Drug excretion (Pharmacokinetics)
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
Excretion vs elimination
Excretion: remove polar drug out of body through urine by renal system.
Elimination:
process of removing drug through hepatic metabolism & excretion.
Metabolism + Excretion = Elimination
(Hepatic metabolism = non polar drugs → polar drugs for excretion easily through urine)
4 Drug excretion routes ( + 1 key feature or examples)
Renal excretion
Primary route for most drugs (incl glomerular filtration, active tubular secretion and passive reabsorption)
Biliary excretion
Secretion from liver into bile, may undergo enterohepatic circulation
Pulmonary excretion
Volatile substances like anaesthetic gases ,alcohol (ethanol)
Minor routes
Small quantities but clinically relevant
Eg: Sweat ,saliva, tears, breast milk (careful dose for lactating women)
Kidney functional and structural unit for filtering blood and forming urine.
Nephron structural and functional unit of kidney for filtering blood and forming urine
Components:
Glomerulus
Proximal convoluted tubules
Loop of Henle
Distal convoluted tubules
Collecting ducts
Renal excretion mechanism : Glomerular filtration
Passive process where drugs & their metabolites filtered through glomerular capillaries
only unbound (free) drugs can be filtered
Lipid soloubility & pH DONT influence drug passage into glomerular filtrate
Renal excretion mechanism : Active tubular secretion ( def, types of acidic/basic drugs excreted, Transport of drugs)
Active transport of drugs from blood to tubular lumen (by transporter)
Acidic drugs (salicylates, sulfonamides, penicillin) (some antibiotics)
Basic drugs (morphine, atropine, quinine)
Transport of acidic drugs can be blocked by probenecid
Renal excretion mechanism : Passive tubular reabsorption ( Ionised vs unionised drug)
Unionised, lipophilic drugs can be reabsorbed into blood circulation (low urinary excretion).
Ionised drugs poorly reabsorbed (high urinary excretion)
Glomerular filtration rate + clinical note on glomerular filtrate)
Glomerular filtration rate 125mL/min is around 20% of renal plasma flow (600mL/min)
Clinical Note: Premature infants & neonates incomplete developed secretory mechanism → may retain certain drugs in glomerular filtrate
Water soluble free drugs (unbound to plasma protein) goes into Bowmans capsule
pH- dependent reabsorption: Urine acidification vs alkalisation (How, Effect, clinical application)
Acidification of Urine
How: Use Vit C to make urine more acidic
Effect: ↑ excretion of basic drugs
Clinical: Overdose cases to enhance elimination
Alkalisation of Urine
How: Use Sodium bicarbonate (NaHCO3) make urine more alkaline
Effect: ↑ excretion of acidic drugs
Clinical: Used in salicylate poisoning
Examples of Drug classes (and drugs) excreted by kidney , % unchanged in urine and caution
Aminoglycoside antibiotics (90 → 95% excreted unchanged in urine)
Eg: Gentamicin, Tobramycin, Amikacin
Penicillins (60-90% excreted unchanged in urine)
Eg: Amoxicillin,Ampicillin
Other : Digoxin, Lithium, Metformin (Primarily eliminated through renal excretion)
Caution : Prescribe drug carefully in elderly and renal disease patients as ↓ clearance & toxicity risk
Biliary excretion (process and enterohepatic circulation (def and steps))
Process:
Drugs secreted from liver to bile by active transported into duodenum.
Occurs for limited number of drugs that are excreted into feces
Enterohepatic circulation
Def: Some drugs recycle back into systemic circulation
Drugs excreted in bile in glucouronide form hydrolysed in intestine by bacterial flora
This liberates free drugs that can be reabsorbed in blood if drug is lipid soluble
Prolongs action duration of drugs like digoxin, morphine and thyroxine
Drug clearance concepts (Drug excretion, Drug clearance, Total body clearance)
Drug excretion:
Drug movement from tissues & blood to external environment
Drug clearance (CL):
Apparent vol (mL,L) blood cleared of drug per unit time (min,h)
Total body clearance:
CL total = CLhepatic + CLrenal + CLpulmonary + CLother
Hepatic and renal most imp (kidney often major organ of excretion mainly kidney but liver significant through metabolism or excretion into bile)
Factors affecting drug clearance (Hepatic CL, Renal CL, Patient)
Hepatic clearance factors
Hepatic blood flow (↓ in congestive heart failure)
Hepatic enzyme activity (affected by liver failure, drug inhibition, drug induction)
Plasma protein binding (only free drug metabolised)
Renal clearance factors
Kidney blood flow (↓ in congestive heart failure)
Secretion blockers (aspirin, probenecid)
Glomerular filtration rate (↓ in renal disease)
Urine pH (affects reabsorption)
Patient factor
Age ( elderly & newborns have ↓clearance)
Genetic variations in drug-metabolising enzymes
Disease states affecting liver or kidney function
Plasma protein binding (affects available drug)
Plasma ½ life (Def, Clinical significance, factors ↑ ½ life)
Def: Time needed for plasma conc of drug to be ½ initial conc
Clinical significance:
Measure action duration
determine drug dosing interval
Short ½ life drugs (eg: penicillin) more frequent dosing
Long ½ life drugs (eg: digoxin, thyroxine) less frequent dosing
Factors ↑ ½ life
↓ metabolism ( liver disease, enzyme inhibitors…)
↓ clearance ( renal disease, heart disease…)
↑ protein/tissue binding
Enterohepatic cycling
Multiple dosing and steady state conc (when ssc attained)
Multiple Dosing concept:
Most drug administered regularly over time period (not single dose) so drug accumulates in body till steady state reached.
Steady state concentration
State which therapeutic plasma conc is constant
Steady state conc: Rate drug administered = Rate of elimination
Steady state conc attained after (3 to) 5 half lives
Eg: Morphine with ½ life of 3 hrs reach steady state in 9-15 hrs
Loading dose (Def, Purpose, Clinical application incl eg)
Def: Large initial dose to rapidly achieve therapeutic plasma levels
Purpose:
Balance drug distribution to other tissue
Particularly Important for drugs with long ½ lives
Quick therapeutic levels if waiting for steady state would be too long
Clinical application
Rapid relief is required and waiting for steady state would be too long
Eg: Lidocaine (antiarrythmic drug) with t ½ of 1-2 hrs given a loading dose for life threatening arrhythmias after myocardial infarction
Maintenance doses (Def + features + 1 clinical example)
Def: Dose required to maintain therapeutic level of drug constant or maintain steady state of drug
Features
Balance drug loss during metabolism & clearance
Regular dosing intervals based on drug ½ life.
Clinical example
Amoxicillin 500mg every 8hrs to maintain therapeutic levels
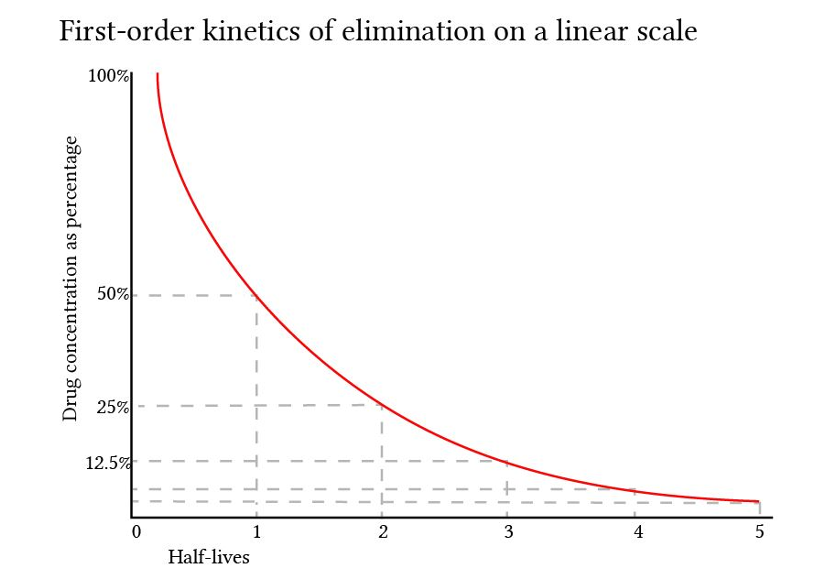
Elimination Kinetics: First-Order elimination kinetics
1st order kinetics AKA non-saturable or linear kinetics
Def: Elimination directly proportional to drug conc
(higher drug conc = higher elimination rate)
Most drugs (95% therapeutic drugs) eliminated by 1st order kinetic
Zero order elimination kinetics
0 order elimination kinetics AKA saturable or dose independent
Rate of elimination occur independently of drug conc in body
( incr drug conc NOT equal increase elimination)
order 0 elimination rare mostly occurring when saturated elimination system (Large doses)
Examples : Ethanol , Aspirin, Phenytoin, Warfarin, Theophylline

Equations for Assessment of drug clearance:
Kel (constant rate of elimination), Plasma CL (mL/kg/min)
Kel (constant rate of elimination) = 0.693÷ t½
Plasma clearance (mL/kg/min) = Vd x Kel