CDC Lymphatic Filariasis
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
90% of LF cases are caused by W. bancrofti
The causative agents of lymphatic filariasis (LF) include the mosquito-borne filarial nematodes Wuchereria bancrofti, Brugia malayi, B. timori An estimated__________(Bancroftian filariasis).
Mansonia spp. and Aedes spp.
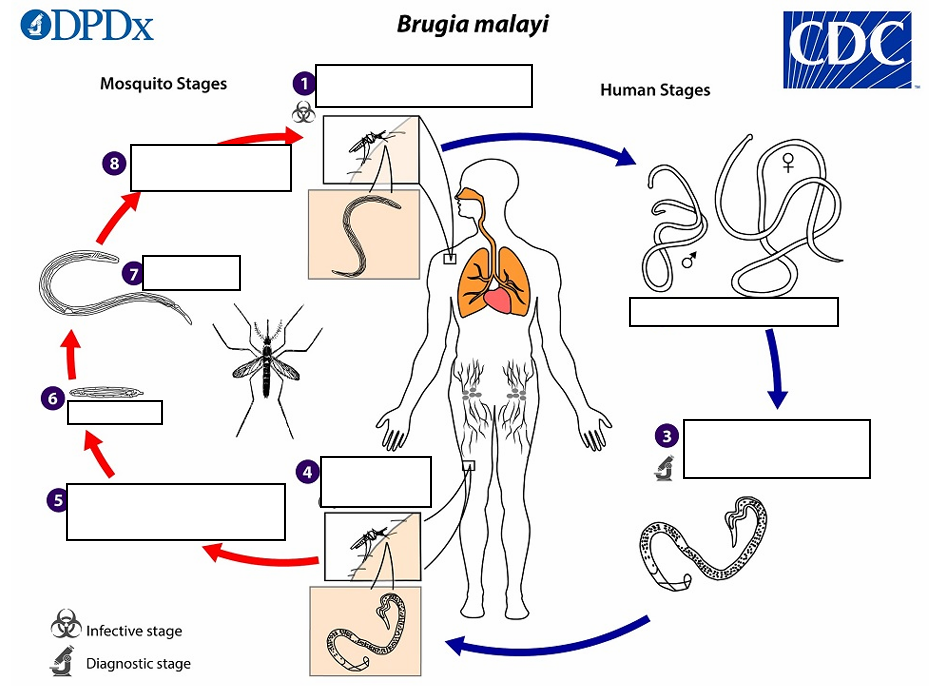
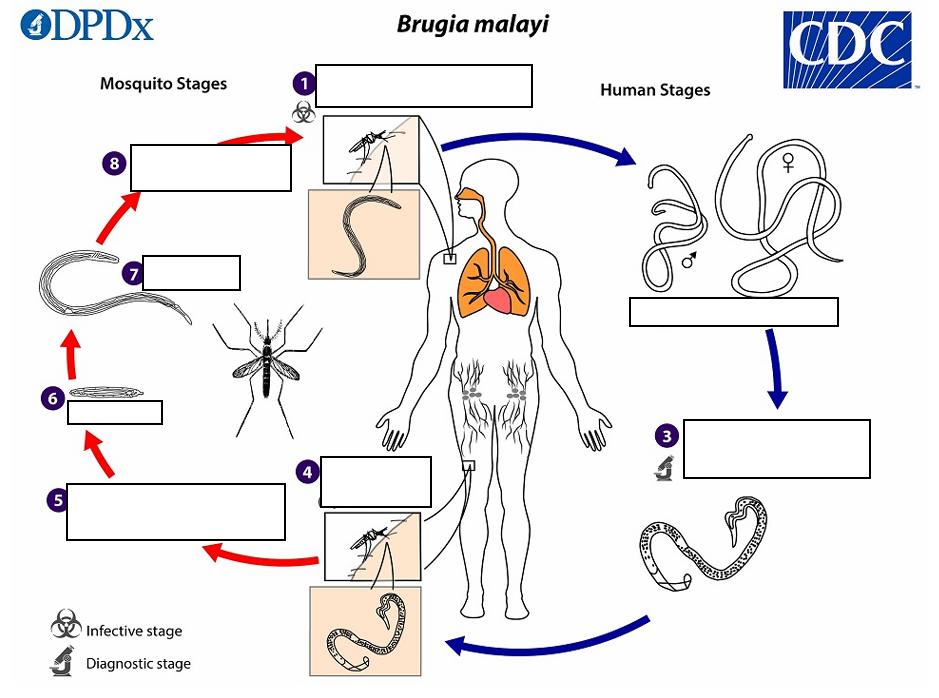
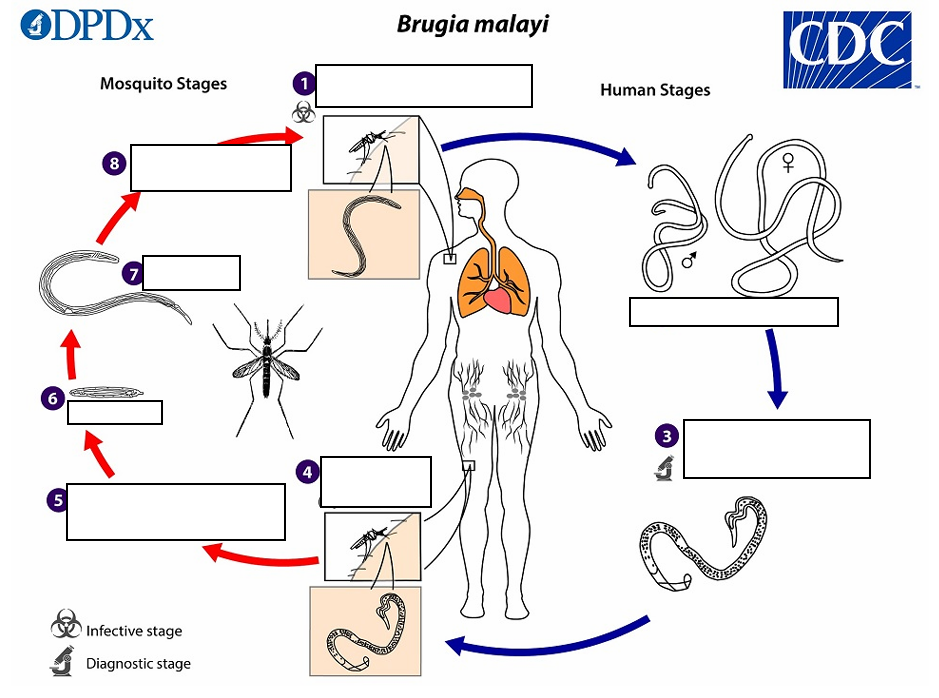
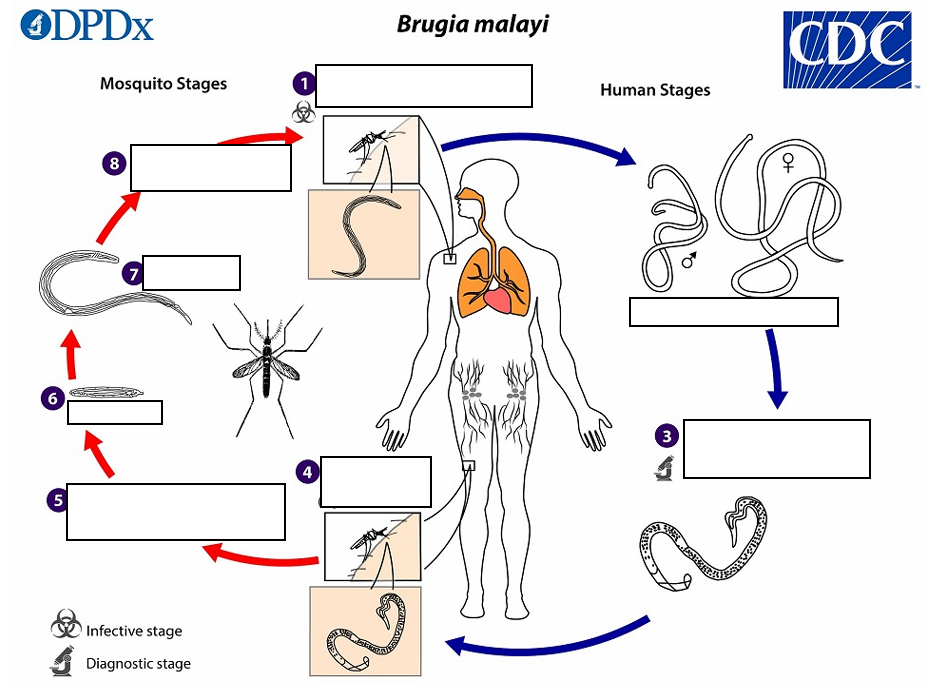
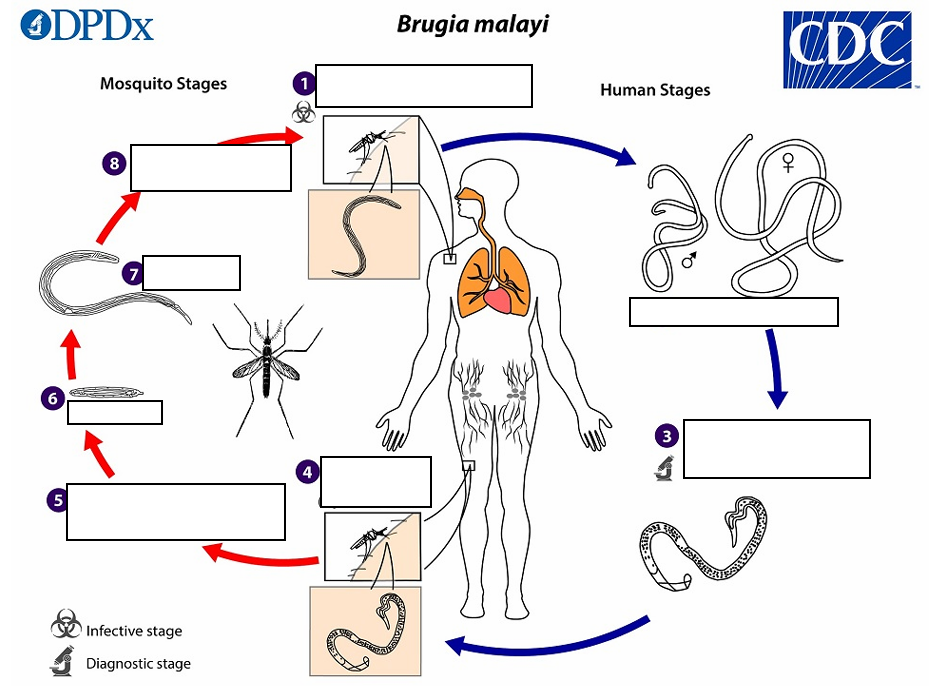
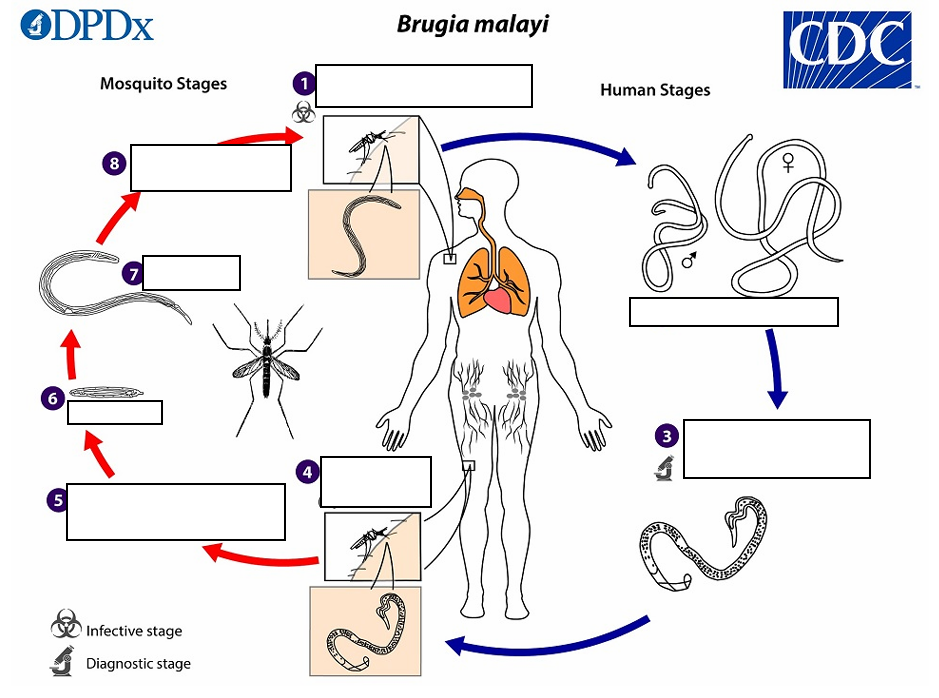
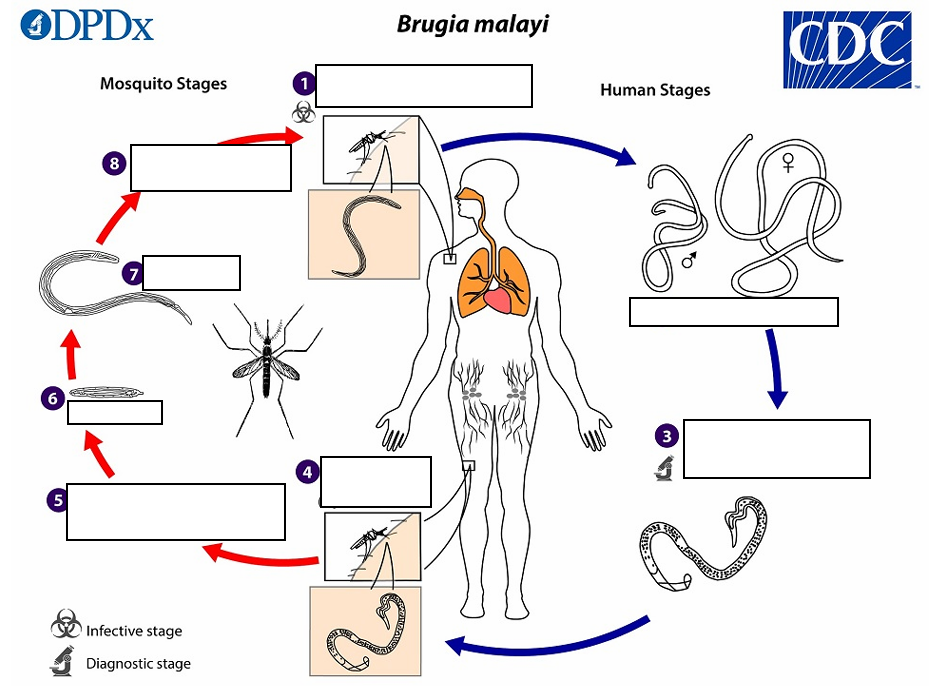
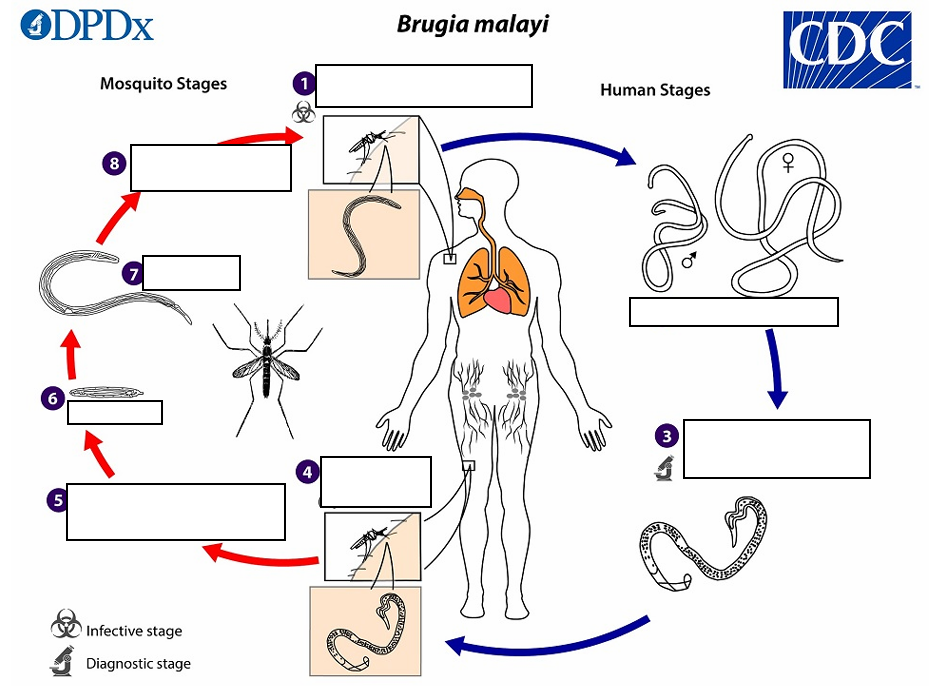
During a blood meal, an infected mosquito (typically_______and ____________) introduces third-stage filarial larvae onto the skin of the human host, where they penetrate into the bite wound
Wuchereria bancrofti but are smaller
(1) They develop into adults that commonly reside in the lymphatics
(2) The adult worms outwardly resemble those of.
43 to 55 mm, 130 to 170 μm
Female worms measure __ in length by in width,
13 to 23 mm, 70 to 80 μm
and males measure in length by in width.
sub-periodic
Adults produce microfilariae, measuring 177 to 230 μm in length and 5 to 7 μm in width, which are sheathed and have nocturnal periodicity (in some regions B. malayi may be _, and note that microfilariae are usually not produced in B. pahangi infections).
microfilariae (B. Malayi)
(3) A mosquito ingests the_______during a blood meal
sheaths
(4) After ingestion, the microfilariae lose their _____ and work their way through the wall of the proventriculus and cardiac portion of the midgut to reach the thoracic muscles.
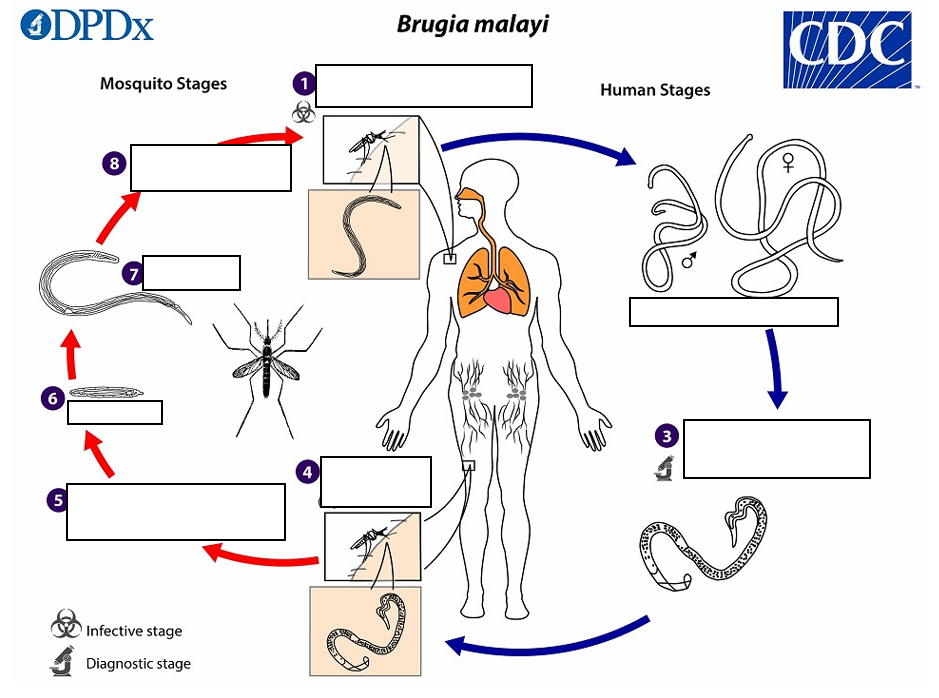
lymph and enter the blood stream,third-stage larvae
(5)The microfilariae migrate into_______reaching the peripheral blood and (6) subsequently into ______
hemocoel (B. Malayi)
(6) The third-stage larvae migrate through the______ to the mosquito’s proboscis and subsequently and can infect another human when the mosquito takes a blood meal
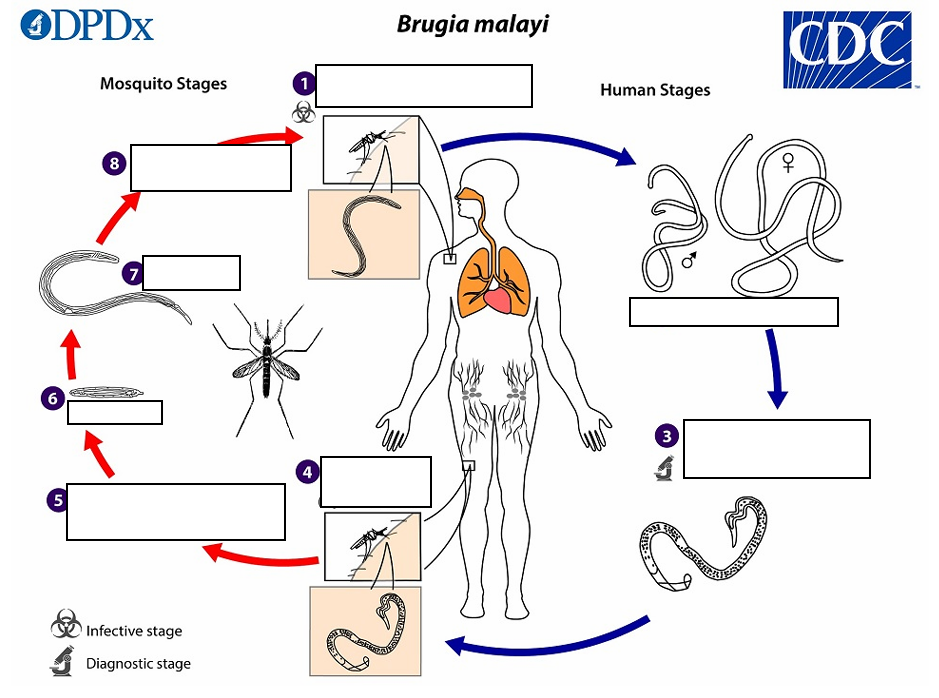
Mosquito takes a blood meal (L3 larvae enter skin) (B. Malayi)
(1) Infective Stage
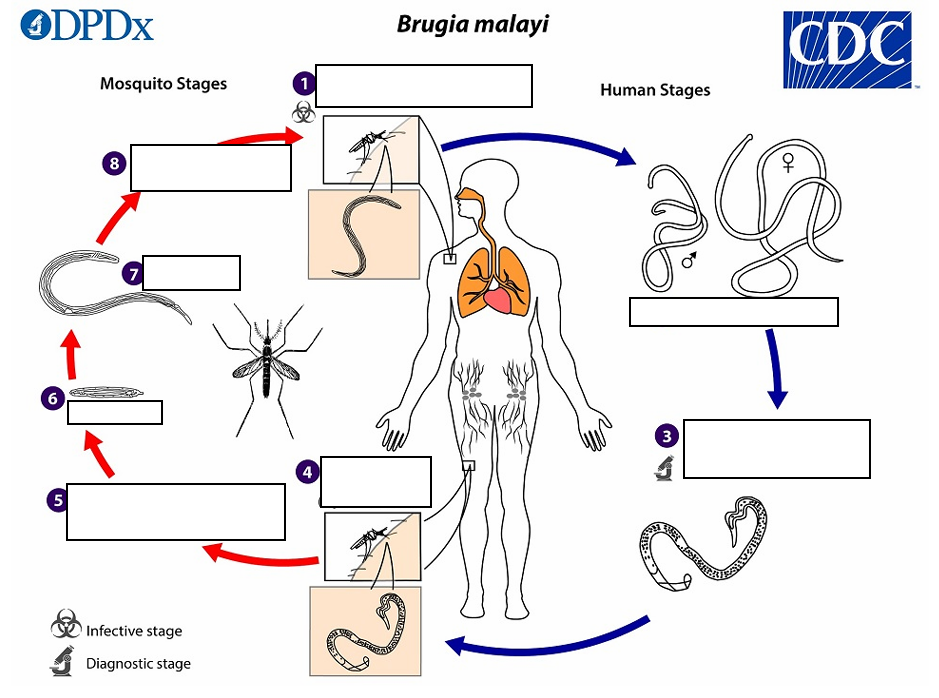
Adults in lymphatics (B. Malayi)
(2)
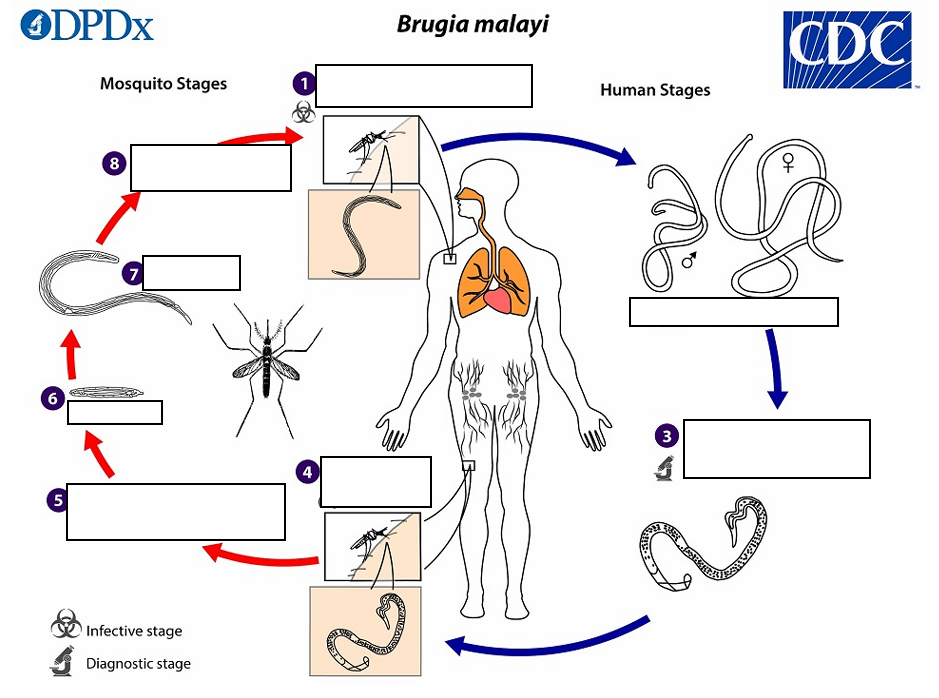
Adults produce sheathed microfilariae that enter peripheral circulation (B. Malayi)
(3) Diagnostic stage
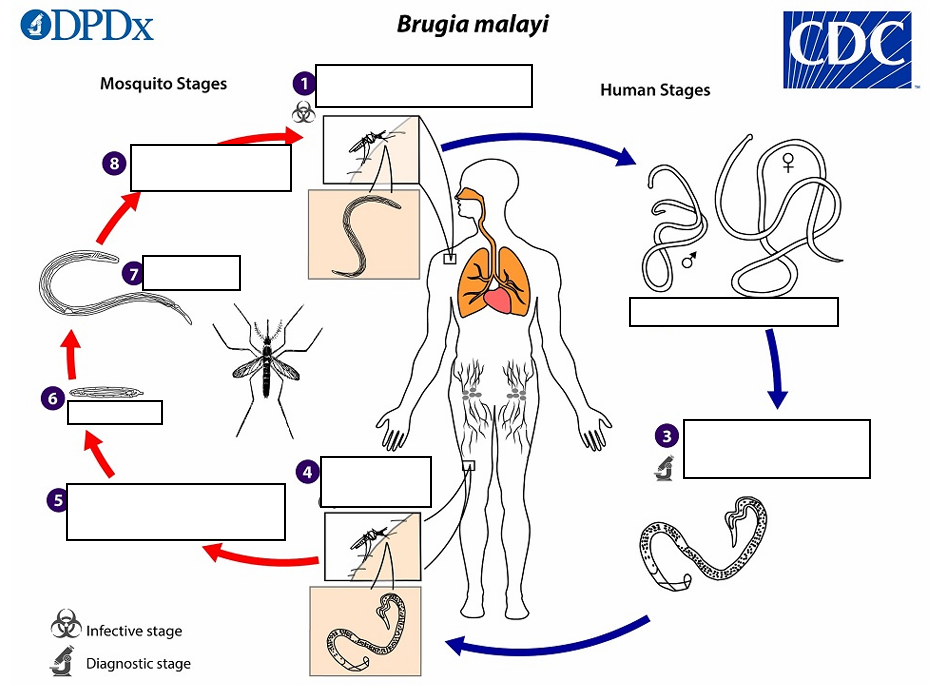
Mosquito takes a blood meal (ingests microfilariae) (B. Malayi)
(4)
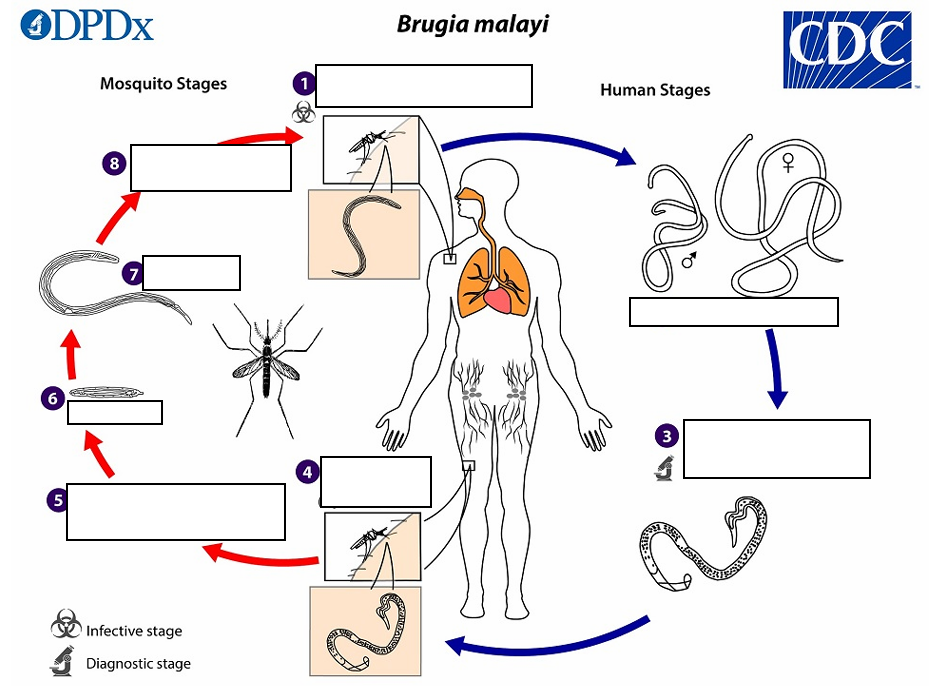
Microfilariae shed sheaths, pentrate mosquito's midgut, and migrate to thoracic muscles (B. Malayi)
(5)
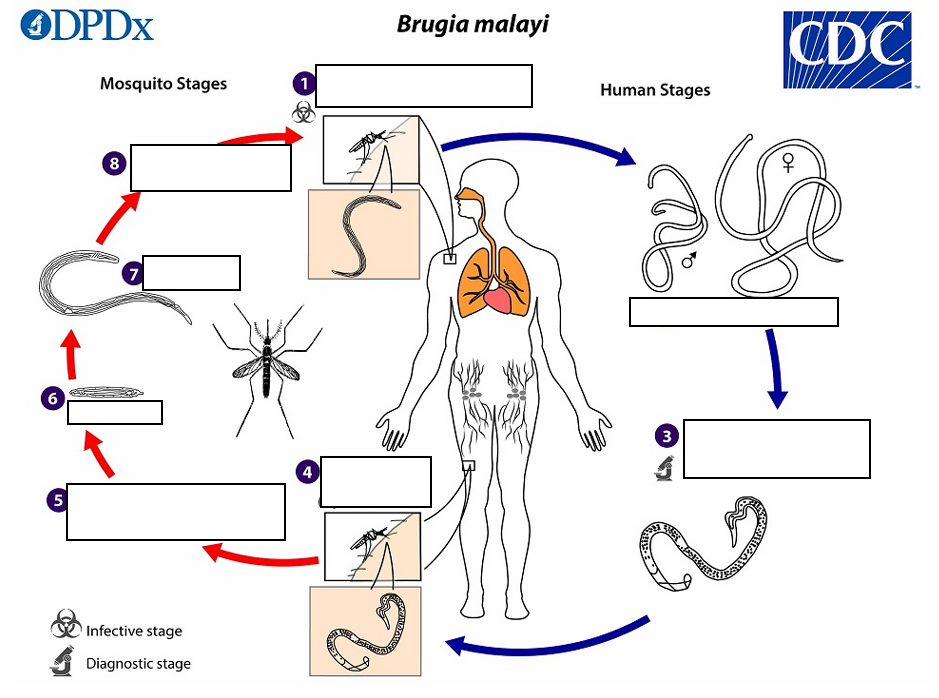
L1 larvae (B. Malayi)
(6)
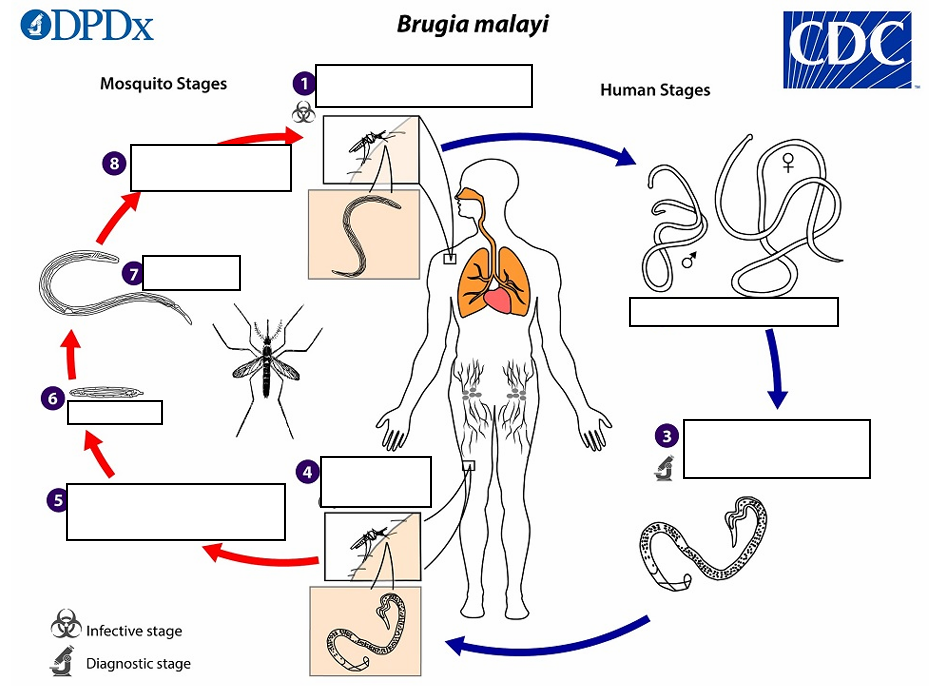
L3 larvae (B. Malayi)
(7)
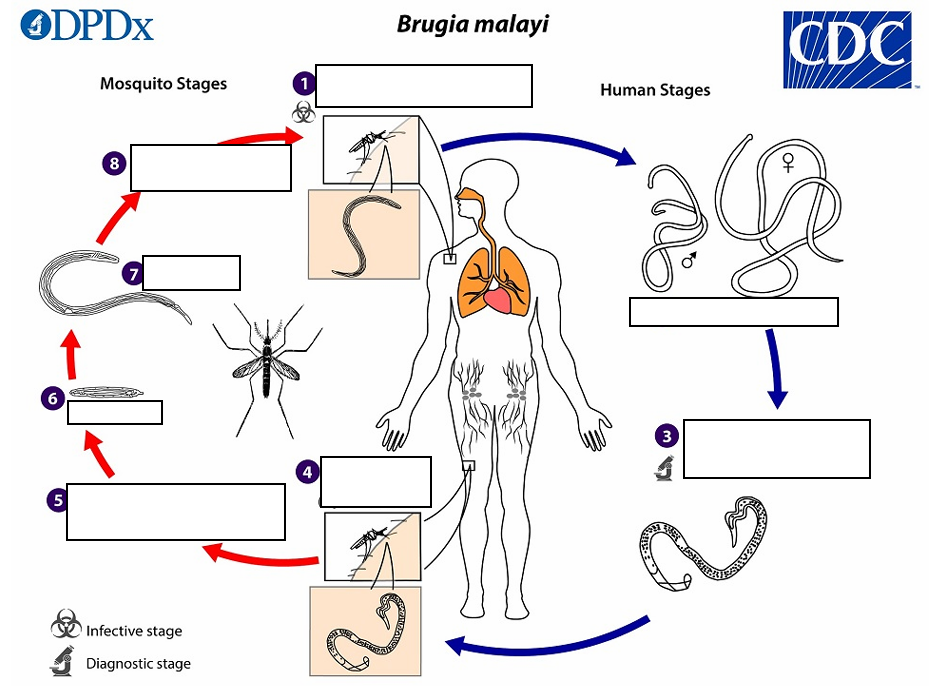
Migration to mosquito head and proboscis (B. Malayi)
(8)
filarial larvae (W. bancrofti)
During a blood meal, an infected mosquito introduces third-stage _________ onto the skin of the human host, where they penetrate into the bite wound
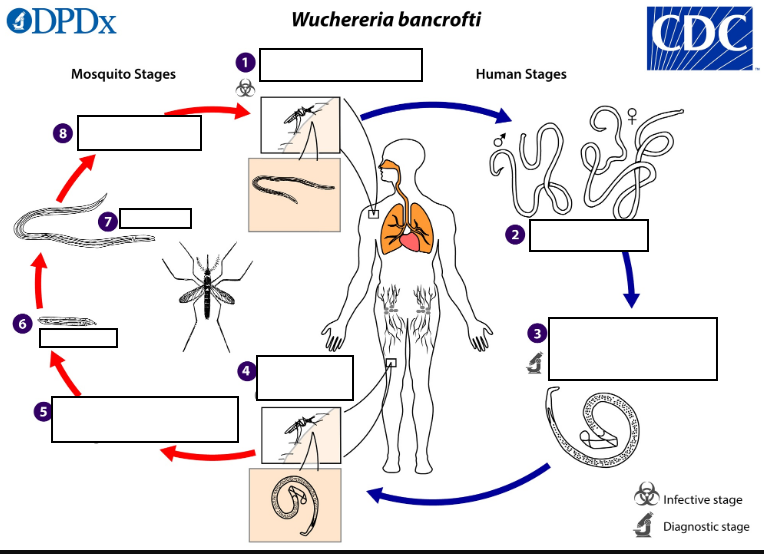
lymphatics (W. bancrofti)
(2) They develop in adults that commonly reside in the _______.
80 to 100, 0.24 to 0.30
The female worms measure in_______ mm length and ________mm in diameter,
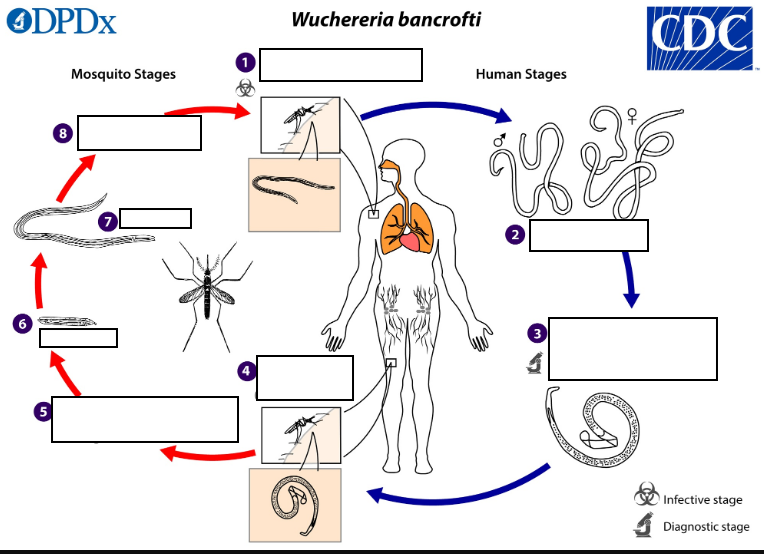
40 mm by 1 mm.
while the males measure about ____________
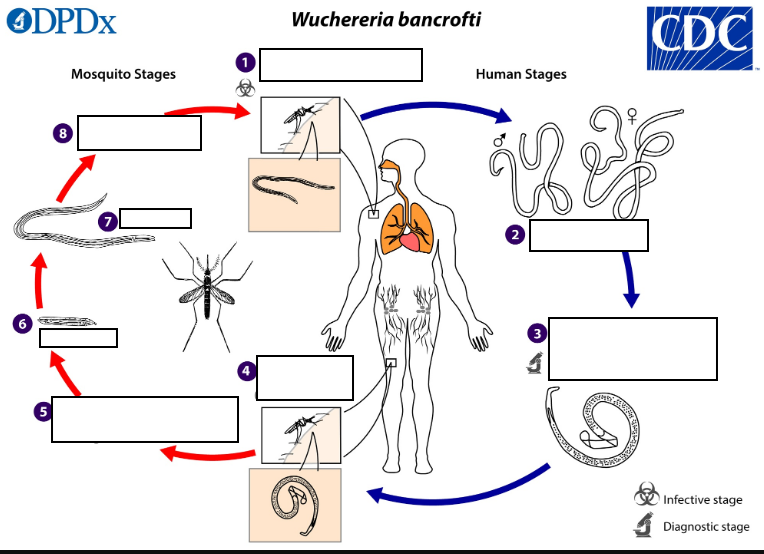
244 to 296 μm by 7.5 to 10 μm (W. bancrofti)
Adults produce microfilariae measuring _____by _______, which are sheathed and have nocturnal periodicity, except the South Pacific microfilariae which have the absence of marked periodicity.
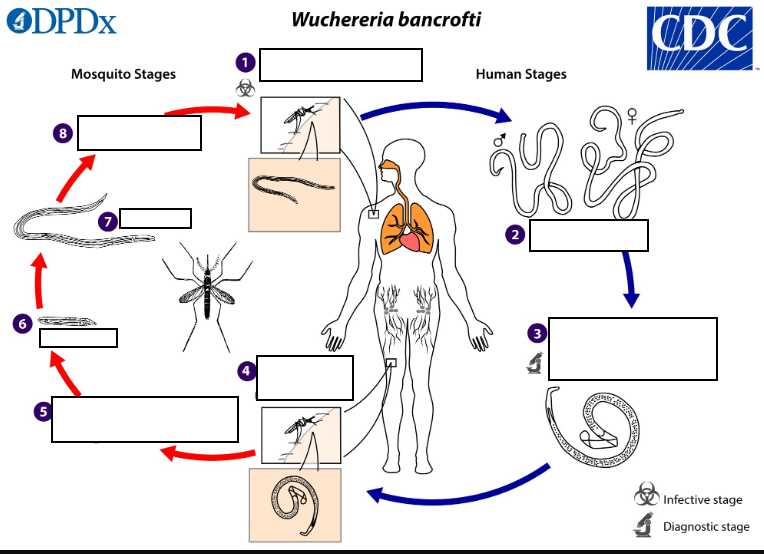
microfilariae (W. bancrofti)
The ______ migrate into lymph and blood channels moving actively through lymph and blood
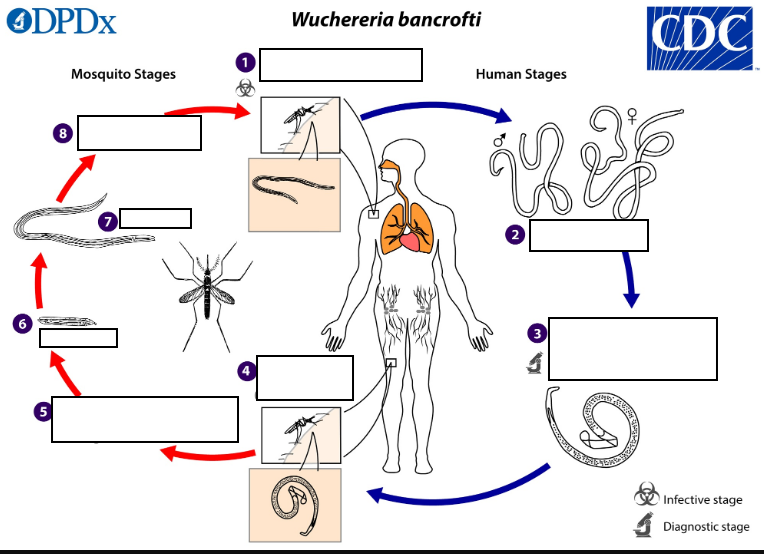
ingests the microfilariae (W. bancrofti)
A mosquito_________ during a blood meal
sheaths (W. bancrofti)
After ingestion, the microfilariae lose their __________and some of them work their way through the wall of the proventriculus and cardiac portion of the mosquito’s midgut and reach the thoracic muscles
first-stage (W. bancrofti)
(5) There the microfilariae develop into _______
third-stage (W. bancrofti)
(6) larvae and subsequently into _________
hemocoel (W. bancrofti)
(7) The third-stage infective larvae migrate through the_______ to the mosquito’s prosbocis (8) and can infect another human when the mosquito takes a blood meal
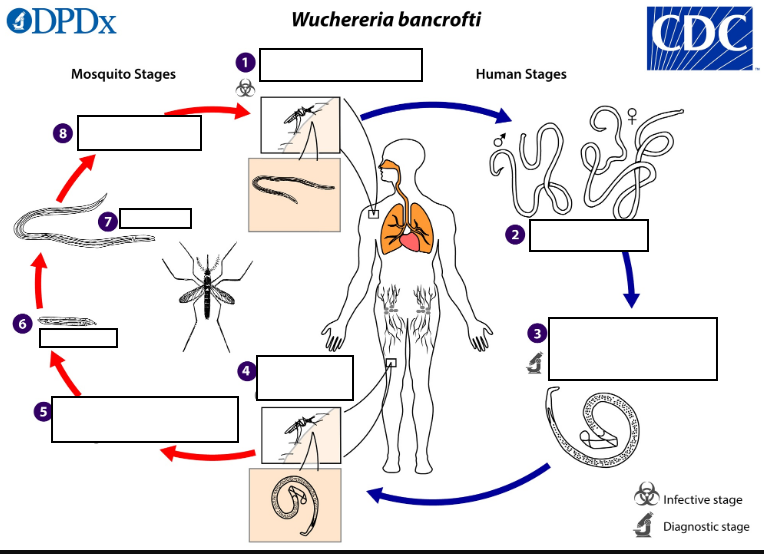
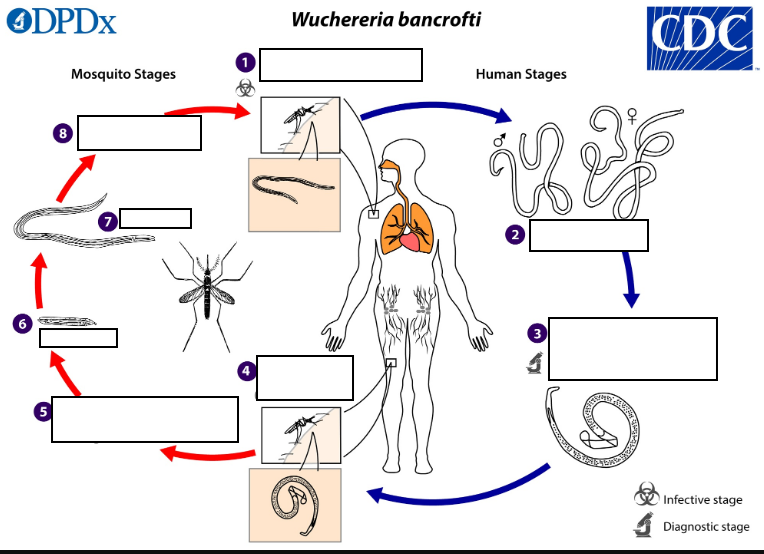
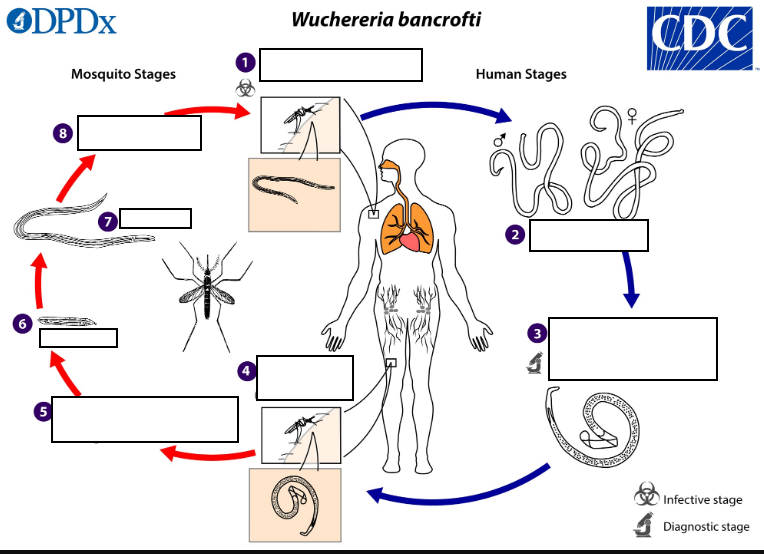
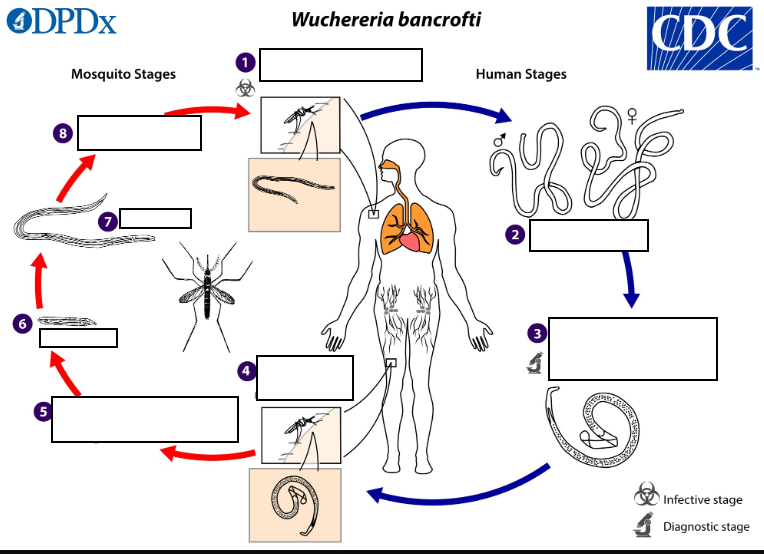
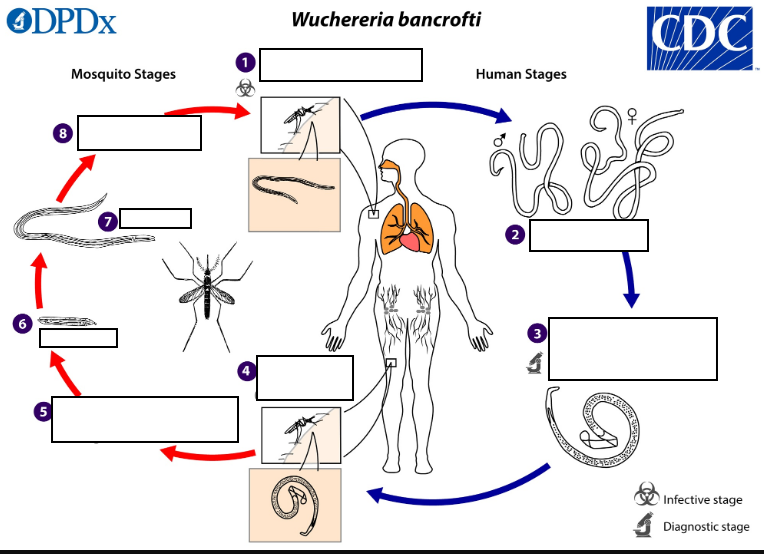
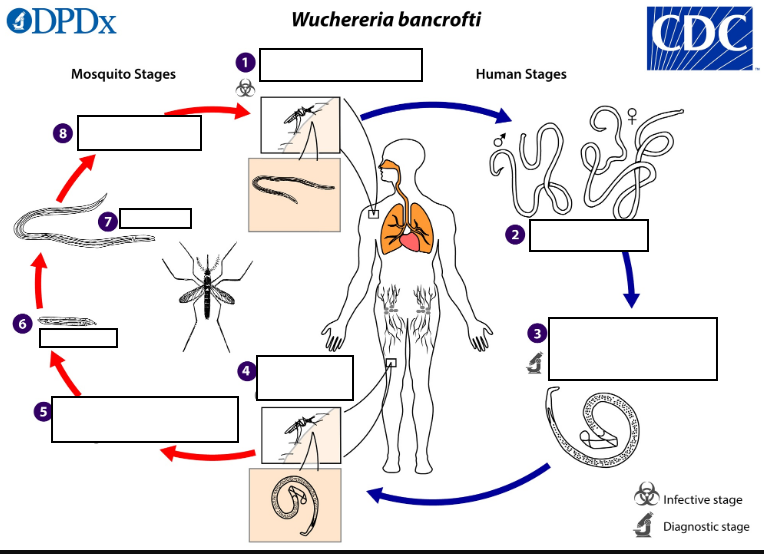
Mosquito takes a blood meal (L3 larvae enter skin) (W. bancrofti)
(1)
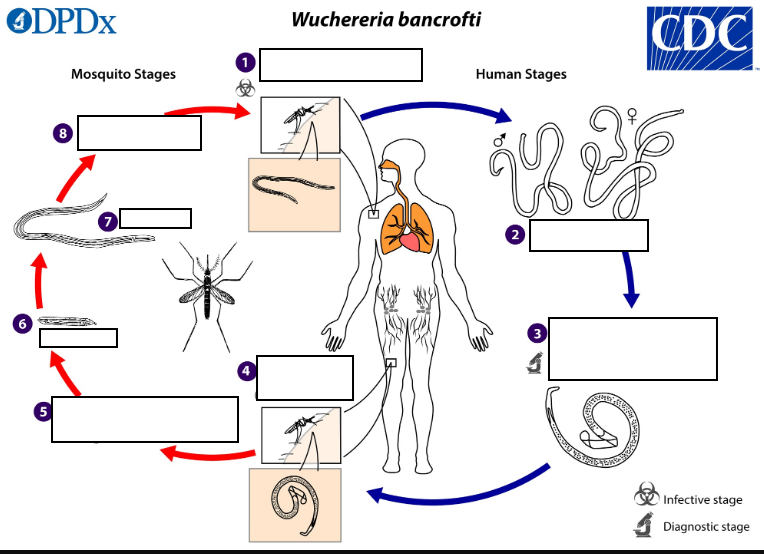
Adults in lymphatics (W. bancrofti)
(2)
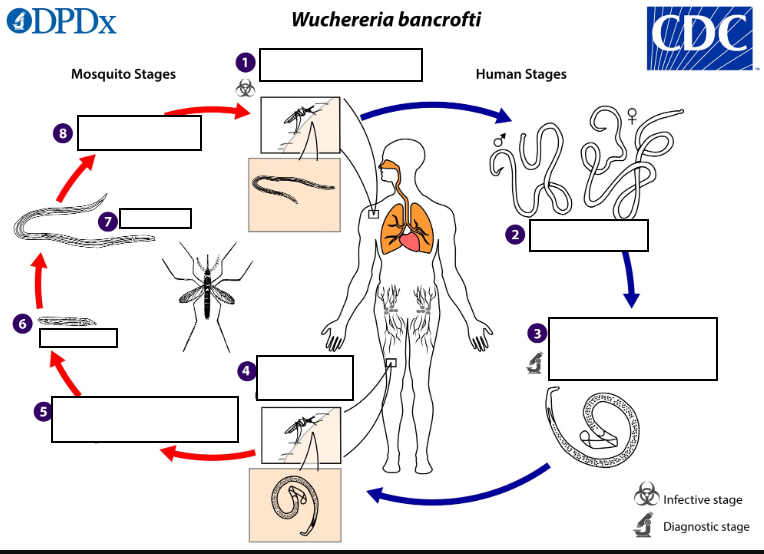
Adults produce sheathed microfilariae that migrate into lymphatic and peripheral blood circulation (W. bancrofti)
(3)
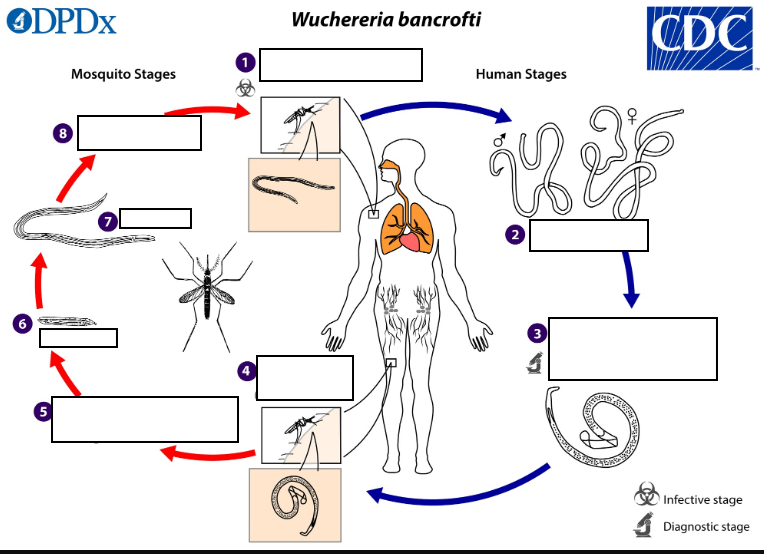
Mosquito takes a blood meal (ingests microfilariae) (W. bancrofti)
(4)
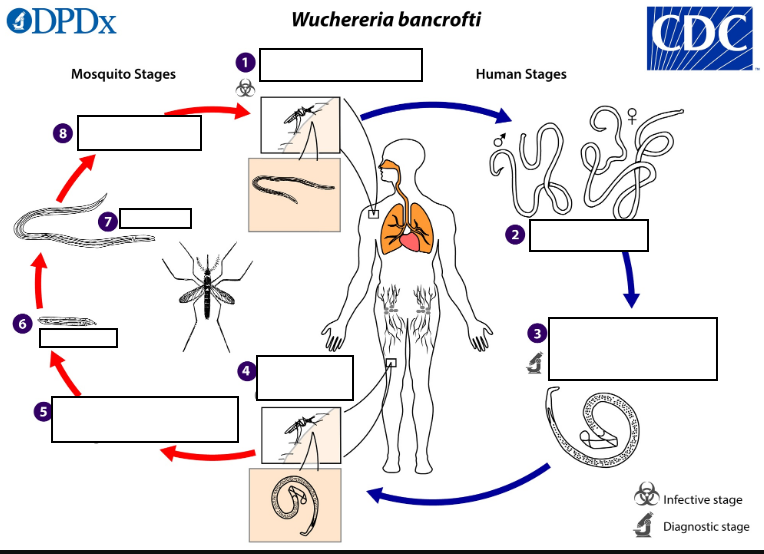
Microfilariae shed sheaths, pentrate mosquito's midgut, and migrate to thoracic muscles (W. bancrofti)
(5)
L1 larvae , L3 larvae (W. bancrofti)
(6)(7)
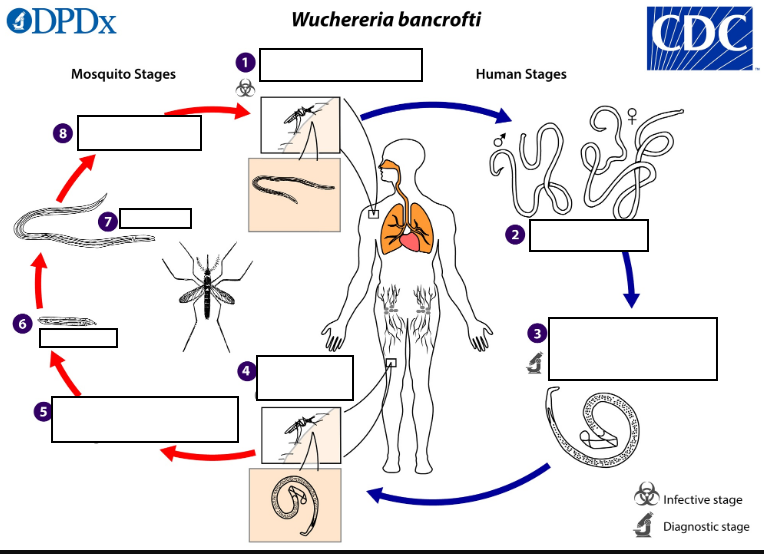
Migration to mosquito head and proboscis (W. bancrofti)
(8)
Western Pacific Island nations and territories
W. bancrofti was once widespread in tropical regions globally but control measures have reduced its geographic range. It is currently endemic throughout Sub-Saharan Africa (excluding the southern portion of the continent), Madagascar, several ________________ and parts of the Caribbean. Bancroftian filariasis also occurs sporadically in South America, India, and Southeast Asia
Brugia spp.
_________associated with LF are more geographically limited and occur only in Southeast Asia. Like W. bancrofti, control measures have reduced the occurrence and endemic range considerably. Brugia timori is restricted to the Lesser Sunda Islands of Indonesia.
LF is a potentially highly disfiguring and disabling disease
While severe manifestations do not develop in the majority of infections,_____________.
dysfunction of lymphatic vessels
The most prominent clinical feature is the development of severe lymphedema of the limbs (“elephantiasis”) and occasionally genitalia (hydrocele) due to ________.
Affected limbs become grossly swollen
_______________; the skin may become thick and pitted, and secondary infection are frequent due to lymphatic dysfunction. Scrotal hydrocele is also seen in some infected males. Lymphangitis, lymphadenopathy, and eosinophilia may accompany infection in the early stages.
tropical pulmonary eosinophilia,South and Southeast Asia
A chronic syndrome called “_____________” has been associated with W. bancrofti and B. malayi infections, involving eosinophilic pulmonary infiltrate, peripheral hypereosinophilia, wheezing, chest pain, splenomegaly, and bloody sputum. This has most frequently been documented in ____________.
Figure A: Microfilaria of W. bancrofti in a thick blood smear stained with Giemsa. Image courtesy of the Oregon State Public Health Laboratory

Giemsa or hematoxylin-and-eosin
Lymphatic filariasis is usually identified by the finding of microfilaria in peripheral blood smears (thick or thin) stained with __________ and subsequent morphologic species identification.
2% formalin
Foincreased sensitivity, concentration techniques can be used. These include centrifugation of the blood sample lysed in _________ (Knott’s technique), or filtration through a polycarbonate membrane.
nocturnal periodicity
Microfilariae of Wuchereria bancrofti and Brugia spp. exhibit a _______ and an accurate diagnosis is best achieved on blood collected at night. W. bancrofti that are sub-periodic may be encountered in some regions of the Pacific Islands, eastern Malaysia, and Vietnam.
Malaysia
Sub-periodic B. malayi also occurs in parts of ________. Adults of both species may be identified in biopsy specimens of lymphatic tissue.
immunochromatographic test
Antigen detection using an immunoassay for circulating filarial antigens constitutes a useful diagnostic approach because sensitivity for detection of microfilariae can be low and variable. Unlike microfilariae with nocturnal periodicity, filarial antigens can be detected in blood samples collected at any time of day. A rapid format _______________________ has been shown to be a useful and sensitive tool for the detection of Wuchereria bancrofti antigen and is being used widely by lymphatic filariasis elimination programs. Currently, this test is not licensed for use in the United States and cannot be used for patient diagnosis.
Serologic enzyme
________immunoassay tests, including antifilarial IgG1 and IgG4, provide an alternative to microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays