L3 - Epithelium II
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
54 Terms
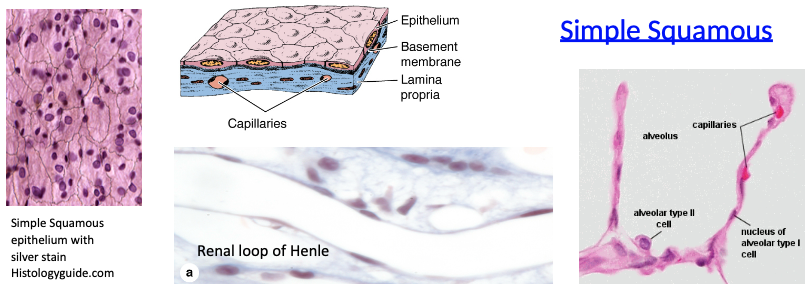
What are the features and functions of simple squamous epithelium?
Made of thin, flat cells with flat nuclei
Lines blood vessels (endothelium), air sacs (alveoli), and body cavities (mesothelium)
Allows for rapid exchange or diffusion of substances
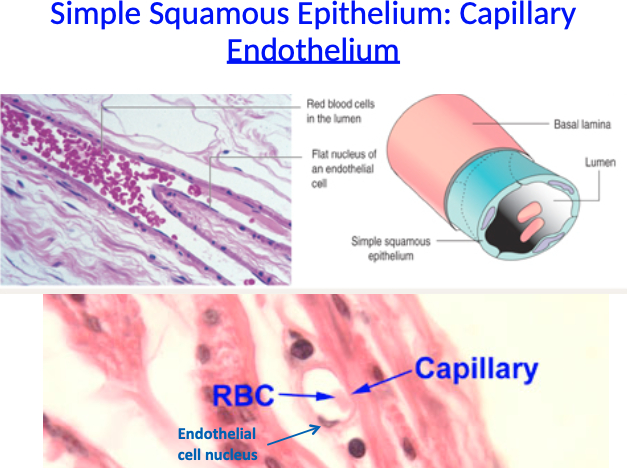
What is capillary endothelium and what type of epithelium is it made of?
Capillary endothelium is the inner lining of capillaries
Made of simple squamous epithelium
Consists of flat endothelial cells with flat nuclei, allowing efficient exchange of gases and nutrients
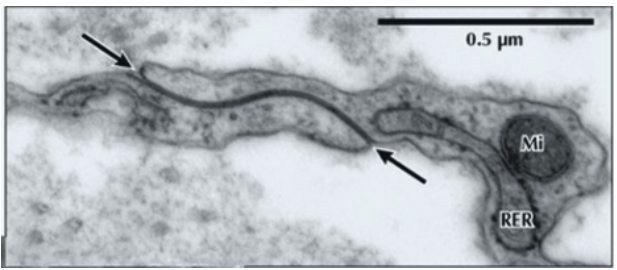
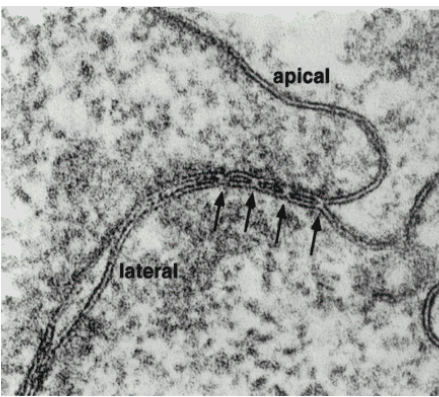
EM of tight junction between 2 simple squamous epithelial cells:
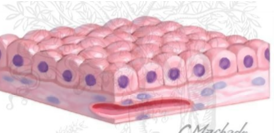
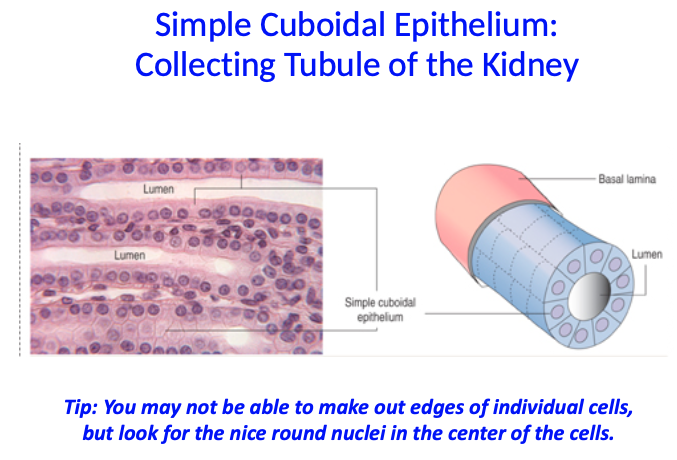
What are the features and functions of simple cuboidal cells?
As tall as they are wide
Round nuclei
Absorption and secretion
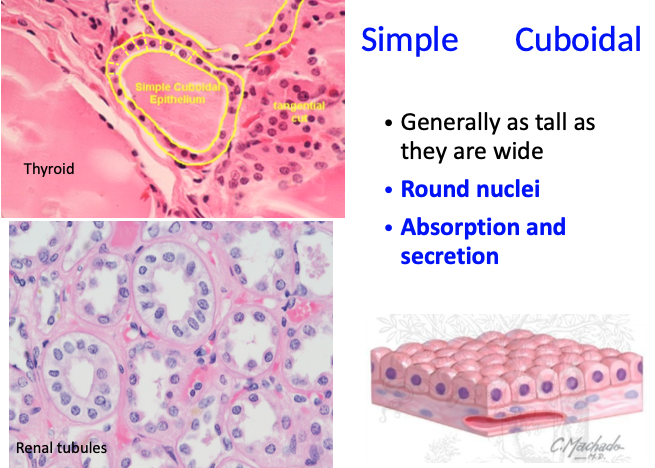
Simple cuboidal epithelium - collecting tubule of kidney:
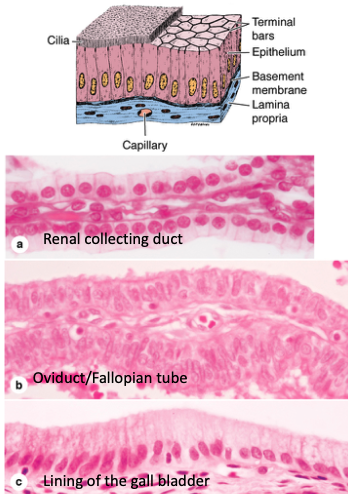
What are the features and functions of simple columnar epithelium?
Cells are taller than they are wide
Nuclei are round or oval, located basally or centrally
Specialized in absorption
May have microvilli or cilia, and often contain goblet cells (e.g. in intestines)
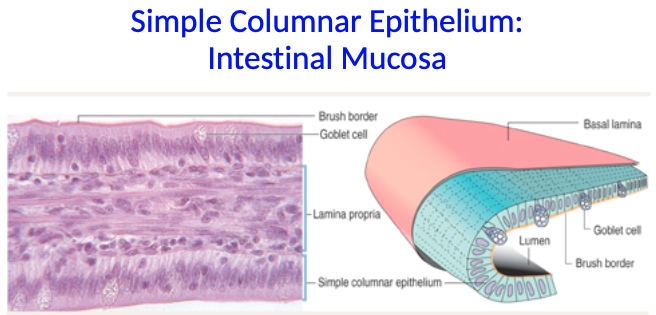
What are key features of simple columnar epithelium in the intestinal mucosa?
Has an elongated nucleus in the medial portion of the cell
Microvilli on the apical surface form a brush border
Goblet cells contain mucus in their apical cytoplasm, which is secreted to coat the epithelium
Stratified epithelium:
More than one cell layer thick
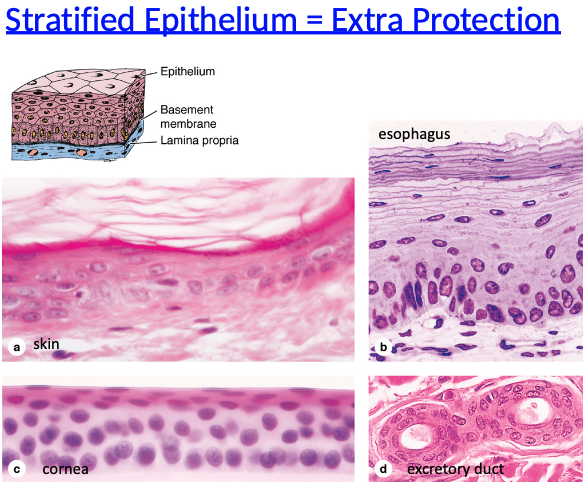
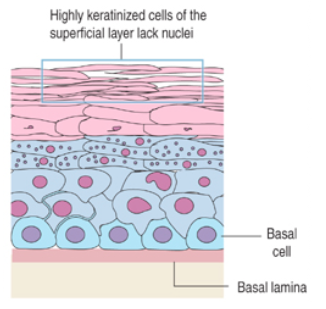
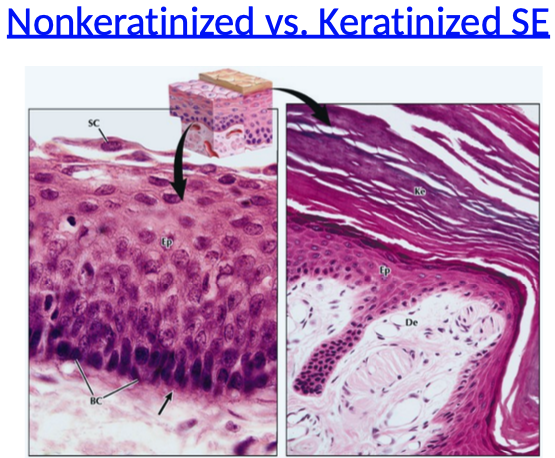
What are the two types of stratified squamous epithelium and where are they found?
Keratinized: found in dry areas like the epidermis, prevents moisture loss
Nonkeratinized: found in wet areas like the esophagus and mucous membranes
What is the role of basal cells in stratified squamous epithelium?
Basal cells undergo mitosis and push new cells upward
As cells rise, they differentiate and flatten
Keratinized cells in the superficial layer lose their nuclei
Non-keratinized vs. Keratinized SE:
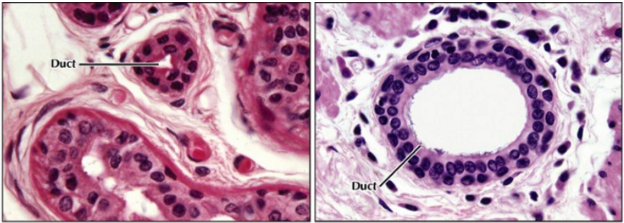
Where is stratified cuboidal epithelium found and what is its structure?
Not common; mostly found in glandular ducts
Usually consists of two layers of cuboidal cells
Where is stratified columnar epithelium found and how common is it?
Not common
Found in the male urethra and palpebral conjunctiva (inner eyelid)
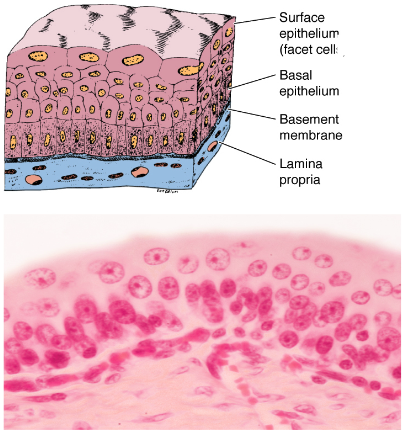
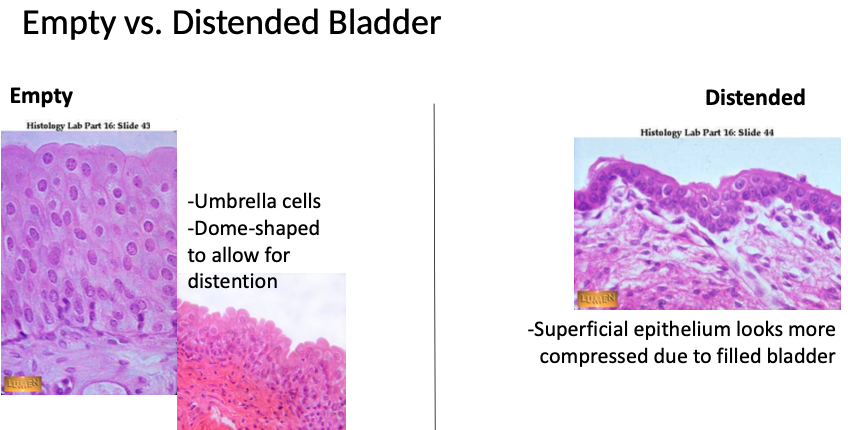
What are the structural features of transitional epithelium?
Has dome-shaped superficial cells called umbrella cells
These cells have specialized membranes for protection
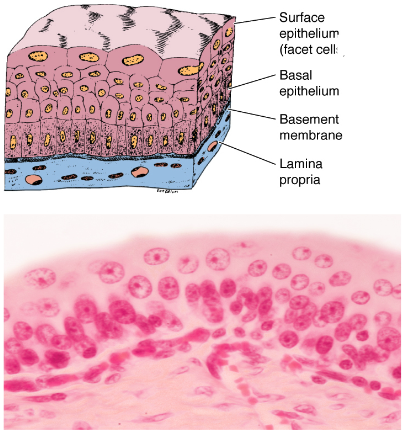
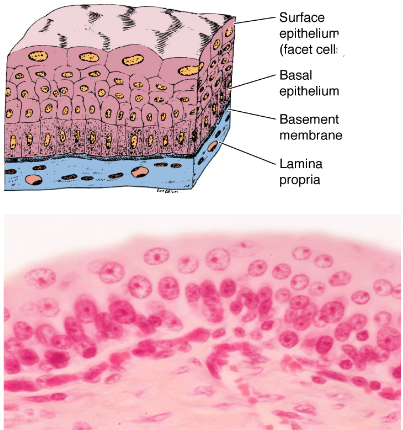
What is the function and location of transitional epithelium (uroepithelium)?
Allows for stretching and distension
Found in the bladder, ureters, urethra, and prostate
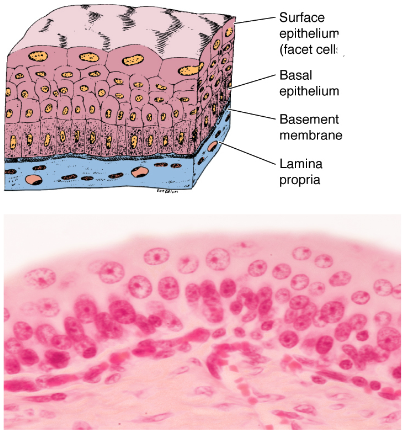
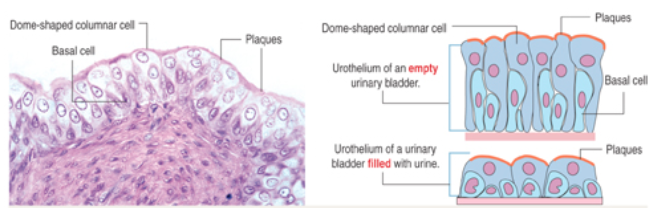
What is the role of dome-shaped cells in transitional epithelium of the bladder?
Dome-shaped columnar cells can change shape in response to tension (e.g. bladder filling)
They are protected by protein plaques at their apical surface, shielding from hypertonic urine
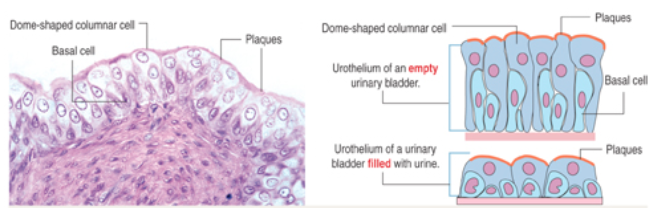
What are basal cells in transitional epithelium and where are they located?
Basal cells are columnar to cuboidal in shape
They attach to the basal lamina but do not reach the lumen
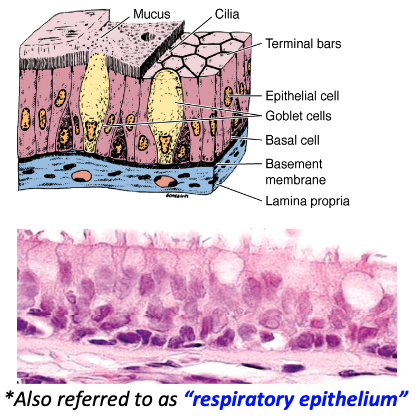
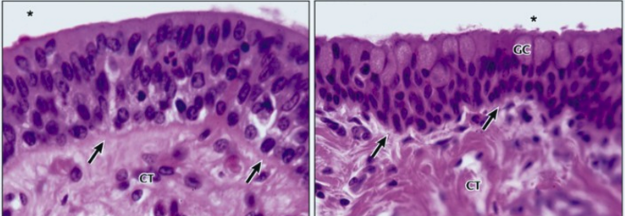
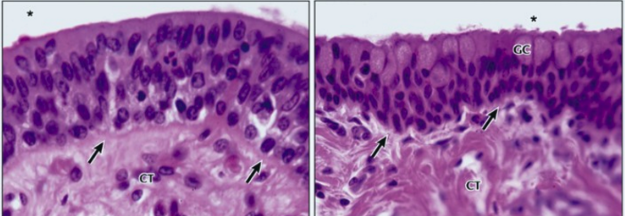
What is pseudostratified epithelium and why does it appear layered?
Appears layered due to crowded cells and irregular nuclei
It’s actually a single layer because every cell touches the basement membrane
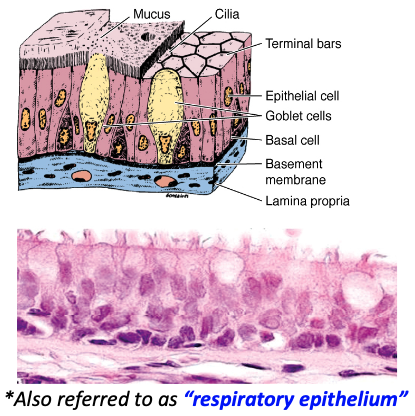
What are common features and associations of pseudostratified epithelium?
Usually ciliated
Often found with goblet cells
Also called respiratory epithelium
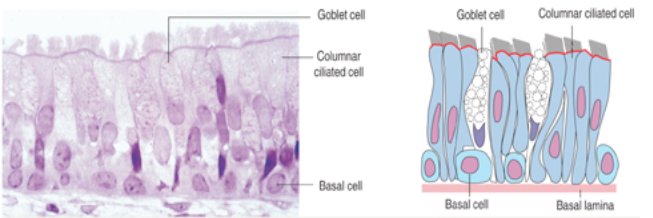
What are the key cell types in pseudostratified columnar epithelium of the trachea and their functions?
Columnar cells: have cilia to move mucus
Basal cells: anchored to the basal lamina, don't reach the lumen
Goblet cells: secrete mucus
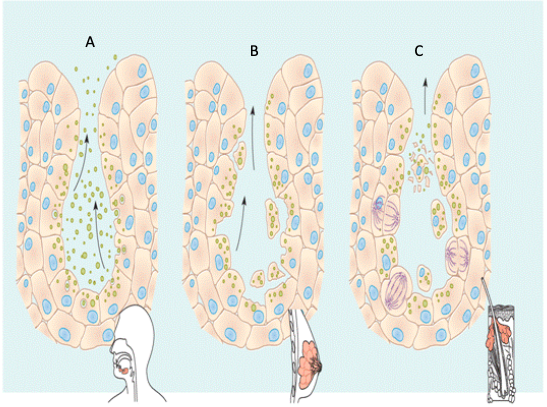
Development of glands:
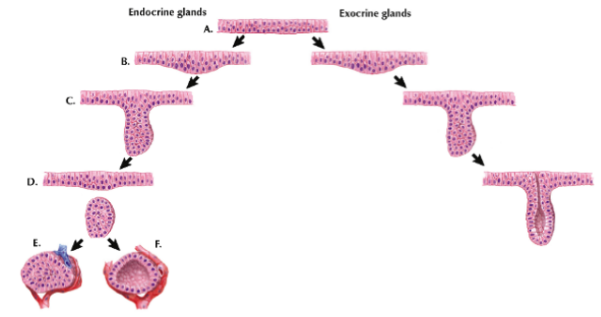
How do exocrine and endocrine glands form from covering epithelium?
Exocrine glands: form by epithelial down-growth; retain a duct and secrete onto a surface
Endocrine glands: the stalk degenerates; they secrete into the blood via nearby capillaries
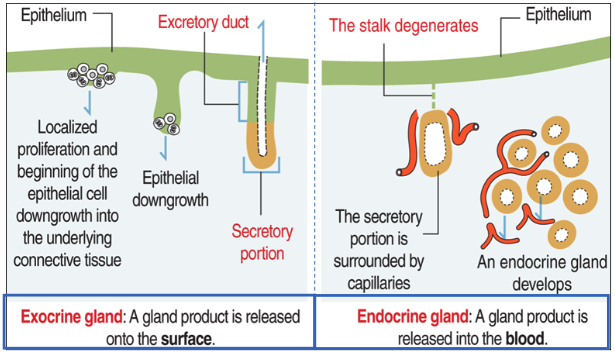
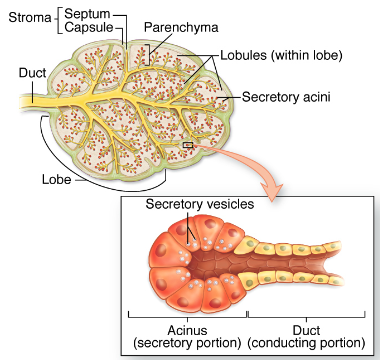
General structure of an exocrine gland:
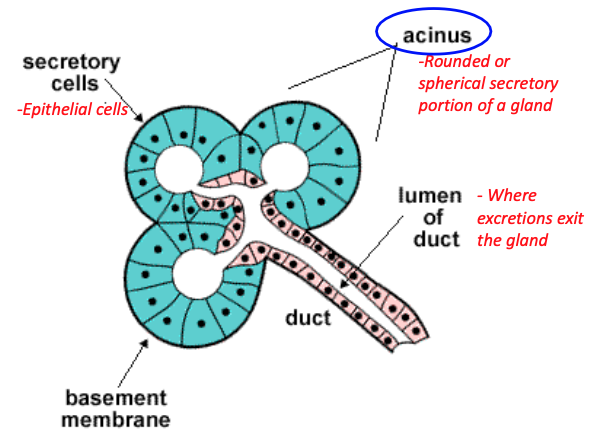
General structure of an exocrine gland:
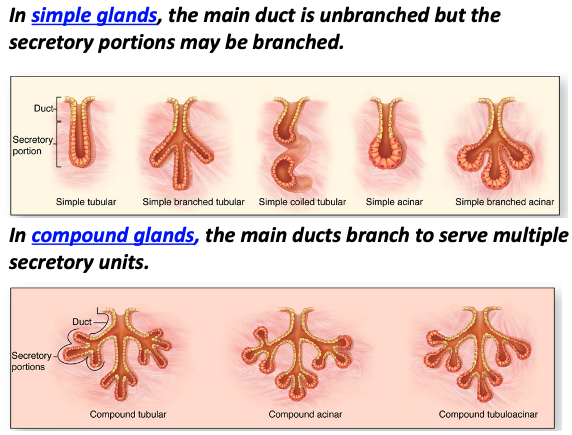
Simple vs. Compound glands:

What is merocrine secretion and where does it occur?
Secretion of protein products by exocytosis of secretory granules
Example: salivary gland
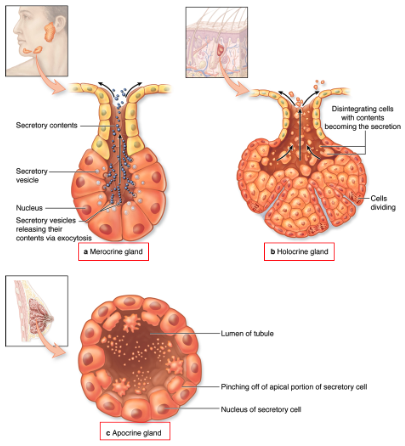
What is holocrine secretion and where does it occur?
Secretion is released by total disintegration of the cell
Example: sebaceous gland
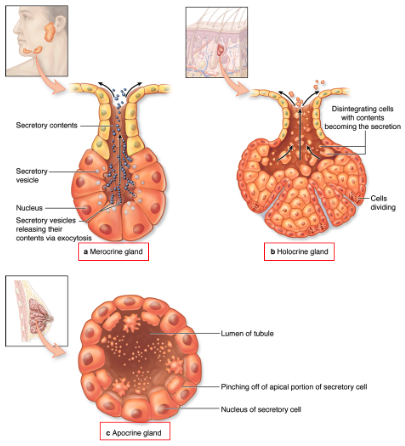
What is apocrine secretion and where does it occur?
Secretion involves loss of apical portion of the cell with lipid droplets
Example: mammary gland
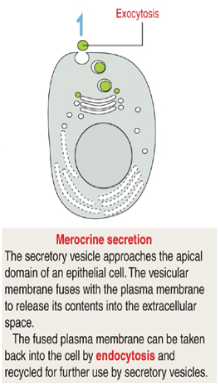
What is merocrine secretion and how does it work?
Secretory vesicles fuse with the apical membrane to release contents via exocytosis
The membrane can be recycled by endocytosis
Example: milk protein (casein) in mammary glands
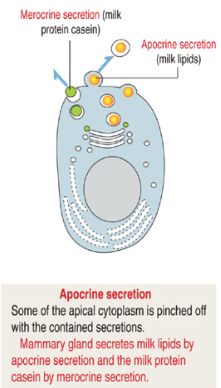
What is apocrine secretion and what does it release?
Apical cytoplasm is pinched off with the secretory contents
Releases milk lipids in mammary glands
Cytoplasm is lost along with the secretions
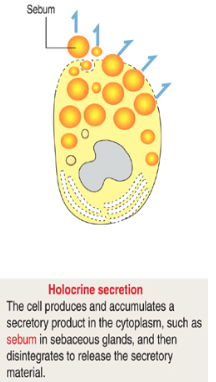
What is holocrine secretion and what happens to the cell?
The cell accumulates secretory product, then disintegrates to release it
Seen in sebaceous glands secreting sebum
How does holocrine secretion occur in sebaceous glands?
Cells disintegrate, releasing their cytoplasm and contents
Secretions are emptied into a hair follicle
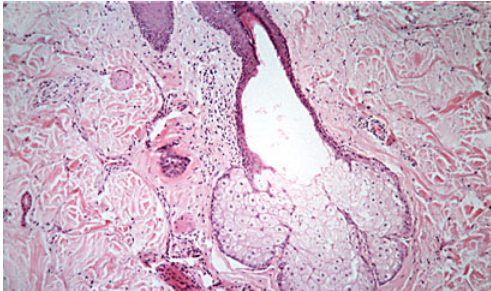
Apocrine secretion - mammary gland:

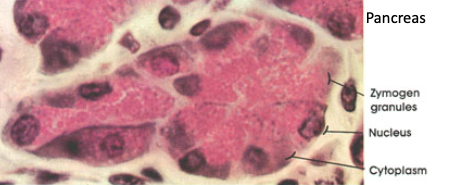
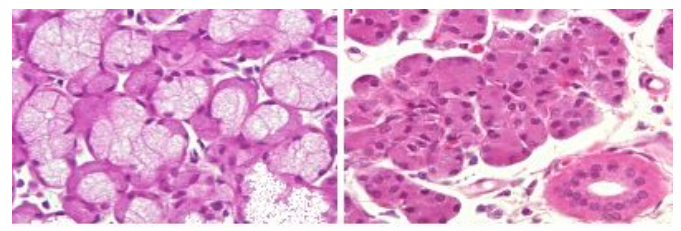
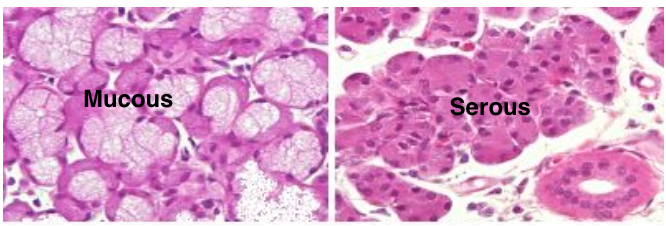
What type of secretion do serous merocrine glands produce?
Serous glands secrete liquid or watery secretions
Example: pancreas
Why are the apical and basal ends of serous cells stained differently?
Apical ends are eosinophilic due to secretory vesicles (pink stain)
Basal ends are basophilic due to abundant RER and nucleus displacement (purple/blue stain)
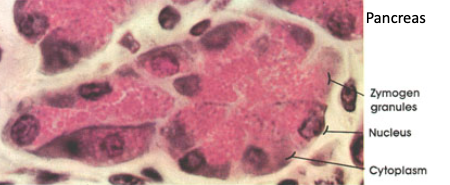
What structures are found in serous gland cells (e.g. pancreas)?
Zymogen granules at the apical side
Nucleus at the basal side
Prominent cytoplasm filled with secretory machinery
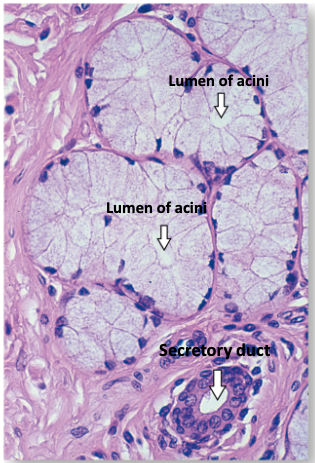
What do mucous merocrine glands secrete and how do they compare to serous glands?
Secrete thick, viscous glycoproteins (mucus)
Cells are larger than serous cells
Found in mucous acini with pale-staining apical regions
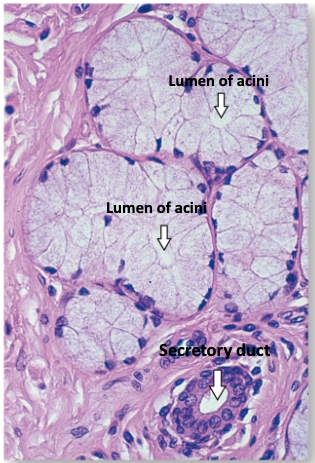
What are the features of mucous gland cell regions?
Apical region: filled with pale mucin granules
Basal region: contains a flattened nucleus, RER, and well-developed Golgi
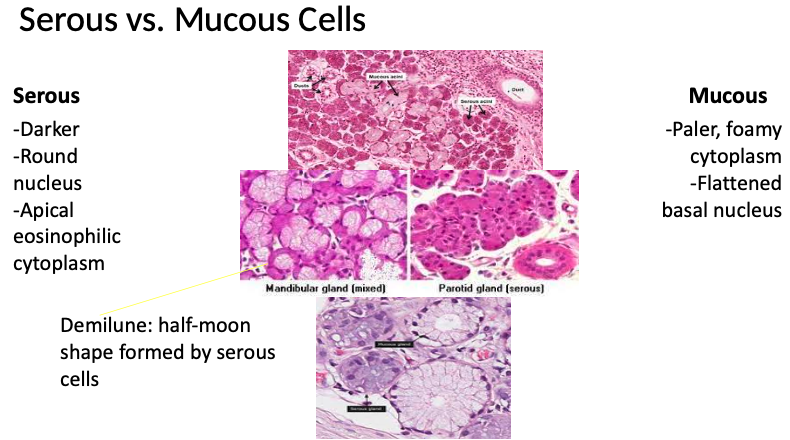
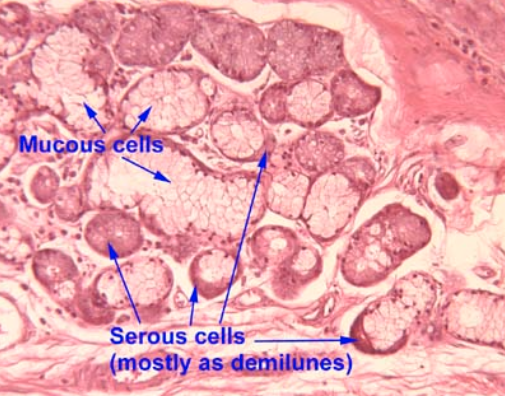
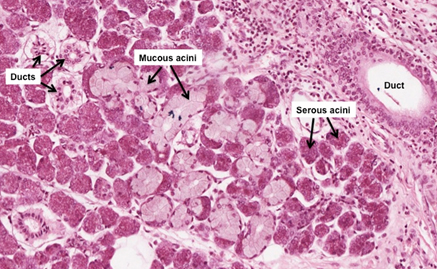
What are mixed glands and where are they found?
Glands that contain both mucous and serous cells
Found in salivary glands
What are the features of mucous and serous cells in mixed glands?
Mucous cells: flattened basal nuclei, clear spongy cytoplasm
Serous cells: round basal nuclei, eosinophilic apical cytoplasm with reddish granules
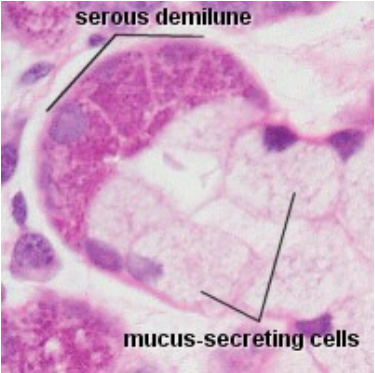
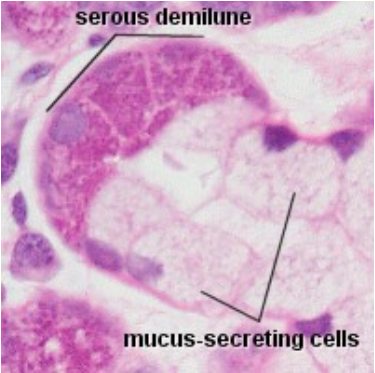
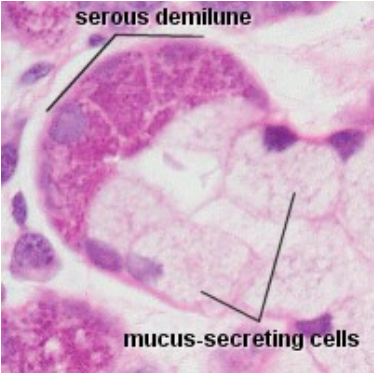
What is a serous demilune?
A half-moon shaped cluster of serous cells
Located at the edge of mucous acini, releasing secretions into spaces between mucous cells
Glands in the trachea:
Serous vs. Mucous glands:
Where does epithelial regeneration occur and when is it most pronounced?
Occurs throughout most of the body
Most pronounced in exposed surfaces, holocrine glands, intestinal tract, and female reproductive tract
Why is epithelium a target of chemotherapy, and what are the side effects?
Chemotherapy targets rapidly dividing cells, including epithelium
Side effects include nausea, vomiting, hair loss, and anemia due to epithelial cell death
How does epithelial regeneration change with age?
Regeneration capabilities decline with increasing age
What are the types of epithelial tumors?
Adenoma: benign epithelial (glandular) growth
Carcinoma: malignant tumor from surface epithelium
Adenocarcinoma: malignant tumor from glandular epithelium
Most common tumor type in adults over age 45
Which contains mostly serous, which contains mostly mucous?
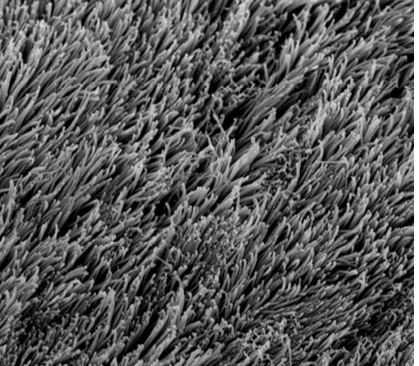
What is this?
Cilia → consistent length and density, no branching, longer and not as dense as microvilli
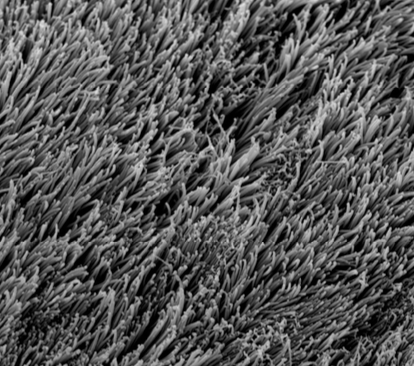
Identify this.
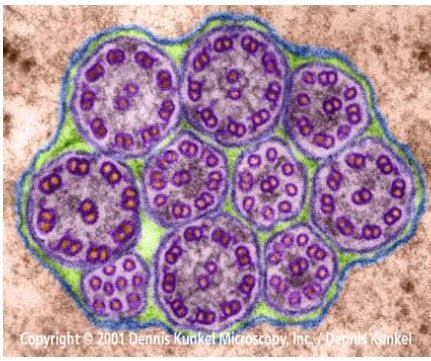
Cilia (remember 9+2 organization)
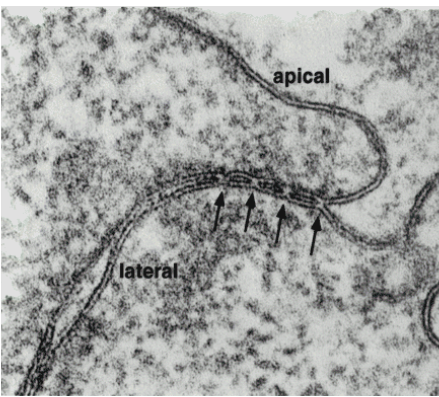
What are the arrows pointing to?
Tight junctions (zonula occludens)
(hint - located near apical end)
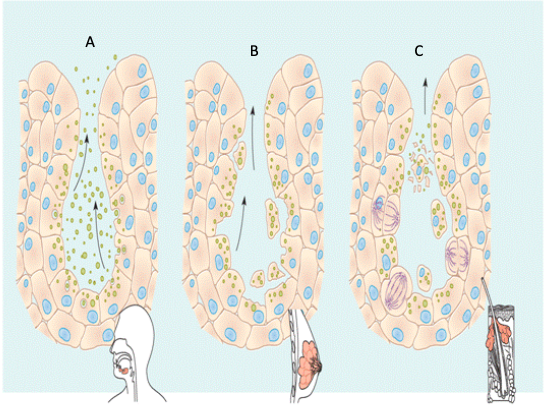
Identify each type of gland.
A = Merocrine
B = Apocrine
C = Holocrine
Empty vs. distended bladder:
Serous vs. mucous cells: