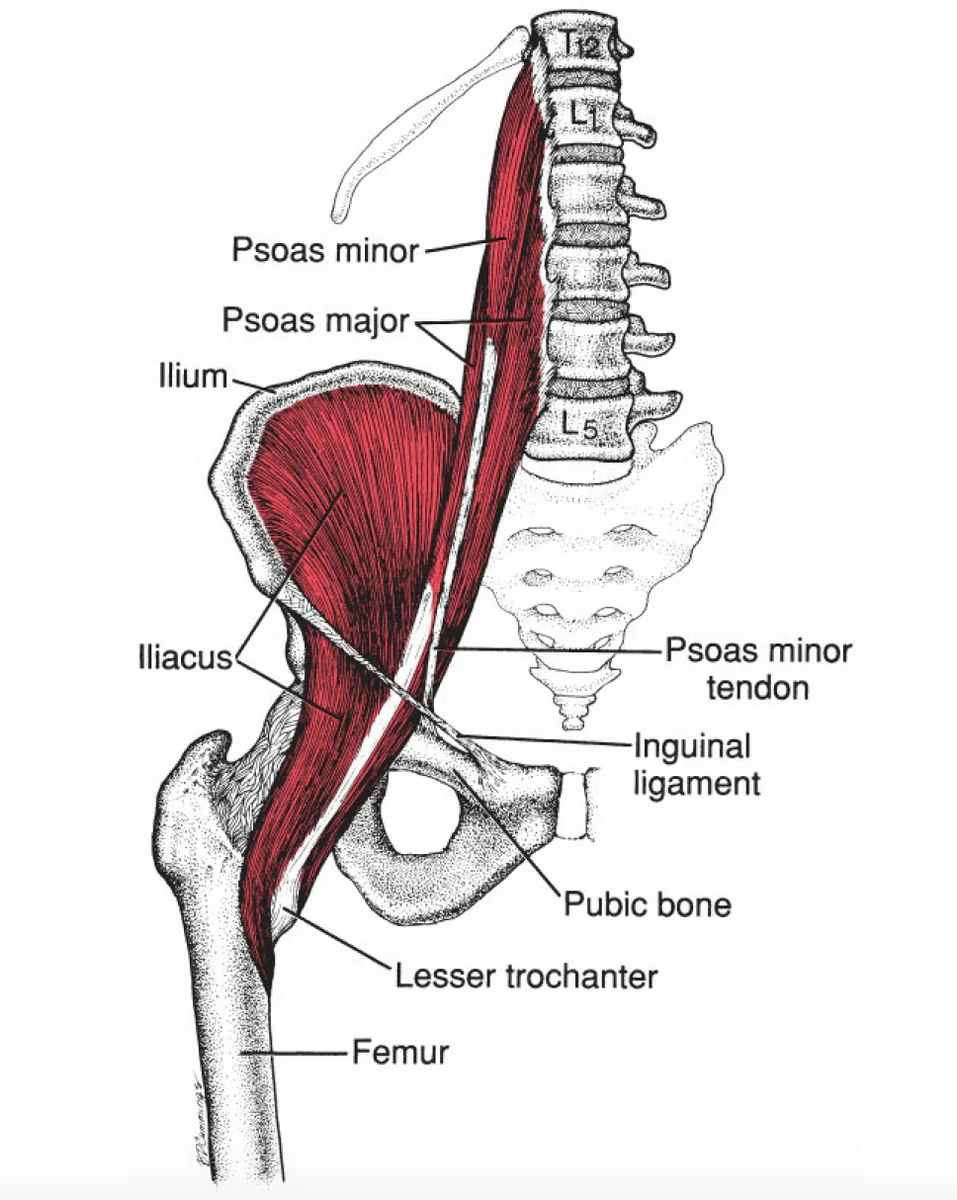
What sensory and motor symptoms would you see with lumbar disc herniations of L1, L2, and L3?
•L1 nerve root: Exits between L1 and L2 foramina, innervates iliopsoas muscle, sensory distribution: upper third thigh, assessed with the cremasteric reflex (male).
•L2 nerve root: Exits between L2 and L3 foramina, innervates iliopsoas muscle, hip adductor, and quadriceps, sensory distribution: middle third thigh, no reflex.
•L3 nerve root: Exits between L3 and L4 foramina, innervates iliopsoas muscle, hip adductor, and quadriceps, sensory distribution: lower third thigh, no reflex.
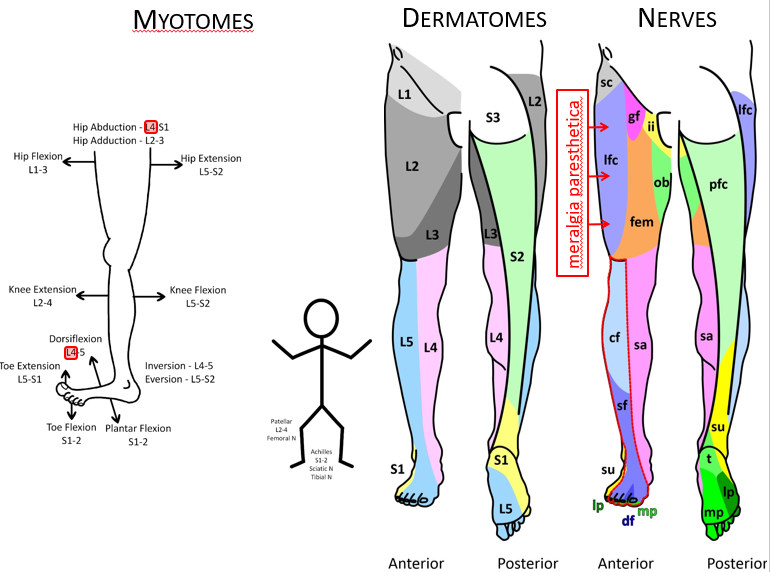
What sensory and motor symptoms would you see with lumbar disc herniations of L4, L5, and S1?
•L4 nerve root: Exits between L4 and L5 foramina, innervates quadriceps and tibialis anterior, sensory distribution: anterior knee, medial side of the leg, assessed with patellar reflex.
•L5 nerve root: Exits between L5 and S1 foramina, innervates extensor hallucis longus, extensor digitorum longus, and brevis, and gluteus medius, sensory distribution: anterior leg and dorsum of the foot, no reflex.
•S1 nerve root: Exits between S1 and S2 foramina, innervates gastrocnemius, soleus, and gluteus maximus, sensitive distribution: posterior thigh, lateral distal lower extremity, plantar region, assessed with Achilles reflex.
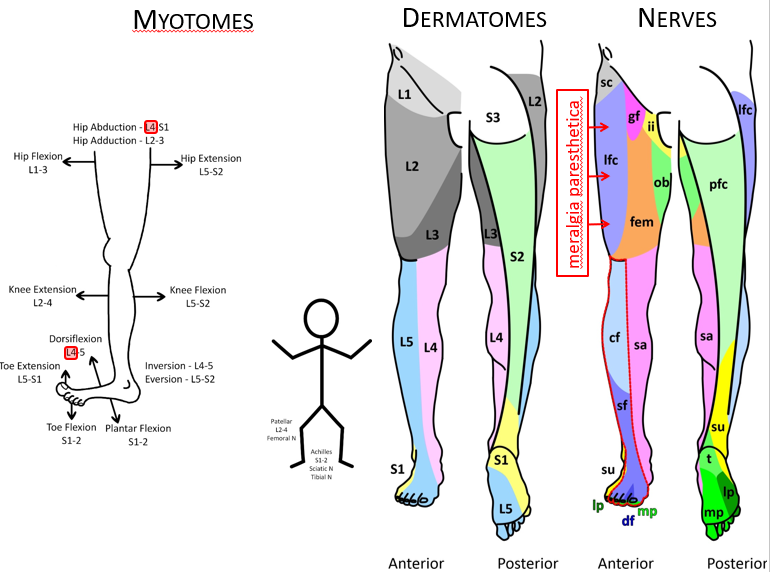
When testing T12-L3 motor function what action should you have the pt do? What muscle is this testing?
Hip flexion
Iliopsoas
When testing L2-L4 motor function what action should you have the pt do? What muscle is this testing?
Knee extension
Quadriceps
When testing L4 motor function what action should you have the pt do? What muscle is this testing?
Foot inversion and dorsiflexion
Tibialis anterior
Also do the patellar reflex
When testing L5 motor function what action should you have the pt do? What muscle is this testing?
Great toe extension
Extensor hallucis longus
When testing S1 motor function what action should you have the pt do? What muscle is this testing?
Gastronemius for plantar flexion
Fibularis longus and brevis for foot eversion
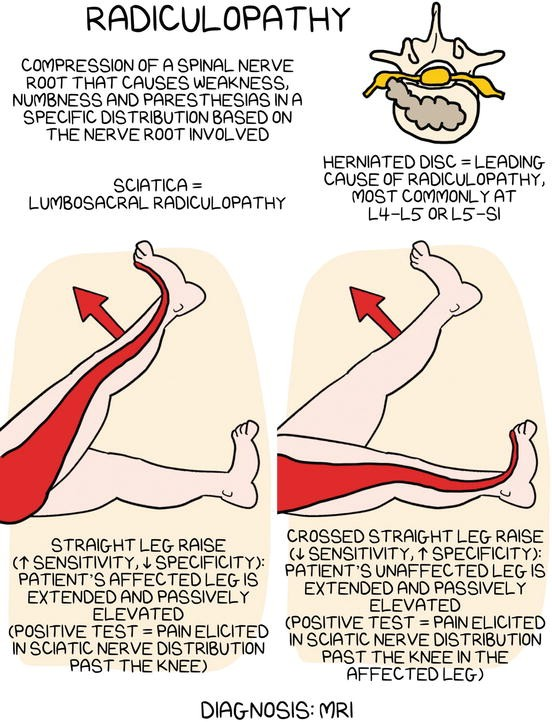
Straight leg test
Straight leg test is better at ruling out a lumbar disc herniation with a sensitivity upwards of 92%.
It has a poor specificity of ruling in a lumbar disc herniation.

Crossed straight leg test
Crossed straight leg test is better at ruling in a lumbar disc herniation with a specificity upwards of 90%.
It has a poor sensitivity of ruling out a lumbar disc herniation.
Back pain red flags
•Urinary retention/incontinence
•Fecal incontinence/decreased sphincter tone
•Saddle anesthesia (a loss of sensation in the area covered by a saddle, including the buttocks, perineum, and inner thighs)
•Lower leg weakness or numbness
•Progressive neurologic deficit, major motor or sensory deficit (cauda equina syndrome)
•Cancer
•History of cancer
•Weight loss
•Night pain
•History prolonged corticosteroid use or significant trauma = fracture
•Infection
•Fever
•Recent or current bacterial infection
•Rest pain
Vertebrae, spinal cord, and nerve root anatomy
•Five lumbar vertebrae, distinct large quadrangular spinous processes.
•Large vertebral bodies able to sustain longitudinal loads.
•Nerve roots exit intervertebral foramen below corresponding vertebrae, just above the intervertebral disc.
•Spinal cord typically terminates at L1/L2, with nerve roots becoming longer in the lower segments of the spine.
Posterior longitudinal ligament anatomy
•Runs vertically along the posterior vertebral bodies.
•Ligament begins to narrow in the lumbar region, at L4-L5 is ~1/2 width as compared to L1 level.
•Narrowing weakens posterior lateral aspect of intervertebral discs, making lumbar area more susceptible to disc herniations.
•Tapers laterally below L3
Lordotic curve
Natural curve present in the lumbar spine designed for longitudinal loads
Iliopsoas muscle
•Primary flexor of the hip
•Important role in maintaining lumbosacral angle.
•Composed of psoas major and iliacus muscles.
•Origin T12-L5 vertebral bodies, insertion lesser trochanter of femur.
•Somatic dysfunction of iliopsoas very common, usually secondary to prolonged shortening of the muscle.
At what spinal level is the umbilicus?
Area anterior to L3-L4
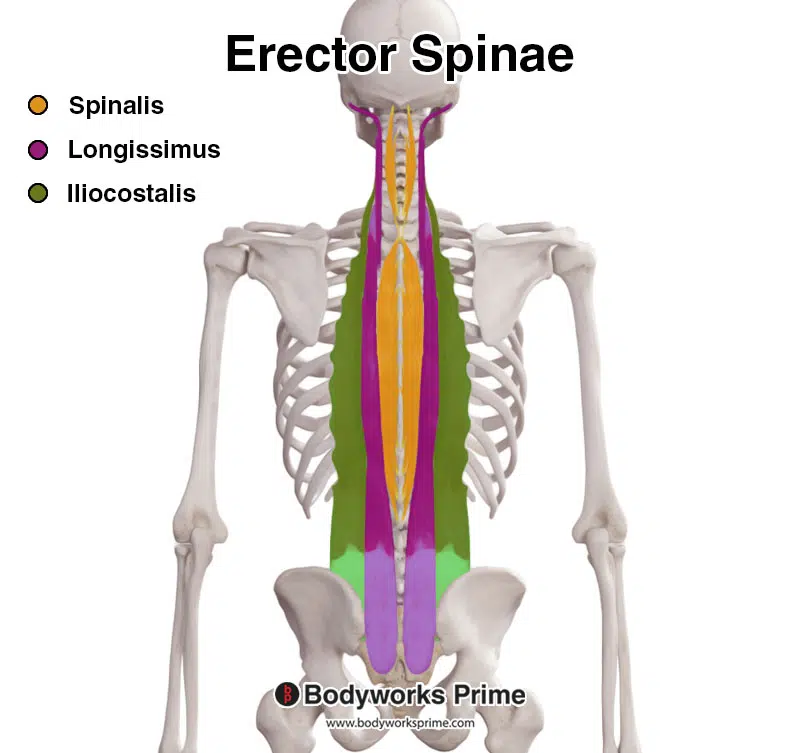
Way to remember the erector spinae muscles?
“I love spaghetti”
I = iliocostalis
LO = longissimus
S = spinalis
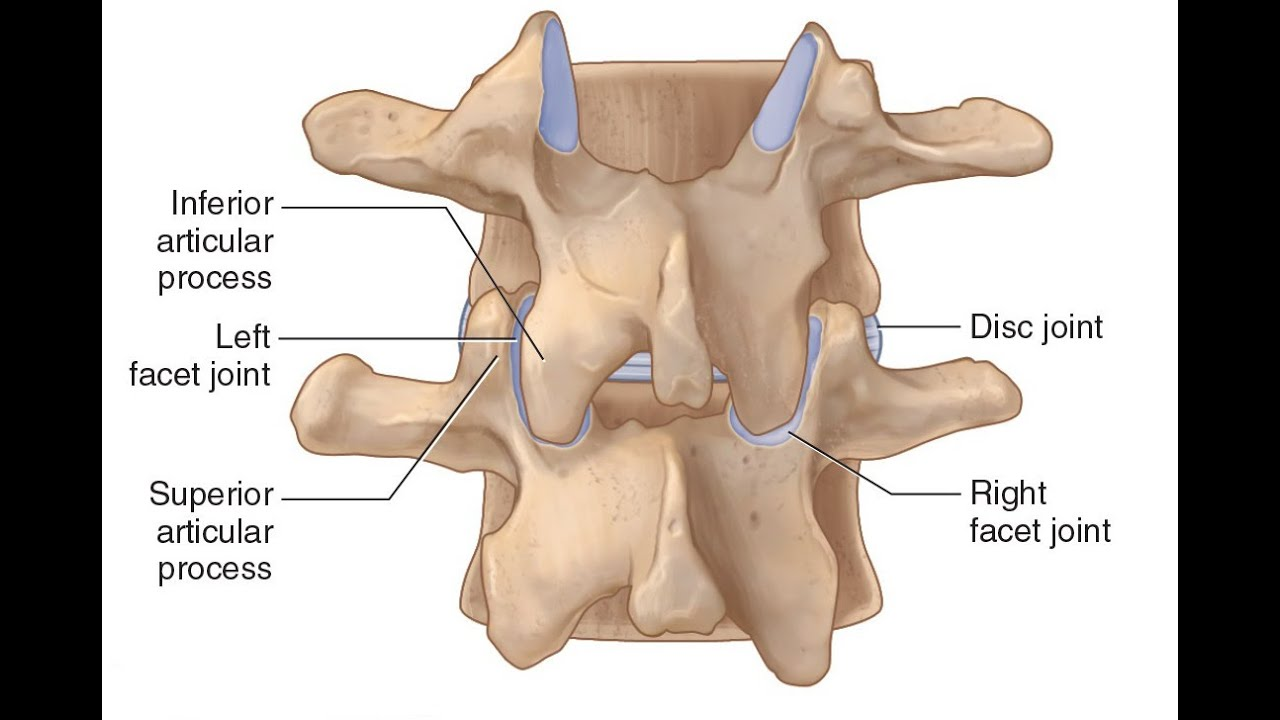
Facet tropism
•Most common anomaly of the lumbar spine
•Asymmetry of facet joint angles
•Most common anomaly
•Pre-disposition to early degenerative changes
Also called zygopophyseal trophism
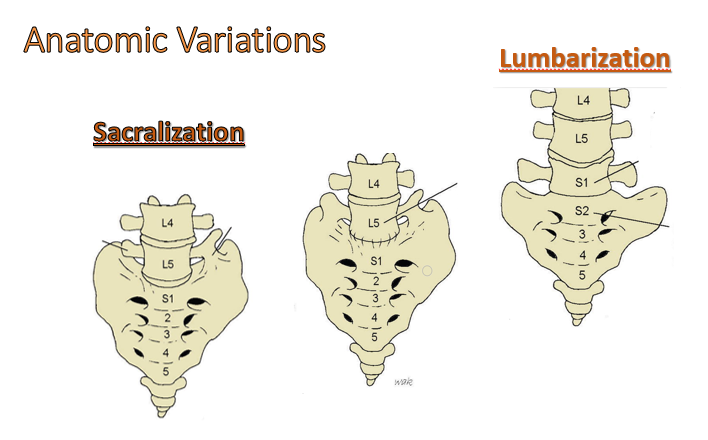
Sacralization vs Lumbarization
Sacralization:
deformity where one or both transverse processes of L5 articulate with the sacrum.
~3.5% of people have this, may lead to early disc degeneration.
Lumbarization: S1 failure to fuse with rest of sacrum. Less common than Sacralization.
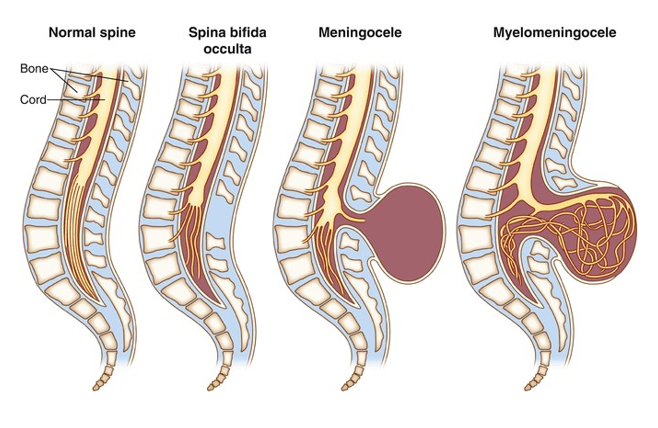
Spina bifida types
•Spina Bifida: Developmental anomaly, lamina of vertebral segment fails to close
3 Types:
•Spina Bifida Occulta
•No herniation through defect
•Rare neurological deficits
•often only physical sign is coarse hair patch over the defect site.
•Spina Bifida Meningocele
•Herniation of the meninges through defect.
•Spina Bifida Meningomyelocele
•Herniation of meninges and nerve root through defect.
•Associated with neurological deficits.
How does L5 motion affect the motion of the sacrum?
•L5 sidebending causes sacral oblique access to be engaged on same side.
•L5 rotation causes sacrum to rotate to opposite side.
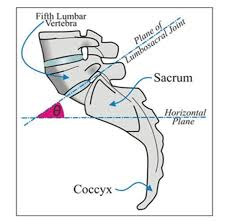
Lumbosacral Angle aka Ferguson’s angle
•Formed in upright position, side view, by extending line of inclination of the sacrum as it meets a line parallel to the ground.
•Normal angle 25-35 degrees
•increased angle changes articular relationships (results in back pain), inferior lumbar facets slide caudally on matched superior sacral facets, and results in back pain.
•Obesity, pregnancy, abdominal muscle weakness, wearing high heeled shoes, foot pronation, spondylolisthesis, poor posture, occupation, hereditary predisposition, and many more factors can influence angle
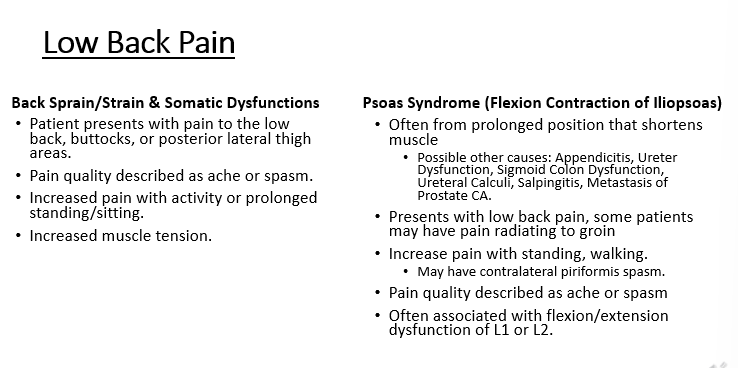
Low back pain: Back sprain, strain, and somatic dysfunctions
•Patient presents with pain to the low back, buttocks, or posterior lateral thigh areas.
•Pain quality described as ache or spasm.
•Increased pain with activity or prolonged standing/sitting.
•Increased muscle tension.
Low Back Pain: Psoas Syndrome (Flexion Contraction of Iliopsoas)
•Often from prolonged position that shortens muscle
•Possible other causes: Appendicitis, Ureter Dysfunction, Sigmoid Colon Dysfunction, Ureteral Calculi, Salpingitis, Metastasis of Prostate CA.
•Presents with low back pain, some patients may have pain radiating to groin
•Increase pain with standing, walking.
•May have contralateral piriformis spasm.
•Pain quality described as ache or spasm
•Often associated with flexion/extension dysfunction of L1 or L2
Low Back Pain: herniated Nucleus Pulposus
•Due to posterior lateral herniation of intervertebral disc near narrowing of posterior longitudinal ligament exerting pressure on nerve root.
•98% at L4 and L5
•Patient presents with pain to the low back, and lower extremity.
•Pain quality described as numbness/tingling, possible sharp/burning/shooting pain toward lower extremity
•Increased pain with flexion.
•Weakness & Decreased Reflexes from affected nerve root, sensory deficit to affected dermatome.
Treatment: Conservative, PT, OMT (HVLA: Relative contraindication)
Spinal Stenosis
•Narrowing of spinal canal or foramen
•Secondary to degenerative changes
•Symptoms:
•LBP that may radiate to lower extremities
•Worse with extension
•Goals of OMT
•Decrease restrictions
•Improve range of motion
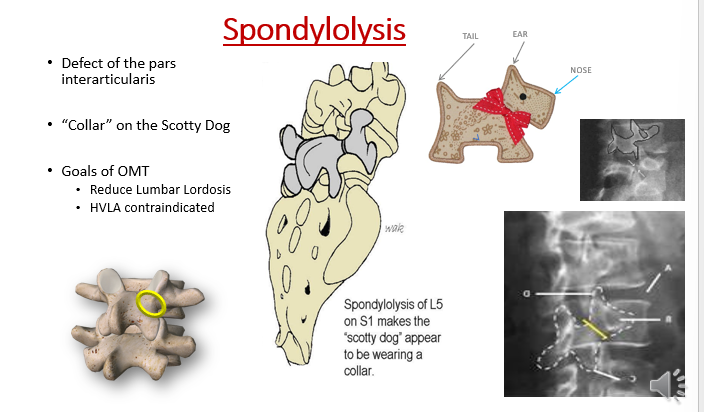
Spondylolysis
•Defect of the pars interarticularis without anterior displacement of vertebral body.
•“Collar” on the Scotty Dog
•Goals of OMT: Reduce Lumbar Lordosis; HVLA contraindicated
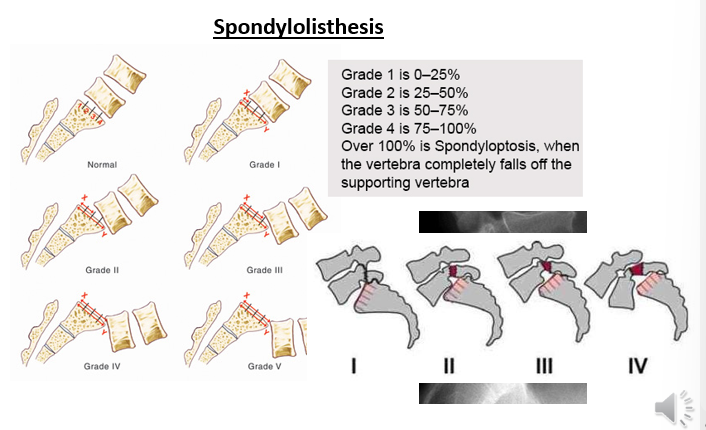
Spondylolisthesis
•Anterior displacement of one vertebrae on the other
•Vertebral step-off sign
•Graded I – IV based on degree of anterior displacement
• Diagnosed using lateral x-rays
20% to 70% of persons with spondylolisthesis also have a spondylolysis
Backwards slippage = retrolisthesis
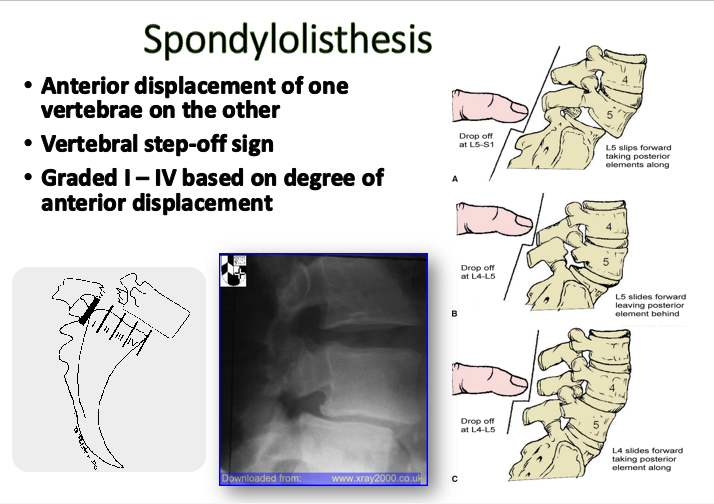
Spondylolisthesis grading
Graded I – IV based on degree of anterior displacement
1 = 0-25%
2 = 25-50%
3 = 50-75%
4 = 75-100%
Over 100% is spondyloptosis, when the vertebra completely falls off the supporting vertebrae
Cauda equina syndrome
•Large central disc herniation with compression on nerve roots
•Signs/Symptoms:
•Saddle anesthesia
•Decreased DTR
•Decreased rectal sphincter tone
•Loss of bowel / bladder control
Condition requires emergent surgical decompression, if surgery is delayed irreversible paralysis may result.