A&P1- Exam 2
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What is the Nervous System?
A complex, highly organized network of billions of neurons and neuroglia, along with supporting blood vessels and connective tissue.
What are the major structures of the Nervous System?
Brain: housed within the skull.
Contains 100 billion neurons.
Cranial nerves and their branches: 12 pairs of cranial nerves (I-XII)
The cranial nerves emerge from the base of the brain.
Nerve: a nerve is a bundle containing 100-1000s of axons plus associated connective tissue and blood vessels.
Each nerve follows a defined path and serves a specific region of the body.
Spinal cord: connects to the brain through the foramen magnum of the skull.
It is encircled by the bones of the vertebral column.
It contains about 100 million neurons.
Spinal nerves and their branches: 31 pairs of spinal nerves.
The spinal nerves emerge from the spinal cord, each serving a specific region on the right or left side of the body.
Enteric plexuses: extensive networks of neurons found in the walls of organs of the digestive tract.
The enteric plexus helps regulate the digestive system.
What are the basic functions of the Nervous System?
The Nervous System integrates, processes, and correlates incoming sensory information and outgoing motor commands. It is the source of thoughts, emotions, and memories, and most nerve impulses that stimulate muscles and glands originate here.
What are the two major divisions of the Nervous System?
- Central Nervous System (CNS)
- Peripheral Nervous System (PNS)
Define the Central Nervous System (CNS).
Contains neural tissue, blood vessels, and connective tissue. It includes the Brain and Spinal Cord.
What are the functions of the CNS?
- Integrates, processes, and correlates different types of incoming sensory information and outgoing motor commands.
- Source of thoughts, emotions, and memories (learning/intelligence).
- Most nerve impulses for muscle contraction and gland secretion originate here.
Define the Peripheral Nervous System (PNS).
Includes all nervous tissue outside the CNS and serves as communication lines.
Which structures belong to the Peripheral Nervous System (PNS)?
- Cranial nerves and their branches
- Spinal nerves and their branches
- Ganglia
- Sensory receptors
What are the two divisions of the Peripheral Nervous System (PNS)?
- Sensory (afferent) division
- Motor (efferent) division
Describe the Sensory (afferent) division.
Made up of nerve fibers that convey impulses to the CNS from sensory receptors located throughout the body.
What is the role of somatic afferent fibers?
Transmitting sensory information from the body's surface and deeper structures (skin, skeletal muscles, joints) to the central nervous system. They relay information about touch, pain, temperature, and proprioception.
What are the roles of visceral afferent fibers?
Transmitting sensory information from internal organs (viscera) to the central nervous system. This information is vital for maintaining homeostasis and regulating various bodily functions.
Describe the Motor (efferent) division.
Transmits impulses from the CNS to effector organs (muscles, glands). Its two main divisions are the Somatic Nervous System (SNS) and the Autonomic Nervous System (ANS).
What is the role of the Somatic Nervous System (SNS)?
Controls skeletal muscle contractions and is considered voluntary. It consists of somatic motor neurons from the CNS that conduct impulses to skeletal muscles.
What is the role of somatic motor neurons?
Transmitting signals from the central nervous system (brain and spinal cord) to skeletal muscles, enabling voluntary movements. They act as messengers translating the brain's commands into physical actions.
What is the role of the Autonomic Nervous System (ANS)?
Allows automatic regulation of smooth muscles, cardiac muscle, and gland secretions at the subconscious level, meaning its actions are involuntary. It consists of visceral motor neurons from the CNS that conduct nerve impulses to smooth muscle, cardiac muscle, glands, and adipose tissue.
What are the two major divisions of the Autonomic Nervous System?
- Sympathetic Division (fight or flight)
- Parasympathetic Division (fed and rest)
What is the role of visceral motor neurons?
Control involuntary functions of the body, such as heart rate, digestion, and breathing. They are a key component of the autonomic nervous system and innervate smooth muscle, cardiac muscle, and glands.
What structures do the somatic afferent fibers (neurons) innervate?
They innervate skeletal muscles, which control voluntary muscle movements.
What structures do the visceral afferent fibers (neurons) innervate?
They innervate involuntary (smooth) muscles, cardiac muscle, and glands, regulating the internal environment of the body (e.g., heart rate, digestion, gland secretions) for homeostasis.
What is the function of the Enteric Nervous System (ENS)?
Also known as the "brain of the gut," it consists of neurons in enteric plexuses that extend the entire length of the gastrointestinal tract. Many act independently of the ANS and CNS, though they communicate with the CNS via sympathetic and parasympathetic neurons.
Relate the terms voluntary and involuntary to the various subdivisions of the Nervous System (NS).
- Somatic Nervous System (SNS): Voluntary, controls skeletal muscles.
- Autonomic Nervous System (ANS): Involuntary, controls smooth muscle, cardiac muscle, and glands.
- Sympathetic Division (ANS): Involuntary, manages stress responses (fight or flight).
- Parasympathetic Division (ANS): Involuntary, supports resting functions (rest and digest).
What are Neurons?
The excitable nerve cells that transmit electrical signals. They have the property of electrical excitability.
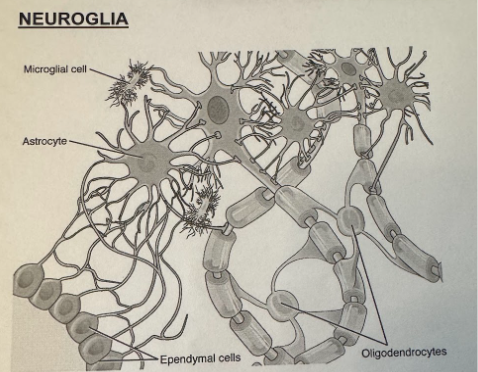
What are Neuroglia (Supporting cells)?
Smaller, supporting cells that surround and wrap the more delicate neurons. They are 5-50x more numerous than neurons and can multiply and divide in the mature NS.
Define "electrical excitability".
The capability of excitable cells to produce action potentials or impulses in response to stimuli.
Describe the structural parts of a neuron and state the functions of each.
- Cell body (soma): Contains nucleus, cytoplasm, and organelles for energy and synthesis (e.g., neurotransmitters). Most lack centrioles and cannot divide.
- Processes: Arm-like extensions from the cell body.
- Dendrites: Receiving or input portion of a neuron; convey incoming messages toward the cell body as graded potentials.
- Axon: Propagates nerve impulses (action potentials) away from the cell body toward another neuron, muscle, or gland; contains voltage-gated Na^+ and K^+ channels.
- Axon hillock: Elevation where the axon joins the cell body.
- Initial segment: The first part of the axon.
- Trigger zone: Junction of the axon hillock and initial segment; site where most neural impulses arise.
- Axon terminals: Fine processes at the end of the axon and its collaterals.
- Synaptic end bulbs (synaptic terminals): Swollen tips of some axon terminals; contain synaptic vesicles that store neurotransmitters.
Define Nuclei (in the NS context).
Clusters of cell bodies in the Central Nervous System (CNS).
Define Ganglion.
Clusters of cell bodies that lie along the nerves in the Peripheral Nervous System (PNS).
Define Tracts.
Bundles of neuron processes in the Central Nervous System (CNS).
Define Nerves.
Bundles containing 100-1000s of axons plus associated connective tissue and blood vessels in the Peripheral Nervous System (PNS).
What are the 3 structural classifications of neurons?
- Multipolar neurons: Have several dendrites and 1 axon (most neurons in brain/spinal cord; all somatic motor neurons).
- Bipolar neurons: Have 1 main dendrite and 1 axon (found in retina, inner ear, olfactory area).
- Unipolar neurons: Sensory neurons; dendrites monitor a sensory stimulus (most PNS sensory neurons).
Which structural class do somatic motor neurons belong to?
Multipolar neurons.
Which structural class do most sensory neurons of the peripheral NS belong to?
Unipolar neurons.
What are the 3 functional classifications of neurons?
- Sensory (afferent) neurons: Convey impulses to the CNS.
- Motor (efferent) neurons: Convey instructions from CNS to peripheral effectors.
- Interneurons (association neurons): Located mostly within the brain and spinal cord, involved in complex responses and higher functions.
How are somatic sensory neurons different from visceral sensory neurons?
- Somatic sensory neurons: Monitor the outside world and our position within it.
- Visceral sensory neurons: Monitor internal conditions and the status of other organ systems.
Define Interoceptors.
Monitor digestive, respiratory, cardiovascular, urinary, and reproductive systems; provide sensations of taste, deep pressure, and pain.
Define Exteroceptors.
Provide information about the external environment such as touch, temperature, or pressure sensations, and senses of sight, smell, and hearing.
Define Proprioceptors.
Monitor the position and movement of skeletal muscles and joints.
How is a somatic motor neuron different from a visceral motor neuron?
- Somatic motor neurons: Innervate skeletal muscles at the neuromuscular junctions (voluntary control).
- Visceral motor neurons: Innervate smooth muscle, cardiac muscle, glands, and adipose tissue (involuntary control via ANS).
Where are most of the interneurons (association neurons) located?
Almost all interneurons are located within the brain and spinal cord.
List types of neuroglia and their main functions.
- Astrocytes: Maintain the blood-brain barrier (BBB).
- Oligodendrocytes: Produce myelin sheaths in the CNS.
- Microglia: Monitor neuron health and act as phagocytes.
- Ependymal Cells: Line brain ventricles and spinal cord central canal; role in CSF production.
- Schwann (neurilemmal) Cells: Produce myelin sheaths in the PNS.
- Satellite Cells: Regulate the environment surrounding neurons in the PNS.
What are the benefits of neuronal axon myelination?
Myelin sheaths:
- Protect and electrically insulate fibers from one another.
- Increase the speed of transmission of nerve impulses.
What are Nodes of Ranvier?
Gaps in the myelin sheath that appear at intervals along the axon.
What is the difference between gray matter and white matter?
- White Matter: Aggregations of myelinated processes in regions of the brain and spinal cord.
- Gray Matter: Consists of neuronal cell bodies, dendrites, unmyelinated axons, axon terminals, and neuroglia.
What are the two types of electrical signals used by neurons?
- Action Potentials: Allow communication over both short and long distances.
- Graded Potentials: Used for short distances only.
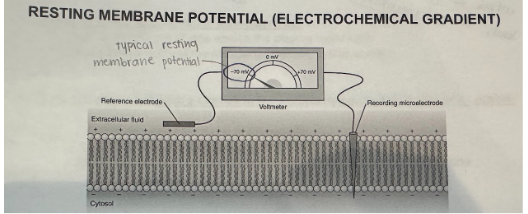
Which two basic features of excitable cells allow for the production of graded potentials and action potentials?
- Existence of a resting membrane potential (RMP): An electrical voltage difference across the plasma membrane.
- Presence of specific ion channels: These channels open and close in response to specific stimuli, allowing ion diffusion.
Define resting membrane potential (RMP).
The electrical voltage difference across the plasma membrane of excitable cells, which exists due to a small buildup of negative ions inside and positive ions outside. Typically range from -40 mV to -90 mV in neurons (-70 mV is a common value).
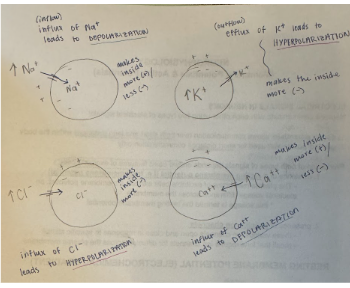
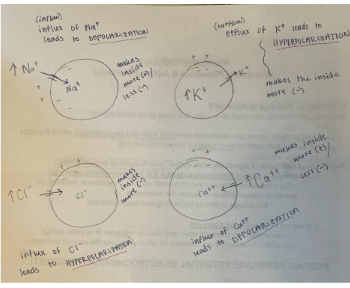
Define Depolarization.
A reduction in membrane potential where the inside of the membrane becomes less negative (more positive) than the resting membrane potential.
Define Refractory Period.
A period of time during which an excitable cell cannot generate another action potential.
Define Absolute Refractory Period.
The period of time during which a second action potential CANNOT be initiated, even with a very strong stimulus.
Define Relative Refractory Period.
The period of time during which a second action potential can be initiated, but only by a suprathreshold stimulus.
Define Hyperpolarization.
The membrane potential becomes more negative (less positive) than the resting membrane potential.
Define Nerve Impulse (Action Potential).
A sequence of rapidly occurring events that decrease and eventually reverse the membrane potential and then restore it to the resting state. It is the primary mode of communication in neurons and can travel long distances without dying out. A nerve impulse.
Compare the following types of ion channels: leakage, voltage gated, ligand gated, and mechanically gated.
- Leakage (open most of the time) Gated Channels: Special proteins that are generally open, allowing continuous passage of ions.
- Chemically (ligand) Gated Channels: Open when a specific chemical (ligand) binds to the channel (e.g., neurotransmitter binding).
- Voltage Gated Channels: Open when there is a change in the electrical charge (voltage) across the cell membrane (e.g., during a nerve impulse).
- Mechanically Gated Channels: Open when the membrane is stretched or pressure is applied (e.g., in touch receptors).
What type of channels are needed for Action Potential generation?
Voltage-gated Na^+ and K^+ channels are required for action potential generation and are located on the axon only.
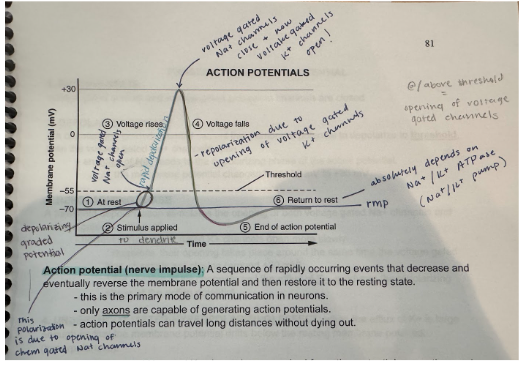
Know the various phases of an action potential (including values for RMP, threshold, and max depolarization).
- Resting State (-70 mV): Voltage-gated Na^+ and K^+ channels are closed.
- Depolarizing Phase (from -55 mV to +30 mV): If depolarization reaches threshold, voltage-gated Na^+ channels open, leading to an influx of Na^+ (rapid depolarization).
- Repolarizing Phase: Voltage-gated Na^+ channels inactivate, and slower voltage-gated K^+ channels open, leading to an efflux of K^+ (repolarization).
- Undershoot (After-Hyperpolarizing Effect): Efflux of K^+ is large enough to cause the membrane potential to drift below the resting membrane potential (hyperpolarization) before returning to RMP.
What ionic events are associated with the various phases of an action potential?
- Resting State: Voltage-gated Na^+ and K^+ channels are closed.
- Depolarization: Voltage-gated Na^+ channels open when depolarized to threshold, causing an influx of Na^+ into the cell.
- Repolarization: Voltage-gated Na^+ channels inactivate, and voltage-gated K^+ channels open (more slowly), leading to an efflux of K^+ out of the cell.
- Undershoot (After-hyperpolarization): Continued efflux of K^+ causes the membrane potential to become more negative than the RMP for a brief period.
What events are taking place during the depolarization phase?
If a depolarizing graded potential causes the membrane potential to depolarize to threshold (-55 mV), then voltage-gated Na^+ channels open, leading to a rapid influx of Na^+ and changing the membrane potential to +30 mV.
What events are taking place during the repolarization phase?
A threshold depolarization stimulates the opening of both voltage-gated Na^+ and K^+ channels. The voltage-gated K^+ channels open more slowly, typically around the same time voltage-gated Na^+ channels are closing (+30 mV). The opening of K^+ channels and the efflux of K^+ produces the repolarizing phase.
Why is there an after-hyperpolarization phase?
The after-hyperpolarization phase occurs when the efflux (outflow) of K^+ is large enough that the membrane potential briefly drifts below the resting membrane potential, making it more negative (hyperpolarizes).
What is the role of the Na^+/K^+ ATPase (pump)?
The Na^+/K^+ exchange pump is essential for maintaining ion concentrations within limits, especially after rapid firing of action potentials. It ensures that Na^+ and K^+ ions are pumped back to their respective sides of the membrane (3 Na^+ out for every 2 K^+ in) to restore the resting membrane potential.
Describe the characteristics of a graded potential.
A stimulus produces a temporary, localized change in the resting potential that decreases with increased distance from the stimulus. These small deviations can make the membrane either more or less polarized and occur most often in dendrites and cell bodies.
The membrane can become either:
More polarized
Less polarized
Occur most often in the dendrites and cell body of a neuron
Produce graded potentials only because they lack voltage gated Na+ and K+ channels
They have chemically gated Na+ channels
Axons have voltage gated Na+ and K+ channels
Vary in amplitude (size)m depending on the strength of the stimulus
They are larger or smaller, depending on the number of ion channels that have opened (or closed), and how long they stay open
The current dies out shortly
Therefore, graded potentials are only good for short-distance communications, but are essential in initiating action potentials
Graded potentials produced on the dendrites and cell body are responsible for generating action potentials on the axon, which travel to the synaptic terminal
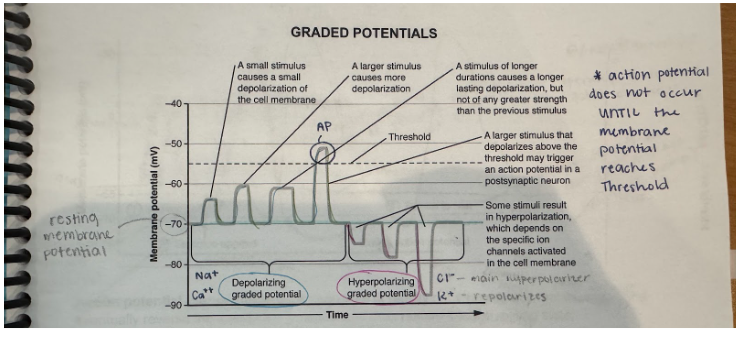
What type of channels are needed for the generation of graded potentials?
Chemically gated Na^+ channels (responsible for generating graded potentials in dendrites and cell bodies where voltage-gated channels are absent).
What is a hyperpolarizing graded potential?
A hyperpolarizing graded potential occurs when the membrane becomes more polarized (more negative), typically due to the influx of Cl^- or efflux of K^+.
What is a depolarizing graded potential?
A depolarizing graded potential occurs when the membrane becomes less polarized (less negative/more positive), typically due to the influx of Na^+ or Ca^{++}.
What is the "all or none principle" of action potentials?
The principle stating that if depolarization reaches a certain threshold (between -60 to -55 mV), an action potential will occur, always with the same size (amplitude), regardless of the stimulus strength. If threshold is not reached, no action potential (none at all) will fire.
What does action potential "propagation" mean?
Propagation (conduction) refers to the self-propagation of a nerve impulse along the membrane of an axon, typically moving in one direction only. The action potential reaching the synaptic knob has the same magnitude as the one generated at the initial segment.
How is saltatory conduction different from continuous conduction?
- Continuous Conduction: Occurs in unmyelinated axons, where the action potential propagates stepwise across every segment of the axon membrane.
- Saltatory Conduction: Occurs in myelinated axons (and muscle fibers), where the action potential "jumps" from one Node of Ranvier to the next. This is faster and more energy-efficient than continuous conduction.
What factors determine the speed of propagation of nerve impulses? How do these factors influence the speed of propagation?
- Axon Diameter: Larger diameter axons conduct impulses faster.
- Myelination: Myelinated axons conduct impulses faster (saltatory conduction).
- Temperature: Increased temperature generally increases nerve transmission speed; cold decreases it.
How is the intensity of a stimulus encoded in the nervous system?
- Frequency of impulses: How often action potentials are generated.
- Number of sensory neurons recruited: A stronger stimulus can activate more sensory neurons.
Define Synapse.
The site of communication between two neurons or between a neuron and an effector cell (e.g., muscle fiber, gland).
What are the two types of synapses? Which one uses gap junctions? Which one uses chemicals (Neurotransmitters)?
- Electrical Synapses: Action potential spreads directly through gap junctions between adjacent cells; involve direct physical contact. Advantages include faster communication and synchronization.
- Chemical Synapses: Involve neurotransmitters; the most common type in the NS. Advantages include adjustment and fine-tuning of postsynaptic cell activity.
What is a presynaptic cell and what is a postsynaptic cell (in chemical synapses)?
- Presynaptic cell (neuron): Sends the message.
- Postsynaptic cell: Receives the message (can be a neuron or another cell type like skeletal muscle).
Which type of synapse (chemical or electrical) is the most common in the NS?
The most common type of synapse in the NS is chemical synapses.
Explain the events of signal transmission at a chemical synapse.
- Action potential arrives at the synaptic end bulb of a presynaptic axon.
- Action potential opens voltage-gated Ca^{++} channels, causing Ca^{++} influx.
- Increased intracellular Ca^{++} triggers exocytosis of synaptic vesicles, releasing neurotransmitters (NT) into the synaptic cleft.
- NT molecules diffuse across the cleft and bind to NT receptors on the postsynaptic neuron's plasma membrane.
- NT binding opens ligand-gated ion channels, allowing specific ions to flow across the membrane, causing depolarization or hyperpolarization of the postsynaptic membrane.
- If depolarization reaches threshold, one or more action potentials are generated in the axon of the postsynaptic neuron.
Define Synaptic Fatigue.
When the neurotransmitter store cannot keep up with the demand for NT, leading to inactivation of the synapse until more neurotransmitters are available.
What are excitatory and inhibitory neurotransmitters? Provide a few examples.
- Excitatory NTs: Cause depolarization and promote action potential generation (e.g., Acetylcholine at neuromuscular junction).
- Inhibitory NTs: Cause hyperpolarization and inhibit action potential generation (e.g., GABA, Acetylcholine at some other synapses).
Define neurotransmitter Agonist.
An agent that enhances synaptic transmission or mimics the effect of a natural neurotransmitter.
Define neurotransmitter Antagonist.
An agent that blocks the action of a neurotransmitter.
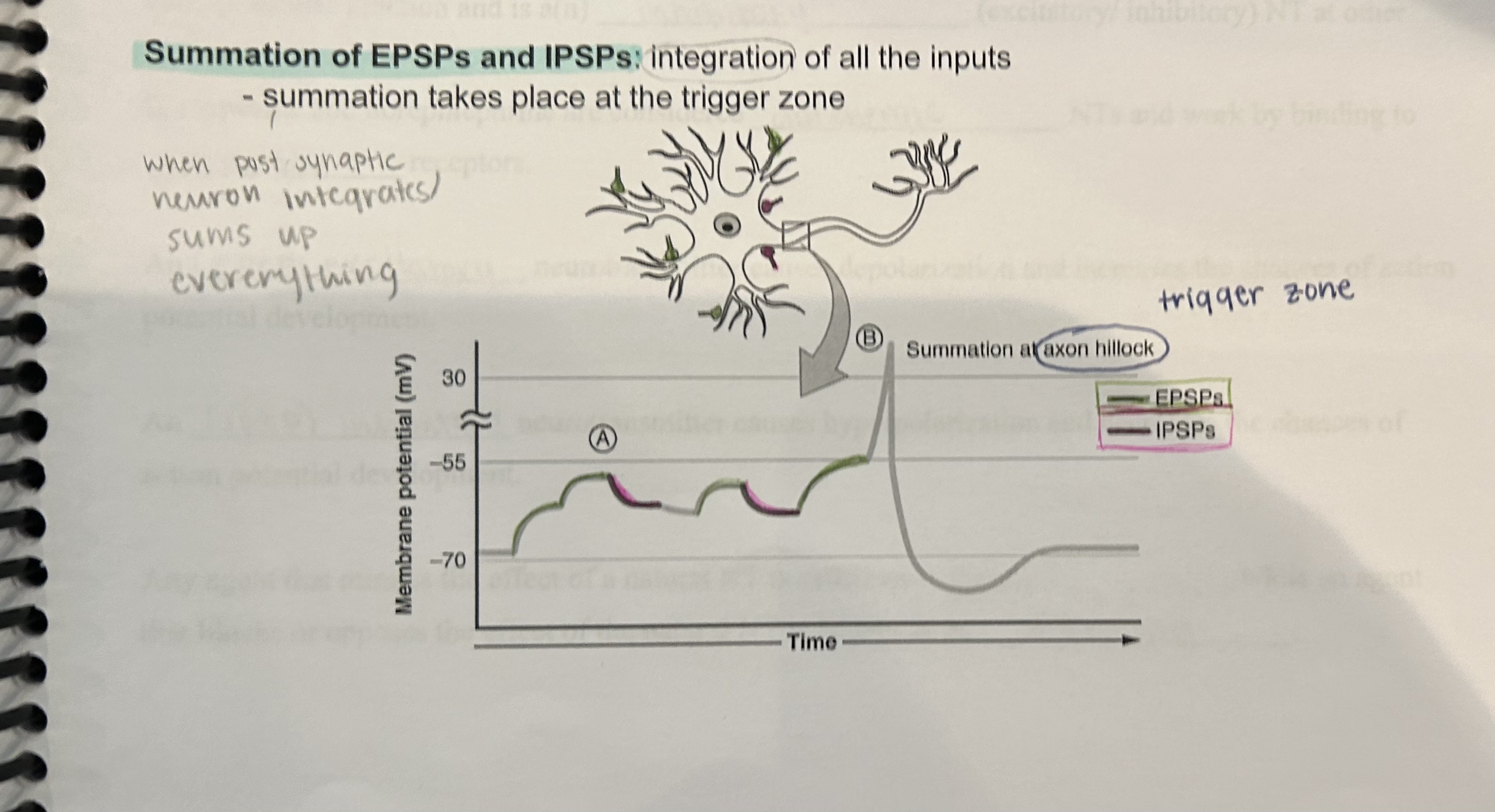
Distinguish between Excitatory Postsynaptic Potential and Inhibitory Postsynaptic Potential.
- Excitatory Postsynaptic Potential (EPSP): A depolarizing postsynaptic potential caused by an excitatory NT, bringing the membrane closer to threshold. A single EPSP usually does not initiate a nerve impulse.
- Inhibitory Postsynaptic Potential (IPSP): A hyperpolarizing postsynaptic potential caused by an inhibitory NT, increasing the membrane potential by making the inside more negative and farther away from threshold.
Define threshold.
The minimum level of depolarization required for an action potential to be generated.
Define After-hyperpolarizing phase (undershoot).
The hyperpolarization that occurs after the repolarizing phase of an action potential.
Define Repolarization.
Recovery of the resting potential due to the opening of voltage-gated K+ channels and closing of voltage-gated Na+ ion channels.
Ion channels required for the generation and conduction of action potentials is _____.
Voltage-gated ion channels.
Ion channels that are always open is ____.
Leakage channels.
Gated ion channels found primarily on the axon of a neuron is ____.
Voltage-gated ion channels.
Gated ion channels found primarily on the dendrite and cell body of a neuron is ____.
Ligand-gated ion channels.
Ion channels that open and close in response to a specific chemical stimulus (NT) is ____.
Ligand-gated ion channels.
Ion channels that open in response to changes in membrane potential is ____.
Voltage-gated ion channels.
Give three specific examples and locations of voltage gated ion channels that you are familiar with (think neuron and skeletal muscle fibers).
Voltage-gated Na+ —> located in axon of neurons.
Voltage-gated K+ —> located in axon of neurons.
Voltage-gated Ca++ —> located in synaptic end bulbs.
When the membrane potential of a plasma membrane becomes more polarized, it has become _____ (more/less) negative.
More negative (hyperpolarized).
When the membrane potential of a plasma membrane becomes less polarized, it has become _____ (more/less) negative.
Less negative (depolarized).
A more negative polarization is termed ____ graded potential.
Hyperpolarization.
A less negative polarization is termed ____ graded potential.
Depolarization.
A typical neuron has a resting membrane potential of ____ mV and a threshold value of ____ mV.
-70 mV ; -55 mV
T or F: a neuron cell membrane can be hyperpolarized either by an influx of negatively charged ions or by an outflow of positively charged ions.
True
Define Synaptic Delay.
The delay that occurs between the arrival of the action potential at the synaptic end bulb and the effect it has on the postsynaptic membrane (i.e. the time required for the process at the chemical synapse, such as Ca++ influx and NT release).
This is why reflexes are so vital for survival.
The fewer synapses involved, the shorter the total synaptic delay and therefore, the faster the response.
Chemical synapse is an example of this.
Define Summation of EPSPs and IPSPs.
Integration of all the inputs.
Summation takes place at the trigger zone.
When postsynaptic neuron integrates/sums up everything.
What several ways can the effects of NTs at chemical synapses be modified?
NT synthesis can be stimulated or inhibited
NT release can be blocked or enhanced
NT removal can be stimulated or inhibited
the receptor site can be blocked or activated
Give me examples of NTs.
Acetylcholine (ACh)/ cholinergic synapses:
an excitatory NT at the neuromuscular junction
an inhibitory NT at other synapses
amino acids:
gamma aminobutyric acid (GABA): inhibitory: GABA may reduce anxiety
biogenic amines:
norepinephrine (adrenergic synapses)
epinephrine (adrenergic synapses)
dopamine.
Ex: Parkinson's disease: (due to decreases in dopamine levels). At all other places in the brain, dopamine can be excitatory.
serotonin
deficiency of this NT is associated with many cases of severe chronic depression.
SSRIs (selective serotonin reuptake inhibitors): these chemicals (i.e. Paxil, Prozac, Zoloft) increase the concentration of serotonin at the synapse by inhibiting its reabsorption and therefore, degradation.