Bio 1.5 Endocrine system
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
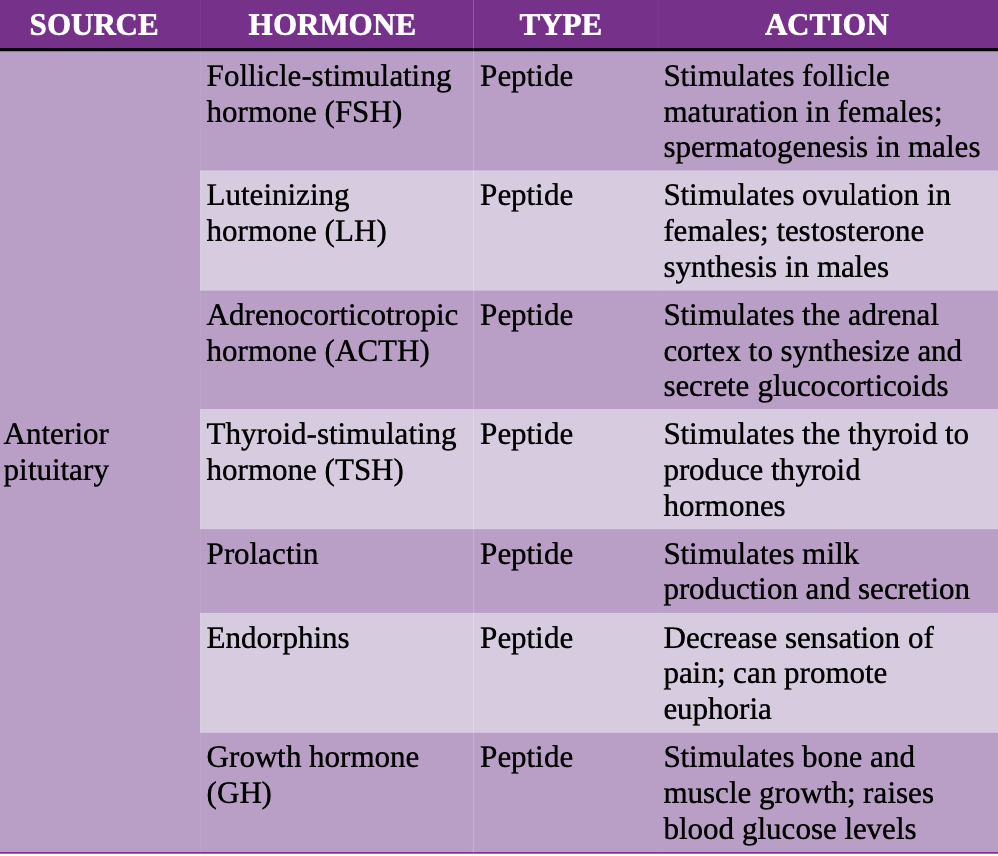
endocrine signalling
involves the secretion of hormones directly into the bloodstream. The hormones travel to distant target tissues, where they bind to receptors and induce a change in gene expression or cell function.
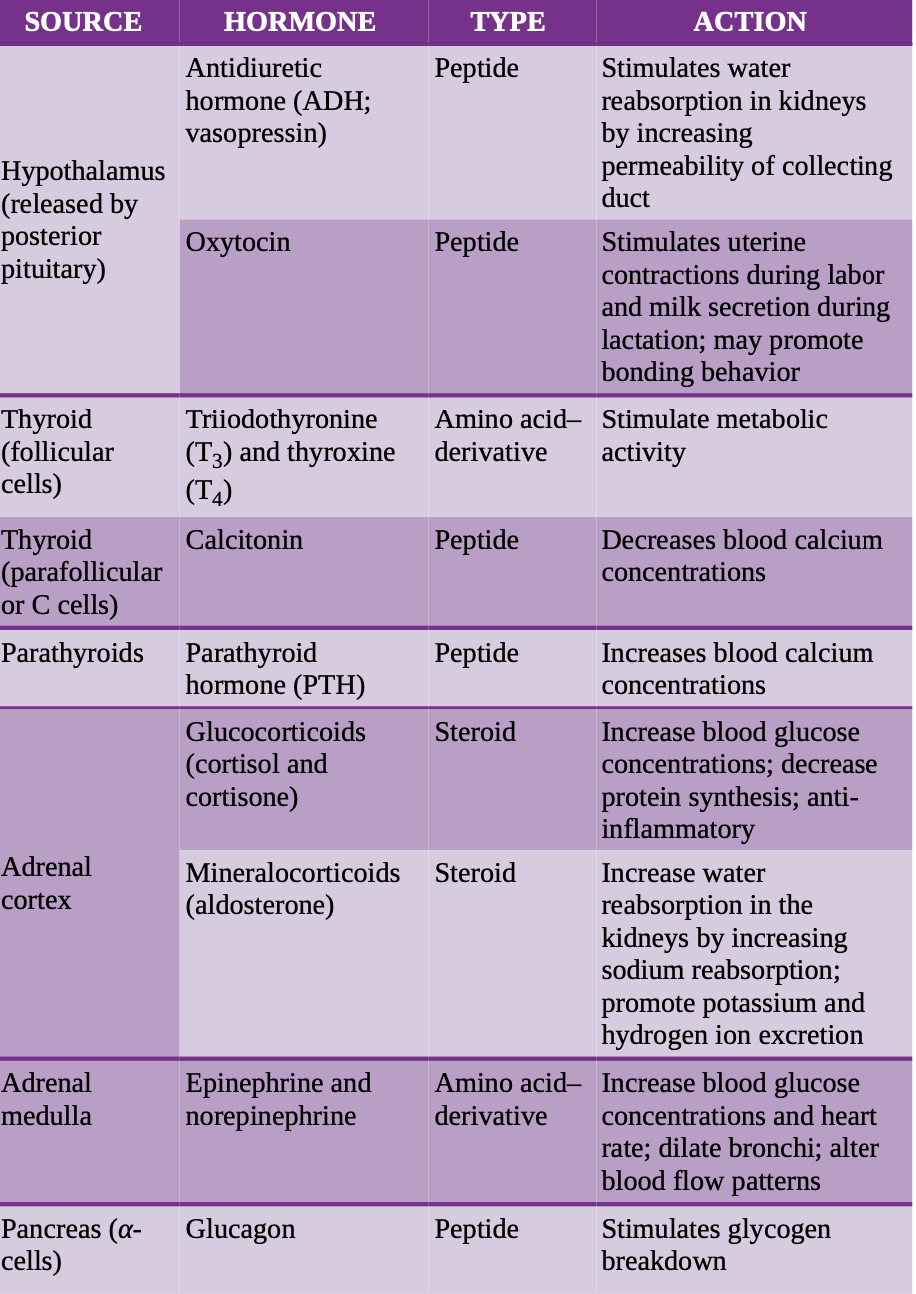
Peptide hormones
are composed of amino acids and are derived from larger precursor proteins that are cleaved during posttranslational modification.
Peptide hormones are polar and cannot pass through the plasma membrane.
These hormones bind to extracellular receptors, where they trigger the transmission of a second messenger.
eg cAMP, IP3 and calcium
Each step of the signaling cascade can induce amplification of the signal. [each stope can result in increase intensity]
Peptide hormones exert effects that usually have rapid onset but are short lived.
These hormones are water-soluble, so they travel freely in the bloodstream and do not require a special carrier.
smaller units are transported to golgi apparatus for further modifications that activate the hormone, released via exocytosis
GPCR
when a peptide hormones binds to a GPCR it triggers the receptor to activate or inhibit adenylate cyclase > raising or lowering the levels of cAMP accordingly.
cAMP can bind to intracellular targets such as protein kinase A which phosphorylates transcription factors like cAMP response to exert the hormone’s ultimate effect
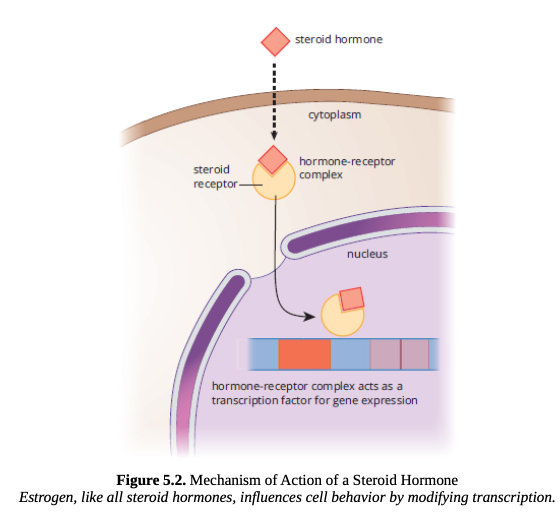
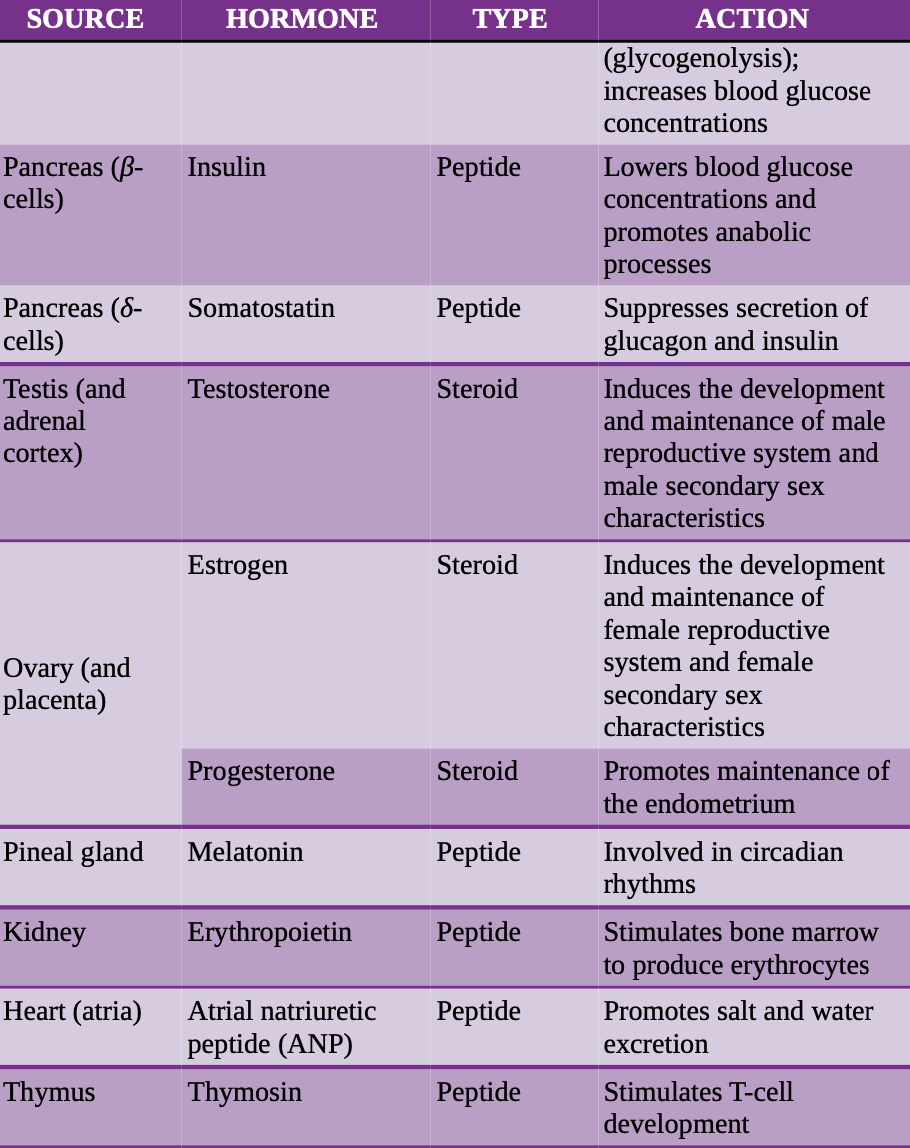
steroid hormones
derived from cholesterol.
Steroid hormones are minimally polar and can pass through the plasma membrane. hence their receptors are intracellular (in they cytosol) or intranuclear (in the nucleus)
These hormones bind to and promote a conformational change in cytosolic or intranuclear receptors; the hormone–receptor complex binds to DNA, altering the transcription of a particular gene.
eg dimerization (pairing of 2 receptor hormone complexes)
Steroid hormones exert effects that usually have slow onset but are long- lived.
Because these hormones are lipid-soluble, they cannot dissolve in the bloodstream and must be carried by specific proteins.
hormones are generally inactive while attached to a carrier protein and must dissociate from the carrier to function.
AA derivative hormones
are modified amino acids.
Their chemistry shares some features with peptide hormones and some features with steroid hormones; different amino acid–derivative hormones share different features with these other hormone classes.
Common examples are epinephrine, norepinephrine [bind to GPCRs], triiodothyronine, and thyroxine.[bind intracellularly]
Hormones can be classified by their target tissues.
direct vs tropic hormones
direct hormones
have major effects on non-endocrine tissues
act directly on target tissue
tropic hormones
have major effects on other endocrine tissues.
require an intermediary to act
usually originate in the brain
most steroid hormones
–one, –ol, or –oid
most peptide hormones
–in or –ine
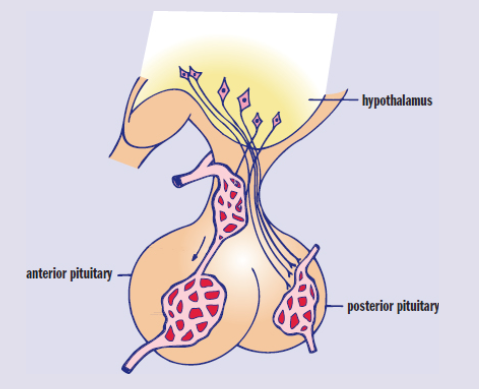
hypothalamus
is the bridge between the nervous and endocrine systems.
The release of hormones from the hypothalamus is mediated by a number of factors, including projections from other parts of the brain, chemo- and baroreceptors in the blood vessels, and negative feedback from other hormones.
hypothalamus controls the pituitary through paracrine release of hormones into a portal system that directly connects the 2 organs.
negative feedback
final hormone (or product) of a pathway inhibits hormones (or enzymes) earlier in the pathway, maintaining homeostasis.
anterior pituitary
The hypothalamus stimulates the anterior pituitary gland through paracrine release of hormones into the hypophyseal portal system, which directly connects the two organs.
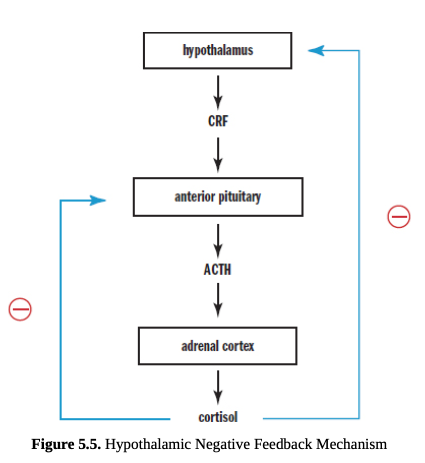
hypothalamic–pituitary–adrenal (HPA) axis
a crucial neuroendocrine system that regulates the body's stress response, involving the hypothalamus, pituitary gland, and adrenal glands, and plays a vital role in maintaining homeostasis and responding to stress.
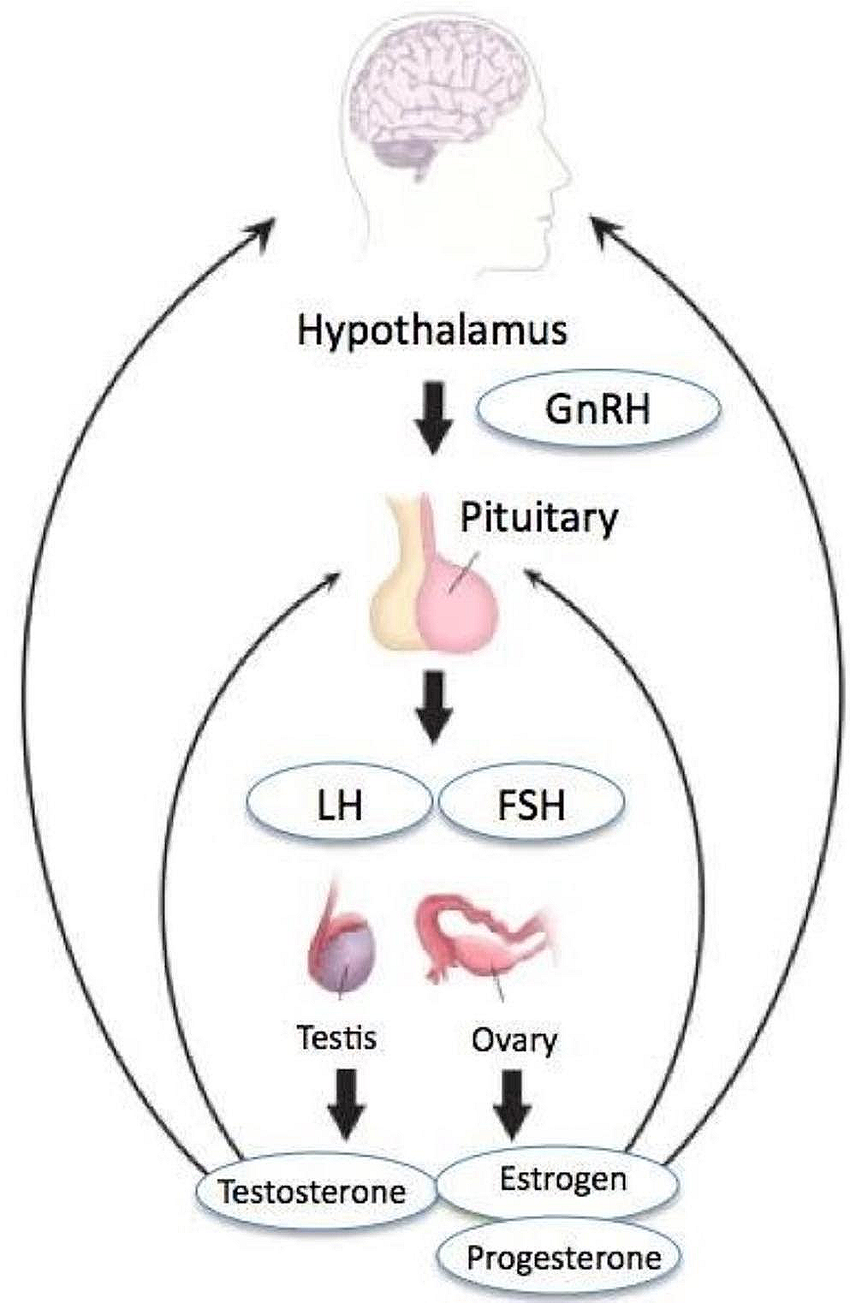
hypothalamic–pituitary–ovarian (HPO) axis
a complex system that regulates the female reproductive cycle, involving the hypothalamus, pituitary gland, and ovaries, with hormones like GnRH, FSH, LH, estrogen, and progesterone playing key roles.
Gonadotropin-releasing hormone (GnRH)
promotes the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Growth hormone–releasing hormone (GHRH)
promotes the release of growth hormone.
[AP] Thyroid-releasing hormone (TRH)
promotes the release of thyroid- stimulating hormone (TSH).
Corticotropin-releasing factor (CRF)
promotes the release of adrenocorticotropic hormone (ACTH).
Prolactin-inhibiting factor (PIF or dopamine)
inhibits the release of prolactin.
posterior pituitary
interactions with the posterior pituitary occur via the axons of nerves projected by the hypothalamus directly.
eg Antidiuretic hormone (ADH or vasopressin) and oxytocin are synthesized in the hypothalamus and then travel down these axons to the posterior pituitary, where they are released into the bloodstream.
[AP] FSH
promotes the development of ovarian follicles in females and spermatogenesis in males.
[AP] LH
promotes ovulation in females and testosterone production in males.
[AP] ACTH
promotes the synthesis and release of glucocorticoids from the adrenal cortex.
[AP] TSH
promotes the synthesis and release of triiodothyronine and thyroxine from the thyroid.
[AP] prolactin
promotes milk production.
Prolactin is an unusual hormone in that the release of dopamine from the hypothalamus decreases its secretion
[AP] endorphins
decrease perception of pain and can produce euphoria.
[AP] Growth hormone (GH)
promotes growth of bone and muscle and shunts glucose to these tissues. It raises blood glucose concentrations
is energetically expensive and requires large quantities of glucose. Growth hormone prevents glucose uptake in certain tissues (those that are not growing) and stimulates the breakdown of fatty acids. This increases the availability of glucose overall, allowing muscle and bone to use it. GH release is stimulated by growth hormone–releasing hormone (GHRH) from the hypothalamus.
An excess of GH released in childhood (before this closure) can cause gigantism, and a deficit results in dwarfism. In adults, the situation is slightly different. Because the long bones are sealed, GH still has an effect, but it is primarily in the smaller bones.
![<p>[Posterior] ADH </p>](https://knowt-user-attachments.s3.amazonaws.com/9cfa45d0-8bc5-4266-8dce-3a27b9a12dca.png)
[Posterior] ADH
is secreted in response to low blood volume (as sensed by baroreceptors) or increased blood osmolarity (as sensed by osmoreceptors) and increases reabsorption of water in the collecting duct of the nephron, increasing blood volume and decreasing blood osmolarity.
[Posterior] Oxytocin
is secreted during childbirth and promotes uterine contractions. It also promotes milk ejection and may be involved in bonding behavior. It is unusual in that it has a positive feedback loop, not negative.
thyroid
is located at the base of the neck in front of the trachea; it produces three key hormones.
T3
T4
calcitonin
setting basal metabolic rate and promoting calcium homeostasis
![<p>[thyroid] T3 (<span><strong>Triiodothyronine</strong></span>) , T4 (<span><strong>thyroxine</strong></span>)</p>](https://knowt-user-attachments.s3.amazonaws.com/aacbcf8f-7d59-4952-9da1-d5670ec7aa8b.png)
[thyroid] T3 (Triiodothyronine) , T4 (thyroxine)
are produced by follicular cells and contain iodine. (iodinationation of the amino acid tyrosine in the follicular cells of the thyroid)
They increase basal metabolic rate and alter the utilization of glucose and fatty acids.
increased T3 and T4 lead to increasse cellular respiration.
Thyroid hormones are required for proper neurological and physical development in children.
hypothyroidism
deficiency of iodine or inflammation of the thyroid
thyroid hormones are secreted in insufficient amounts or not at all. The condition is characterized by lethargy, decreased body temperature, slowed respiratory and heart rate, cold intolerance, and weight gain.
hyperthyroidism
which may result from a tumor or thyroid overstimulation
heightened activity level, increased body temperature, increased respiratory and heart rate, heat intolerance, and weight loss.
[thyroid] calcitonin
is produced by parafollicular (C) cells. It decreases plasma calcium concentration by promoting calcium excretion in the kidneys, decreasing calcium absorption in the gut, and promoting calcium storage in bone.
Calcitonin tones down calcium levels in the blood.
![<p>[parathyroid glands] PTH </p>](https://knowt-user-attachments.s3.amazonaws.com/2f7db8bb-18c6-445c-a7f0-99e8e74fc6e3.png)
[parathyroid glands] PTH
The parathyroid glands release parathyroid hormone (PTH), which increases blood calcium concentration.
PTH decreases excretion of calcium by the kidneys and increases bone resorption directly to increase blood calcium concentration.
PTH activates vitamin D, which is necessary for calcium and phosphate absorption from the gut.
PTH promotes resorption of phosphate from bone and reduces reabsorption of phosphate in the kidney, but vitamin D promotes absorption of phosphate from the gut; these two effects on phosphate concentration somewhat cancel each other out.
PTH is also subject to feedback inhibition.
calcium
is an exceptionally important ion. The critically important functions of calcium include:
Bone structure and strength
Release of neurotransmitters from neurons
Regulation of muscle contraction
Clotting of blood (calcium is a cofactor)
plays a role in cell movement and exocytosis of cellular materials.
adrenal cortex
located on top of the kidneys. Each adrenal gland consists of a cortex and a medulla
produces three classes of steroid hormones.
Glucocorticoids
Mineralocorticoids
Cortical sex hormones
[adrenal cortex] Glucocorticoids
regulate glucose levels and affect protein metabolism
such as cortisol and cortisone increase blood glucose concentration (by increasing gluconeogensis), reduce protein synthesis, inhibit the immune system, and participate in the stress response.
Glucocorticoid release is stimulated by ACTH.
[adrenal cortex] mineralocorticoids
such as aldosterone promote sodium reabsorption in the distal convoluted tubule and collecting duct, thus increasing water reabsorption. Aldosterone also increases potassium and hydrogen ion excretion. Aldosterone activity is regulated by the renin–angiotensin– aldosterone system, not ACTH.
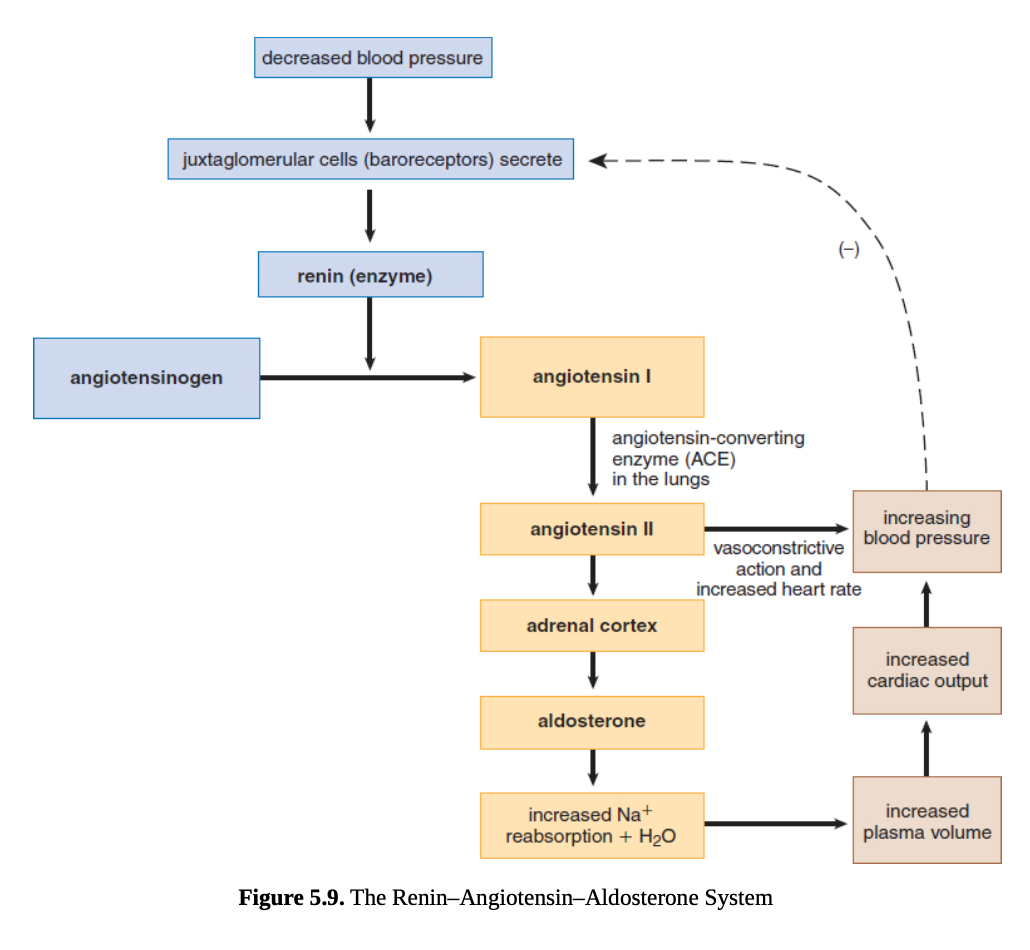
RAAS
Decreased
blood pressure causes the juxtaglomerular cells of the kidney to secrete renin,
which cleaves an inactive plasma protein, angiotensinogen, to its active form,
angiotensin I. Angiotensin I is then converted to angiotensin II by angiotensin-
converting enzyme (ACE) in the lungs. Angiotensin II stimulates the adrenal
cortex to secrete aldosterone. Once blood pressure is restored, there is a decreased drive to stimulate renin release, thus serving as the negative feedback
mechanism for this system.
[adrenal cortex] cortical sex hormone
include androgens (like testosterone) and estrogens in both males and females.
adrenal medulla
is derived from the nervous system and secretes catecholamines into the bloodstream.
production of the sympathetic hormones epinephrine and norepinephrine
[adrenal medulla] catecholamines
include epinephrine and norepinephrine, which are involved in the fight-or-flight (sympathetic) response.
These hormones promote glycogenolysis, increase the basal metabolic rate, increase heart rate, dilate the bronchi, and alter blood flow.
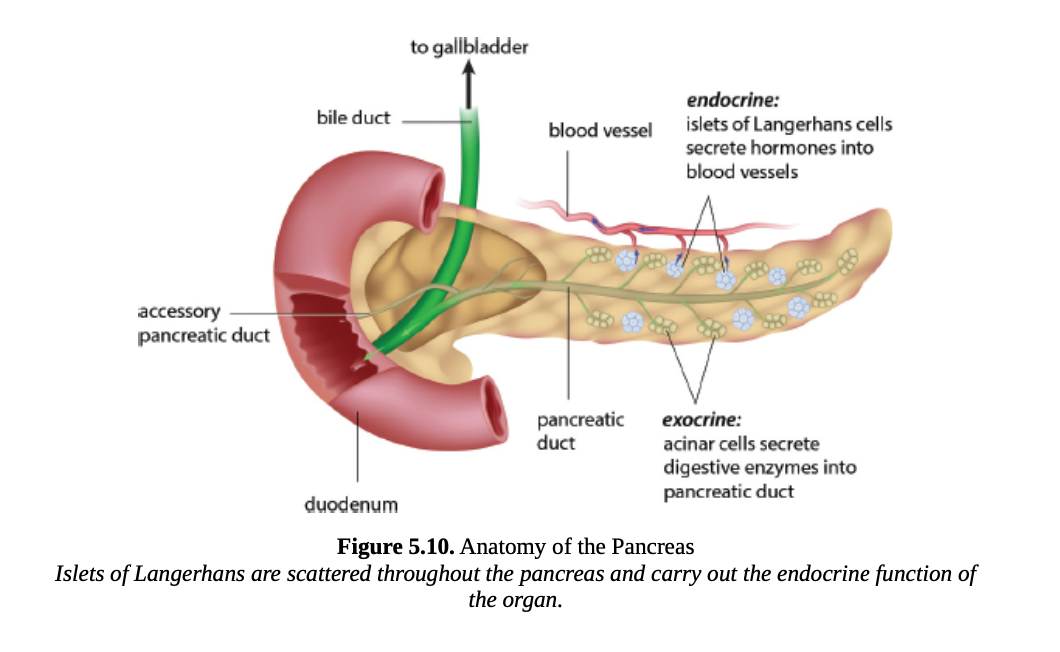
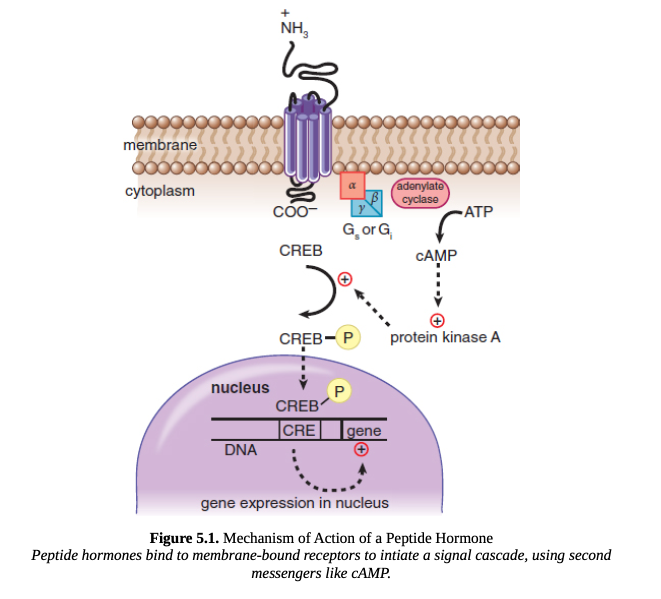
pancreas
produces hormones that regulate glucose homeostasis.
α-cells
β-cells
δ-cells
[pancreas] alpha cells
Glucagon is produced by α-cells and raises blood glucose levels by stimulating protein and fat degradation, glycogenolysis, and gluconeogenesis.
Glucagon levels are high when glucose is gone.
![<p>[pancreas] beta cells </p>](https://knowt-user-attachments.s3.amazonaws.com/676c6753-3633-41ad-95e4-45c2c7f62df8.png)
[pancreas] beta cells
insulin is produced by β-cells and lowers blood glucose levels by stimulating glucose uptake by cells and promoting anabolic processes, like glycogen, fat, and protein synthesis.
hypoglycemia
characterized by low blood glucose concentration
diabetes mellitus
excess glucose in the blood
type 1 and type 2
diabetes mellitus type 1
Type I (insulin-dependent) diabetes
mellitus is caused by autoimmune destruction of the β-cells of the pancreas,
resulting in low or absent insulin production. People who have type I diabetes
require regular injections of insulin to prevent hyperglycemia and to permit
uptake of glucose into cells.
diabetes mellitus type 2
(non-insulin-dependent) diabetes mellitus is
the result of receptor-level resistance to the effects of insulin. Type II diabetes
mellitus is partially inherited and partially due to environmental factors, such as
high-carbohydrate diets and obesity.
polyuria
increased frequency of urination
polydipsia
increased thirst
[pancreas] S cells
Somatostatin is produced by δ-cells and inhibits insulin and glucagon secretion.
High blood glucose and amino acid concentrations stimulate its secretion.
gonads
produce hormones that are involved in the development and maintenance of the reproductive systems and secondary sex characteristics.
eg testes, ovaries
[gonads] testes
secrete testosterone promotes the development and maintenance of secondary sex characteristics in males
[gonads] ovaries
secrete estrogen and progesterone development of the female reproductive system during gestation and also promotes the development and maintenance of secondary sex characteristics in females
pineal gland
releases melatonin, which helps to regulate circadian rhythms.
kidneys
secrete erythropoietin, which stimulates bone marrow to produce erythrocytes (red blood cells) in response to low oxygen levels in the blood.
atria of the heart
secrete atrial natriuretic peptide (ANP), which promotes excretion of salt and water in the kidneys in response to stretching of the atria (high blood volume).
thymus
secretes thymosin, which is important for proper T-cell development and differentiation.